Abstract
Drug resistance is a major concern due to the evolution and emergence of pathogenic bacterial strains with novel strategies to resist the antibiotics in use. Mycobacterium tuberculosis (Mtb) is one of such pathogens with reported strains, which are not treatable with any of the available anti-TB drugs. This scenario has led to the need to look for some novel drug targets in Mtb, which may be exploited to design effective treatment strategies against the infection. The goal of this review is to discuss one such class of emerging drug targets in Mtb. MmpL (mycobacterial membrane protein large) proteins from Mtb are reported to be involved in multi-substrate transport including drug efflux and considered as one of the contributing factors for the emergence of multidrug-resistant strains. MmpL proteins belong to resistance nodulation division permeases superfamily of membrane transporters, which are viably and pathogenetically important and their inhibition could be lethal for the bacteria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mycobacterium genera have many non-pathogenic and opportunistic pathogenic species. Its pathogenic members also include human pathogens Mycobacterium tuberculosis (Mtb) and Mycobacterium leprae (M. leprae), the causative agent of two deadly infectious diseases, tuberculosis (TB) and leprosy, respectively (Forrellad et al. 2013). At present, tuberculosis is the leading cause of death due to bacterial infection in spite of the various available efficient treatment strategies. According to the World Health Organization (WHO) tuberculosis report 2016, 9.6 million people are infected with tuberculosis and 1.5 million died in 2014, out of which 0.4 million deaths were caused by HIV co-infection (WHO 2014, 2016). The failure of available treatments in use and emergence of drug-resistant strains is posing threat to the human population. The drug-resistant TB involves multidrug-resistant (MDR) strains, resistant to the first line of anti-TB drugs, namely, isoniazid (INH) and rifampicin (RMP) (Frieden et al. 1993), with the extensively drug-resistant (XDR) strains showing resistance to the second line of anti-TB drugs such as fluoroquinolones and injectable drugs, i.e., capreomycin, kanamycin and amikacin (Alexander and De 2007). The total drug-resistant (TDR) strains of Mtb were reported in 2009; these strains are not treatable with any of the available anti-TB drugs (Velayati et al. 2009). This development of drug resistance is a major obstruction in the global TB control programs (Parida et al. 2015) (Fig. 1).
Evolution of drug resistance in TB: Mtb has been evolving with various strains having different extents of resistance to available anti-TB drugs. In the earlier times, the TB was drug susceptible and treatable with the first-line anti-TB drugs. Later on, in the 1990s, cases of MDR-TB were reported with resistance to the first-line anti-TB drugs, RMP and INH (Frieden et al. 1993). In the year 2006, the XDR-TB term was defined for TB strains resistant to second-line anti-TB drugs, fluoroquinolone and injectable anti-TB drugs (Alexander and De 2007). In the year 2009, TDR-TB strains were reported with complete resistance against the first- and second-line anti-TB drugs (Velayati et al. 2009)
Multiple mechanisms operating exclusively or/and in combination may cause the evolution of highly pathogenic drug-resistant mycobacterial strains. The major mechanism behind the drug-resistant strains of bacteria is the mutation in the drug targets, the evolution of drug-degrading enzymes, modification of drug molecules by drug-inactivating enzymes and expulsion of drug from the bacterial cell by the drug efflux pump (Fig. 2) (Nikaido 1998).
The thick waxy cell wall of mycobacteria is constituted by mycolic acid which forms an insoluble cell envelope and acts as a primary defense apparatus against the host immune system. It also restricts entry of hydrophilic drugs inside the bacteria, thus making them ineffective and thereby reducing the permeability of the cell wall. Mycolic acid is synthesized by the associated and sequential action of enzymes fatty acid synthase I (FAS-I), fatty acid synthase II (FAS-II) and a polyketide synthase (Pks13) on very long-chain α-alkyl, β-hydroxy fatty acids. These components are also essential for the viability and virulence of the pathogen (Marrakchi et al. 2014).
Efflux pumps are the membrane transporters and linked to the drug resistance in bacteria. Some transporters, such as the tetracycline efflux proteins, are dedicated systems which mediate extrusion of a single drug or class of drugs. In contrast to these specific drug transporters, some multidrug efflux pumps may transport a diverse variety of structurally unrelated compounds. These multidrug transporters are divided into two major categories, i.e., primary multidrug transporters containing ATP-binding cassette known as ABC type, which uses the energy generated from ATP hydrolysis to pump drugs out of the cells, and secondary multidrug transporters, which utilize the protons or sodium ions-generated electrochemical gradient to drive the drug extrusion from the cells. The secondary multidrug transporters have four known major families, namely, major facilitator superfamily (MFS), multidrug and toxic efflux (MATE), resistance nodulation division (RND) and small multidrug resistant (SMR). RND is a ubiquitous family of efflux pumps and has known members from bacteria, archaea and eukaryotes. RND family transporters are widespread, especially among Gram-negative bacteria, and catalyze the proton-motive force (PMF)-driven active efflux of many antibiotics and chemotherapeutic agents. Some well-known RND proteins from Gram-negative bacteria exhibit similar but unusual topological features (Saier et al. 1994). These have 12 putative α-transmembrane helices (TMHs) and two large hydrophilic extra-periplasmic loops between TMH 1 and 2 and TMH 7 and 8 (Saier et al. 1994; Lange and Steck 1998). Transporters from the RND family are energized by the PMF similar to all other secondary drug transporters, with proton translocation occurring across the TM domain (Paulsen et al. 1996).
The efflux pumps of the RND family may contribute to the resistance to the widest range of antibacterial agents (Nikaido 1998; Schweizer 2003) and are also the major reported cause behind the multidrug-resistance phenomenon of many Gram-negative pathogenic bacteria, including Pseudomonas aeruginosa, Escherichia coli, Burkholderia pseudomallei, Neisseria meningitides, Haemophilus influenzae, Neisseria gonorrhoeae, Salmonella typhimurium, Stenotrophomonas maltophilia and Vibrio cholerae (Moore et al. 1999; Helms et al. 2002). The identification of 14 RND genes in the genome of Burkholderia cenocepacia suggests that active efflux could be a major mechanism underlying antimicrobial resistance of this pathogen (Guglierame et al. 2006).
The Mtb genome was reported to have 14 mmpL genes which translate into putative integral membrane proteins and lipid transporters. In some cases, they were reported to be responsible for drug efflux. These proteins were designated as MmpL (mycobacterial membrane protein large) on the basis of their large size and TM localization. When their topologies were studied, most of them were found to possess 10–12 TMHs, a characteristic feature of RND efflux proteins (Tekaia et al. 1999; Sandhu and Akhter 2015). MmpL proteins have been reported to transport lipid derivative molecules. Many mmpL genes were reported to be associated with the clusters of genes responsible for the biosynthesis of cell wall-associated glycolipids like glycopeptidolipids (GPL), lipooligosaccharides, sulfolipids, polyacylated trehalose and other lipid derivatives like phthiocerol dimycocerosate (PDIM) (Converse et al. 2003; Pasca et al. 2005). These are pathogenetically and physiologically essential proteins of the Mtb (Domenech et al. 2005), but are less studied and there is scarce information available about their structure and functional mechanism.
The goal of this review is to discuss the role of MmpL proteins as potent drug targets in light of their contribution in the pathogenicity of mycobacterial species, drug resistance and the evolutionary context of these proteins in comparison to other members of the RND superfamily owing to their diverse and crucial transport functions, which helps the pathogen in adaptation according to the varying stressful environment presented by the host.
Role of MmpL proteins in pathogenicity
RND efflux pumps have been reported to be associated with the export of virulence factors (Piddock 2006). MexAB-OprM efflux pump was reported to enhance the virulence of P. aeruginosa. This pump was observed to facilitate expulsion of compound furanone C-30, which is a quorum sensing inhibitor and interacts with the LasR, a transcription regulator protein from quorum sensing-related las operon and thus attenuates the virulence of this pathogen (Beceiro et al. 2013). RND proteins in Erwinia chrysanthemi 3937 were reported to be essential for the virulence of the pathogen, as encoding gene knockout mutants of this bacteria were observed to be less virulent and more susceptible toward the toxic substances. The efflux of plant antimicrobial peptide thionin was also observed to be carried out by two Acr transporter systems (Valecillos et al. 2006). Mycobacterial RND proteins, MmpL, are generally designated to be related to lipid transport and with the reported drug efflux of several anti-TB drugs (Camacho et al. 1999; Bailo et al. 2015). Some of the mmpL genes were also reported to be essential for Mtb virulence in mice when analyzed by insertional mutation analysis (Domenech et al. 2005). The role of MmpL proteins in the pathogenicity of Mtb has been summarized in the following subsections.
MmpL proteins involved in the export of virulent molecules
The cell wall-associated and surface-exposed polyketides have been reported to play an important role in Mtb pathogenesis. These lipids provide a first barrier from the attack of the host immune system, and the genes related to the biosynthesis and export of these lipids are also indispensable for the survival and virulence of the bacteria (Camacho et al. 1999; Domenech et al. 2005). These surface-exposed lipids are synthesized in the cytoplasm and then transferred to the outer leaflet of the cell wall by some unknown mechanism and then aid in the interaction between the host and the microbial pathogen (Goren et al. 1974; Brennan and Nikaido 1995). The transport of these molecules is mediated by several membrane transporters. However, very little information is available on the transport of polyketides, but MmpL proteins were reported to be associated with the transport of these compounds. MmpL7 along with the DrrC proteins were reported to be essential for the transport of PDIM, a polyketide compound reported to be important for the pathogenicity of Mtb (Cox et al. 1999) (Fig. 3). MmpL7 was also observed to interact with biosynthetic enzyme PpsE in vivo and this activity was found to be essential for PDIM biosynthesis (Fig. 3) (Jain and Cox 2005). Further, MmpL8 has been also reported to aid sulfolipid-1 (SL-1) biosynthesis by transporting SL-1 precursor SL1278 across the membrane (Converse et al. 2003; Jain and Cox 2005) (Fig. 3). These types of coupling of synthesis and transport as shown by MmpL7 and MmpL8 with the respective lipid biosynthesis-associated proteins may be favorable for providing specificity and directionality in lipid transport processes (Jain and Cox 2005). MmpL proteins were reported to be responsible for the pleiotropic actions of mycobacteria. The effect was unveiled using the missense mutation in one of the essential tyrosine residue Tyr842 related to GPL transport and is common in all of the MmpL proteins. Replacement of this tyrosine with histidine residue in MmpL4a and with phenylalanine in MmpL3 leads to impairment of smooth-to-rough bacterial transition in M. bolletii and Mtb, respectively, as well as reduced virulence. The Tyr842 residue was also observed to be critical for proton influx in pairing with Asp841 in MmpL4a (Bernut et al. 2016; Szekely and Cole 2016).
MmpL proteins involved in the transport of drugs and lipid derivatives across the cell membrane: MmpL3 protein is reported to be involved in the import of heme and export of TMM (Tullius et al. 2011; Grzegorzewicz et al. 2012); MmpL4 protein is reported to be responsible for the efflux of MBT and GPL (Wells et al. 2013); MmpL5 protein is reported to carry out efflux of MBT, cMBT and econazole (Milano et al. 2009; Wells et al. 2013); MmpL7 protein is reported to cause efflux of PDIM and INH (Jain and Cox 2005; Pasca et al. 2005); MmpL8 protein is reported to be responsible for the efflux of SL-1; and MmpL11 protein is reported to be responsible for the import of heme and efflux of mycolate wax ester (Tullius et al. 2011; Pacheco et al. 2013)
mmpL genes are essential for the viability of the pathogen inside the host cell
MmpL proteins have been reported to be essential for the viability of bacterial pathogen inside the mice lung (Lamichhane et al. 2005; Wells et al. 2013). The results were derived from the mmpL mutant strains in which the mmpL genes were replaced by hygromycin-resistant cassette (Domenech et al. 2005). From the survival time analysis of Mtb-infected mice, it was observed that mmpL4 and mmpL7 mutants of Mtb were impaired in growth after 49 days and infected mice survived after 490 days of infection, whereas those infected with the wild-type strain of Mtb H37Rv did not survive. Further, mmpL8 and mmpL11 knockout mutants-infected mice showed considerably longer survival period than the wild-type with Mtb infection (Domenech et al. 2005). Furthermore, results from a separate study suggested that MmpL5 and MmpL10 proteins are required for Mtb survival in mouse lungs. However, the requirement of mmpL genes for the viability of Mtb in two different organs was observed to be not identical, as the mmpL7 gene was reported to be essential for growth in mouse lungs, but was not required for the survival of the pathogen in spleen or in the liver (Lamichhane et al. 2005). These reports indicate the essentiality and important role of mmpL genes in the survival of Mtb pathogen inside the host.
Molecular evolution of mmpL genes across the mycobacterial genomes
Evolution is an important mechanism in all living organisms to adapt themselves to the changing surrounding environment. The emergence of the antibiotic era has come with novel and advanced therapies against various infectious agents, which in turn has resulted in the evolution of drug-resistant strains of the bacterial pathogens as an adaptation strategy to survive inside the host. This has led to the failure of current antibiotic strategies and thus leaving many bacterial infections untreatable (Nikaido 2009). From the available data on various drug transporter protein structures, the phenomenon of conserved structural architecture and inverted repeat topology or duplication were deduced (Crisman et al. 2009; Khafizov et al. 2010). All these events describe the evolution of membrane transporters with time (Keller et al. 2014). MmpL transporters exist in varying numbers in different mycobacterial species. These proteins were also observed to exhibit patterns of internal gene duplication and pseudogenization as analyzed from their sequence analysis (Sandhu and Akhter 2015). These evolutionary events in mmpL genes have been discussed in detail in the next subsections.
Distribution of mmpL genes in pathogenic and non-pathogenic species
MmpL proteins have been reported to be in abundance in rapid growing mycobacteria than slow growing mycobacterial species (Viljoen et al. 2017). The comparison of mmpL genes across the different pathogenic and non-pathogenic strains of mycobacteria shows that their distribution varies among the pathogenic strains ranging from the highest number in M. bovis to the lowest in the case of M. leprae (Table 1). In the case of non-pathogenic Mycobacterium smegmatis (M. smegmatis), the number of mmpL genes is limited to only three (Table 1), which is fewer as compared to its homologs in pathogenic mycobacteria. However, the number of mmpL genes is also fewer exceptionally in M. leprae, which is highly pathogenic in nature but possesses a special status among mycobacterial pathogens. It has followed a reductive type of evolution and shredded off most of its non-essential genes not required for its metabolism inside host cell, leading to the smallest genome size among the mycobacterial species (Akhter et al. 2008). mmpL5, which has been reported as a siderophore exporter in Mtb, is absent in M. leprae (Wells et al. 2013; Sandhu and Akhter 2017). The possible reason behind the absence of this gene is the lack of complete siderophore anabolism pathway in the M. leprae (Cole et al. 2001), which might have also led to the deletion of siderophore export-related genes from the bacteria. Mtb clinical strain CDC1551, on the other hand, has an additional mmpL gene named mmpL14 (MT1802), absent in Mtb H37Rv. This mmpL14 gene was found to be confined to the deleted segment RvD2 of M. tuberculosis H37Rv (Gordon et al. 1999).
Duplication and pseudogenization events in mmpL transporter genes with global genome evolution
Internal gene duplication brings the versatility in genes by assigning them novel functions or by enhancing their already established functions (Chen et al. 2007). The internal gene duplication and fusion events lead to the evolution of internal symmetries in α-helical TMHs containing transporter proteins, needed for conformational changes to occur during performance of their attributed function (Hennerdal et al. 2010). The internal gene duplication event is common during molecular evolution and may be detected and analyzed by internal homology in the sequences. MmpL proteins have also been shown to be evolved by the events of internal duplication, resulting in a double number of TM helices than the primordial helices. However, the internal duplication patterns was mostly observed in MmpL proteins with a number of TM helices ranging from 10 to 12 (Sandhu and Akhter 2016). The duplicated forms may also result due to a fusion event as reported in other bacteria for the SecDF protein with 12 TM helices from Brucella and Staphylococcus aureus which was found to be evolved from the fusion of independent gene units secD and secF (Hennerdal et al. 2010).
The comparison of MmpL family members among the mycobacterial species from the Mtb complex and the non-pathogenic species M. smegmatis clearly indicates that the numbers of mmpL genes are more in the case of highly pathogenic species (Table 1). It was also observed that some MmpL proteins encoding genes like mmpL13a and mmpL13b are present in Mtb, and M. leprae genomes seem to undergo gene splitting event as part of continued pseudogenization, while the gene is intact and expresses a single protein product MmpL13 in the case of ancestral strains of Mtb complex such as M. bovis (Sandhu and Akhter 2015). These gene splitting events result in interrupted coding sequences (ICDSs) which may break or shift the reading frame and result in shorter ORFs with changed function or loss of function in the overall context of genome pseudogenization. This is similar to the case with the mmpL13 gene. This member from MmpL family has two functional units, mmpL13a and mmpL13b in Mtb, and two similar units in M. leprae with lost functionality due to the absence of the start codon from the ORFs. The splitting of the gene resulted in the loss of internal symmetry required for the trimer generation and transport function. In addition to mmpL13, mmpL9 in M. bovis was also reported to be an example of ICDS. The analysis of ICDSs and the corresponding promoter regions indicated that loss of function in ICDSs is not the result of mutations in the promoter regions, but is brought about by additional secondary mutations within these ICDSs following splitting events, which finally led to the loss of function of particular genes (Deshayes et al. 2008). These reported events indicate the evolution of mmpL genes among the different strains of mycobacteria, depending on their metabolic requirements and physiological conditions inside the host.
Transport functions of MmpL proteins
Mycobacterial cells have a lipid-rich coat of mycolic acid. Mycolic acid derivatives are synthesized in the cytoplasm and then transferred to the cell exterior via the cell membrane and periplasm. In mycobacteria, many proteins have dedicated roles for the lipid biosynthesis and its transport. Drug efflux pumps of the MmpL family of proteins have been also reported to have major roles in the export of mycolic acid derivatives (Table 2) (Pacheco et al. 2013). We have summarized the reported multi-substrate transport functions of MmpL proteins in the next subsections.
MmpL proteins in the transport of mycolic acid derivatives
For MmpL proteins, there are many documented evidences which suggest their role in the biosynthesis and transport of cell wall lipid constituents. Diversification in the biofilm formation was also observed for mmpL11 mutants of M. smegmatis as compared to the wild-type strains of M. smegmatis and similar results were also observed in Mtb bacteria (Pacheco et al. 2013; Wright et al. 2017). These variations in the lipid constituent of biofilm were reported due to impairment of their extracellular export of the mycolic acid-containing lipids, mycolate ester wax as evident from the cell wall lipidomics results and intracellular accumulation of mycolylphospholipid (MycPL) which is a precursor of mycolic acid (Pacheco et al. 2013) (Fig. 3). mmpL4a (tmtpB), mmpL4b (tmtpC) and mmpS4 mutants of M. smegmatis were also observed to lack GPL in their biofilm lipid constituent, resulting in the reduction in the sliding motility of the bacteria (Recht et al. 2000; Deshayes et al. 2010). MmpL3 protein from Mtb has been also reported to be involved in the transport of TMM across the cell membrane. This was evident from the inhibitory action of a urea derivative, AU1235 [1-(2-adamantyl)-3-(2,3,4-trifluorophenyl)urea], against MDR-Mtb, M. bovis BCG, M. smegmatis and Mycobacterium fortuitum, which is generally inactive against Gram-negative and Gram-positive bacteria. This compound has been shown to disturb the distribution of trehalose monomycolate (TMM) owing to the inhibition of the MmpL3 protein (Grzegorzewicz et al. 2012) (Fig. 3). MmpL3 has been reported to transport mycolic acids across the cell membrane by its flippase action (Xu et al. 2017). MmpL10 has been recently reported to export acylated trehalose to the cell surface in association with unknown periplasmic and outer membrane proteins from Mtb (Belardinelli et al. 2014). All these reports indicate the essential role of MmpL proteins in the transport of mycolic acid derivatives present in the cell envelope (Table 2).
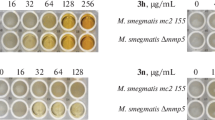
Contribution of MmpL proteins in mycobacterial drug resistance
Whole genome sequencing of mycobacterial strains revealed that they encode several putative drug efflux proteins (Cole et al. 1998), only a few of which have been characterized yet. There has been compelling evidence suggesting that these active efflux systems extrude drugs in mycobacteria (Table 2) (Louw et al. 2009). Some of these efflux pumps are specialized only for antibiotics, while others extrude diverse compounds which are structurally and functionally related and are involved in the housekeeping metabolism of the bacteria (Lomovskaya et al. 2001; Marquez 2005). The MmpL7 protein was reported to efflux INH in M. smegmatis (Fig. 3) after the intracellular accumulation of drug was observed to reach up to a threshold value (Pasca et al. 2005). Azole-resistant mutant strains of Mtb and M. bovis BCG were reported to exhibit increased efflux of econazole (Fig. 3) along with the higher transcription rate of mmpL5 and mmpS5 genes (Milano et al. 2009). Clofazimine-resistant Mtb strains with the mutation in Rv0678 protein were reported to have enhanced expression of mmpL5 efflux pump encoding genes with additional resistance to novel antituberculosis drug bedaquiline (Hartkoorn et al. 2014). The resistance of M. abscessus strains to thiacetazone (TAC) derivatives was also reported due to overexpression of mmpL5/mmpS5 efflux apparatus, due to mutations in a TetR repressor protein MAB_4384 indicating the role of MmpL5/MmpS5 assembly in the efflux of TAC derivatives D6, D15 and D17 (Halloum et al. 2017). MmpL5 protein from Mtb was also reported to capture linezolid and pyrazinamide drugs from the cytoplasm and release them in the periplasm as observed from protein–ligand binding and MD simulation analysis. This has further strengthened the putative role of MmpL5 in the transport and efflux of anti-TB drugs across the cell membrane and thereby indicating its contribution to the evolution of drug resistance (Sandhu and Akhter 2016; Briffotaux et al. 2017).
Evolution of structural fitness in RND transporters of Mtb
RND multidrug efflux pumps are common among the pathogenic bacteria. They provide a second-line barrier against the antibiotics. They consist of a tripartite assembly across the bacterial cell envelope with an inner membrane spanning transporter protein, a periplasmic adaptor protein and an outer membrane efflux protein (Daury et al. 2016). All three components help to extrude the substrate directly to the extracellular environment through the water-filled channel created by the three-component assembly of RND efflux pumps (Nikaido 2011). However, none of the full-length MmpL proteins has been characterized yet, while the prediction of their secondary structure topologies and homology-modeled tertiary structures offered their comparative analysis with well-studied RND pumps (Sandhu and Akhter 2015). Structural evolution leading to their specialized function in MmpL proteins has been summarized in the following subsections.
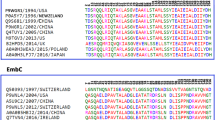
Unusual periplasmic topology facilitating diverse transport functions
Periplasmic porter sub-domains PN1 and PN2 of AcrB efflux pump from E. coli were reported to interact with the periplasmic accessory protein AcrA, and docking sub-domains, DC and DN were reported to interact with the outer membrane efflux protein TolC (Symmons et al. 2009). In the MmpL protein family from Mtb, none of the members posses DN sub-domain as observed from their topological representations (Chim et al. 2015). According to the phylogenetic classification of these proteins, ten proteins of this family, MmpL1, MmpL2, MmpL4-MmpL10 and MmpL12, constitute cluster-1 with single PN1 sub-domain and two PC1 and PC2 sub-domains along with an additional D3 sub-domain extended in the cytoplasm. This shows that cluster-I proteins have structural similarity to the well-known RND proteins at the C-terminal, but they differ structurally at the N-terminal due to the absence of the PN2 sub-domain (Chalut 2016). Cluster-II constitutes the MmpL3, MmpL11 and MmpL13 proteins. These proteins possess more structural variation and unique periplasmic topology, as they lack both of the docking sub-domains, DC and DN, at the C- and N-terminal, respectively (Chim et al. 2015). In recent studies using cryo-electron microscopy on the MmpL3 protein of Mtb and its orthologous protein CmpL1 from Corynebacterium, the PN porter domain was reported to interact with the adjacent monomer units to form an oligomer, while in other RND proteins like AcrB, the PN1 sub-domain was observed to be responsible for the interaction with periplasmic efflux proteins and form the periplasmic pore region (Belardinelli et al. 2016). Unusual topologies of these proteins due to partial loss of porter and docking sub-domains containing part of the protein, constituted by the additional periplasmic loop regions, may be an indication of their evolutionary adaptation.
The shortening of the loop regions may increase the overall thermodynamic stability of the proteins by reducing the energy required for the folding process and making them relatively more stable at higher ambient temperatures. These kinds of adaptations are more beneficial for the Mtb, an intracellular pathogen parasite of warm-blooded hosts like humans (Sandhu and Akhter 2015). This kind of unique periplasmic topology may also facilitate accommodation of the diverse interacting partners other than the usual periplasmic counterparts of the RND proteins (Wells et al. 2013).
Therapeutic interventions against the RND efflux pumps
Efflux pumps have been reported to play a major role in drug-resistance mechanisms of bacteria. Many studies have been carried out in recent years to control the multidrug resistance in bacteria by targeting efflux pumps (Askoura et al. 2011; Opperman and Nguyen 2015). One of such pyranopyridine-based efflux pump inhibitor was reported to bind with the soluble periplasmic part of the AcrB efflux pump from the RND superfamily from E. coli with high potency and thereby compete with the actual substrates of the protein (Sjuts et al. 2016). The therapeutic inventions against the MmpL proteins in terms of small molecule inhibitors have been already reviewed recently (Rayasam 2014; Bailo et al. 2015; Poce et al. 2016). In the last few years, some of the inhibitors have been found to block the activity of the MmpL3 protein (Fig. 4). MmpL3 has been reported to play an essential role in viability and normal growth of Mtb. Its conditional deletion has shown an adverse effect on the cell wall biosynthesis and cell replication, which established it as a crucial drug target (Degiacomi et al. 2017). It was reported that the MmpL3 protein could be inhibited by an ethambutol derivative SQ109. This compound is a broad-range antituberculosis agent. SQ109-treated Mtb showed increased intracellular concentrations of TMM and altered cell wall generation due to unavailability of this mycolic acid component, which resulted due to disrupted MmpL3 function (Tahlan et al. 2012). Adamantyl urea inhibitor AU1235 was also observed to inhibit MmpL3 activity resulting in the intracellular accumulation of the TMM. AU1235-resistant Mtb mutants were found to posses G253E mutation in a TM helix (Grzegorzewicz et al. 2012). MmpL3 efflux activity was also reported to be inhibited by indolcarboxamide (Rao et al. 2013), BM212 (La Rosa et al. 2012), benzimidazole (Stanley et al. 2012), tetrahydropyrazolo pyrimidine (THPP) and spiro analogs (Remuiñán et al. 2013) (Fig. 4). Many compounds out of these known inhibitors like BM212, SQ109 and the THPPs disrupt the electrochemical gradient and may be effective against the other MmpL protein targets (Bailo et al. 2015). PIPD1, a derivative of piperidinol, was shown to inhibit the MmpL3 efflux activity (Fig. 4), thereby affecting mycolic acid transport in Mycobacterium abscessus, whereas the PIPD1-resistant strains of the bacterium were reported to have a mutated MmpL3 encoding gene MAB_4508 (Dupont et al. 2016). The inhibitors have been designed against the MmpL3 protein only; however, MmpL5 and MmpL11 proteins have also been reported to be involved in the crucial physiological processes. Thus, these kinds of studies should be extended to other important MmpL proteins.
Inhibitors for MmpL3 efflux protein of mycobacterial pathogenic strains: showing different inhibitor compounds reported to be effective against the MmpL3 protein from Mtb and M. abscessus. These compounds have been found to inhibit the trehalose monomycolate transport and disrupt the proton-motive force, thereby disrupting the normal efflux activity of the protein
Concluding remarks and future directions
Membrane proteins have a crucial role in fulfilling the physiological requirements of the cells. Their types and functions differ according to the physiology and habitat of the organism. The MmpL protein family is one of such viably essential group of RND transporters in Mtb. Their role in lipid transport and drug efflux has been established by intracellular accumulation of some known drug candidates in mmpL gene knockout mutants (Table 2). They also have been reported to carry out essential roles in the virulence of mycobacteria. All these functions suggest their contribution in the overall pathogenesis of the Mtb. However, only a few in vitro studies have been performed to ascertain the biochemical functional mechanism of MmpL proteins. No full-length structures of these proteins have been determined till date.
MmpL proteins are involved in various important physiological processes such as the export of virulence factors, iron acquisition, and export of cell wall lipid derivatives, which are crucial for the survival of the bacterium. To target Mtb, these processes may be selectively blocked. In this way, MmpL proteins may serve as novel drug discovery hot spots for the inhibitor designing against the Mtb (Fig. 5). In recent years, inhibitors against the MmpL3 has been identified also affecting the viability of the Mtb bacteria and in some cases reducing the extent of resistance to particular drugs. However, many new findings have come across in recent years for this family of proteins in Mtb, but only a few members have been explored in terms of their function and essentiality. The family constitutes 14 members in total, but the major focus has been upon MmpL3, MmpL4, MmpL5, MmpL7, MmpL8 and MmpL11. Eight members still need to be explored more to prove their worth as drug targets. There are still several questions remaining to be answered about the regulation of MmpL transporters gene expression in Mtb. It was reported that sigma factor, SigF, regulates the differential expression of 14 mmpL genes (Williams et al. 2007). Although the regulatory regions of mmpL genes have been reported to contain binding sites for many transcription regulators, there are only a few experimentally characterized transcription factors reported so far. Two of the transcription factors, Rv3249c and Rv1816, were recently reported to regulate their gene expressions (Delmar et al. 2015). It was documented that PknD, a serine/threonine protein kinase, is involved in the phosphorylation of the MmpL7 protein. This may have regulatory roles in its transport function (Perez et al. 2006). Post-translational modifications are also reported to regulate the transport functions of ABC multidrug transporters. However for RND proteins, there are not many reports available about such regulatory modifications; therefore, future studies should be focussed on this aspect of research (Perego et al. 2010; Stolarczyk et al. 2011). Some of the MmpL proteins like MmpL3 and MmpL5 have been shown to perform multiple functions simultaneously (Table 2) (Sandhu and Akhter 2016, 2017), but we need more of such future studies to discover further the novel pleiotropic functions of other members of this family of transporters in Mtb physiology.
Three crucial transport processes carried out by MmpL proteins could be targeted against Mtb: MmpL proteins have been reported to be involved in iron acquisition from the host cells, efflux of mycolic acid (lipid) derivatives and drug efflux across the cell membrane. These processes are important for the viability and survival of the bacteria and could be inhibited to subjugate the Mtb bacteria. The quaternary structure of MmpL5 protein modeled on template protein CusA (PDB ID: 3K07) from E. coli is shown (Kelley et al. 2015)
Nowadays RND efflux pumps have been established as one of the major contributing causes of drug resistance in bacteria and much experimentations are going on to inhibit their function, but none of the RND efflux pump inhibitors has been successfully tested clinically till date. The main reason behind this is very less structural and functional information available about RND proteins required for designing inhibitors. This may be due to the large failure rates of in vitro techniques for isolation and purification of integral membrane proteins. Isolation and purification of membrane proteins involve treatment of cells with harsh chemicals to dissolve the lipid bilayer components, which may sometimes lead to the mixing of cellular constituents. This becomes more difficult, especially in the case of mycobacteria where the cell envelope has lipid content much more than other Gram-positive and Gram-negative bacteria. This may be the major reason behind only a few well-characterized membrane proteins known to researchers out of the total mycobacterial proteome. However, there have been landmark advancements in the field of recombinant expression and purification, making it easy to obtain a target protein at a larger scale and expression of a large pool of genes in surrogate homologous hosts to analyze their function at genome levels. For instance, M. smegmatis has been recently used as an optimum surrogate heterologous host for efficiently expressing and analyzing the physiological functions of Mtb proteins (Singhal et al. 2015). Heterologous expression of integral membrane proteins is still difficult because when they are expressed in the heterologous host they have been shown to be toxic to the host cells, expressed in very low quantities or acquire insoluble misfolded or unfolded structural conformations due to the presence of hydrophobic helices, which may remain biochemically inactive (Bernaudat et al. 2011).
Hence, much more information is required about this important family of proteins, which are emerging as a battery of novel drug targets. This may help the community to devise therapeutic intervention against these strains also, which may ultimately help to overcome the global TB burden.
Abbreviations
- Mtb :
-
Mycobacterium tuberculosis
- MmpL:
-
Mycobacterial membrane protein large
- RND:
-
Resistance nodulation division
- TMH:
-
Transmembrane helices
- MDR:
-
Multidrug resistant
References
Akhter Y, Yellaboina S, Farhana A, Ranjan A, Ahmed N, Hasnain SE (2008) Genome scale portrait of cAMP-receptor protein (CRP) regulons in mycobacteria points to their role in pathogenesis. Gene 407:148–158
Alexander PE, De P (2007) The emergence of extensively drug-resistant tuberculosis (TB): TB/HIV coinfection, multidrug-resistant TB and the resulting public health threat from extensively drug-resistant TB, globally and in Canada. Can J Infect Dis Med Microbiol 18:289–291
Askoura M, Mottawea W, Abujamel T, Taher I (2011) Efflux pump inhibitors (EPIs) as new antimicrobial agents against Pseudomonas aeruginosa. Libyan J Med 6:5870
Bailo R, Bhatt A, Aínsa JA (2015) Lipid transport in Mycobacterium tuberculosis and its implications in virulence and drug development. Biochem Pharmacol 96:159–167
Beceiro A, Tomás M, Bou G (2013) Antimicrobial resistance and virulence: a successful or deleterious association in the bacterial world? Clin Microbiol Rev 26:185–230
Belardinelli JM, Larrouy-Maumus G, Jones V, de Carvalho LPS, McNeil MR, Jackson M (2014) Biosynthesis and translocation of unsulfated acyltrehaloses in Mycobacterium tuberculosis. J Biol Chem 289:27952–27965
Belardinelli JM et al (2016) Structure-function profile of MmpL3, the essential mycolic acid transporter from Mycobacterium tuberculosis. ACS Infect Dis 2(10):702–713
Bernaudat F et al (2011) Heterologous expression of membrane proteins: choosing the appropriate host. PLoS One 6:e29191
Bernut A et al (2016) Insights into the smooth-to-rough transitioning in Mycobacterium bolletii unravels a functional Tyr residue conserved in all mycobacterial MmpL family members. Mol Microbiol 99:866–883. doi:10.1111/mmi.13283
Brennan PJ, Nikaido H (1995) The envelope of mycobacteria. Annu Rev Biochem 64:29–63
Briffotaux J, Huang W, Wang X, Gicquel B (2017) MmpS5/MmpL5 as an efflux pump in Mycobacterium species. Tuberculosis 107:13–19. doi:10.1016/j.tube.2017.08.001
Camacho LR, Ensergueix D, Perez E, Gicquel B, Guilhot C (1999) Identification of a virulence gene cluster of Mycobacterium tuberculosis by signature-tagged transposon mutagenesis. Mol Microbiol 34:257–267
Calgin MK, Sahin F, Turegun B, Gerceker D, Atasever M, Koksal D, Karasartova D, Kiyan M (2013) Expression analysis of efflux pump genes among drug-susceptible and multidrug-resistant Mycobacterium tuberculosis clinical isolates and reference strains. Diagn Microbiol Infect Dis 76(3):291–297
Chalut C (2016) MmpL transporter-mediated export of cell-wall associated lipids and siderophores in mycobacteria. Tuberculosis 100:32–45
Chen C-C, Li W-H, Sung H-M (2007) Patterns of internal gene duplication in the course of metazoan evolution. Gene 396:59–65
Chim N et al (2015) The structure and interactions of periplasmic domains of crucial MmpL membrane proteins from Mycobacterium tuberculosis. Chem Biol 22:1098–1107
Cole S et al (1998) Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature 393:537–544
Cole S et al (2001) Massive gene decay in the leprosy bacillus. Nature 409:1007–1011
Converse SE, Mougous JD, Leavell MD, Leary JA, Bertozzi CR, Cox JS (2003) MmpL8 is required for sulfolipid-1 biosynthesis and Mycobacterium tuberculosis virulence. Proc Natl Acad Sci USA 100:6121–6126
Cox JS, Chen B, McNeil M, Jacobs WR (1999) Complex lipid determines tissue-specific replication of Mycobacterium tuberculosis in mice. Nature 402:79–83
Crisman TJ, Qu S, Kanner BI, Forrest LR (2009) Inward-facing conformation of glutamate transporters as revealed by their inverted-topology structural repeats. Proc Natl Acad Sci USA 106:20752–20757
Daury L et al (2016) Tripartite assembly of RND multidrug efflux pumps. Nat Commun 7:10731
Degiacomi G et al (2017) Essentiality of mmpL3 and impact of its silencing on Mycobacterium tuberculosis gene expression. Sci Rep 7:43495
Delmar JA et al (2015) Structural basis for the regulation of the MmpL transporters of Mycobacterium tuberculosis. J Biol Chem 290:28559–28574. doi:10.1074/jbc.M115.683797
Deshayes C et al (2008) Detecting the molecular scars of evolution in the Mycobacterium tuberculosis complex by analyzing interrupted coding sequences. BMC Evol Biol 8:1
Deshayes C et al (2010) MmpS4 promotes glycopeptidolipids biosynthesis and export in Mycobacterium smegmatis. Mol Microbiol 78:989–1003
Domenech P, Reed MB, Barry CE (2005) Contribution of the Mycobacterium tuberculosis MmpL protein family to virulence and drug resistance. Infect Immun 73:3492–3501
Dupont C et al (2016) A new piperidinol derivative targeting mycolic acid transport in Mycobacterium abscessus. Mol Microbiol 101:515–529
Forrellad MA et al (2013) Virulence factors of the Mycobacterium tuberculosis complex. Virulence 4:3–66
Frieden TR, Sterling T, Pablos-Mendez A, Kilburn JO, Cauthen GM, Dooley SW (1993) The emergence of drug-resistant tuberculosis in New York City. N Engl J Med 328:521–526
Gordon SV, Brosch R, Billault A, Garnier T, Eiglmeier K, Cole ST (1999) Identification of variable regions in the genomes of tubercle bacilli using bacterial artificial chromosome arrays. Mol Microbiol 32:643–655
Goren MB, Brokl O, Schaefer WB (1974) Lipids of putative relevance to virulence in Mycobacterium tuberculosis: phthiocerol dimycocerosate and the attenuation indicator lipid. Infect Immun 9:150–158
Grzegorzewicz AE et al (2012) Inhibition of mycolic acid transport across the Mycobacterium tuberculosis plasma membrane. Nat Chem Biol 8:334–341
Guglierame P et al (2006) Efflux pump genes of the resistance-nodulation-division family in Burkholderia cenocepacia genome. BMC Microbiol 6:66
Halloum I et al (2017) Resistance to thiacetazone derivatives active against Mycobacterium abscessus involves mutations in the MmpL5 transcriptional repressor MAB_4384. Antimicrob Agents Chemother 61:e02509–e02516
Hartkoorn RC, Uplekar S, Cole ST (2014) Cross-resistance between clofazimine and bedaquiline through upregulation of MmpL5 in Mycobacterium tuberculosis. Antimicrob Agents Chemother 58:2979–2981
Helms M, Vastrup P, Gerner-Smidt P, Mølbak K (2002) Excess mortality associated with antimicrobial drug-resistant Salmonella typhimurium. Emerg Infect Dis 8:490–495
Hennerdal A, Falk J, Lindahl E, Elofsson A (2010) Internal duplications in α-helical membrane protein topologies are common but the nonduplicated forms are rare. Protein Sci 19:2305–2318
Jain M, Cox JS (2005) Interaction between polyketide synthase and transporter suggests coupled synthesis and export of virulence lipid in M. tuberculosis. PLoS Pathog 1:e2
Keller R, Ziegler C, Schneider D (2014) When two turn into one: evolution of membrane transporters from half modules. Biol Chem 395:1379–1388
Kelley LA, Mezulis S, Yates CM, Wass MN, Sternberg MJ (2015) The Phyre2 web portal for protein modeling, prediction and analysis. Nat Protoc 10:845–858
Khafizov K, Staritzbichler R, Stamm M, Forrest LR (2010) A study of the evolution of inverted-topology repeats from LeuT-fold transporters using AlignMe. Biochemistry 49:10702–10713
La Rosa V et al (2012) MmpL3 is the cellular target of the antitubercular pyrrole derivative BM212. Antimicrob Agents Chemother 56:324–331
Lamichhane G, Tyagi S, Bishai WR (2005) Designer arrays for defined mutant analysis to detect genes essential for survival of Mycobacterium tuberculosis in mouse lungs. Infect Immun 73:2533–2540
Lange Y, Steck TL (1998) Four cholesterol-sensing proteins. Curr Opin Struct Biol 8:435–439
Lomovskaya O et al (2001) Identification and characterization of inhibitors of multidrug resistance efflux pumps in Pseudomonas aeruginosa: novel agents for combination therapy. Antimicrob Agents Chemother 45:105–116
Louw G, Warren R, Van Pittius NG, McEvoy C, Van Helden P, Victor T (2009) A balancing act: efflux/influx in mycobacterial drug resistance. Antimicrob Agents Chemother 53:3181–3189
Marquez B (2005) Bacterial efflux systems and efflux pumps inhibitors. Biochimie 87:1137–1147
Marrakchi H, Lanéelle M-A, Daffé M (2014) Mycolic acids: structures, biosynthesis, and beyond. Chem Biol 21:67–85
Milano A et al (2009) Azole resistance in Mycobacterium tuberculosis is mediated by the MmpS5–MmpL5 efflux system. Tuberculosis 89:84–90
Moore RA, DeShazer D, Reckseidler S, Weissman A, Woods DE (1999) Efflux-mediated aminoglycoside and macrolide resistance in Burkholderia pseudomallei. Antimicrob Agents Chemother 43:465–470
Nikaido H (1998) Multiple antibiotic resistance and efflux. Curr Opin Microbiol 1:516–523
Nikaido H (2009) Multidrug resistance in bacteria. Annu Rev Biochem 78:119
Nikaido H (2011) Structure and mechanism of RND-type multidrug efflux pumps. Adv Enzymol Relat Areas Mol Biol 77:1
Opperman TJ, Nguyen ST (2015) Recent advances toward a molecular mechanism of efflux pump inhibition. Front Microbiol 6:421
Pacheco SA, Hsu F-F, Powers KM, Purdy GE (2013) MmpL11 protein transports mycolic acid-containing lipids to the mycobacterial cell wall and contributes to biofilm formation in Mycobacterium smegmatis. J Biol Chem 288:24213–24222
Parida S et al (2015) Totally drug-resistant tuberculosis and adjunct therapies. J Intern Med 277:388–405
Pasca M, Guglierame P, Rossi ED, Zara F, Riccardi G (2005) MmpL7 gene of Mycobacterium tuberculosis is responsible for isoniazid efflux in mycobacterium smegmatis. Antimicrob Agents Chemother 49:4775–4777
Paulsen IT, Brown MH, Skurray RA (1996) Proton-dependent multidrug efflux systems. Microbiol Rev 60:575–608
Perego P, Gatti L, Beretta GL (2010) The ABC of glycosylation. Nat Rev Cancer 10:523
Perez J et al (2006) Mycobacterium tuberculosis transporter MmpL7 is a potential substrate for kinase PknD. Biochem Biophys Res Commun 348:6–12. doi:10.1016/j.bbrc.2006.06.164
Piddock LJ (2006) Clinically relevant chromosomally encoded multidrug resistance efflux pumps in bacteria. Clin Microbiol Rev 19:382–402
Poce G, Consalvi S, Biava M (2016) MmpL3 inhibitors: diverse chemical scaffolds inhibit the same target. Mini Rev Med Chem 16:1274–1283
Rao SP et al (2013) Indolcarboxamide is a preclinical candidate for treating multidrug-resistant tuberculosis. Sci Transl Med 5:214ra168
Rayasam GV (2014) MmpL3 a potential new target for development of novel anti-tuberculosis drugs. Expert Opin Ther Targets 18:247–256
Recht J, Martínez A, Torello S, Kolter R (2000) Genetic analysis of sliding motility in Mycobacterium smegmatis. J Bacteriol 182:4348–4351
Remuiñán MJ et al (2013) Tetrahydropyrazolo [1,5-a] pyrimidine-3-carboxamide and N-benzyl-6′,7′-dihydrospiro[piperidine-4,4′-thieno [3,2-c]pyran] analogues with bactericidal efficacy against Mycobacterium tuberculosis targeting MmpL3. PLoS One 8:e60933
Saier M, Tam R, Reizer A, Reizer J (1994) Two novel families of bacterial membrane proteins concerned with nodulation, cell division and transport. Mol Microbiol 11:841–847
Sandhu P, Akhter Y (2015) The internal gene duplication and interrupted coding sequences in the MmpL genes of Mycobacterium tuberculosis: towards understanding the multidrug transport in an evolutionary perspective. Int J Med Microbiol 305:413–423
Sandhu P, Akhter Y (2016) The drug binding sites and transport mechanism of the RND pumps from Mycobacterium tuberculosis: Insights from molecular dynamics simulations. Arch Biochem Biophys 592:38–49
Sandhu P, Akhter Y (2017) Siderophore transport by MmpL5–MmpS5 protein complex in Mycobacterium tuberculosis. J Inorg Biochem 170:75–84. doi:10.1016/j.jinorgbio.2017.02.013
Schweizer HP (2003) Efflux as a mechanism of resistance to antimicrobials in Pseudomonas aeruginosa and related bacteria: unanswered question. Genet Mol Res 2:48–62
Singhal A et al (2015) Systematic analysis of mycobacterial acylation reveals first example of acylation-mediated regulation of enzyme activity of a bacterial phosphatase. J Biol Chem 290:26218–26234. doi:10.1074/jbc.M115.687269
Sjuts H et al (2016) Molecular basis for inhibition of AcrB multidrug efflux pump by novel and powerful pyranopyridine derivatives. Proc Natl Acad Sci USA 113:3509–3514
Stanley SA et al (2012) Identification of novel inhibitors of M. tuberculosis growth using whole cell based high-throughput screening. ACS Chem Biol 7:1377–1384
Stolarczyk EI, Reiling CJ, Paumi CM (2011) Regulation of ABC transporter function via phosphorylation by protein kinases. Curr Pharm Biotechnol 12:621–635
Symmons MF, Bokma E, Koronakis E, Hughes C, Koronakis V (2009) The assembled structure of a complete tripartite bacterial multidrug efflux pump. Proc Natl Acad Sci USA 106:7173–7178. doi:10.1073/pnas.0900693106
Szekely R, Cole S (2016) Mechanistic insight into mycobacterial MmpL protein function. Mol Microbiol 99:831–834
Tahlan K et al (2012) SQ109 targets MmpL3, a membrane transporter of trehalose monomycolate involved in mycolic acid donation to the cell wall core of Mycobacterium tuberculosis. Antimicrob Agents Chemother 56:1797–1809
Tekaia F, Gordon S, Garnier T, Brosch R, Barrell B, Cole S (1999) Analysis of the proteome of Mycobacterium tuberculosis in silico. Tuber Lung Dis 79:329–342
Tullius MV et al (2011) Discovery and characterization of a unique mycobacterial heme acquisition system. Proc Natl Acad Sci USA 108:5051–5056
Valecillos AM, Palenzuela PR, López-Solanilla E (2006) The role of several multidrug resistance systems in Erwinia chrysanthemi pathogenesis. Mol Plant Microbe Interact 19:607–613
Varela C, Rittmann D, Singh A, Krumbach K, Bhatt K, Eggeling L, Besra GS, Bhatt A (2012) MmpL genes are associated with mycolic acid metabolism in mycobacteria and corynebacteria. Chem Biol 19(4):498–506
Velayati AA et al (2009) Emergence of new forms of totally drug-resistant tuberculosis bacilli: super extensively drug-resistant tuberculosis or totally drug-resistant strains in Iran. Chest J 136:420–425
Viljoen A, Dubois V, Girard-Misguich F, Blaise M, Herrmann JL, Kremer L (2017) The diverse family of MmpL transporters in mycobacteria: from regulation to antimicrobial developments. Mol Microbiol 104(6):889–904
Wells RM et al (2013) Discovery of a siderophore export system essential for virulence of Mycobacterium tuberculosis. PLoS Pathog 9:e1003120. doi:10.1371/journal.ppat.1003120
WHO (2014) Drug-resistant TB: surveillance and response: supplement to global tuberculosis report 2014. WHO, Geneva
WHO (2016) Global tuberculosis report 2015. World Health Organization, Geneva
Williams EP, Lee JH, Bishai WR, Colantuoni C, Karakousis PC (2007) Mycobacterium tuberculosis SigF regulates genes encoding cell wall-associated proteins and directly regulates the transcriptional regulatory gene phoY1. J Bacteriol 189:4234–4242. doi:10.1128/jb.00201-07
Wright CC, Hsu FF, Arnett E, Dunaj JL, Davidson PM, Pacheco SA, Harriff MJ, Lewinsohn DM, Schlesinger LS, Purdy GE (2017) The Mycobacterium tuberculosis MmpL11 cell wall lipid transporter is important for biofilm formation, intracellular growth, and nonreplicating persistence. Infect Immun 85(8). doi:10.1128/IAI.00131-17
Xu Z, Meshcheryakov VA, Poce G, Chng S-S (2017) MmpL3 is the flippase for mycolic acids in mycobacteria. Proc Natl Acad Sci USA 114(30):7993–7998
Acknowledgements
The Indian Council of Medical Research (ICMR) is acknowledged for providing financial support in the form of a stipend to PS. Research in the YA lab is supported by extramural research funds from the Science and Engineering Research Board (DST, SERB), ICMR and UGC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Additional information
Communicated by Michael Berney.
Rights and permissions
About this article
Cite this article
Sandhu, P., Akhter, Y. Evolution of structural fitness and multifunctional aspects of mycobacterial RND family transporters. Arch Microbiol 200, 19–31 (2018). https://doi.org/10.1007/s00203-017-1434-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00203-017-1434-6