Abstract
This narrative review considers the key challenges facing healthcare professionals and policymakers responsible for providing care to populations in relation to bone health. These challenges broadly fall into four distinct themes: (1) case finding and management of individuals at high risk of fracture, (2) public awareness of osteoporosis and fragility fractures, (3) reimbursement and health system policy and (4) epidemiology of fracture in the developing world. Findings from cohort studies, randomised controlled trials, systematic reviews and meta-analyses, in addition to current clinical guidelines, position papers and national and international audits, are summarised, with the intention of providing a prioritised approach to delivery of optimal bone health for all. Systematic approaches to case-finding individuals who are at high risk of sustaining fragility fractures are described. These include strategies and models of care intended to improve case finding for individuals who have sustained fragility fractures, those undergoing treatment with medicines which have an adverse effect on bone health and people who have diseases, whereby bone loss and, consequently, fragility fractures are a common comorbidity. Approaches to deliver primary fracture prevention in a clinically effective and cost-effective manner are also explored. Public awareness of osteoporosis is low worldwide. If older people are to be more pro-active in the management of their bone health, that needs to change. Effective disease awareness campaigns have been implemented in some countries but need to be undertaken in many more. A major need exists to improve awareness of the risk that osteoporosis poses to individuals who have initiated treatment, with the intention of improving adherence in the long term. A multisector effort is also required to support patients and their clinicians to have meaningful discussions concerning the risk-benefit ratio of osteoporosis treatment. With regard to prioritisation of fragility fracture prevention in national policy, there is much to be done. In the developing world, robust epidemiological estimates of fracture incidence are required to inform policy development. As the aging of the baby boomer generation is upon us, this review provides a comprehensive analysis of how bone health can be improved worldwide for all.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 2016, the first of the baby boomer generation entered their eighth decade of life. Consequently, the next 10 years will bear witness to a significant increase in the number of individuals living with osteoporosis and experiencing the morbidity consequent upon fragility fractures. Fragility fractures can be defined as fractures which result from a fall from a standing height or less or that present in the absence of trauma. The most common fragility fractures occur at the hip, wrist, spine, humerus or pelvis. As such, it is timely to take stock of the key challenges facing healthcare professionals and policymakers responsible for providing care for populations in relation to bone health and to identify solutions that will reduce fracture rates and ameliorate their personal and societal burden. These challenges broadly fall into four distinct themes:
-
1.
Case finding and management of individuals at high risk of fracture
-
2.
Public awareness of osteoporosis and fragility fractures
-
3.
Reimbursement and health system policy
-
4.
Epidemiology of fracture in the developing world
This narrative review explores each of these themes in terms of current gaps in delivery of best clinical practice, levels of public awareness, appropriateness of funding and policy arrangements and characterisation of the current and future burden of disease in the developing world. Most importantly, the work of innovators who have successfully addressed each challenge will be reviewed. Clinically effective and cost-effective models of care have been developed in many countries to case find and manage individuals who are at high risk of sustaining fragility fractures. Award-winning public awareness campaigns have been implemented which empower individuals who are living with osteoporosis to be pro-active in seeking medical advice to reduce their own fracture risk. A number of governments have identified osteoporosis as a national health priority and implemented comprehensive quality improvement programs across their national health systems. New epidemiological studies from Asia and Latin American have begun to quantify the impact of osteoporosis in the developing world. While there is much to be done, there is a reason for optimism. All of the challenges identified are solvable: now is the time for these solutions to be implemented throughout the world.
Case finding and management of individuals at high risk of fracture
During the last 25 years, a broad range of therapeutic options has become available to reduce an individual’s risk of fragility fracture [1]. These medicines are available as daily, weekly or monthly oral tablets or as daily, three-monthly or six-monthly injections or annual infusions, providing patients and physicians with a uniquely flexible array of dosing regimens. Getting the right treatment to the right patient at the right time is of paramount importance if fracture rates are to be significantly reduced as the world’s population ages. This section of the review focuses on strategies to ensure that individuals who are at high risk of sustaining fragility fractures, in general and hip fractures, in particular, are reliably identified by health systems and treated in accordance with the best practice guidance. Opportunities to systematise case finding in four scenarios will be considered.
-
1.
Secondary fracture prevention
-
2.
Primary fracture prevention
-
3.
Osteoporosis induced by medicines
-
4.
Diseases associated with osteoporosis
For each scenario, evidence relating to fracture risk in the population in question is considered. Current levels of case finding and appropriate osteoporosis management are reviewed. Where available, analysis of published work describing models of care to implement best practice is presented. Finally, selected examples of clinical guidelines and recommendations made therein are highlighted.
Secondary fracture prevention
Secondary fracture prevention is an obvious first step in the development of a systematic approach to prevention of all fragility fractures caused by osteoporosis. Since the 1980s, it has been known that up to one half of hip fracture patients have already sustained a previous fracture [2–5]. Meta-analyses have shown that individuals who have sustained a fracture are at approximately double the risk of sustaining subsequent fractures, as compared to their fracture-free peers [6, 7]. Accordingly, the notion that fracture begets fracture is well established in the literature and well represented in clinical guidelines for osteoporosis in many countries [8, 9]. Further, subsequent fractures appear to occur rapidly after an index fracture. In 2004, Johnell et al. examined the pattern of fracture risk following a prior fracture at the spine, shoulder or hip [10]. During 5 years of follow-up, one third of all subsequent fractures occurred within the first year after fracture, and less than 9% of all subsequent fractures occurred in the fifth year.
The effectiveness of the broad range of currently available osteoporosis treatments has been comprehensively reviewed elsewhere [1]. Cochrane Collaboration systematic reviews have evaluated alendronate [11], etidronate [12] and risedronate [13] specifically in the secondary fracture prevention context for treatment of postmenopausal women, and Cochrane protocols have been published for zoledronate [14] and denosumab [15]. The findings of the Cochrane reviews for the bisphosphonates which were statistically significant are summarised in Table 1. The methodology used for pooling of results from the individual trials included in the Cochrane reviews has been described elsewhere [16]. When the relative risk reduction (RRR) for a particular agent was significant (p < 0.05), the absolute risk reduction (ARR) and number needed to treat (NNT) were calculated. For these calculations, the Cochrane authors based the 5-year risk of fracture in the untreated population on the FRACTURE Index (FI) [17] and the lifetime and 5-year age-specific risks in the untreated population on the model by Doherty et al. for predicting osteoporotic fractures in postmenopausal women [18].
Other osteoporosis treatments have been evaluated for secondary fracture prevention in randomised controlled trials (RCTs) or sub-analyses of RCTs:
-
Zoledronate: The HORIZON Recurrent Fracture Trial (RFT) evaluated zoledronate in the treatment of individuals who had sustained a hip fracture [19]. Statistically significant reductions were observed for any new clinical fracture (RRR 35% [95% CI 16–50%], ARR 5.3%), clinical non-vertebral fracture (RRR 27% [95% CI 2–45%], ARR 3.1%) and new clinical vertebral fracture (RRR 46% [95% CI 8–68%], ARR 2.1%). A non-significant trend towards reduction in hip fracture (RRR 30% [95% CI 19–59%], ARR 1.5%) was observed. The safety analysis revealed a statistically significant reduction in deaths from any cause for the individuals treated with zoledronate (RRR 28% [95% CI 7–44%], ARR 3.7%). A sub-group analysis of the HORIZON-Pivotal Fracture Trial (PFT) observed a comparable effect of zoledronate treatment on the incidence of new vertebral and non-vertebral fractures for individuals with and without prevalent vertebral fracture at baseline [20].
-
Denosumab: A post hoc analysis of the FREEDOM study evaluated denosumab for secondary fracture prevention [21]. A statistically significant reduction in the incidence of any subsequent fracture (RRR 39% [95% CI 28–49%], ARR 6.8%) was observed, with similar efficacy in those who had prior vertebral fractures (RRR 35%, ARR 6.6%) or non-vertebral fractures (RRR 34%, ARR 6.1%) at baseline which was highly significant (p < 0.0001 for both groups).
-
Raloxifene: Among the sub-group of women in the MORE study who had a vertebral fracture at baseline, those receiving the licensed 60 mg dose of raloxifene sustained significantly fewer new vertebral fractures compared to placebo (RRR 30% [95% CI 20–50%], ARR 6%) [22]. However, raloxifene did not demonstrate a statistically significant reduction in the incidence of non-vertebral or hip fractures.
-
Teriparatide: In women with postmenopausal osteoporosis and at least one vertebral fracture at baseline [23], teriparatide 20 μg per day significantly reduced the incidence of new vertebral fractures (RRR 65% [95% CI 45–78%], ARR 9.3%) and non-vertebral fragility fractures (RRR 53% [95% CI 12–75%], ARR 2.9%). However, the definition of non-vertebral fracture was not directly comparable to that used in other studies, and teriparatide did not demonstrate a statistically significant reduction in the incidence of hip fractures.
-
Strontium ranelate: Strontium ranelate significantly reduced the incidence of new vertebral fracture (RRR 41% [95% CI 27–52%], ARR 11.9%) but not non-vertebral fractures in women with postmenopausal osteoporosis and at least one vertebral fracture at baseline [24]. A pooled analysis of the SOTI and TROPOS study populations reported a statistically significant reduction in the incidence of first vertebral fracture (RRR 46% [95% CI 19–63%], ARR 7.6%) among women with a prevalent non-vertebral fracture, who did not have a prevalent vertebral fracture [25]. A pre-planned sub-analysis of postmenopausal women with osteopenia and a prevalent vertebral fracture, in the combined studies, reported a significant reduction in the incidence of new vertebral fractures (RRR 37% [95% CI 11–56%], ARR 8.1%) [26].
In light of the diverse array of effective osteoporosis treatments which are available to reduce future fracture risk, it is of great concern that a pervasive and persistent secondary prevention care gap is evident throughout the world. The International Osteoporosis Foundation (IOF) Capture the Fracture® program website provides an up-to-date bibliography of all PubMed cited secondary prevention audits and surveys, undertaken internationally, nationally, regionally and locally [27]. Studies from all regions of the world are featured on the website:
-
Africa: South Africa
-
Asia: China, Hong Kong, Japan, Malaysia, Singapore, South Korea, Taiwan, Thailand
-
Europe: Austria, Belgium, Denmark, Finland, France, Germany, Ireland, Italy, The Netherlands, Norway, Sweden, Switzerland, UK
-
Latin America: Brazil
-
Middle East: Israel, Saudi Arabia
-
North America: Canada, USA
-
Oceania: Australia, New Zealand
In response to this widely documented care gap, models of care have been developed in many countries to ensure that fragility fracture patients receive secondary preventive care—which includes both osteoporosis management and intervention to prevent falls—in a consistent and reliable fashion. The most common models are referred to as orthogeriatrics services (aka orthopaedic-geriatric co-care services or geriatric fracture centres) and Fracture Liaison Services (FLS).
The complementary roles of orthogeriatrics services and FLS are nicely illustrated in consensus guidelines from the UK. In 2007, the British Orthopaedic Association (BOA) and the British Geriatrics Society (BGS) published The Care of Patients with Fragility Fracture (aka ‘the Blue Book’), with contributions from representatives of the Age Anaesthesia Association, Faculty of Public Health, Society for Endocrinology, Royal College of Nursing and the UK National Osteoporosis Society [28]. The first section of the Blue Book advocated widespread implementation of coordinated, multidisciplinary care for hip fracture patients through establishment of orthogeriatrics services in hospitals. Such models of care are designed to expedite surgery, ensure optimal management of the acute phase through adherence to a care plan overseen by senior staff in orthopaedics and geriatrics/internal medicine and deliver secondary fracture prevention through osteoporosis management and falls prevention. Implementation of orthogeriatrics services has gained momentum globally in recent years, supported by development of national hip fracture registries to enable benchmarking of the quality of hip fracture care against best practice guidelines [29].
The UK National Health Service (NHS) provides a large-scale illustration of the impact that orthogeriatrics services, supported by the National Hip Fracture Database (NHFD) [30] and quality incentives from government [31], can have upon posthip fracture secondary preventive care. The UK NHFD is currently the largest ongoing audit of hip fracture care in the world, with more than 454,000 case records entered since it was launched in tandem with the Blue Book in 2007 (personal communication: C. Boulton). The 2015 NHFD annual report described the care of 64,102 people who presented with a hip fracture in 2014, representing nearly 95% of all cases in England, Wales and Northern Ireland [32]. More than 80% of the patients were started on osteoporosis treatment or were referred for bone mineral density (BMD) testing or bone clinic assessment. Further, more than 96% of the patients were offered a multifactorial risk assessment to identify and address future falls risk and were offered individualised intervention where appropriate.
The second section of the Blue Book called for widespread implementation of FLS. The purpose of an FLS is to ensure that all patients aged 50 years or over who present to health services with a fragility fracture undergo fracture risk assessment and receive osteoporosis treatment in accordance with national guidelines. The FLS would also refer older patients into local falls prevention services. In terms of a ‘division of labour’, orthogeriatrics services typically deliver secondary preventive care for hip fracture patients and FLS deliver secondary preventive care for non-hip fragility fracture patients (e.g. wrist, humerus, pelvis and those vertebral fractures which come to clinical attention).
During the last 15 years, studies describing the design and performance of FLS have been published from many countries [8]. However, variation in FLS service design and reporting of processes and outcomes make comparisons between services difficult. In order to establish which specific features of an FLS are associated with optimal case finding and implementation of osteoporosis treatment guidelines, Australian investigators undertook a systematic review and meta-analysis of the secondary fracture prevention literature [33]. The various FLS were classified into four types:
-
Type A or 3i FLS models which deliver identification, investigation and initiation of interventions.
-
Type B or 2i FLS models which deliver identification and investigation but rely on initiation of interventions by the primary care physician (PCP).
-
Type C or 1i FLS models which deliver identification and an alert to the PCP that further investigations are needed but rely on the PCP to organise those investigations and initiate interventions, where warranted.
-
Type D or ‘Zero i’ models which provide osteoporosis education to the patient but do not alert or educate the PCP.
The proportion of patients undergoing BMD testing and receiving osteoporosis treatment for each type of FLS model is shown in Table 2. Clearly, type A (3i) and type B (2i) FLS models result in considerably more fracture patients being investigated and initiated on treatment. While practically all osteoporosis treatment guidelines worldwide recommend that fragility fracture patients should be assessed for osteoporosis, the proportion that should receive osteoporosis treatment remains an ongoing matter of debate. In 2005, the first UK National Institute for Health and Care Excellence (NICE) technology appraisal on osteoporosis treatments for the secondary prevention of fracture estimated that up to 70% of women over 50 years of age with a fragility fracture could benefit from treatment [34]. This analysis assumed that all women aged 75 years or over could be indicated for treatment in the absence of BMD testing and a smaller proportion of younger women. Given that a minority of fracture patients in this age group are likely to suffer early postfracture mortality, 50 to 70% might represent a pragmatic estimate of what would constitute a clinically appropriate range for treatment rates among all fragility fracture patients aged 50 years or over.
A meta-analysis has reported that osteoporosis treatments are associated with reduced mortality when taken by individuals who are at high risk of fracture [35]. This finding could be influenced by referral bias: individuals who are perceived to have a low life expectancy may be less likely to receive osteoporosis treatments. In 2014, however, in addition to a beneficial effect on fracture rates, care delivered by an FLS was shown to reduce mortality of fracture patients [36]. The FLS model of care has also been subject to cost-effectiveness modelling. An example of this approach is a cohort health-state transition model (a Markov model) developed to evaluate the Glasgow FLS in Scotland, UK [37]. The model demonstrated that 18 fractures were prevented, including 11 hip fractures, and £21,000 (26,250 €, US$30,000) was saved per 1000 patients managed by the Glasgow FLS vs ‘usual care’ in the UK.
It should be noted that vertebral fractures make up only a small proportion of FLS case loads [38–45], as shown in Table 3. This is an important shortcoming which must be addressed, because vertebral fractures are the most common fragility fracture and are underdiagnosed throughout the world [46]. Further, the prevalence of vertebral fractures among individuals who sustain hip fractures has been shown to be very high. Studies from Japan and Spain reported that 78 and 63% of hip fracture patients had prevalent vertebral fractures, respectively [47, 48]. Vertebral fractures were defined by the Japanese and Spanish investigators on the basis of the criteria established by The Japanese Society for Bone and Mineral Research [49] and Genant [50], respectively. It should be noted that while clinical vertebral fractures are a risk factor for hip fracture, asymptomatic grade 1 morphometric fractures have no prognostic value [51]. A considerable volume of imaging with plain radiography, and X-rays, CT and MRI scans is undertaken among older people in hospitals worldwide every day. Approaches to improve vertebral fracture case finding from such activity has been reviewed elsewhere [52].
Vertebral fracture assessment (VFA) provides a low radiation exposure alternative to standard X-ray that could be conducted when patients attend for a dual energy X-ray absorptiometry (DXA) scan. This approach has been explored in the FLS setting [53, 54]. Among patients presenting with non-vertebral fractures that were assessed by a FLS, the overall prevalence of vertebral deformity was of the order of a quarter to a fifth (25 [53] and 20% [54]). VFA identified a substantial burden of prevalent vertebral fractures that had not been previously documented. The proportion of non-vertebral fracture patients that would be managed differently as a result of conducting VFA was relatively small (9 [53] and 3% [54]). This is perhaps not surprising given that the patients investigated had a non-vertebral fracture which triggered FLS assessment. However, incorporation of VFA into FLS protocols has the potential to reveal two sub-groups of non-vertebral fracture patients that may be managed differently as a result of ascertainment of vertebral fracture status:
-
Patients with ≥1 vertebral fracture (grade 2 or higher) and an osteopenic BMD
-
Patients with multiple vertebral fractures and profoundly osteoporotic BMD
In both cases, knowledge of the presence of vertebral fractures has the potential to impact upon clinical decision making to optimise care for the individual patient’s circumstances. In 2007, Siris et al. evaluated the combination of ascertaining vertebral fracture status and BMD measurement in fracture risk prediction [55]. These investigators concluded
‘For any given BMD T-score, the risk of an incident vertebral, non-vertebral fragility, and any fracture differs by up to twelve times, 2 times, and 7 times, respectively, when information regarding spine fracture burden is considered. In the absence of knowledge about the prevalent vertebral fracture status, assessments based solely on BMD may under- or overestimate the true risk of a patient experiencing an incident fracture’.
Further, when clinicians use the FRAX® tool to calculate an individual’s fracture risk, the notes on risk factors state [56]
‘A special situation pertains to a prior history of vertebral fracture. A fracture detected as a radiographic observation alone (a morphometric vertebral fracture) counts as a previous fracture. A prior clinical vertebral fracture or a hip fracture is an especially strong risk factor. The probability of fracture computed may therefore be underestimated. Fracture probability is also underestimated with multiple fractures’.
Accordingly, the presence of a vertebral fracture could significantly influence the fracture risk calculated by FRAX®. Given that an increasing number of clinical guidelines make reference to intervention thresholds based upon a FRAX® score, the decision to treat or not may be influenced by knowledge of vertebral fracture status. Another conclusion of the FLS VFA work was that VFA should ideally be conducted on all patients that are referred for DXA who do not have a clinical fracture history, in order to improve case finding of vertebral fractures [53].
Clinical or Quality Standards for FLS have been developed in Canada [57], New Zealand [58] and the UK [59, 60]. IOF has also developed internationally endorsed standards for FLS in the form of the Capture the Fracture® Best Practice Framework (BPF) [61–63]. The Capture the Fracture® BPF comprises a comprehensive suite of 13 standards:
-
1.
Patient identification standard
-
2.
Patient evaluation standard
-
3.
Postfracture assessment timing standard
-
4.
Vertebral fracture standard
-
5.
Assessment guidelines standard
-
6.
Secondary causes of osteoporosis standard
-
7.
Falls prevention services standard
-
8.
Multifaceted health and lifestyle risk-factor assessment standard
-
9.
Medication initiation standard
-
10.
Medication review standard
-
11.
Communication strategy standard
-
12.
Long-term management standard
-
13.
Database standard
The Capture the Fracture® program encourages FLS throughout the world to apply for Best Practice Recognition which can result in the FLS featuring on the ‘Map of best practice’ on the Capture the Fracture® program’s website. In 2015, an analysis of the first 60 FLS to apply for Best Practice Recognition was undertaken to confirm that a single framework with set criteria was able to benchmark services across healthcare systems worldwide [62]. The FLS represented six continents and were highly heterogeneous in many aspects, serving populations from 20,000 to 15 million individuals, being a mixture of private and publicly funded systems and managing vastly different number of fracture patients at individual sites. The assessment process considered performance of the FLS against the standards across five domains: (a) patients with hip fractures, (b) patients admitted for other non-hip fragility fractures, (c) patients seen primarily in the ambulatory setting with fragility fractures, (d) patients with vertebral fragility fractures and (e) organisational and falls services. The domain-level rankings contributed to an overall ranking of gold, silver, bronze or black (insufficient) level of achievements for the FLS, in addition to a score in the range zero to five. Overall, 27 hospitals scored gold, 23 silver and 10 bronze, with care for the hip fracture patients achieving the highest proportion of gold grading for an individual domain, while vertebral fracture achieved the lowest. The authors concluded that the BPF was fit for purpose as a tool to benchmark performance of FLS globally. At the time of writing, 174 FLS were featured on the map of best practice: 41 ranked gold, 47 silver, 20 bronze and 66 still under review or in development.
Government organisations in several countries have supported implementation of systematic approaches to fragility fracture care and prevention which prioritise secondary fracture prevention, including Australia, Canada, New Zealand, Singapore and UK [8, 64]. The overarching strategy originally developed by the Department of Health in England [65] has informed policy development in other countries, such as New Zealand [66, 67], as illustrated in Fig. 1.
Primary fracture prevention
While in many populations, approximately one in two women and one in five men will sustain a fragility fracture during their lifetimes after age 50 years [68]: at any given point in time, the majority of older people lack a fracture history. Strategies to develop clinically effective and cost-effective approaches to primary fracture prevention must first establish the size of the primary prevention population in a particular jurisdiction. Further, which first fragility fracture is to be prevented will significantly influence the cost-effectiveness of such strategies, with ‘hip fracture as first fragility fracture’ being an obvious candidate.
Several studies make quantification of the primary prevention population possible for some European countries, which have sought to determine the incidence and prevalence of osteoporosis and fragility fractures among postmenopausal women. In 2011, Gauthier et al. developed a disease model that aimed to estimate the burden of osteoporosis at a national level [69]. This model was validated using Swedish data and has since been adapted for France [70], Germany [71], Italy [72] and the UK [73]. As illustrated in Table 4, the individual national models identified the number of women aged 50 years or over in each country based on information from the relevant national statistics organisation. The proportion of women with a prior history of at least one fragility fracture varied from 10% in France to almost 23% in Sweden. Consequently, the proportion of fracture-free women—the primary prevention population—ranged from 77% in Sweden to almost 90% in France.
Studies have not been conducted to determine the proportion of men with a history of at least one fragility fracture at any skeletal site in the countries mentioned previously. However, a compendium of country-specific reports for the European Union countries did provide estimates of prior hip and vertebral fracture history for men in 2010 [74]. An associated report suggests that the sum of prior hip and prior clinical vertebral fractures represents approximately 30% of all prior fragility fractures [75]. The relative proportions of women and men in the five countries with a prior history of hip or vertebral fracture in 2010 is shown in Table 5 (n.b. the populations of women aged 50 years and over differ slightly between Tables 4 and 5 because of a different data source for the populations being used in the compendium of country-specific reports). As is well known, more fractures occur in older women compared to older men, resulting in a higher proportion of older women having a prior fracture history compared to older men. That being said, approximately one third of hip fractures worldwide occur in men, so osteoporosis management of the relatively small proportion of men who have a prior history of fracture should not, as is often the case, be neglected [76].
While demonstrating cost-effectiveness of a primary fracture prevention strategy is of great importance in the cost-constrained circumstances in which many health systems currently operate, providing appropriate clinical care to individuals who are at high risk of sustaining debilitating first fractures at sites other than the hip should not be ignored. Vertebral fractures result in pain, functional disability and decreased quality of life and are also associated with excess mortality [77]. Major non-hip, non-vertebral fractures have been demonstrated to be associated with 20% excess mortality during the first 5 years postfracture [78].
The secondary fracture prevention care gap has been well documented, as described in the previous section of this review. While specific studies have not been undertaken in primary fracture prevention, it seems reasonable to assume that a care gap also exists for the high-risk primary prevention population. A report on osteoporosis in the European Union (EU) published in 2013 documented national prescribing levels [75]. These data, in combination with an algorithm which calculated the number of patients who were eligible for treatment in each of the 27 EU member states at the time, enabled estimation of the potential treatment gap for each country in 2010. This approach assumed that all those treated were actually eligible for treatment and not at a lower level of risk, so may have underestimated the treatment gap among high-risk patients. In total in the EU, 10.6 million out of 18.4 million women who were eligible received treatment. Among men, 1.7 million men out of the 2.9 million men who were eligible received treatment.
Strategies to prevent first fractures could function through several ‘tracks’. For example, the next two sections of this review, relating to osteoporosis induced by medicines and diseases associated with osteoporosis, will, in part, serve to deliver primary fracture prevention in a systematic fashion. The advent of absolute fracture risk calculators, such as the FRAX® tool, provides a means to stratify fracture risk in the entire older population. The UK National Osteoporosis Guideline Group (NOGG) has based its guidance on FRAX®, where an intervention threshold for 40 to 90 year olds is set at a risk equivalent to that expected in a woman with a prior fracture [79]. Many countries have subsequently adopted the approach taken by NOGG [9]. The US National Osteoporosis Foundation (NOF) guidance recommends initiation of treatment in the following three scenarios [80]:
-
In those with hip or vertebral (clinical or asymptomatic) fractures.
-
In those with T-scores ≤−2.5 at the femoral neck, total hip or lumbar spine by DXA.
-
In postmenopausal women and men age 50 years old or older with low bone mass (T-score between −1.0 and −2.5, osteopenia) at the femoral neck, total hip or lumbar spine by DXA and a 10-year hip fracture probability ≥3% or a 10-year major osteoporosis-related fracture probability ≥20% based on the US version of FRAX®.
Just as the FLS model of care has been developed to close the secondary prevention care gap, analogous models now need to be developed to deliver primary fracture prevention in a systematic fashion. Equipped with knowledge of which medicines induce osteoporosis, what other diseases have osteoporosis as a common comorbidity and online access to absolute fracture risk calculators to stratify fracture risk in the population, the necessary case-finding tools are now available to develop effective models of care to prevent the first fracture.
Osteoporosis induced by medicines
Many classes of drugs have been shown to adversely affect BMD and/or elevate fracture risk. While links have not been proven to be causal in every case, the drug classes shown in Table 6 have all been associated with fracture outcomes. It is beyond the scope of this review to describe in detail the mechanisms of action, epidemiology of BMD loss and/or increase in risk of fragility fractures, and utility of interventions to prevent bone loss for each drug class. Accordingly, key observations on the impact of each class on BMD and fracture risk are indicated in Table 6, primarily in accordance with the findings of Panday et al. in their 2014 review on medication-induced osteoporosis [81]. Recent literature reviews specific to each drug class are also cited to provide the reader with a source of more detailed current information [82–91]. A focus on three commonly used classes—glucocorticoids, androgen deprivation therapy and aromatase inhibitors—serves to illustrate the potential benefits of strategies to prevent osteoporosis induced by medicines.
Glucocorticoid-induced osteoporosis
Glucocorticoid (GC)-induced osteoporosis is the most common cause of secondary osteoporosis [92]. Among adults aged 18 years or over, it has been estimated that 7.5% have received at least one prescription for an oral GC [93]. GCs exert their effects on bone quality and bone mass through a number of direct effects on osteoblasts, osteoclasts and osteocytes, in addition to indirect effects mediated through the neuroendocrine system, calcium metabolism and muscle [92]. GC-induced fractures occur most commonly at sites with significant amounts of cancellous bone, such as the vertebrae and femoral neck. Among chronic GC users, up to 30–50% of the patients may sustain fractures, depending on the population studied.
Clinical guidelines for the prevention and treatment of GC-induced osteoporosis are available in many countries. In 2012, the Joint IOF–European Calcified Tissue Society (ECTS) Glucocorticoid-induced Osteoporosis Guidelines Working Group published a framework for the development of guidelines for the management of GC-induced osteoporosis [94]. This comprehensive framework reviewed the epidemiology of GC-induced osteoporosis and fracture risk assessment based on 10-year probabilities ascertained from FRAX®. A systematic review was performed to assess the efficacy of interventions. The Working Group proposed management algorithms which could be tailored to context of healthcare delivery in individual countries.
Despite the widespread availability of licensed medications to prevent and treat GC-induced osteoporosis, and numerous clinical guidelines to support healthcare professionals to deploy these interventions, a major care gap exists. In 2014, Albaum et al. published a systematic review of studies undertaken between 1999 and 2013 which reported the proportion of patients on chronic oral GC therapy who received osteoporosis management [93]. The meta-analysis included studies from North America, Europe and other regions of the world. The majority of studies (>80%) reported that less than 40% of chronic oral GC users received BMD testing or osteoporosis therapy. A temporal analysis concluded that there was little evidence for improvement over time.
Clinicians from the Geisinger Health System in the USA identified the GC-induced osteoporosis care gap among their own GC users, despite educational and process changes which had been implemented over several years. To overcome this deficiency, a specific Glucocorticoid-Induced Osteoporosis Program (GIOP) was developed and implemented [95]. The GIOP team included a nurse specialist program leader, physician co-leader, nurse specialist care provider, physician consultants and data manager. The stated goals of GIOP were
-
identifying at-risk patients in the Geisinger Health System
-
educating patients
-
developing/implementing pathways to improve GC-induced osteoporosis diagnosis and treatment
-
monitoring GC-induced osteoporosis outcomes
-
using technology/process flows to ‘make it easy to do the right thing’
Two hundred chronic GS users were seen at baseline, and follow-up visits were scheduled at 6 and 12 months. Key outcomes of the program at 12 months included
-
Patients’ retention of knowledge, frequency of exercise and 25(OH) vitamin D concentrations all significantly improved.
-
A significant decrease in GC dose was observed.
-
Ninety-one percent of the patients considered at high fracture risk were taking a bisphosphonate or teriparatide, and 96% of the patients overall were adherent to their prescribed regimen of calcium, vitamin D and prescription treatment, where indicated.
Geisinger’s GIOP provides an example of a model of care which can reliably deliver best practice in the prevention and treatment of GC-induced osteoporosis.
Androgen deprivation therapy-induced osteoporosis
Prostate cancer is the most common non-cutaneous malignancy. The current lifetime risk of developing prostate cancer (PC) is estimated to be almost 17% (i.e. one in six men) [96]. Androgen deprivation therapy (ADT), usually in the form of a gonadotropin-releasing hormone agonist (GnRH), is a mainstay of treatment of metastatic, locally advanced or recurrent PC. Currently, approximately one third of PC patients receive ADT [97]. The purpose of ADT is to reduce serum testosterone to castrate levels, with the consequent potential to induce osteoporosis and increase fracture risk.
Clinical guidelines for the prevention and treatment of ADT-induced osteoporosis are available in many countries. In 2013, the IOF Committee of Scientific Advisors (CSA) Working Group on Cancer-induced Bone Disease published a position paper on cancer-associated bone disease [98]. In relation to prostate cancer, the pathophysiology and epidemiology of ADT-induced osteoporosis were reviewed. The role of BMD testing and fracture risk assessment was considered, in addition to analysis of the evidence base for the prevention of bone loss and fractures with osteoporosis treatments. An algorithm for the management of ADT-induced osteoporosis was provided. In 2014, the European Society for Medical Oncology (ESMO) published clinical practice guidelines relating to bone health in cancer patients, including PC [99]. The guidelines identified three distinct areas of cancer management that make consideration of bone health in cancer patients important:
-
Bone metastases are common in many solid tumours, including those of the prostate.
-
Many cancer treatments, including ADT, have effects on reproductive hormones which can adversely affect the process of normal bone remodelling.
-
On account of the bone marrow micro-environment being intimately involved in metastatic processes, bone-targeted treatments can reduce metastasis of cancer to bone and so, potentially, improve survival.
The ESMO guidelines provide a management algorithm and practical recommendations on optimising bone health for cancer patients.
While the osteoporosis care gap for ADT-induced osteoporosis has not been documented as comprehensively as is the case for secondary fracture prevention and GC-induced osteoporosis, local studies from several countries suggest that a gap exists:
-
Canada: In 2012, a cross-sectional survey-based study was conducted involving practicing urologists and genitourinary radiation oncologists across Canada [100]. The majority of respondents correctly identified the guideline-concordant frequency of repeat DXA scans (76.3%), vitamin D (70.3%) and calcium (53.2%) intake and that bisphosphonates/denosumab should always be considered for patients with a history of one low-trauma fracture (57.6%). However, in practice, only one third (32.5%) reported routinely measuring BMD prior to starting ADT and routinely measuring BMD 1–2 years following the initiation of ADT (36.6%). Less than 5% of the respondents routinely used a validated fracture risk assessment tool.
-
India: In 2011, telephone interviews were undertaken with 108 members of the Urological Society of India. Less than one fifth (19.8%) of the urologists routinely measured BMD before starting ADT. Only half of respondents stated that they advised their patients that osteoporosis and adverse skeletal events could be a side effect of ADT. While a majority of urologists (59.6%) frequently used zoledronic acid in their clinical practice, approximately half of these users prescribed the bisphosphonate to men without knowledge of their BMD status. Very limited access to BMD testing in India is likely to contribute to this practice, as reported in the IOF Asia-Pacific Regional Audit published in 2013 [101].
-
USA: Men diagnosed with PC between 2005 and 2007 in the Texas Cancer Registry/Medicare-linked database (n = 2290) were analysed to determine what proportion underwent BMD testing and/or received osteoporosis treatment [102]. Less than one tenth (8.6%) underwent DXA within 1 year before and 6 months after initiation of ADT. Among the approximately 50% of study subjects who were enrolled in the Medicare part D scheme (n = 1060), 5.6% received bone sparing drugs when started on ADT, and 12.6% received bone sparing drugs or underwent DXA.
The Kaiser Permanente Healthy Bones Program has specifically focused on delivery of appropriate osteoporosis assessment to men diagnosed by PC between 2003 and 2007 in the Kaiser Permanente Southern California health system [97]. The investigators created two study cohorts:
-
Healthy Bones Program (HBP) group: any patient with PC who underwent BMD measurement at most 3 months before their first administration of ADT.
-
Non-HBP group: all other PC patients.
Men managed by the HBP group with BMD T-scores ≥−2.5 received lifestyle advice relating to smoking cessation, exercise and adequate intake of calcium (1200 mg/day) and vitamin D (400–800 IU/day). Men with T-scores <−2.5 were also treated with a bisphosphonate and followed up by an endocrinologist. The incidence rate of hip fractures per 1000 person-years was 5.1% (95% CI, 3.0–8.0) in the HBP group as compared to 18.1% (95% CI, 10.5–29.0) in the non-HBP group.
Kaiser Permanente’s HBP provides an example of a model of care which can reliably deliver best practice in the prevention and treatment of ADT-induced osteoporosis.
Aromatase inhibitor-induced osteoporosis
Breast cancer (BC) is the most common neoplasm in women and the leading cause of cancer-related mortality in women [103]. One in eight women will develop BC during their lifetime, and it accounts for almost a quarter (23%) of total cancer cases and 14% of all cancer-related deaths. Aromatase inhibitors (AI) are currently considered to be the gold standard adjuvant treatment for postmenopausal women with hormone receptor-positive BC. The aromatase enzyme converts androgens into estrogens providing the main source of endogenous estrogens after the menopause. Thus, bone loss and increased fracture risk is an expected side effect of AI therapy.
Clinical guidelines for the prevention and treatment of AI-induced osteoporosis are available in many countries. In 2012, the European Society for Clinical and Economical Aspects of Osteoporosis (ESCEO) published guidance on prevention of bone loss and fractures in postmenopausal women treated with AIs [85]. Key recommendations included:
-
All women starting AI therapy should be assessed for their baseline risk of sustaining a fragility fracture, using DXA examination, biochemical assessment and evaluation of all clinical risk factors with the FRAX® tool.
-
General advice on appropriate levels of physical exercise and vitamin D and calcium intake should be given.
-
Antiresorptive treatment should be offered to the following groups:
-
Pre-menopausal women with ovarian suppression undergoing tamoxifen or AI therapy with T-score <−1.0 or presence of ≥1 vertebral fracture or history of fragility fracture (any site, irrespective of BMD).
-
Postmenopausal women with history of personal fragility fracture (any site) or age ≥75 years old (irrespective of BMD).
-
Postmenopausal women with T-score <−2.5 or <−1.5 + ≥1 clinical risk factor or T-score <−1.0 + ≥2 clinical risk factors or FRAX® 10-year risk of hip fracture ≥3%.
While the osteoporosis care gap for AI-induced osteoporosis has not been documented as comprehensively as is the case for secondary fracture prevention and GC-induced osteoporosis, studies from the UK [104] and the USA [105] have again identified a care gap. The US study reported that less than half (44%) of women underwent BMD testing within 14 months of continuous AI use for at least 9 months [105]. Furthermore, 75 and 66% of women failed to have BMD tests done during the second and third annual time periods after continuous AI use for almost 2 and 3 years, respectively.
Quality improvement initiatives from Italy [106] and the UK [104] provide examples of efforts to manage bone health of women treated with AI therapy in a systematic fashion. Investigators from London, UK, used a text recognition system installed on the computers of secretaries in the oncology department to automate referral of women age 50 to 80 years who were undergoing treatment for BC to an Osteoporosis Nurse Specialist (ONS) [104]. In addition, text was automatically inserted into letters from the oncology department to the patients’ PCP, advising them that their patient would receive an osteoporosis assessment and management, where warranted. The proportion of BC patients referred for osteoporosis assessment increased tenfold upon implementation of this system.
Diseases associated with osteoporosis
Many diseases pre-dispose an individual to developing osteoporosis and/or sustaining fragility fractures. These comprise a broad array of disorders including autoimmune, digestive and gastrointestinal, endocrine and hormonal, hematological, neurological, mental illness, cancer and AIDS/HIV. An overview of associations between several common diseases [107–112] and bone loss and/or fracture risk [113–120] and current evidence for the existence of an osteoporosis care gap [121–125] for individuals with these diseases are provided in Table 7. For some of the diseases, the frequent presence of osteoporosis as a comorbidity has prompted development of disease-specific clinical guidelines intended to reduce fracture risk [126–128]. Where guidelines have been developed, efforts should be made throughout the world to implement their recommendations to improve the bone health of these individuals as a standard component of management of the particular disease. With regard to diabetes, in light of the enormous number of individuals already affected, evidence-based guidelines for the management of osteoporosis in type 2 diabetes must be drafted and implemented as soon as possible. Similarly, evidence-based guidelines for the management of osteoporosis—and falls risk—in dementia must be drafted and implemented globally.
Public awareness of osteoporosis and fragility fractures
Throughout the world, public awareness of osteoporosis, and the fragility fractures it causes, is low. If the projected dramatic increase in the number of individuals sustaining fragility fractures in the first half of this century is to be attenuated, awareness must be increased. This section of the review will consider three key aspects of raising awareness and eliminating current confusion among lay people:
-
The importance of staying on treatment
-
Public awareness of osteoporosis and fracture risk
-
Public awareness of benefits vs risks of osteoporosis treatment
A determined global effort is required, involving healthcare professionals and their organisations, patient societies and policymakers, to provide the public with clear, consistent and compelling messages regarding bone health. Focusing on these three issues provides a framework to achieve that objective.
Adherence to treatment
There are two measures of adherence to treatment which are commonly used in studies; maximal achievement of these often requires contribution from prescriber as well as the patient:
-
Persistence: defined as either the time to treatment discontinuation or as the proportion of patients that at a certain time point still fill prescriptions without a gap in refills longer than an allowed period of time (e.g. 30, 60 or 90 days).
-
Compliance: defined as the ability of a patient to adhere to the dosing, timing and conditions described by the prescriber or in accordance with the medicine’s patient information leaflet. One indirect measure of compliance is the medication possession ratio (MPR). MPR is usually defined as the number of days of medication available to the patient divided by the number of days of observation.
Osteoporosis is a long-term condition which, therefore, requires a long-term management plan. Frequently, individuals at high risk of sustaining fragility fractures who have been initiated on osteoporosis treatment cease to take that treatment within the first year [129]. This problem should come as no surprise to our field as this phenomenon has been widely reported for other classes of medicines for treatment of chronic diseases, such as antihypertensives and statins. That being said, osteoporosis is somewhat unique in medicine in terms of the flexibility of dosing options that are available to patients, including daily, weekly or monthly tablets and daily, quarterly, six-monthly or annual injections or infusions. Accordingly, a first important step in raising awareness of osteoporosis is to ensure that individuals who have been initiated on drug therapy understand why their physician has decided that treatment is warranted.
In 2013, the Medication Adherence and Persistence Special Interest Group of the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) undertook a systematic literature review of interventions to improve osteoporosis medication adherence [130]. Key findings included:
-
patients who were most persistent with medications which had the least frequent dosing regimens.
-
electronic prescriptions in combination with verbal counselling that were associated with a 2.6-fold improvement in short-term compliance compared to verbal counselling alone.
-
with regard to patient education based interventions, the largest and least biased studies reviewed showed only marginal improvement in adherence.
An emerging body of evidence suggests that osteoporosis treatment initiated by a FLS for fragility fracture patients is more likely to be adhered to than regimens for patients managed in other settings. In 2011, the FLS at the University Hospital of St. Etienne, France, evaluated adherence among 155 fracture patients who were initially prescribed a specific osteoporosis treatment by the FLS [131]. Among the 90% of the patients (n = 140) who actually used the prescription to begin treatment, 80% were still taking treatment at 12 months. In terms of longer-term persistence, after 27.4 months (±11.7 months) of follow-up, 68% of the patients were persistent with their treatment. Among the persistent patients, 87% reported that they continued to comply with both the treatment dosing and administration conditions. In 2014, similar findings were reported by the FLS at Amiens University Hospital, France [132]. The proportion of patients initially treated by the FLS who continued to take treatment at 12 and 18 months was 74 and 67%, respectively. A report from the FLS at the Concord Repatriation General Hospital, Sydney, Australia, compared adherence among patients initiated on treatment by the FLS who were subsequently followed up by either the FLS or local PCPs [133]. Persistence at 24 months was similar in both groups, leading the investigators to conclude that the main function of an FLS is to initiate a management plan for osteoporosis after fractures occur. If effective communication between the FLS and local PCPs is established, PCPs are well placed and willing to manage osteoporosis care in the longer term.
Awareness of osteoporosis and fracture risk
In recent years, numerous studies have been conducted to characterise public awareness and understanding of osteoporosis, fracture risk and the link between them. In 2008, investigators from Kaiser Permanente Northwest, USA, sought to evaluate stakeholder perspectives on postfracture osteoporosis care delivered by an outreach program which targeted patients and PCPs [134]. Qualitative evaluation was undertaken by semi-structured, in-depth individual interviews with women aged 67 years or older who had sustained a clinical fracture (n = 10), PCPs (n = 9), quality and other healthcare managers (n = 20) and orthopaedic clinicians and staff (N = 28). As compared to other common conditions, PCPs noted, and patients demonstrated, a lack of understanding of osteoporosis and its management, which included:
-
Fatalism: Osteoporosis being confused with osteoarthritis, so promoting the notion that osteoporosis is an inevitable but benign consequence of aging.
-
Media influence: PCPs noted that patients would often seek BMD testing in response to suggestions to do so in the popular press.
-
Long-term treatment: Patients expressed concern regarding the duration of treatment with specific osteoporosis therapies and uncertainty regarding the consequence of stopping treatment.
In 2013, investigators from Toronto, Canada, evaluated the fragility fracture patients’ understanding of the link between osteoporosis and fractures [135]. The participants were drawn from a database created by the provincial postfracture screening programme, a component of the Ontario Osteoporosis Strategy. The main outcome for the study was the fracture patients’ response to the question ‘Do you think your broken bone could have been caused by having osteoporosis (thin or brittle bones)?’ The range of responses that were not in the affirmative was collapsed into one category ‘did not make the link’. At baseline, 93% (1615/1735) of fracture patients did not believe that their fracture could have been caused by osteoporosis. At follow-up, only 8.2% changed their perception. In adjusted analyses, several baseline characteristics were shown to be predictive of individuals who would be more likely to make the link. These included individuals who had sustained a previous fracture (odds ratio [OR] 1.7, 95% CI, 1.2–2.6), perception of osteoporosis pharmacotherapy benefits (OR 1.2, 95% CI, 1.0–1.5), diagnosis of rheumatoid arthritis (OR 2.6, 95% CI, 1.4–4.9) and perception of bones as ‘thin’ (OR 8.2, 95% CI, 5.1–13.1).
The international GLOW study has compared self-perception of fracture risk with actual risk among more than 60,000 postmenopausal women in ten countries in Europe, North America and Australia [136]. Key findings included
-
Among women reporting a diagnosis of osteopenia or osteoporosis, only 25 and 43%, respectively, thought their fracture risk was increased.
-
Among women whose actual fracture risk was increased based on the presence of any one of seven risk factors for fracture, the proportion who recognised their increased risk ranged from 19% for smokers to 39% for current users of glucocorticoid medication.
-
Only 33% of those with at least two risk factors perceived themselves as being at higher risk.
These studies illustrate that a major awareness gap exists in terms of what osteoporosis actually is and how osteoporosis underpins fracture risk. A number of Disease Awareness Campaigns (DAC) have been developed to provide the public with clear, evidence-based messages relating to osteoporosis and reducing fracture risk. The 2Million2Many campaign from the National Bone Health Alliance (NBHA) in the USA provides an innovative example of implementing this approach [137]. The key messages for 2Million2Many are very simple and compelling:
-
Every year, there are two million bone breaks that are no accident (in the USA).
-
They are the signs of osteoporosis in people as young as 50.
-
But only 2 out of 10 get a simple follow-up assessment.
-
Together, we can break osteoporosis before it breaks us. But we must speak up. Remember
-
Break a bone, request a test.
-
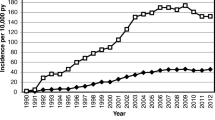
The impact of the 2Million2Many campaign cannot be assessed in isolation, because pursuant to the launch of this campaign in 2012, NBHA and NOF launched a major FLS implementation initiative in 2013 and a Qualified Clinical Data Registry focused on outcomes in osteoporosis and postfracture care in 2014 [137]. In 2015, the National Committee on Quality Assurance (NCQA) published The State of Health Care Quality 2015 which reported on postfracture osteoporosis care for women for the period 2007 to 2014 [138]. The concurrence of the NBHA/NOF initiatives and an improvement in postfracture care in the USA is illustrated in Fig. 2.
Postfracture osteoporosis assessment and/or treatment in the USA [138]. Footnote beneath Fig. 2: n.b. The data presented is for the Healthcare Effectiveness Data and Information Set (HEDIS®) measure Osteoporosis Management in Women Who Had a Fracture. This represents the percentage of women aged 65 to 85 years who sustained a fracture and who had either a BMD test or a prescription for a drug to treat osteoporosis in the 6 months after the fracture. Reproduced with permission from The State of Health Care Quality Report 2015 by the National Committee for Quality Assurance (NCQA). HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). To obtain a copy of this publication, contact the NCQA Customer Support at +1-888-275-7585 or www.ncqa.org/publications
In light of the widely documented secondary fracture prevention care gap described previously in this review, the initial focus of DACs should be to drive awareness throughout the population of the world that fracture begets fracture and that appropriate assessment and intervention, where warranted, can reduce the incidence of subsequent fractures.
Awareness of benefits and risks of osteoporosis treatments
During the last decade, treatment of osteoporosis has become embroiled in considerable controversy in the media on account of reports of rare side effects in the clinical literature. Mass media coverage of studies describing the incidence of osteonecrosis of the jaw (ONJ), atrial fibrillation (AF) and atypical femur fractures (AFF) has caused alarm and confusion among patients and PCPs. The importance of vigilant adverse event monitoring cannot be understated. However, healthcare professionals and their patients must not lose sight of the fact that the risk-benefit analysis in individuals who are at high risk of sustaining fragility fractures strongly favours treatment [139]. The current evidence base regarding the incidence of ONJ, AF and AFF can be summarised as follows:
-
ONJ: In 2015, an International Task Force estimated the incidence of ONJ in the osteoporosis population to be from 0.001 to 0.01%, which was marginally higher than the incidence observed in the general population of <0.001% [140].
-
AF: In 2015, a systematic review and meta-analysis determined the effects of bisphosphonates on AF, total adverse cardiovascular (CV) events, myocardial infarction (MI), stroke and CV death in adults with or at risk for low bone mass [141]. While the risk of AF was modestly but not significantly elevated for zoledronic acid exposure (6 trials; OR 1.24, 95% CI, 0.96–1.61), it was not for oral bisphosphonates (26 trials; OR 1.02, 95% CI, 0.83–1.24).
-
AFF: In 2012, investigators from Kaiser Permanente in the USA analysed a large population of bisphosphonate users to explore the relationship between duration of therapy and risk of AFF [142]. Age-adjusted incidence rates for an AFF were 1.78 per 100,000 person-years (95% CI, 1.5–2.0) with exposure from 0.1 to 1.9 years, which increased to 113.1 per 100,000 person-years (95% CI, 69.3–156.8) with exposure from 8 to 9.9 years. The authors concluded that the incidence of AFF increases with longer duration of bisphosphonate use, but this risk should be counterbalanced with the proven benefits in terms of fracture reduction.
In 2016, an analysis of hip fracture patients insured by United HealthCare Services in the USA observed that posthip fracture bisphosphonate treatment had declined from 15% in 2004 to 3% in the last quarter of 2013 [143]. During this period, the US Food and Drug Administration (FDA) issued three drug safety announcements relating to bisphosphonates and ONJ (2005), AF (2007) and AFF (2010). For the period 2003–2007, a 4% increase in bisphosphonate prescribing for hip fracture patients was observed every quarter (OR 1.04, 95% CI, 1.02–1.07). Pursuant to the 2007 FDA announcement on AF, this trend was reversed, with a 4% decrease in bisphosphonate use every quarter (OR 0.94, 95% CI 0.93–0.99). This sequence of events is clearly at odds with global efforts, including multisector collaboration in the USA through NBHA (a public-private partnership with five government liaisons from FDA, the Centers for Disease Control and Prevention [CDC], Centers for Medicare and Medicaid Services [CMS], National Aeronautics and Space Administration [NASA] and National Institutes of Health [NIH]) [137], to prevent individuals who have sustained serious fragility fractures from sustaining further and potentially life-threatening fractures. This experience underscores the need for healthcare professionals, their professional organisations and regulatory agencies to deliver balanced, tailored and meaningful information to patients regarding risk-benefit ratios.
Reimbursement and health system policy
In contrast with other comparable common non-communicable chronic diseases, osteoporosis has often not attracted a commensurate level of attention from health providers and governments. This section of the review will summarise findings relating to reimbursement and health system policy from regional audits conducted during this decade by IOF. An overview of the current situation in North America is also provided.
Access and reimbursement for osteoporosis assessment and treatment
Asia-Pacific
In 2013, IOF published the Asia-Pacific Regional Audit which provided an overview of the epidemiology, costs and burden of osteoporosis for 16 jurisdictions: Australia, China, Chinese Taipei, Hong Kong, India, Indonesia, Japan, Malaysia, New Zealand, Pakistan, Philippines, Republic of Korea, Singapore, Sri Lanka, Thailand and Vietnam [101]. This audit also provided information on access and reimbursement for diagnosis and treatment of osteoporosis. While Australia, Hong Kong, Japan, New Zealand, Republic of Korea and Singapore had 12–24 DXA machines per million of population, China, India, Indonesia, Pakistan, Philippines, Sri Lanka and Vietnam were severely underresourced with less than 1 DXA machine per million of population. Further, BMD testing was not fully reimbursed in many countries, which served as a barrier to accessing treatment. Reimbursement of osteoporosis treatment varied greatly across the region, ranging from 0 to 100% reimbursement for the most commonly prescribed medications.
Eastern Europe and Central Asia
In 2010, IOF published the Eastern European and Central Asian Regional Audit which provided an overview of the epidemiology, costs and burden of osteoporosis for 21 countries: Armenia, Azerbaijan, Republic of Belarus, Bulgaria, Czech Republic, Estonia, Georgia, Hungary, Republic of Kazakhstan, Kyrgyz Republic, Latvia, Lithuania, Republic of Moldova, Poland, Romania, Russian Federation, Slovakia, Slovenia, Republic of Tajikistan, Ukraine and Republic of Uzbekistan [144]. The number of DXA machines per million of population ranged from 20 in Slovenia to less than 1 in many Central Asian countries. In most countries, BMD testing was only accessible in the main cities. However, more than 40% of the population resides in a rural area in about one third of the countries. Reimbursement of osteoporosis treatment varied considerably between countries. In the Russian Federation, salmon calcitonin was the only treatment available.
European Union
In 2013, IOF in collaboration with the European Federation of Pharmaceutical Industry Associations (EFPIA) undertook a comprehensive osteoporosis and fragility fracture audit of the 27 EU member states at the time [74, 75, 145]. The audit used a previous estimate that European countries required 11 DXA machines per million of population to provide adequate osteoporosis care [146]. Austria, Belgium, Cyprus, Denmark, Finland, France, Germany, Greece, Italy, Portugal and Slovenia exceeded this threshold, while nine countries were considered to have very inadequate provision (Bulgaria, Czech Republic, Hungary, Latvia, Lithuania, Luxembourg, Poland, Romania and the UK). Eighteen countries offered unconditional reimbursement for DXA scanning. While most treatments were reimbursed in most countries, full reimbursement without income conditions was provided in only seven member states (Austria, Germany, Italy, The Netherlands, Slovenia, Sweden and UK). In the remaining countries, the level of reimbursement varied from 0 in Malta up to 100% for selected treatments in Luxembourg and Spain.
Latin America
In 2012, IOF published the Latin America Regional Audit which provided an overview of the epidemiology, costs and burden of osteoporosis for 14 countries: Argentina, Bolivia, Brazil, Chile, Columbia, Costa Rica, Cuba, Guatemala, Mexico, Nicaragua, Panama, Peru, Uruguay and Venezuela [147]. Brazil and Chile had 10 DXA machines per million of population, while other countries ranged from 0.9 to 6.7 per million of population. Access to BMD testing was often limited to urban areas throughout the region. Bisphosphonates were widely available throughout the region with considerable variability in reimbursement policy. Other osteoporosis therapies were also available, but access was often restricted.
Middle East and Africa
In 2011, IOF published the Middle East and Africa Regional Audit which provided an overview of the epidemiology, costs and burden of osteoporosis for 17 countries: Bahrain, Egypt, Kuwait, Iran, Iraq, Jordan, Kenya, Lebanon, Morocco, Palestine, Qatar, Saudi Arabia, South Africa, Syria, Tunisia, Turkey and United Arab Emirates [148]. The number of DXA machines per million of population ranged from 27 in Lebanon to 0 in Kenya. In most countries, BMD testing was only accessible in urban areas. Reimbursement for DXA scanning and osteoporosis treatment varied widely throughout the region.
North America
IOF has not conducted an audit in North America. Accordingly, the authors of this review sought a current summary of access and reimbursement for osteoporosis assessment and treatment from Osteoporosis Canada (personal communication: D. Theriault) and National Osteoporosis Foundation in the USA (personal communication: D. Lee).
In Canada, there is no single national healthcare system. Health care falls under the independent jurisdiction of each of the 10 provinces and 3 territories. There is reimbursement for many of the oral bisphosphonates in all Canadian provinces for seniors who are indicated for such treatment. However, coverage for other osteoporosis medications such as denosumab and zoledronic acid is quite variable depending on the province/territory.
In the USA, reimbursement for screening, treatment and other bone health interventions varies greatly depending on each patient’s health plan. To address these gaps, NBHA will convene a bone health ‘payer summit’ in 2017 comprising the major payers to solicit their feedback on the scientific and clinical evidence needed to reconsider these coverage and reimbursement decisions. This feedback will be used to inform the development of an evidence report that will provide evidence of the cost-effectiveness of these interventions to reduce future fracture risk.
Fragility fracture prevention in national policy
As for the previous section of this review, the IOF regional audits provide comprehensive information on the level of priority afforded to fragility fracture prevention by governments in the various regions of the world, which is summarised in Table 8 [67, 74, 75, 101, 144, 145, 147, 148]. With regard to the current situation in North America, Osteoporosis Canada (personal communication: D. Theriault) and the National Osteoporosis Foundation in the USA (personal communication: D. Lee) have provided summaries.
In Canada, provincial healthcare administrators are becoming increasingly aware of the compelling benefits of FLS in reducing the fracture burden and the associated healthcare costs. OC has launched a FLS Registry to showcase Canadian FLS meeting all eight of the Essential Elements for Fracture Liaison Services [149].
In the USA, healthcare reform is evolving from fee for service to supporting improved quality, prevention and care coordination with financial incentives (or penalties) to encourage healthcare professionals and health systems to report on and improve patient outcomes. There are a number of quality measures focused on osteoporosis and postfracture care, but performance around these measures remains low compared to other major chronic diseases. Further, a major drop in reimbursement for DXA scans performed in the office setting has led to a drop in the number of providers and more than one million less DXA scans performed per annum.
Fracture epidemiology in the developing world
It is well recognised in the literature that in the coming decades, the burden of fragility fractures will increasingly be borne by older people living in the developing world [150]. The IOF regional audits noted a dearth of data pertaining to fracture epidemiology in many developing countries [101, 144, 147, 148]. Arguably, the most obvious example of this challenge is India, which is poised to become the world’s most populous country in the next few decades. The 2013 IOF Asia-Pacific audit identified the pressing need for multicentre, large-scale hip fracture incidence studies to be conducted [101]. In due course, efforts by the Indian Society for Bone and Mineral Research (ISBMR) will provide robust fracture epidemiology to inform development of policy on fracture prevention in India. Similar initiatives are needed in Malaysia, Pakistan, Sri Lanka, Thailand and Vietnam.
In the course of the development of new FRAX® models, epidemiological estimates of the incidence of fractures have become available for major countries such as Brazil [151] and the Russian Federation [152]:
-
Brazil: In 2015, there were estimated to be 80,640 hip fractures in Brazil, of which 23,422 were in men and 57,218 in women. In 2040, the number of hip fractures is expected to rise to 55,844 in men and 141,925 in women, a rise of 238 and 248%, respectively.
-
Russian Federation: Extrapolation of robust fracture information collected in Yaroslavl and Pervouralsk to the entire population of the Russian Federation suggests that 112,000 hip fractures occurred in 2010. This was expected to rise to 159,000 in 2035. The estimated number of major osteoporotic fractures was expected to rise from 590,000 to 730,000 over the same time interval. Further large-scale, multicentre epidemiological studies should be conducted in Russia to confirm these estimates.
Provision of robust epidemiological estimates of fracture incidence throughout Asia-Pacific, Central Asia, Latin America, the Middle East and Africa will be a critical step towards supporting development of fracture prevention policies for these rapidly aging populations.
Summary and call to action
The first of the baby boomer generation began to retire in 2011. At that time, an editorial in this journal noted that 450 million people would celebrate their 65th birthday during the subsequent two decades [150]. Today, in 2016, a good number of them already have done so. In the absence of implementation of an evidence-based, multidisciplinary, system-wide, global response, osteoporosis and the fragility fractures it causes will impose a catastrophic burden on our older people, their families and carers and our health and social care systems. However, this is a catastrophe that can be averted.
This review has outlined a stepwise approach to case-finding individuals who are at high risk of sustaining fragility fractures. By first closing the secondary fracture prevention care gap, up to half of individuals who would otherwise fracture their hip could be treated to prevent this debilitating and costly injury. Integration of bone health and falls risk assessments into the management of individuals who take medicines which have adverse effects on bone must become standard practice. Similarly, individuals who are diagnosed with diseases which feature osteoporosis as a common comorbidity need to receive care that will minimise their fracture risk. When the needs of these obviously high-risk groups have been addressed, we must turn our attention to development of cost-effective strategies to prevent the first major osteoporotic fracture.
Public awareness of osteoporosis must be increased dramatically throughout the world. Effective disease awareness campaigns are needed to ensure that when an older person sustains a fragility fracture, their first thought—and that of their family and friends—is ‘Did that bone break because of osteoporosis?’ Health professionals and their organisations, national patient societies, health system leaders and regulatory agencies must work together to craft clear, balanced communications concerning the benefits and risks of treatments and the implications of choosing not to take treatment recommended by a clinician.
Finally, all governments need to establish osteoporosis as a national health priority, with commensurate human and financial resources to ensure that best practice is delivered for all patients in their jurisdictions. Where the current disease burden is not known, studies to close such evidence gaps must be commissioned forthwith.
We cannot ignore the current and growing burden that osteoporosis and fragility fractures impose upon our global society. This review clearly illustrates that we have the knowledge and tools that we need to manage bone health optimally for all. The time has come to make that possibility a reality.
References
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for C, Economic Aspects of O, Osteoarthritis, the Committee of Scientific Advisors of the International Osteoporosis F (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Gallagher JC, Melton LJ, Riggs BL, Bergstrath E (1980) Epidemiology of fractures of the proximal femur in Rochester, Minnesota. Clin Orthop Relat Res 163–171
Port L, Center J, Briffa NK, Nguyen T, Cumming R, Eisman J (2003) Osteoporotic fracture: missed opportunity for intervention. Osteoporos Int 14:780–784
McLellan A, Reid D, Forbes K, Reid R, Campbell C, Gregori A, Raby N, Simpson A (2004) Effectiveness of strategies for the secondary prevention of osteoporotic fractures in Scotland (CEPS 99/03). NHS Quality Improvement Scotland
Edwards BJ, Bunta AD, Simonelli C, Bolander M, Fitzpatrick LA (2007) Prior fractures are common in patients with subsequent hip fractures. Clin Orthop Relat Res 461:226–230
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res Off J Am Soc Bone Miner Res 15:721–739
Kanis JA, Johnell O, De Laet C et al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Akesson K, Mitchell PJ (2012) Capture the Fracture: a global campaign to break the fragility fracture cycle. In: Stenmark J, Misteli L (eds) World Osteoporosis Day Thematic Report. International Osteoporosis Foundation, Nyon
Kanis JA, Harvey NC, Cooper C, Johansson H, Odén A, McCloskey EV, the Advisory Board of the National Osteoporosis Guideline Group (2016) A systematic review of intervention thresholds based on FRAX: a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos accepted June, proofs July 2016
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int 15:175–179
Wells GA, Cranney A, Peterson J, Boucher M, Shea B, Robinson V, Coyle D, Tugwell P (2008) Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev CD001155
Wells GA, Cranney A, Peterson J, Boucher M, Shea B, Robinson V, Coyle D, Tugwell P (2008) Etidronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev CD003376
Wells G, Cranney A, Peterson J, Boucher M, Shea B, Robinson V, Coyle D, Tugwell P (2008) Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev CD004523
Albergaria BH, Gomes Silva BN, Atallah ÁN, Fernandes Moça Trevisani V (2010) Intravenous zoledronate for postmenopausal osteoporosis (Protocol). Cochrane Database Syst Rev 1–8
Bennett TG, Le Marshall K, Khan F, Wark JD, Brand C (2012) Denosumab for the treatment and prevention of postmenopausal osteoporosis (Protocol). Cochrane Database Syst Rev 1–10
Fleiss JL (1993) The statistical basis of meta-analysis. Stat Methods Med Res 2:121–145
Black DM, Steinbuch M, Palermo L, Dargent-Molina P, Lindsay R, Hoseyni MS, Johnell O (2001) An assessment tool for predicting fracture risk in postmenopausal women. Osteoporos Int 12:519–528
Doherty DA, Sanders KM, Kotowicz MA, Prince RL (2001) Lifetime and five-year age-specific risks of first and subsequent osteoporotic fractures in postmenopausal women. Osteoporos Int 12:16–23
Lyles KW, Colon-Emeric CS, Magaziner JS et al (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357:1799–1809
Eastell R, Black DM, Boonen S et al (2009) Effect of once-yearly zoledronic acid five milligrams on fracture risk and change in femoral neck bone mineral density. J Clin Endocrinol Metab 94:3215–3225
Palacios S, Kalouche-Khalil L, Rizzoli R et al (2015) Treatment with denosumab reduces secondary fracture risk in women with postmenopausal osteoporosis. Climacteric 18:805–812
Ettinger B, Black DM, Mitlak BH et al (1999) Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) investigators. JAMA 282:637–645
Neer RM, Arnaud CD, Zanchetta JR et al (2001) Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Meunier PJ, Roux C, Seeman E et al (2004) The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med 350:459–468
Roux C, Reginster JY, Fechtenbaum J et al (2006) Vertebral fracture risk reduction with strontium ranelate in women with postmenopausal osteoporosis is independent of baseline risk factors. J Bone Miner Res Off J Am Soc Bone Miner Res 21:536–542
Seeman E, DeVogelaer JP, Lorenc RS, Spector T, Brixen K, Vellas B, Balogh A, Stucki G, Meunier PJ, Reginster JY (2004) Strontium ranelate: the first anti-osteoporotic agent to reduce the risk of vertebral fracture in patients with lumbar osteopenia. IOF World Congress on Osteoporosis. Osteoporos Int, Rio de Janeiro, pp 507–509
International Osteoporosis Foundation (2016) Capture the Fracture® program website: audits & surveys page. http://www.capturethefracture.org/audits-surveys Accessed 30 March 2016
British Orthopaedic Association, British Geriatrics Society (2007) The care of patients with fragility fracture. 2nd edn
Fragility Fracture Network (2016) Fragility Fracture Network: global regions. http://fragilityfracturenetwork.org/global-regions/ Accessed 4 April 2016
Royal College of Physicians (2016) The National Hip Fracture Database. http://www.nhfd.co.uk/ Accessed 4 April 2016
Hawkes D, Baxter J, Bailey C, Holland G, Ruddlesdin J, Wall A, Wykes P (2015) Improving the care of patients with a hip fracture: a quality improvement report. BMJ Qual Saf 24:532–538
Royal College of Physicians (2015) National Hip Fracture Database (NHFD) annual report 2015. London
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, Eisman JA, March L, Seibel MJ (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24:393–406
National Institute for Health and Clinical Excellence (2005) Bisphosphonates (alendronate, etidronate, risedronate), selective oestrogen receptor modulators (raloxifene) and parathyroid hormone (teriparatide) for the secondary prevention of osteoporotic fragility fractures in postmenopausal women. Technology appraisal guidance 87
Bolland MJ, Grey AB, Gamble GD, Reid IR (2010) Effect of osteoporosis treatment on mortality: a meta-analysis. J Clin Endocrinol Metab 95:1174–1181
Huntjens KM, van Geel TA, van den Bergh JP, van Helden S, Willems P, Winkens B, Eisman JA, Geusens PP, Brink PR (2014) Fracture liaison service: impact on subsequent nonvertebral fracture incidence and mortality. J Bone Joint Surg Am 96:e29
McLellan AR, Wolowacz SE, Zimovetz EA, Beard SM, Lock S, McCrink L, Adekunle F, Roberts D (2011) Fracture liaison services for the evaluation and management of patients with osteoporotic fracture: a cost-effectiveness evaluation based on data collected over 8 years of service provision. Osteoporos Int 22:2083–2098
Giles M, Van Der Kallen J, Parker V, Cooper K, Gill K, Ross L, McNeill S (2011) A team approach: implementing a model of care for preventing osteoporosis related fractures. Osteoporos Int 22:2321–2328
Bogoch ER, Elliot-Gibson V, Beaton DE, Jamal SA, Josse RG, Murray TM (2006) Effective initiation of osteoporosis diagnosis and treatment for patients with a fragility fracture in an orthopaedic environment. J Bone Joint Surg Am 88:25–34
Blonk MC, Erdtsieck RJ, Wernekinck MG, Schoon EJ (2007) The fracture and osteoporosis clinic: 1-year results and 3-month compliance. Bone 40:1643–1649
Chevalley T, Hoffmeyer P, Bonjour JP, Rizzoli R (2002) An osteoporosis clinical pathway for the medical management of patients with low-trauma fracture. Osteoporos Int 13:450–455
Premaor MO, Pilbrow L, Tonkin C, Adams M, Parker RA, Compston J (2010) Low rates of treatment in postmenopausal women with a history of low trauma fractures: results of audit in a Fracture Liaison Service. QJM 103:33–40
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14:1028–1034
Clunie G, Stephenson S (2008) Implementing and running a fracture liaison service: an integrated clinical service providing a comprehensive bone health assessment at the point of fracture management. J Orthop Nurs 12:156–162
Harrington JT, Barash HL, Day S, Lease J (2005) Redesigning the care of fragility fracture patients to improve osteoporosis management: a health care improvement project. Arthritis Rheum 53:198–204
Delmas PD, van de Langerijt L, Watts NB, Eastell R, Genant H, Grauer A, Cahall DL, Group IS (2005) Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res Off J Am Soc Bone Miner Res 20:557–563
Imai N, Endo N, Hoshino T, Suda K, Miyasaka D, Ito T (2014) Mortality after hip fracture with vertebral compression fracture is poor. J Bone Miner Metab
Sosa Henriquez M, Saavedra Santana P, grupo de trabajo en osteoporosis de la Sociedad Espanola de Medicina I (2007) Prevalence of vertebral fractures in hip fracture patients. Revista clinica espanola 207:464–468
Orimo H, Hayashi Y, Fukunaga M et al (2001) Gempatsusei kotusosyousyou no sindan kijun 2000 nendo kaitei ban (in Japanese). Nihon Kotsutaisya Gakkai Zasshi 14:76–82
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res Off J Am Soc Bone Miner Res 8:1137–1148
Johansson H, Oden A, McCloskey EV, Kanis JA (2014) Mild morphometric vertebral fractures predict vertebral fractures but not non-vertebral fractures. Osteoporos Int 25:235–241
Mitchell PJ (2013) Best practices in secondary fracture prevention: fracture liaison services. Current osteoporosis reports 11:52–60
Gallacher SJ, Gallagher AP, McQuillian C, Mitchell PJ, Dixon T (2007) The prevalence of vertebral fracture amongst patients presenting with non-vertebral fractures. Osteoporos Int 18:185–192
Howat I, Carty D, Harrison J, Fraser M, McLellan AR (2007) Vertebral fracture assessment in patients presenting with incident nonvertebral fractures. Clin Endocrinol 67:923–930
Siris ES, Genant HK, Laster AJ, Chen P, Misurski DA, Krege JH (2007) Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int 18:761–770
World Health Organization Collaborating Centre for Metabolic Bone Diseases University of Sheffield UK (2016) FRAX® WHO fracture risk assessment tool. http://www.shef.ac.uk/FRAX/ Accessed 10 May 2016
Osteoporosis Canada (2014) Quality Standards for Fracture Liaison Services in Canada. Osteoporosis Canada, Toronto
Osteoporosis New Zealand (2016) Clinical Standards for Fracture Liaison Services in New Zealand. Osteoporosis New Zealand, Wellington
British Orthopaedic Association, National Osteoporosis Society (2014) BOAST 9: Fracture Liaison Services. London
Gittoes N, McLellan AR, Cooper A et al (2015) Effective secondary prevention of fragility fractures: clinical standards for fracture liaison services. National Osteoporosis Society, Camerton
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C, IOF Fracture Working Group (2013) Capture the Fracture: a Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24:2135–2152
Javaid MK, Kyer C, Mitchell PJ et al (2015) Effective secondary fracture prevention: implementation of a global benchmarking of clinical quality using the IOF Capture the Fracture(R) Best Practice Framework tool. Osteoporos Int 26:2573–2578
International Osteoporosis Foundation (2016) Capture the Fracture® programme website. http://www.capture-the-fracture.org/ Accessed 1 April 2016
Mitchell PJ, Ganda K, Seibel MJ (2015) Australian and New Zealand bone and mineral society position paper on secondary fracture prevention programs. In press
Department of Health (2009) Falls and fractures: effective interventions in health and social care. In Department of Health (ed)
Osteoporosis New Zealand (2012) Bone Care 2020: a systematic approach to hip fracture care and prevention for New Zealand. Wellington
Mitchell PJ, Cornish J, Milsom S, et al. (2014) BoneCare 2020: a systematic approach to hip fracture care and prevention for New Zealand. 3rd Fragility Fracture Network Congress 2014 Madrid, Spain
van Staa TP, Dennison EM, Leufkens HG, Cooper C (2001) Epidemiology of fractures in England and Wales. Bone 29:517–522
Gauthier A, Kanis JA, Martin M, Compston J, Borgstrom F, Cooper C, McCloskey E, Committee of Scientific Advisors IOF (2011) Development and validation of a disease model for postmenopausal osteoporosis. Osteoporos Int 22:771–780
Cawston H, Maravic M, Fardellone P, Gauthier A, Kanis JA, Compston J, Borgstrom F, Cooper C, McCloskey E (2012) Epidemiological burden of postmenopausal osteoporosis in France from 2010 to 2020: estimations from a disease model. Arch Osteoporos 7:237–246
Gauthier A, Kanis JA, Jiang Y, Dreinhofer K, Martin M, Compston J, Borgstrom F, Cooper C, McCloskey E (2012) Burden of postmenopausal osteoporosis in Germany: estimations from a disease model. Arch Osteoporos 7:209–218
Piscitelli P, Brandi M, Cawston H, Gauthier A, Kanis JA, Compston J, Borgstrom F, Cooper C, McCloskey E (2014) Epidemiological burden of postmenopausal osteoporosis in Italy from 2010 to 2020: estimations from a disease model. Calcif Tissue Int 95:419–427
Gauthier A, Kanis JA, Jiang Y, Martin M, Compston JE, Borgström F, Cooper C, McCloskey EV (2011) Epidemiological burden of postmenopausal osteoporosis in the UK from 2010 to 2021: estimations from a disease model. Arch Osteoporos 6:179–188
Svedbom A, Hernlund E, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA, IOF EUrpot (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8:137
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Ebeling PR (2014) Osteoporosis in men: why change needs to happen. In: Mitchell PJ (ed) World Osteoporosis Day Thematic Report. International Osteoporosis Foundation, Nyons
Gerdhem P (2013) Osteoporosis and fragility fractures: vertebral fractures. Best Pract Res Clin Rheumatol 27:743–755
Bliuc D, Nguyen TV, Eisman JA, Center JR (2014) The impact of nonhip nonvertebral fractures in elderly women and men. J Clin Endocrinol Metab 99:415–423
Compston J, Bowring C, Cooper A et al (2013) Diagnosis and management of osteoporosis in postmenopausal women and older men in the UK: National Osteoporosis Guideline Group (NOGG) update 2013. Maturitas 75:392–396
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R, National Osteoporosis F (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381
Panday K, Gona A, Humphrey MB (2014) Medication-induced osteoporosis: screening and treatment strategies. Therapeutic advances in musculoskeletal disease 6:185–202
Bienz M, Saad F (2015) Androgen-deprivation therapy and bone loss in prostate cancer patients: a clinical review. Bonekey Rep 4:716
Tufano A, Coppola A, Contaldi P, Franchini M, Minno GD (2015) Oral anticoagulant drugs and the risk of osteoporosis: new anticoagulants better than old? Semin Thromb Hemost 41:382–388
Beerhorst K, van der Kruijs SJ, Verschuure P, Tan IY, Aldenkamp AP (2013) Bone disease during chronic antiepileptic drug therapy: general versus specific risk factors. J Neurol Sci 331:19–25
Rizzoli R, Body JJ, DeCensi A, Reginster JY, Piscitelli P, Brandi ML, European Society for C, Economical aspects of O, Osteoarthritis (2012) Guidance for the prevention of bone loss and fractures in postmenopausal women treated with aromatase inhibitors for breast cancer: an ESCEO position paper. Osteoporos Int 23:2567–2576
Lan GB, Xie XB, Peng LK, Liu L, Song L, Dai HL (2015) Current status of research on osteoporosis after solid organ transplantation: pathogenesis and management. Biomed Res Int 2015:413169
Whittier X, Saag KG (2016) Glucocorticoid-induced osteoporosis. Rheum Dis Clin N Am 42:177–189
Lopez LM, Grimes DA, Schulz KF, Curtis KM, Chen M (2014) Steroidal contraceptives: effect on bone fractures in women. The Cochrane database of systematic reviews 6:CD006033
Lau AN, Tomizza M, Wong-Pack M, Papaioannou A, Adachi JD (2015) The relationship between long-term proton pump inhibitor therapy and skeletal frailty. Endocrine 49:606–610
Rizzoli R, Cooper C, Reginster JY et al (2012) Antidepressant medications and osteoporosis. Bone 51:606–613
Palermo A, D’Onofrio L, Eastell R, Schwartz AV, Pozzilli P, Napoli N (2015) Oral anti-diabetic drugs and fracture risk, cut to the bone: safe or dangerous? A narrative review. Osteoporos Int 26:2073–2089
Canalis E, Mazziotti G, Giustina A, Bilezikian JP (2007) Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos Int 18:1319–1328
Albaum JM, Youn S, Levesque LE, Gershon AS, Cadarette SM (2014) Osteoporosis management among chronic glucocorticoid users: a systematic review. J Popul Ther Clin Pharmacol 21:e486–e504
Lekamwasam S, Adachi JD, Agnusdei D et al (2012) A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int 23:2257–2276
Newman ED, Matzko CK, Olenginski TP, Perruquet JL, Harrington TM, Maloney-Saxon G, Culp T, Wood GC (2006) Glucocorticoid-Induced Osteoporosis Program (GIOP): a novel, comprehensive, and highly successful care program with improved outcomes at 1 year. Osteoporos Int 17:1428–1434
Stangelberger A, Waldert M, Djavan B (2008) Prostate cancer in elderly men. Rev Urol 10:111–119
Zhumkhawala AA, Gleason JM, Cheetham TC, Niu F, Loo RK, Dell RM, Jacobsen SJ, Chien GW (2013) Osteoporosis management program decreases incidence of hip fracture in patients with prostate cancer receiving androgen deprivation therapy. Urology 81:1010–1015
Rizzoli R, Body JJ, Brandi ML et al (2013) Cancer-associated bone disease. Osteoporos Int 24:2929–2953
Coleman R, Body JJ, Aapro M, Hadji P, Herrstedt J, Group EGW (2014) Bone health in cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol 25(Suppl 3):iii124–iii137
Damji AN, Bies K, Alibhai SM, Jones JM (2015) Bone health management in men undergoing ADT: examining enablers and barriers to care. Osteoporos Int 26:951–959
International Osteoporosis Foundation (2013) The Asia-Pacific regional audit: epidemiology, costs and burden of osteoporosis in 2013. Nyon, Switzerland
Suarez-Almazor ME, Peddi P, Luo R, Nguyen HT, Elting LS (2014) Low rates of bone mineral density measurement in Medicare beneficiaries with prostate cancer initiating androgen deprivation therapy. Support Care Cancer 22:537–544
McGuire A, Brown JA, Malone C, McLaughlin R, Kerin MJ (2015) Effects of age on the detection and management of breast cancer. Cancers (Basel) 7:908–929
Dolan AL, Mohammed M, Thakur K (2007) Novel way to implement bone assessment guidelines to identify and manage patients receiving aromatase inhibitors using FITOS software. Osteoporos Int 18:S282–S283 Abstract P242A
Spangler L, Yu O, Loggers E, Boudreau DM (2013) Bone mineral density screening among women with a history of breast cancer treated with aromatase inhibitors. J Women’s Health (Larchmt) 22:132–140
Giusti F, Ottanelli S, Masi L, Amedei A, Brandi ML, Falchetti A (2011) Construction of a database for the evaluation and the clinical management of patients with breast cancer treated with antiestrogens and/or aromatase inhibitors. Clinical cases in mineral and bone metabolism: the official journal of the Italian Society of Osteoporosis, Mineral Metabolism, and Skeletal Diseases 8:37–50
International Diabetes Federation (2015) IDF diabetes atlas Seventh Edition. Brussels, Belgium
World Health Organization (2016) Chronic respiratory diseases: burden of COPD. http://www.who.int/respiratory/copd/burden/en/ Accessed 14 March 2016
Fasano A, Catassi C (2012) Clinical practice: Celiac disease. N Engl J Med 367:2419–2426
World IBD Day (2016) Inflammatory bowel disease: World IBD Day—19 May. http://worldibdday.org/ Accessed 15 March 2016
Alzheimer’s Disease International (2013) Policy brief for heads of government: the global impact of dementia 2013–2050. London, UK
Cross M, Smith E, Hoy D et al (2014) The global burden of rheumatoid arthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73:1316–1322
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes—a meta-analysis. Osteoporos Int 18:427–444
Janghorbani M, Van Dam RM, Willett WC, Hu FB (2007) Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 166:495–505
Graat-Verboom L, Wouters EF, Smeenk FW, van den Borne BE, Lunde R, Spruit MA (2009) Current status of research on osteoporosis in COPD: a systematic review. Eur Respir J 34:209–218
McEvoy CE, Ensrud KE, Bender E, Genant HK, Yu W, Griffith JM, Niewoehner DE (1998) Association between corticosteroid use and vertebral fractures in older men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 157:704–709
West J, Logan RF, Card TR, Smith C, Hubbard R (2003) Fracture risk in people with celiac disease: a population-based cohort study. Gastroenterology 125:429–436
Bernstein CN, Blanchard JF, Leslie W, Wajda A, Yu BN (2000) The incidence of fracture among patients with inflammatory bowel disease. A population-based cohort study. Ann Intern Med 133:795–799
Baker NL, Cook MN, Arrighi HM, Bullock R (2011) Hip fracture risk and subsequent mortality among Alzheimer’s disease patients in the United Kingdom, 1988-2007. Age Ageing 40:49–54
van Staa TP, Geusens P, Bijlsma JW, Leufkens HG, Cooper C (2006) Clinical assessment of the long-term risk of fracture in patients with rheumatoid arthritis. Arthritis Rheum 54:3104–3112
Regan EA, Radcliff TA, Henderson WG, Cowper Ripley DC, Maciejewski ML, Vogel WB, Hutt E (2013) Improving hip fractures outcomes for COPD patients. COPD 10:11–19
Kirchgatterer A, Wenzl HH, Aschl G, Hinterreiter M, Stadler B, Hinterleitner TA, Petritsch W, Knoflach P (2002) Examination, prevention and treatment of osteoporosis in patients with inflammatory bowel disease: recommendations and reality. Acta Med Austriaca 29:120–123
Etzel JP, Larson MF, Anawalt BD, Collins J, Dominitz JA (2011) Assessment and management of low bone density in inflammatory bowel disease and performance of professional society guidelines. Inflamm Bowel Dis 17:2122–2129
Knopp-Sihota JA, Cummings GG, Newburn-Cook CV, Homik J, Voaklander D (2014) Dementia diagnosis and osteoporosis treatment propensity: a population-based nested case-control study. Geriatr Gerontol Int 14:121–129
Caplan L, Hines AE, Williams E, Prochazka AV, Saag KG, Cunningham F, Hutt E (2011) An observational study of glucocorticoid-induced osteoporosis prophylaxis in a national cohort of male veterans with rheumatoid arthritis. Osteoporos Int 22:305–315
Romme EA, Geusens P, Lems WF, Rutten EP, Smeenk FW, van den Bergh JP, van Hal PT, Wouters EF (2015) Fracture prevention in COPD patients; a clinical 5-step approach. Respir Res 16:32
British Society of Gastroenterology (2007) Guidelines for osteoporosis in inflammatory bowel disease and coeliac disease
Duru N, van der Goes MC, Jacobs JW et al (2013) EULAR evidence-based and consensus-based recommendations on the management of medium to high-dose glucocorticoid therapy in rheumatic diseases. Ann Rheum Dis 72:1905–1913
Seeman E, Compston J, Adachi J, Brandi ML, Cooper C, Dawson-Hughes B, Jonsson B, Pols H, Cramer JA (2007) Non-compliance: the Achilles’ heel of anti-fracture efficacy. Osteoporos Int 18:711–719
Hiligsmann M, Salas M, Hughes DA, Manias E, Gwadry-Sridhar FH, Linck P, Cowell W (2013) Interventions to improve osteoporosis medication adherence and persistence: a systematic review and literature appraisal by the ISPOR Medication Adherence & Persistence Special Interest Group. Osteoporos Int 24:2907–2918
Boudou L, Gerbay B, Chopin F, Ollagnier E, Collet P, Thomas T (2011) Management of osteoporosis in fracture liaison service associated with long-term adherence to treatment. Osteoporos Int 22:2099–2106
Dehamchia-Rehailia N, Ursu D, Henry-Desailly I, Fardellone P, Paccou J (2014) Secondary prevention of osteoporotic fractures: evaluation of the Amiens University Hospital’s fracture liaison service between January 2010 and December 2011. Osteoporos Int 25:2409–2416
Ganda K, Schaffer A, Pearson S, Seibel MJ (2014) Compliance and persistence to oral bisphosphonate therapy following initiation within a secondary fracture prevention program: a randomised controlled trial of specialist vs. non-specialist management. Osteoporos Int 25:1345–1355
Feldstein AC, Schneider J, Smith DH, Vollmer WM, Rix M, Glauber H, Boardman DL, Herson M (2008) Harnessing stakeholder perspectives to improve the care of osteoporosis after a fracture. Osteoporos Int 19:1527–1540
Sujic R, Gignac MA, Cockerill R, Beaton DE (2013) Factors predictive of the perceived osteoporosis-fracture link in fragility fracture patients. Maturitas 76:179–184
Siris ES, Gehlbach S, Adachi JD et al (2011) Failure to perceive increased risk of fracture in women 55 years and older: the Global Longitudinal Study of Osteoporosis in Women (GLOW). Osteoporos Int 22:27–35
National Bone Health Alliance (2016) National Bone Health Alliance: Strong Bones America. http://www.nbha.org/ Accessed 16 June 2016
National Committee for Quality Assurance (2015) The State of Health Care Quality 2015. Washington D.C
Black DM, Rosen CJ (2016) Clinical practice: postmenopausal osteoporosis. N Engl J Med 374:254–262
Khan AA, Morrison A, Hanley DA et al (2015) Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res Off J Am Soc Bone Miner Res 30:3–23
Kim DH, Rogers JR, Fulchino LA, Kim CA, Solomon DH, Kim SC (2015) Bisphosphonates and risk of cardiovascular events: a meta-analysis. PLoS One 10:e0122646
Dell RM, Adams AL, Greene DF, Funahashi TT, Silverman SL, Eisemon EO, Zhou H, Burchette RJ, Ott SM (2012) Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res Off J Am Soc Bone Miner Res 27:2544–2550
Kim SC, Kim DH, Mogun H, Eddings W, Polinski JM, Franklin JM, Solomon DH (2016) Impact of the US food and drug administration’s safety-related announcements on the use of bisphosphonates after hip fracture. J Bone Miner Res Off J Am Soc Bone Miner Res
International Osteoporosis Foundation (2011) The Eastern European & Central Asian Regional Audit: epidemiology, costs & burden of osteoporosis in 2010
Kanis JA, Borgstrom F, Compston J, Dreinhofer K, Nolte E, Jonsson L, Lems WF, McCloskey EV, Rizzoli R, Stenmark J (2013) SCOPE: a scorecard for osteoporosis in Europe. Arch Osteoporos 8:144
Kanis JA, Johnell O (2005) Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int 16:229–238
International Osteoporosis Foundation (2012) The Latin America Regional Audit: epidemiology, costs & burden of osteoporosis in 2012. Nyon, Switzerland
International Osteoporosis Foundation (2011) The Middle East & Africa Regional Audit: epidemiology, costs & burden of osteoporosis in 2011
Osteoporosis Canada (2016) Essential elements of Fracture Liaison Services (FLS). http://www.osteoporosis.ca/fls/wp-content/uploads/Osteoporosis-Canada-Essential-Elements-of-an-FLS.pdf Accessed 6 May 2016
Cooper C, Mitchell P, Kanis JA (2011) Breaking the fragility fracture cycle. Osteoporos Int 22:2049–2050
Zerbini CA, Szejnfeld VL, Abergaria BH, McCloskey EV, Johansson H, Kanis JA (2015) Incidence of hip fracture in Brazil and the development of a FRAX model. Arch Osteoporos 10:224
Lesnyak O, Ershova O, Belova K et al (2012) Epidemiology of fracture in the Russian Federation and the development of a FRAX model. Arch Osteoporos 7:67–73
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
BD-H – none for this submission.
CC has received consultancy and honoraria from Alliance for Better Bone Health, Amgen, Eli Lilly, GSK, Medtronic, Merck, Novartis, Pfizer, Roche, Servier, Takeda and UCB.
DDP – none for this submission.
EVM has no disclosures related to this work, and has received consultancy fees, honoraria and/or research funding from Alliance for Better Bone Health, Amgen, AstraZeneca, Consilient Healthcare, GSK, Internis, Lilly, Merck, Pfizer, Servier, Synexus, Tethys, UCB, Warner Chilcott and Wyeth.
JAK and PJM have undertaken consultancy for governments, national osteoporosis societies, healthcare professional organisations and private sector companies relating to systematic approaches to fragility fracture care and prevention.
JYR has no disclosures related to this work, and has received consultancy, lecture fees and grant support from Amgen, Analis, Asahi Kasei, Boehringer, Bristol Myers Squibb, Chiltern, Danone, Ebewee Pharma, Endocyte, Galapagos, GlaxoSmithKline, IBSA-Genevrier, Lilly, Merck Sharp and Dohme, Merckle, Negma, Novartis, NovoNordisk, NPS, Nycomed-Takeda, Organon, Pfizer, PharmEvo, Radius Health, Roche, Rottapharm, Servier, Teijin, Teva, Theramex, Therabel, UCB, Will Pharma, Wyeth, Zodiac.
NCWH has no disclosures related to this work, and has received consultancy, lecture fees and honoraria from Alliance for Better Bone Health, AMGEN, MSD, Eli Lilly, Servier, Shire, Consilient Healthcare and Internis Pharma.
PJM serves as a consultant to the International Osteoporosis Foundation and received remuneration for his contribution to this manuscript.
RR has received honoraria for participation in Advisory boards or speaker bureau fees from Danone, Labatec, Nestlé, and ObsEva.
Additional information
Nicholas C. W. Harvey and Eugene V. McCloskey are joint first authors.
Rights and permissions
About this article
Cite this article
Harvey, N.C.W., McCloskey, E.V., Mitchell, P.J. et al. Mind the (treatment) gap: a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int 28, 1507–1529 (2017). https://doi.org/10.1007/s00198-016-3894-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3894-y