Abstract
Summary
In a 4-year follow-up study that enrolled 1099 subjects aged ≥60 years, sarcopenia prevalence was estimated at 8.2%. Moreover, the presence of osteoporosis was significantly associated with short-term sarcopenia occurrence, but the reciprocal relationship was not observed, suggesting that osteoporosis would increase the risk of osteoporotic fracture and sarcopenia occurrence.
Introduction
The present 4-year follow-up study was performed to clarify the prevalence, incidence, and relationships between sarcopenia (SP) and osteoporosis (OP) in older Japanese men and women.
Methods
We enrolled 1099 participants (aged, ≥60 years; 377 men) from the second survey of the Research on Osteoarthritis/Osteoporosis against Disability (ROAD) study (2008–2010) and followed them up for 4 years. Handgrip strength, gait speed, skeletal muscle mass, and bone mineral density were assessed. SP was defined according to the Asian Working Group for Sarcopenia. OP was defined based on the World Health Organization criteria.
Results
SP prevalence was 8.2% (men, 8.5%; women, 8.0%) in the second survey. In those with SP, 57.8% (21.9%; 77.6%) had OP at the lumbar spine L2–4 and/or femoral neck. SP cumulative incidence was 2.0%/year (2.2%/year; 1.9%/year). Multivariate regression analysis revealed that OP was significantly associated with SP occurrence within 4 years (odds ratio, 2.99; 95% confidence interval, 1.46–6.12; p < 0.01), but the reciprocal relationship was not significantly observed (2.11; 0.59–7.59; p = 0.25).
Conclusions
OP might raise the short-term risk of SP incidence. Therefore, OP would not only increase the risk for osteoporotic fracture but may also increase the risk for SP occurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the average age of the human population increases, there is an urgent need to develop strategies to prevent musculoskeletal disorders, which can impair activities of daily life (ADL) and quality of life (QOL) in the elderly. Sarcopenia (SP) and osteoporosis (OP) are major musculoskeletal diseases that impair ADL and QOL, leading to increased morbidity and mortality rates in the elderly. The recent National Livelihood Survey performed by the Ministry of Health, Labour, and Welfare in Japan [1] found that falls and osteoporotic fractures are ranked fourth, and frailty, to which muscle weakness and low physical performance contribute largely, was ranked third among the causes of disabilities requiring support and long-term care. Therefore, developing approaches to prevent SP and OP could reduce ADL and QOL impairments and subsequent disabilities among the elderly.
In the elderly, SP is characterized by generalized loss of skeletal muscle mass and muscle strength and/or function, causing multiple adverse health outcomes, including physical disability, poor QOL, and death [2–7]. Although cross-sectional studies have investigated SP prevalence [8–14], the epidemiologic evidence of population-based samples remained insufficient. This might be because a widely accepted definition of SP was not established until the European Working Group on Sarcopenia in Older People (EWGSOP) developed a practical clinical definition and diagnostic criteria in 2010 [5]. There is a growing consensus that SP should not be defined based on muscle mass alone but also on muscle strength and function [5]. After publication of the EWGSOP consensus criteria, the Asian Working Group for Sarcopenia (AWGS) announced the appropriate diagnostic cutoff values for Asian populations [15]. In the AWGS consensus report, the reasons for creating different cutoff values from the European criteria were stated as follows: although the recommended approaches for measurements of muscle mass, muscle strength, and physical performance by AWGS were similar to the EWGSOP definition, the cutoff values of these measurements in Asian populations may differ from those in Caucasians because of ethnicities, body size, lifestyles, and cultural backgrounds. Therefore, developing an Asian consensus for sarcopenia diagnosis based on the evidence derived from Asian populations is essential for research and therapeutic approaches to sarcopenia in Asia [15]. This definition is now used widely for the assessment of SP in Asian countries.
The Research on Osteoarthritis/Osteoporosis Against Disability (ROAD) study is a prospective cohort study aimed at elucidating the environmental and genetic background of musculoskeletal diseases [16, 17]. The baseline data and that from the second survey of the ROAD study provided information on the prevalence and incidence of OP at the lumbar spine L2–4 and proximal femur [17, 18]. Furthermore, the prevalence of SP was evaluated using the EWGSOP definition in the second ROAD survey, giving an estimated prevalence in the general Japanese population of 13.8% in men and 12.4% in women [19]. The same study revealed that SP prevalence increased in an age-dependent manner in both sexes [19]. However, the SP incidence according to the AWGS criteria has not been investigated. Furthermore, the relationships of SP with other musculoskeletal diseases, especially OP, have not been determined, and it is not clear whether SP causes OP development, OP causes SP development, the conditions are comorbid, or if SP and OP represent concomitant modifications of one another.
In the present study, we completed the third ROAD study survey, a 4-year follow-up in which examinations identical to those in the second ROAD study survey were conducted. The aims of the present study were to clarify SP prevalence and incidence using the AWGS criteria, determine the co-existing proportions of SP and OP, and evaluate whether there was a significant contribution of SP to subsequent OP development, or vice versa, in elderly Japanese subjects.
Methods
Study participants
The present study was performed using the ROAD study cohorts that were established in 2005. The ROAD study is a national, prospective study of osteoarthritis that consists of population-based cohorts from several communities in Japan. Details of the cohort profiles have been reported elsewhere [16, 17]. In brief, between 2005 and 2007, a baseline database was created that included clinical and genetic information for 3040 residents (1061 men and 1979 women with a mean age of 70.3 (standard deviation [SD], 11.0) years; 71.0 (10.7) years in men, 69.9 (11.2) years in women). The subjects were recruited from resident registration listings in 3 communities with different characteristics: 1350 subjects from an urban region in Itabashi, Tokyo; 864 subjects from a mountainous region in Hidakagawa, Wakayama; and 826 subjects from a coastal region in Taiji, Wakayama.
After the baseline study, a second survey was performed in the same communities from 2008 to 2010 [20], and the third survey was followed from 2012 to 2013. In the second and third surveys, in addition to the OP assessment, examinations for the diagnosis of SP, including measurements such as gait speed, grip strength, and skeletal muscle mass were initiated in mountainous and coastal regions. In the present study, among the 1551 participants (521 men and 1030 women) in the second survey from mountainous and coastal regions who underwent all measurements for SP and OP, those aged ≥60 years were selected based on the AWGS criteria for SP [15]. As a result, 1099 (377 men and 722 women; mean age, 72.1 (7.4) years [72.7 (7.5) years in men, 71.8 (7.4) years in women]) participants were recruited as eligible subjects. A flow chart of subjects’ recruitment and follow-up with reasons for dropout is shown in Fig. 1. The data obtained from these 1099 subjects was used to clarify mutual associations between SP and OP.
Examinations performed during the second ROAD study survey
Interviewer-administered questionnaire
Participants completed an interviewer-administered questionnaire that consisted of 200 questions related to lifestyle including occupation, smoking habits, alcohol consumption, family history, medical history, physical activity, reproductive history, and health-related QOL.
Anthropometric measurements and medical history
Anthropometric measurements, including height and weight, were measured in all participants. Body mass index (BMI; weight [kg]/height [m2]) was calculated as weight in kilograms divided by height in meters squared. Experienced orthopedic surgeons collected medical information about pain, swelling, and the range of motion of the knee.
Skeletal muscle mass
Skeletal muscle mass was measured by bioimpedance analysis [21–25] using the Body Composition Analyzer MC-190 (Tanita Corp., Tokyo, Japan). The protocol was described by Tanimoto et al. [11, 13] and has been validated previously [26]. Appendicular skeletal muscle mass (ASM) was calculated as the sum of the muscle mass of the arms and legs. Absolute ASM was converted to an appendicular muscle mass index by dividing by height in meters squared (kg/m2).
Muscle strength and walking speed
Handgrip strength was measured using a Toei Light handgrip dynamometer (Toei Light Co. Ltd., Saitama, Japan) to assess muscle strength. Both hands were tested and the largest value used to determine the maximum muscle strength. The usual walking speed was measured as an index of physical performance. The time taken (s) to walk 6 m at normal walking speed was recorded, and the usual gait speed was calculated.
BMD examination
Lumbar spine and proximal femur bone mineral density (BMD) values were determined using dual-energy X-ray absorptiometry (DXA; Hologic Discovery C; Hologic, Waltham, MA). To control DXA precision, the equipment was checked at every examination during the second and third surveys using the same phantom. The BMD of the phantom was regulated to within ±1.5% during all examinations. In addition, the same physician (N.Y.) examined all participants to control observer variability. Intraobserver variability of DXA using the Lunar DPX in vitro and in vivo had been measured by the same physician (N.Y.) in another study [27], and the coefficient of variance for L2–4 in vitro was 0.35%. The coefficients of variance for L2–4, the proximal femur, Ward’s triangle, and the trochanter as examined in vivo in five male volunteers were 0.61–0.90, 1.02–2.57, 1.97–5.45, and 1.77–4.17%, respectively.
Definition of SP and OP
SP was determined according to the criteria defined by the AWGS [15]. AWGS criteria were as follows: (A) age ≥60 or ≥65 years; (B) low appendicular skeletal muscle mass, 7.0 kg/m2 for men and 5.7 kg/m2 for women, according to bioimpedance analysis; (C) low handgrip strength, <26 kg in men and <18 kg in women; and (D) low gait speed, with usual gait speed being ≤0.8 m/s. Subjects were diagnosed as having SP if they had criteria A and B and either of criteria C or D. Regarding age definition using the AWGS criteria, because of the different states of aging in Asia, not all countries use the same cutoff age to define elderly populations. Therefore, the AWGS recommends using either 60 or 65 years as the age for SP. In the present study, we defined subjects aged ≥60 years as potential subjects for SP.
In the present study, OP was defined according to the values of BMD. The World Health Organization criteria were used when BMD T-scores were lower than the peak bone mass by 2.5 SDs [28]. In Japan, the mean L2–4 BMD in young adults, as measured using the Hologic DXA, was 1.011 (0.119) g/cm2 [29]. Therefore, lumbar spine osteoporosis was defined as an L2–4 BMD of <0.714 g/cm2. In Japan, the mean femoral neck BMDs in young adult males and females are 0.863 (0.127) and 0.787 (0.109) g/cm2, respectively [28]. Therefore, OP at the femoral neck was defined as a BMD of <0.546 and <0.515 g/cm2 for men and women, respectively.
Incidence of SP and OP
The cumulative incidences of SP and OP were determined based on changes in measurements between the second and third surveys. New cases of SP or OP were defined as when an individual did not meet criteria for SP or OP at the second survey but did meet them at the third survey.
Statistical analyses
All statistical analyses were performed using STATA statistical software (STATA Corp., College Station, TX). Differences in proportions were compared using the chi-square test. Differences in continuous variables were tested for significance using analysis of variance for comparisons among multiple groups or Scheffe’s least significant difference test for group pairs.
Logistic regression analysis was used to test the association between the presence of SP and OP occurrence. OP occurrence was used as the objective variable, and the presence of SP (1: yes, 0: no) was used as the explanatory variable, after adjusting for age (years), sex (0: men, 1: women), and unconfirmed confounding factors. A second logistic regression analysis was conducted by replacing the objective and explanatory variables in the model mentioned above with SP occurrence and the presence of OP (1: yes, 0: no), respectively. The unconfirmed risk factors used for adjustment in the multivariate logistic analysis included residing area (0: mountainous area, 1: coastal area), emaciated stature (BMI <18.5 kg/m2; [0: no, 1: yes]), current smoking habit (0: ex or never smoker, 1: current smoker), and alcohol consumption habit (0: ex or never drinker, 1: current drinker).
Results
SP prevalence
SP prevalence according to age group stratifications of 60–64, 65–69, 70–74, 75–79, and ≥80 years were 0.5, 0.0, 4.3, 11.2, and 27.0%, respectively (men, 1.5, 0.0, 4.7, 11.5, and 23.9%, for 60–64, 65–69, 70–74, 75–79, and ≥80 years, respectively; women, 0.0, 0.0, 4.1, 10.9, and 28.7%, for 60–64, 65–69, 70–74, 75–79, and ≥80 years, respectively). Above the age of 70 years, SP prevalence increased in an age-dependent manner, but there was no significant difference in prevalence according to sex.
OP prevalence
OP prevalence estimates were conducted on 1097 participants (376 men, 721 women) because the BMD at the spine L2–4 or femoral neck could not be measured in 2 individuals (1 man, 1 woman). OP prevalence according to age group stratifications of 60–64, 65–69, 70–74, 75–79, and ≥80 years were 10.8, 18.0, 19.5, 34.0, and 44.0%, respectively (men, 1.5, 1.5, 4.7, 13.8, and 11.3%, for 60–64, 65–69, 70–74, 75–79, and ≥80 years, respectively; women, 15.4, 24.8, 26.9, 47.7, and 62.0%, for 60–64, 65–69, 70–74, 75–79, and ≥80 years, respectively). OP prevalence increased in an age-dependent manner in women and was significantly higher in each age strata in women compared with that in men.
SP and OP co-existence
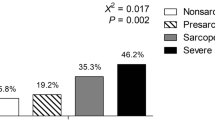
In the population aged ≥60 years, SP and OP co-existence was observed in 4.7%, SP alone was present in 3.5%, OP alone was noted in 20.2%, and 71.7% had neither SP nor OP.
In men, the prevalences of co-existing SP and OP, SP alone, OP alone, and neither SP nor OP were 1.9, 6.7, 5.1, and 86.4%, respectively, and in women, those were 6.2, 1.8, 28.0, and 63.9%, respectively. The difference in distribution in prevalences between men and women was most significant for OP. That is, prevalences of the co-existence of SP and OP and OP alone were significantly higher in women compared with men (p < 0.001).
Associated factors classified by the presence or absence of SP or OP
Table 1 shows a comparison of background characteristics for those with and without SP. Among subjects with SP, 57.8% had a concomitant diagnosis of OP, which was a significantly higher proportion than those without SP (22.0%, p < 0.001). Similarly, in those with OP, 19.1% had a concomitant diagnosis of SP, which was a significantly greater proportion than those without OP (4.6%, p < 0.001).
Diagnostic SP values such as grip strength and usual walking speed were significantly lower in the subjects with OP (p < 0.001). In addition, OP diagnostic values such as lumbar spine L2–4 and femoral neck BMD were significantly lower in the subjects with SP (p < 0.0001). Age and smaller stature were both significantly associated with SP and OP. Residing region was significantly associated with SP (p = 0.005). Being female and drinking and smoking less were significantly associated with OP (Table 1).
Table 2 (A), (B) shows the mutual associations between the presence of SP and OP at the lumbar spine L2–4 and/or the femoral neck. After adjustment for potential confounding factors mentioned above, logistic regression analysis revealed that the presence of OP was significantly associated with SP presence (odds ratio, 2.86; 95% confidence interval, 1.59–5.13; p < 0.001; Table 2 (A)). Furthermore, the presence of SP was significantly associated with OP presence (odds ratio, 2.78; 95% confidence interval, 1.55–4.99; p < 0.001; Table 2 (B)).
Participants in both the second and third surveys
Among 1099 participants in the second survey who were aged ≥60 years at the assessment of SP, 865 individuals (78.7%, 289 men, 576 women) attended the third survey performed 4 years later. Therefore, 234 individuals (21.3%; 88 men, 146 women) dropped out in the third survey. The reasons for dropout are shown in Fig. 1. Among the 865 participants in both the second and third surveys, 98 (11.3%, 36 men, 62 women) did not have complete measurements for the diagnosis of SP and OP. Therefore, the data from 767 completers (69.8%, 253 men, 514 women) was used in the present study to assess the contribution of OP to the occurrence of SP, and vice versa.
Cumulative incidence of SP
Among 767 completers (253 men, 514 women) of the third survey of the ROAD study, 32 subjects (9 men and 23 women) were diagnosed with SP at the second survey. Therefore, the number of population at risk for SP occurrence was 735 (244 men, 491 women). The cumulative incidence of SP during the 4-year period between the surveys was 2.0%/year (men, 2.2%/year; women, 1.9%/year). Figure 2 shows the age-sex classified SP incidence. The cumulative SP incidences for the at-risk populations according to age group were 0.4, 0.5, 1.5, 4.2, and 6.9%/year for 60–64, 65–69, 70–74, 75–79, and ≥80 years, respectively. The incidence increased in an age-dependent fashion (p < 0.001 for all subjects, p = 0.005 for men, and p < 0.001 for women), but there was no significant difference in incidence according to sex (p = 0.61) (Fig. 2).
Cumulative incidence of OP
Among 767 completers (253 men, 514 women), 2 male subjects were excluded from the assessment of OP incidence at the third survey because their BMD measurements for both lumbar spine L2–4 and femoral neck could not be performed. Among the remaining 765 subjects (251 men, 514 women), 90 (2 men and 88 women) were diagnosed with OP at both the lumbar spine L2–4 and femoral neck at the second survey. Therefore, in the present study, the population at risk for OP at the lumbar spine L2–4 and/or femoral neck was 675 subjects (249 men, 426 women). The cumulative OP incidence during the 4-year period between the surveys was 1.9%/year (men, 0.8%/year; women, 2.5%/year). The cumulative OP incidences for the at-risk populations according to age group were 1.1, 2.3, 2.1, 1.7, and 2.7%/year for 60–64, 65–69, 70–74, 75–79, and ≥80 years, respectively (men, 1.0, 1.0, 0.9, 0.0, and 1.5%/year, for 60–64, 65–69, 70–74, 75–79, and ≥80 years, respectively; women, 1.1, 2.9, 2.8, 3.0, and 4.0%/year, for 60–64, 65–69, 70–74, 75–79, and ≥80 years, respectively.) OP incidence was not associated with age (p = 0.38 for total subjects, p = 0.60 for men, p = 0.23 for women), and it was significantly higher in women compared with that in men (p = 0.001).
Assessment of contribution of OP to the subsequent occurrence of SP, and vice versa
Table 3 shows the comparison of the background characteristics according to the occurrence or non-occurrence of SP during the 4-year follow-up. Among subjects without SP at the second survey, in addition to higher age, lower height, lower weight, and residing in a mountainous area, the presence of OP was significantly associated with future SP development (p < 0.001).
Table 3 also shows the comparison of the background characteristics according to the occurrence or non-occurrence of OP during the 4-year follow-up. In addition to female sex, lower height, lower weight, emaciation, and residing in a mountainous area, the presence of SP was significantly associated with the future incidence of OP (p = 0.043).
After adjustment for the potential confounding factors such as, age, sex, regional difference, emaciation (BMI < 18.5 kg/m2), smoking habit, and alcohol drinking habit, logistic regression analysis revealed that the presence of OP was a significant predictive factor for SP occurrence in the near future (odds ratio, 2.99; 95% confidence interval, 1.46–6.12; p = 0.003; Table 4 (A)). This tendency was shown for both men and women when the logistic analysis was performed using identical adjustment factors except for sex; although, the association in men was diluted (men: odds ratio 6.92, 95% confidence interval 0.86–55.66, p = 0.069; women: odds ratio 2.58, 95% confidence interval 1.16–5.73, p = 0.020).
By contrast, the logistic regression analysis revealed that the presence of SP was no longer a significant predictive factor for OP occurrence in the near future (odds ratio, 2.11; 95% confidence interval, 0.59–7.59; p = 0.253; Table 4 (B)).
Discussion
In the present study, using information from the second and third surveys of the population-based ROAD cohort, we clarified the prevalence and characteristics of SP in Japan. We found that the prevalence of SP was significantly higher in those with OP compared to in those without OP. In addition, the prevalence of OP was significantly higher in those with SP compared to in those without SP. In the 4-year follow-up between the surveys, we estimated the SP incidence and found that the presence of OP significantly increased the future risk of SP, but the presence of SP did not increase the future risk of OP.
In the present study, SP prevalence was estimated using the AWGS definition because previous prevalence estimates on this cohort were conducted before the publication of the AWGS definitions [19]. The previous prevalences were higher compared with those noted in the present study, which is most likely because of the differences in cutoff values between the EWGSOP and AWGS definition criteria. According to the EWGSOP criteria, low handgrip strength was defined as <30 kg in men and <20 kg in women [5], whereas those for the AWGS definition are <26 and <18 kg, respectively. However, because all of the participants in the ROAD study were Japanese, we decided that the AWGS criteria would better reflect the SP prevalence of the cohort.
Besides previous reports using the EWGSOP definition [19], few studies have estimated the SP prevalence in the Japanese population. Applying the SP prevalence rate obtained in subjects aged ≥60 years in the present study (8.2%) to the Japanese 2010 census data [30] would indicate that in Japan, approximately 3,700,000 people (1,200,000 men and 2,500,000 women) aged ≥60 years might be affected by SP. Furthermore, in the present report, the degree of co-existence of SP and OP in those aged ≥60 years was clarified. The majority of patients with SP had OP, but patients with OP did not always have SP. Therefore, individuals with SP should be assessed for the potential co-existence of OP. Furthermore, not only was the presence of OP associated with the presence of SP, and vice versa, but also subjects with SP tended to have low BMD, whereas those with OP tended to have low physical performance and low muscle mass. Therefore, not only prevalence but also elements assessed for the diagnosis of SP and OP showed significant associations.
Regarding stature, emaciation is a well-known feature of OP. In a meta-analysis of prospective cohorts from >25 countries, including baseline BMI data from 398,610 women with an average age of 63 years and a follow-up of 2.2 million person-years, Johansson et al. reported that a high BMI was a protective factor for most fragility fracture sites [31]. Moreover, we reported previously that fast bone losers have significantly lighter body composition compared with healthy subjects [32]. However, regarding SP, despite consideration of sarcopenic obesity [33, 34], the association of emaciation and SP has received little attention. In the present study, emaciation was significantly associated with both OP and SP. Additionally, in the present study, none of the individuals with SP were obese (BMI >27.5 kg/m2). In an overview of sarcopenic obesity, Cauley stated that obesity was usually defined by a high BMI, but some studies have relied on percentage body or visceral fat [35]. The findings of the present study suggest that high BMI might not be associated with the existence of SP. The definition of sarcopenic obesity should be incorporated from the view of the prevention of severe health illness of the elderly, such as cardiovascular diseases.
Regarding SP incidence, few reports have estimated SP incidence in not only Japan but also worldwide. In the present study, the cumulative SP incidence in Japanese subjects aged ≥60 years was 2.0%/year. Using the age-sex SP incidence against the Japanese 2010 census data [31], this suggests that approximately 1,050,000 people (350,000 men and 700,000 women) aged ≥60 years become newly affected by SP each year. The cumulative SP incidence increased with age, but there were no significant differences in the SP prevalence or incidence rates according to sex.
We reported the cumulative OP incidence previously, using the 3-year follow-up data from the baseline to second ROAD study surveys [36]. In that study, we estimated that the annual cumulative OP incidences were 0.76%/year at the lumbar spine and 1.83%/year at the femoral neck. In the present study, the annual OP incidence of subjects aged ≥60 years, between the second and third surveys, was estimated to clarify any associations with SP. The incidence of lumbar spine L2–4 OP in female subjects aged ≥60 years who participated in the baseline to the second survey [35] was compared with that in the present study (1.06 vs. 0.84%/year, respectively; p < 0.01; data not published). Similarly, the incidence of femoral neck OP in female subjects between these studies was significantly lower between the second and third surveys (2.49 vs. 1.87%/year, respectively; p < 0.001; data not published). We did not compare the OP incidence in men because the numbers were too low to provide statistical power for a comparison. This comparison shows that the OP incidence rate in women might be decreasing, although the reasons for this are unknown. Observation of the ROAD cohort is ongoing, and changes in incidence rates will be clarified after completion of the 10-year follow-up.
Finally, the logistic regression analysis revealed that the presence of OP significantly increased the risk of SP occurrence within 4 years. By contrast, the presence of SP did not predict OP occurrence within 4 years. However, as we noted, there was a significant proportion of patients with co-existent SP and OP (so-called ‘osteosarcopenia’), suggesting that individuals with SP should be assessed for the presence of OP.
There are several limitations to the present study. First, although the ROAD study includes a large number of participants, the participants in the present study (second survey, individuals from the mountainous and coastal regions only) may not be completely representative of the general population. To address this issue, we compared the anthropometric measurements between the present study participants and the general Japanese population. The values for the general population were obtained from the report on the 2008 National Health and Nutrition Survey conducted by the Ministry of Health, Labour, and Welfare, Japan [37] when the second ROAD survey began. For mean BMI, there were no significant differences between the second ROAD survey participants and the Japanese general population. In addition, among lifestyle factors, the proportion of current smokers and drinkers (those who regularly drink more than one drink/month) in the Japanese general population was compared with that in the present study population. The proportion of current smokers was lower in males in the present study population compared with the general Japanese population, but there was no significant difference in the number of female smokers (men, 19.1 vs. 25.6%, p < 0.01; women, 3.1 vs. 4.0%, p = 0.28). Moreover, the proportion of current drinkers was significantly lower in both men and women in our study population compared with the general Japanese population (men, 58.9 vs. 64.7%, p < 0.05; women, 16.0 vs. 21.0%, p < 0.01), suggesting that compared to the general Japanese population, the participants of the present study lead healthier lifestyles, at least in terms of smoking habits. This selection bias should be taken into consideration when generalizing the results obtained from the present study. Second, in the present study, handgrip strength, and 6-m walking tests were measured only once. Therefore, we could not exclude the effect of incidental changes in participants’ performance around the examination date. Recurrent measurements should be taken into consideration to minimize fluctuation of measurements. However, we confirmed that none of the participants harbored hand or knee injuries that could have affected the measurements. Third, in the present study, OP was defined by BMD values using DXA alone. We might have to include participants who started medication for OP and/or those who developed new fractures. Although we had information regarding the medication and history of fractures, they were obtained from the self-report questionnaire leading to the possibility of recall bias. Therefore, in the present study, the incidence of OP might be underestimated. After the confirmation of medication by the interviewer, and assessment of fractures diagnosed by radiographic examinations performed in the ROAD study, the cumulative incidence of OP should be revised. Finally, the 4-year follow-up period might be too short to determine the causal relationship between SP and OP. Only a small number of new OP and SP cases occurred during the 4-year observation period. However, the ROAD study continues, so determining the occurrence of OP and SP over an extended period will be possible in the future, enabling the validation of the causal relationship between SP and OP using the incidence rate, rather than cumulative incidence as an epidemiological index.
In conclusion, the prevalence of co-existing SP and OP were high, suggesting that subjects ≥60 years with SP should be assessed for concomitant OP. Moreover, the presence of OP was significantly associated with SP occurrence within 4 years. Therefore, treatment for OP might not only have clinical benefit for the treatment of OP itself but might also reduce the risk of subsequent SP development.
References
Ministry of Health, Labour and Welfare. The outline of the results of the National Livelihood Survey (2013) available at http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa13/dl/16.pdf [in Japanese]
Rosenberg I (1989) Summary comments: epidemiological and methodological problems in determining nutritional status of older persons. Am J Clin Nutr 50:1231–1233
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127(5 Suppl):990S–991S
Morley JE, Baumgartner RN, Roubenoff R, Mayer J, Nair KS (2001) Sarcopenia. J Lab Clin Med 137:231–243
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkova E, Vandewoude M, Zamboni M, European Working Group on Sarcopenia in Older People (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 39:412–423. doi:10.1093/ageing/afq034
Delmonico MJ, Harris TB, Lee JS, Visser M, Nevitt M, Kritchevsky SB, Tylavsky FA, Newman AB, Health, Aging and Body Composition Study (2007) Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc 55:769–774
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, Simonsick EM, Tylavsky FA, Visser M, Newman AB (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 61:1059–1064
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763
Melton LJ III, Khosla S, Crowson CS, O’Connor MK, O’Fallon WM, Riggs BL (2000) Epidemiology of sarcopenia. J Am Geriatr Soc 48:625–630
Iannuzzi-Sucich M, Prestwood KM, Kenny AM (2002) Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women. J Gerontol A Biol Sci Med Sci 57:M772–M777
Tanimoto Y, Watanabe M, Sun W, Sugiura Y, Tsuda Y, Kimura M, Hayashida I, Kusabiraki T, Kono K (2012) Association between sarcopenia and higher-level functional capacity in daily living in community-dwelling elderly subjects in Japan. Arch Gerontol Geriatr 55:e9–e13
Patel HP, Syddall HE, Jameson K, Robinson S, Denison H, Roberts HC, Edwards M, Dennison E, Cooper C, Aihie Sayer A (2013) Prevalence of sarcopenia in community-dwelling older people in the UK using the European Working Group on Sarcopenia in Older People (EWGSOP) definition: findings from the Hertfordshire Cohort Study (HCS). Age Ageing 42:378–384. doi:10.1093/ageing/afs197
Tanimoto Y, Watanabe M, Sun W, Tanimoto K, Shishikura K, Sugiura Y, Kusabiraki T, Kono K (2013) Association of sarcopenia with functional decline in community-dwelling elderly subjects in Japan. Geriatr Gerontol Int 13:958–963. doi:10.1111/ggi.12037
Lin CC, Lin WY, Meng NH, Li CI, Liu CS, Lin CH, Chang CK, Lee YD, Lee CC, Li TC (2013) Sarcopenia prevalence and associated factors in an elderly Taiwanese metropolitan population. J Am Geriatr Soc 61:459–462. doi:10.1111/jgs.12129
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O, Lee JS, Lee WJ, Lee Y, Liang CK, Limpawattana P, Lin CS, Peng LN, Satake S, Suzuki T, Won CW, Wu CH, Wu SN, Zhang T, Zeng P, Akishita M, Arai H (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 15:95–101. doi:10.1016/j.jamda.2013.11.025
Yoshimura N, Muraki S, Oka H, Kawaguchi H, Nakamura K, Akune T (2010) Cohort profile: research on osteoarthritis/osteoporosis against disability study. Int J Epidemiol 39:988–995. doi:10.1093/ije/dyp276
Yoshimura N, Muraki S, Oka H, Mabuchi A, En-Yo Y, Yoshida M, Saika A, Yoshida H, Suzuki T, Yamamoto S, Ishibashi H, Kawaguchi H, Nakamura K, Akune T (2009) Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J Bone Miner Metab 27:620–628. doi:10.1007/s00774-009-0080-8
Yoshimura N, Muraki S, Oka H, Nakamura K, Kawaguchi H, Tanaka S, Akune T (2015) Serum levels of 25-hydroxyvitamin D and the occurrence of musculoskeletal diseases: a 3-year follow-up to the road study. Osteoporos Int 26:151–161. doi:10.1007/s00198-014-2844-9
Akune T, Muraki S, Oka H, Tanaka S, Kawaguchi H, Nakamura K, Yoshimura N (2014) Exercise habits during middle age are associated with lower prevalence of sarcopenia: the ROAD study. Osteoporos Int 25:1081–1088. doi:10.1007/s00198-013-2550-z
Yoshimura N, Oka H, Muraki S, Akune T, Hirabayashi N, Matsuda S, Nojiri T, Hatanaka K, Ishimoto Y, Nagata K, Yoshida M, Tokimura F, Kawaguchi H, Nakamura K (2011) Reference values for hand grip strength, muscle mass, walking time, and one-leg standing time as indices for locomotive syndrome and associated disability: the second survey of the ROAD study. J Orthop Sci 16:768–777. doi:10.1007/s00776-011-0160-1
No authors listed (1996) Bioelectrical impedance analysis in body composition measurement: National Institutes of Health Technology Assessment Conference Statement. Am J Clin Nutr 64(3 Suppl):524S–532S
Janssen I, Heymsfield SB, Baumgartner RN, Ross, R (2000) Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol (1985) 89:465–471
Kyle UG, Genton L, Slosman DO, Pichard C (2001) Fat-free and fat mass percentiles in 5225 healthy subjects aged 15 to 98 years. Nutrition 17:534–541
Kyle UG, Genton L, Karsegard L, Slosman DO, Pichard C (2001) Single prediction equation for bioelectrical impedance analysis in adults aged 20–94 years. Nutrition 17:248–253
Roubenoff R, Baumgartner RN, Harris TB, Dallal GE, Hannan MT, Economos CD, Stauber PM, Wilson PW, Kiel DP (1997) Application of bioelectrical impedance analysis to elderly populations. J Gerontol A Biol Sci Med Sci 52:M129–M136
Nemoto M, Yasbushita N, Kim M, Tomoaki M, Satoshi S, Jung S, Hiroyuki S, Kiyoji T (2012) Validity of the bioelectrical impedance method for assessing body composition in non-frail and pre-frail older adults. Int J Body Comps Res 10:225–262
Yoshimura N, Kakimoto T, Nishioka M, Kishi T, Iwasaki H, Niwa T, Morioka S, Sakata T, Hashimoto T (1997) Evaluation of reproducibility of bone mineral density measured by dual energy X-ray absorptiometry (Lunar DPX-L). J Wakayama Medical Society 48:461–466
World Health Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. In: WHO Technical Report Series 843. WHO, Geneva
Orimo H, Hayashi Y, Fukunaga M, Sone T, Fujiwara S, Shiraki M, Kushida K, Miyamoto S, Soen S, Nishimura J, Oh-Hashi Y, Hosoi T, Gorai I, Tanaka H, Igai T, Kishimoto H, Osteoporosis Diagnostic Criteria Review Committee: Japanese Society for Bone and Mineral Research (2001) Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab 19:331–337
Portal site of Official Statistics of Japan (2010) Population Census 2010 available at http://www.e-stat.go.jp/SG1/estat/GL08020103.do?_toGL08020103_&tclassID=000001034991&cycleCode=0&requestSender=search [In Japanese]
Johansson H, Kanis JA, Odén A, McCloskey E, Chapurlat RD, Christiansen C, Cummings SR, Diez-Perez A, Eisman JA, Fujiwara S, Glüer CC, Goltzman D, Hans D, Khaw KT, Krieg MA, Kröger H, LaCroix AZ, Lau E, Leslie WD, Mellström D, Melton LJ 3rd, O’Neill TW, Pasco JA, Prior JC, Reid DM, Rivadeneira F, van Staa T, Yoshimura N, Zillikens MC (2014) A meta-analysis of the association of fracture risk and body mass index in women. J Bone Miner Res 29:223–233. doi:10.1002/jbmr.2017
Yoshimura N, Takijiri T, Kinoshita H, Danjoh S, Kasamatsu T, Morioka S, Sakata K, Hashimoto T, Takeshita T (2004) Characteristics and course of bone mineral densities among fast bone losers in a rural Japanese community: the Miyama study. Osteoporos Int 15:139–144
Kohara K (2014) Sarcopenic obesity in aging population: current status and future directions for research. Endocrine 45:15–25
Vincent HK, Raiser SN, Vincent KR (2012) The aging musculoskeletal system and obesity-related considerations with exercise. Ageing Res Rev 11:361–373. doi:10.1016/j.arr.2012.03.002
Cauley JA (2015) An overview of sarcopenic obesity. J Clin Densitom 18:499–505. doi:10.1016/j.jocd.2015.04.013
Yoshimura N, Muraki S, Oka H, Nakamura K, Kawaguchi H, Tanaka S, Akune T (2015) Serum levels of 25-hydroxyvitamin D and occurrence of musculoskeletal diseases, such as osteoporosis, knee osteoarthritis and lumbar spondylosis: a three-year follow-up of the road study. Osteoporos Int 26:151–161
Ministry of Health, Labour and Welfare. The report of National Health and Nutrition Survey (2008) Available at http://www.mhlw.go.jp/bunya/kenkou/eiyou/h20-houkoku.html [In Japanese]
Acknowledgments
This work was supported by Grant-in-Aid funding from the Ministry of Health, Labour and Welfare: H17-Men-eki-009 (Director, Kozo Nakamura), H20-Choujyu-009 (Director, Noriko Yoshimura), H23-Choujyu-002 (Director, Toru Akune), H25-Choujyu-007 (Director, Noriko Yoshimura), and H25-Nanchitou (Men)-005 (Director, Sakae Tanaka). The study was also supported by Scientific Research grants B26293139, B23390172, and B20390182 and Challenging Exploratory Research grants 15K15219 and 24659317 to Noriko Yoshimura; Scientific Research grants B23390356 and C20591774 and Challenging Exploratory Research grant 23659580 to Shigeyuki Muraki; Challenging Exploratory Research grants 24659666 and 21659349 and Young Scientists A18689031 to Hiroyuki Oka; Scientific Research grants B26293329, B23390357, C20591737 and Challenging Exploratory Research grant 25670293 to Toru Akune; and Collaborating Research with NSF from the Ministry of Education, Culture, Sports, Science, and Technology in Japan 08033011-00262 (Director, Noriko Yoshimura). The study was also supported by grants from the Japan Osteoporosis Society (Noriko Yoshimura, Shigeyuki Muraki, Hiroyuki Oka, and Toru Akune), Japan Osteoporosis Foundation (2015, Noriko Yoshimura), research aids from the Japanese Orthopaedic Association (JOA—Subsidized Science Project Research 2006-1 and 2010-2, Director, Hiroshi Kawaguchi; 2014-1, Director, Kozo Nakamura), and the Japanese Society for Musculoskeletal Medicine (2015, Director, Shigeyuki Muraki). The authors wish to thank Dr. Naoki Hirabayashi of the Kawakami Clinic, Hidakagawa Town; Mrs. Tomoko Takijiri, Mrs. Rie Takiguchi, Mrs. Kyoko Maeda, Ms. Ikuyo Ueyama, Mrs. Michiko Mori, Mrs. Hisayo Sugimoto, and other members of the public office in Hidakagawa Town; and Mrs. Tamako Tsutsumi, Mrs. Kanami Maeda, Mrs. Megumi Takino, Mrs. Shuko Okada, Mrs. Kazuyo Setoh, Mrs. Chise Ryouno, Mrs. Miki Shimosaki, Mrs. Chika Yamaguchi, Mrs. Yuki Shimoji, and other members of the public office in Taiji Town for their assistance in locating and scheduling participants for examinations. We would also like to thank Ms. Kyoko Yoshimura, Mrs. Toki Sakurai, Mrs. Saeko Sahara, and Mr. Noriyuki Oe for their assistance with data reduction and administration.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
All participants provided written informed consent, and the study was conducted with the approval of the ethics committees of the University of Tokyo (Nos. 1264 and 1326) and the University of Wakayama Medical University (No. 373). All procedures were conducted in accordance with the ethical standards as described in the 1964 Declaration of Helsinki, and its later amendments.
Rights and permissions
About this article
Cite this article
Yoshimura, N., Muraki, S., Oka, H. et al. Is osteoporosis a predictor for future sarcopenia or vice versa? Four-year observations between the second and third ROAD study surveys. Osteoporos Int 28, 189–199 (2017). https://doi.org/10.1007/s00198-016-3823-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3823-0