Abstract
Summary
This study examines demographic patterns and body size relationships in trabecular bone score and lumbar spine BMD of US adults from NHANES 2005–2008.
Introduction
Limited data exist on demographic and body size relationships for trabecular bone score (TBS), a new variable derived from bone texture analysis of lumbar spine dual-energy X-ray absorptiometry (DXA) scans. This study compares demographic patterns and correlations with body size (body mass index (BMI), weight, waist circumference, total body fat, trunk fat, trunk lean) between TBS and lumbar spine bone mineral density (LSBMD) for adults age ≥20 years from the National Health and Nutrition Examination Survey (NHANES) 2005–2008 with BMI in the optimal range for TBS (15–37 kg/m2).
Methods
LSBMD, TBS, body fat, and lean were obtained by DXA. Weight, height, and waist circumference were measured. BMI was calculated from height and weight.
Results
Sex differences in TBS varied by age and race/ethnicity (p sex X age interaction and p sex X race/ethnicity interaction < 0.001). In most of the nine demographic subgroups examined, TBS did not differ by sex (four subgroups) or was significantly higher in women (three subgroups). TBS differences by race/ethnicity were inconsistent in men; in women, non-Hispanic whites (NHWs) had higher TBS than non-Hispanic blacks (NHBs) or Mexican Americans (MAs) in all age groups. In contrast, LSBMD was either significantly higher in men (five subgroups) or did not differ by sex (four subgroups). Race/ethnic differences in LSBMD were consistent across age and sex (NHB > NHW > MA). All body size variables were negatively related to TBS but positively related to LSBMD.
Conclusions
Demographic patterns and body size relationships differed between TBS and LSBMD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trabecular bone score (TBS) is a new variable that is derived from bone texture analysis of lumbar spine dual-energy X-ray absorptiometry (DXA) scans [1]. TBS predicts vertebral fracture risk independently of lumbar spine bone mineral density (LSBMD) [1], and an algorithm to account for TBS when calculating the 10-year fracture risk probability scores with the WHO FRAX® model has recently been developed [2]. The International Society for Clinical Densitometry (ISCD) has published guidelines for the clinical use of TBS measures as well [3]. To date, however, there are limited data available on demographic patterns in TBS, especially for men and nonwhites. In addition, although the TBS measurement is adversely affected by excessive abdominal soft tissue [1], there are little data describing the relationship between TBS and body size parameters that may reflect abdominal tissue.
Lumbar spine DXA scans were recently re-analyzed to obtain TBS data for adults aged 20 years and older who were examined in the National Health and Nutrition Examination Survey (NHANES) cycles conducted between 2005 and 2008. The objective of the present study is to examine patterns in TBS by age, sex, and race/ethnicity. The relationships between TBS and variables that reflect body soft tissue overall (BMI, weight, total body fat mass) or more specifically in the general area of the lumbar spine where TBS is measured (waist circumference, trunk fat mass, trunk lean mass) are also explored. Finally, the relationships between TBS with these demographic and body size variables are compared with those seen with LSBMD.
Methods
Sample
The present study used data from two survey cycles of the NHANES, which is currently conducted annually by the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention, to assess the health and nutritional status of a representative sample of the non-institutionalized, civilian US population. Although a representative sample is currently collected each year in NHANES, data are released for 2-year periods to protect confidentiality and increase statistical reliability. The present study combines data collected in two of these cycles, NHANES 2005–2006 and NHANES 2007–2008. NHANES collects data via household interviews and direct standardized physical examinations that were conducted in specially equipped mobile examination centers [4]. All procedures in NHANES 2005–2008 were approved by the NCHS Research Ethics Review Board, and written informed consent was obtained from all subjects. The overall unweighted examination response rate for adults aged 20 years and older was 71 % in NHANES 2005–2008.
Estimates by race/ethnicity are presented separately for non-Hispanic whites (NHWs), non-Hispanic blacks (NHBs), and Mexican Americans (MAs) because NHANES 2005–2008 provides reliable estimates for these three groups. Race and ethnicity were self-reported by the participants.
The analytic sample used in the present study consisted of 7682 adults aged 20 years and older with valid data for TBS and LSBMD for at least two lumbar vertebrae and whose body mass index (BMI) value fell between 15 and 37 kg/m2, which is the BMI range for which TBS measurements have been optimized for the software version used in the present study. The sample was limited to respondents with valid data for at least two lumbar vertebrae to be consistent with recommendations of the ISCD [5]. Ninety percent (n = 6684) of respondents in the analytic sample had valid TBS data for all four lumbar vertebrae, 7 % (n = 672) had valid data for three lumbar vertebrae, and 3 % (n = 326) had valid data for two lumbar vertebrae.
Variables
LSBMD was measured from posterior-anterior (PA) lumbar spine scans obtained with Hologic QDR 4500A fan-beam densitometers (Hologic, Inc., Bedford, MA) using Apex version 3.0 software. TBS was measured on the same lumbar vertebrae as LSBMD using TBS iNsight® version 2.1 software (Med-Imaps, Pessac, France). TBS is derived from the PA spine DXA image by evaluating pixel gray-level variations [1]. TBS is affected by the amount of soft tissue in the lumbar spine region, so the TBS software includes an adjustment for BMI. The TBS software version used in the present study (version 2.1) is optimized for the BMI range between 15 and 37 kg/m2.
Details of the DXA examination protocol have been published elsewhere [6]. Scanning was done in the fast mode. Rigorous quality control (QC) programs were employed, which included use of anthropomorphic phantoms and review of each QC and respondent scan at a central site (Department of Radiology of the University of California, San Francisco), using standard radiologic techniques and study-specific protocols developed for the NHANES [6]. Survey respondents were not eligible for a lumbar spine DXA scan if they were pregnant, self-reported an imaging procedure using contrast material in the previous seven days, or weighed >300 lb (DXA table limitation). LSBMD and TBS data for an individual vertebra were considered invalid if any of the following were noted for that vertebra: degenerative diseases, fusions or fractures, removable or nonremovable (e.g., implants, protheses) objects, excessive x-ray “noise” due to obesity, positioning problems, or participant movement during the scan. TBS data also were not calculated for respondents with missing BMI data. Total LSBMD and TBS were calculated as the average values for the individual lumbar vertebra in respondents with at least two valid vertebrae.
BMI was calculated as body weight (kilograms) divided by height (meters squared). The publicly released BMI variable (BMXBMI), which was reported to two decimal places, was used in the present study. Height and weight were measured using standardized protocols [7]. Waist circumference was measured just above the uppermost lateral border of the right ilium while respondents were standing [7]. Care was taken to ensure that the tape measurement was horizontally aligned parallel to the floor and was snug but did not compress the skin.
Body composition data, including total body fat mass, trunk fat mass, and trunk lean mass, from whole body DXA scans were available for a subsample of respondents ages 20–69 years who were examined in NHANES 2005–2006. The same densitometers and methods described for obtaining lumbar spine scans were used to perform the whole body scans [6, 8]. Respondents with missing whole body DXA data were not a random subset of the eligible sample, so multiple imputation of missing data was performed using a sequential regression multivariate imputation procedure [9] prior to public release on the NHANES website. The body composition subsample used in the present study consisted of 2791 respondents aged 20–69 years with non-missing TBS data and BMI between 15 and 37 kg/m2. The multiply imputed body composition data were used in the present study.
Statistical analysis
Analyses were conducted with PC-SAS (Version 9.3, SAS Institute, Cary, NC) and SUDAAN (Version 11.0.1, Research Triangle Institute, NC). All analyses used the examination sample weights and incorporated the complex design of the survey in calculating statistical tests. Linear regression (PROC REGRESS) was used to assess interactions between age, sex, and race/ethnicity in terms of their relationship with TBS. Linear regression was also used to examine differences in mean TBS and LSBMD by these demographic characteristics after adjusting for age. The Pearson correlation coefficients (PROC VARGEN) were calculated to assess the strength and direction of the relationship between TBS or LSBMD and the selected body size variables examined in the present study.
Secondary analyses were conducted to assess the impact of calculating total LSBMD and TBS for those with two or three valid individual vertebrae. Analyses were repeated after restricting the analytic sample to those with four valid vertebrae only; results and conclusions were similar to those observed in the full analytic sample with two to four valid vertebrae, so results are shown for the full analytic sample. Secondary analyses were also conducted to assess the impact of limiting respondents to those with BMI between 15 and 37 kg/m2 by comparing mean TBS between respondents age 20 years and older before and after limiting BMI to this range. Mean TBS was also compared by age, sex, and race/ethnicity between the analytic sample and respondents with non-missing TBS and BMI >37 kg/m2 (n = 1069); there were too few individuals with non-missing TBS and BMI <15 (n = 5) to permit an analysis of this group.
Missing data
The main analytic sample was derived from the 9212 examined adults age 20 years and older in NHANES 2005–2008 with non-missing BMI values between 15 and 37 kg/m2. Of these, 1530 (17 %) were excluded because they lacked valid BMD and TBS data. The final main analytic sample consisted of 7682 respondents.
Analyses were also conducted on a subsample of adults aged 20–69 years with body composition data from NHANES 2005–2006. Of the 3467 adults age 20–69 with body composition data and non-missing BMI values between 15 and 37 kg/m2, 676 were excluded due to missing BMD data for at least two lumbar vertebrae. The final body composition subsample consisted of 2781 respondents.
Because 17 % of the examined sample of adults age 20 years and older from NHANES 2005–2008 had been excluded from the main analytic sample, nonresponse bias analyses were conducted. Excluded respondents were more likely to be older, female, non-Hispanic black, and self-reported their health status as fair or poor than respondents in the analytic sample. To further examine the potential for nonresponse bias, the publicly released examination sample weights were adjusted for item nonresponse using the PROC WTADJUST procedure in SUDAAN. We used this model-based calibration procedure to re-weight the data by computing nonresponse and post-stratification weight adjustments by age, sex, and race/Hispanic origin. The adjusted sample weights resulted in similar conclusions to those seen when the publicly released examination sample weights were used, so only the latter results are shown.
Results
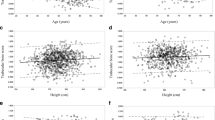
Patterns in TBS and LSBMD by age, sex, and race/ethnicity are illustrated in Figs. 1 and 2, respectively. TBS declined cross-sectionally by age decade in each race/ethnic group in both men and women (p < 0.001). LSBMD also declined cross-sectionally by age decade in each race/ethic group in women (p < 0.001), but not in men. Specifically, mean LSBMD increased significantly with age in NHW men, but mean LSBMD did not differ by age in NHB and MA men (Fig. 2).
TBS patterns by sex and race/ethnicity are complex, as illustrated by Fig. 1 and confirmed by the presence of significant sex X age and sex X race/ethnicity interaction terms (p < 0.001) when tested in a linear regression model. To summarize these complex relationships more succinctly, age-adjusted results for TBS are presented in Table 1 using three broad age groups (20–39, 40–59, and 60 years and older). Differences in mean TBS by sex varied by both age and race/ethnicity. Young and middle-aged adult NHW women had significantly higher mean TBS than NHW men, but mean TBS in NHW women age 60 years and older did not differ significantly from mean TBS in older NHW men. In contrast, mean TBS in NHB did not differ by sex in young or middle-aged adults, but was approximately 5 % higher in men than women in the older age group. Among MAs, mean TBS did not differ by sex in young adults, was significantly higher (by ∼3 %) in women compared to men in middle-aged adults, but was significantly higher in men (by ∼4 %) than women in the older adults.
The pattern of race/ethnic differences in TBS by age also differed between men and women (Table 1). There were fewer significant differences between race/ethnic groups in men overall, and the differences were not consistent by age. In young adult men, mean TBS was significantly higher in NHW than NHB, whereas this pattern was reversed in the oldest group of men. In middle-aged men, NHB had significantly higher mean TBS than MA, but mean TBS did not differ between NHB and NHW in this age group. In contrast, among women, race/ethnic differences were consistent, with NHW having higher mean TBS than either NHB or MA in all age groups.
Age-adjusted mean LSBMD by sex, broad age group, and race/ethnicity is also shown in Table 1. Unlike TBS, LSBMD did not differ by sex in young adults in any of the race/ethnic groups, but in middle-aged and older adults, mean LSBMD was significantly higher in men than women in each race/ethnic group except middle-aged MA. Also in contrast to TBS, mean LSBMD patterns by race/ethnicity were consistent across sex and age groups, with NHB having the highest values, NHW having intermediate values, and MA having the lowest values.
Table 2 shows the correlation between TBS and selected anthropometric and body composition variables by sex and age. The relationship between these body size variables and TBS did not vary by race/ethnicity (e.g., the race X body size variable interactions were not significant), so results are shown for all races combined. TBS was negatively correlated with all the body size variables in all sex and age groups. In addition, correlations with all body size variables were larger in men than in women overall. Within sex, correlations with TBS were significantly higher (p < 0.05) for waist circumference than for all body size variables except trunk fat mass in men. Among women, the correlation between TBS and waist circumference was significantly higher than that with BMI, body weight, or trunk lean mass, but did not differ from the correlation between TBS and total body or trunk fat mass.
Correlations of these body size variables with LSBMD are shown for comparison in Table 3. In contrast to TBS, LSBMD was positively correlated with all six body size variables. The correlations with LSBMD also did not differ by sex. Finally, within sex, the correlations between trunk lean mass and LSBMD were significantly higher overall (p < 0.05) than correlations for all the other body size variables except body weight in both men and women.
The Pearson correlation between LSBMD and TBS was 0.30 (95 % CI 0.27, 0.34) in men and 0.52 (95 % CI 0.49, 0.55) in women (data not shown).
Results of the sensitivity analyses designed to assess the impact of BMI exclusions for TBS revealed that mean TBS values among those with BMI >37 kg/m2 were approximately 26 % lower in men and 15 % lower in women than mean TBS in those with BMI between 15 and 37 kg/m2 (p < 0.001 for both sexes). However, mean TBS estimates for the entire sample with non-missing TBS values (e.g., no BMI exclusions applied) were only 1–2 % lower than mean TBS for the analytic sample that was limited to BMI between 15 and 37 kg/m2, and conclusions regarding demographic patterns in TBS were unchanged. This is likely due to the fact that only 8 % of respondents in NHANES 2005–2008 with non-missing TBS data had BMI >37 kg/m2.
Discussion
TBS varied by age, sex, and race/ethnicity in a complex manner among US adults with BMI in the optimal range for this measurement. TBS demographic patterns were also generally more complex than those seen in LSBMD, and in some cases, results for the two bone variables suggested different conclusions regarding the group with the lowest values, and hence higher fracture risk. For example, the similar TBS values in older NHW men and women suggest that their fracture risk does not differ, whereas sex differences in LSBMD suggest that women are at higher risk. The two variables also came to divergent conclusions about racial differences in risk among women in all age groups: the TBS pattern suggested that NHB women were more at-risk than NHW women, while the LSBMD pattern suggested the converse. In both cases where conclusion about the relative ranking of risk diverged between TBS and LSBMD, the LSBMD pattern appeared to be more consistent with available data on bone architecture and vertebral fracture patterns, as those data suggest that vertebral bone architecture is weaker and vertebral fracture risk is higher in women than men and in whites than in blacks or Mexican Americans [10–14].
Interestingly, age patterns in TBS and LSBMD were similar in women (negative for both variables), but they diverged in men. Specifically, TBS was negatively related to age in men, whereas LSBMD either increased with age or was similar in older and younger men, depending on the race/ethnic group considered. A negative pattern in values indicates increasing risk with age, which is consistent with vertebral fracture patterns [11, 12]. The divergence in age patterns between TBS and LSBMD in men may be due to the higher prevalence of spinal artifacts, such as osteophytes, in men [15]. These artifacts can falsely elevate BMD but appear to have little or no effect on TBS [16–19].
We also compared the relationship between TBS or LSBMD and various body size variables, since body size and composition differs significantly by sex and race/ethnicity [20]. Specifically, we compared relationships between TBS and LSBMD with variables that reflect both total amount of body tissue (BMI, weight, total body fat mass, and total body percent fat) and amount of tissue in the lumbar spine region (waist circumference, trunk fat mass, and trunk lean mass). TBS and LSBMD differed in their relationship with these body size variables in several ways. First, they differed in direction: TBS was negatively associated with the body size variables, while LSBMD was positively associated. Having a positive relationship with BMI appears to be more consistent with vertebral fracture risk: although data linking BMI to vertebral fracture risk are somewhat mixed, the majority of studies published to date suggest that high BMI is either associated with a lower risk of vertebral fracture or has no effect [21–30]. The body size variable with the strongest relationship with TBS and LSBMD also differed. Waist circumference and trunk fat mass had the strongest correlations with TBS overall, while trunk lean mass and weight had the strongest correlations with LSBMD.
The reasons for the differences in demographic patterns between TBS and LSBMD are not clear. The use of an adjustment for BMI to address the impact of soft tissue on TBS measurements might be one possible factor. For example, BMI reflects overall body fatness, so a BMI adjustment only indirectly addresses the issue of interference from soft tissue in the lumbar spine scan area when calculating TBS [1]. We found significantly higher correlations between TBS and waist circumference or trunk fat mass than between TBS and BMI in both sexes, which is consistent with this possibility. In addition, the relationship between fatness and BMI differs by age, sex, and race/ethnicity [31–34], which could potentially introduce confounding when comparing TBS by these demographic variables. Furthermore, the procedures used for the BMI adjustment in the TBS software are proprietary, so it is not possible to assess whether overcorrection by BMI played a role in the TBS-body size relationships observed in the present study. Identifying the best approach to address the impact of soft tissue interference on TBS may be complex, however. For example, although waist circumference was significantly correlated with TBS and is relatively simple to measure, it also varies in its relationship with adipose tissue in the abdominal area by age, sex, and race/ethnicity [35, 36].
There are currently very little published data on TBS values in men or in blacks, and, to our knowledge, no data in Mexican Americans. Comparing TBS results from different studies is complicated by differences in the software version used to generate the TBS data, as a previous version was optimized for women of average body size and was found to have limitations when used in men [37]. Studies based on the earlier TBS software version found higher values in women than in men [37, 38]. However, after using the updated software version, Leslie et al. [37] found significantly higher mean TBS value, by roughly 3 %, in white Canadian men vs. women over the age 40 years. Despite using the updated software version in the present study, we found that NHW men had significantly lower values than NHW women for age 20–59 years, and similar TBS values for age 60 years and older. It is important to note, however, that both these previous studies [37, 38] used a different DXA system than did the present study, which might play a role in observed differences in study results.
The present study also came to a different conclusion regarding TBS differences in older NHW and NHB women than did Aloia et al. [39], who reported that postmenopausal black women in their study had higher TBS values than published values for white women from other studies. Aloia et al. [39] used a different software version (e.g., version 2.0.0.1; personal communication, Dr. John Aloia) than the present study, which may have contributed to the different study results. Differences in the study samples could also play a role in the discrepant results seen between in the present study and some of the previous studies [37, 39]. For example, Aloia et al. [39] used medical history as well as physical and laboratory tests to identify healthy women for their sample, while the white Canadian sample was drawn from a clinical registry [37]. In contrast, the NHANES sample was selected to be representative of the non-institutionalized US population. Additionally, men in the white Canadian sample had significantly lower BMI than women (26.8 versus 27 kg/m2, respectively) whereas the opposite was true in the older NHW white men and women in the present study (28.2 versus 26.9 kg/m2, respectively).
The correlations between TBS and BMI in the present study also differed from previously published studies. Most of these studies focused on women and used earlier versions of the TBS software. TBS correlations with BMI in those studies ranged from roughly −0.13 to −0.19 [37, 40–43], in contrast to the present study where the correlation between TBS and BMI in women was −0.33 in women overall. To our knowledge, only the study by Leslie et al. [37] has reported the correlation between TBS and BMI in men. They reported a relatively similar correlation (e.g., r = −0.40) to that seen in the present study (e.g., r = −0.53) when the earlier software version 1.8 was used, but much lower correlations (r = 0.01) than the present study when the same updated software version (version 2.1) was used. Interestingly, correlations between TBS and weight in women reported in most of these previous studies ranged from −0.16 to −0.17, which is reasonably similar to the correlation between TBS and weight seen among women in the present study. Reasons for these differences in the correlations between TBS and BMI are not clear, especially in light of the general agreement between studies for the correlation between TBS and body weight.
The present study has some advantages, including use of a large, nationally representative sample and TBS measurements that are based on the most recent software version that was updated to address limitations in its application to men [37]. However, the study also has limitations. For example, TBS data were pooled across the three DXA instruments used in NHANES 2005–2008, but we were unable to directly assess comparability of the TBS data between these three instruments because a TBS quality control phantom did not exist at that time and those DXA instruments are no longer available. There were no statistically significant differences in BMD data from standard spine phantoms that were regularly circulated among the three DXA instruments during that time period [44], but it is not clear whether the BMD phantom results are applicable to TBS. However, the effect of potential calibration differences on the NHANES TBS data is likely minimized in the relative comparisons between demographic groups made in the present study, because the TBS data for these demographic groups were obtained in roughly equal proportions from the three DXA instruments. Another potential limitation is that the TBS data in this study were collected on Hologic DXA instruments using the fast scan mode, and it is unclear whether they are directly comparable with TBS data collected on other DXA systems or scan modes.
Other limitations include potential nonresponse bias in the estimates presented in our study. Use of sample weights in the analysis helps to address this bias to some extent, since a nonresponse adjustment factor is included in their calculation. However, 17 % of the respondents ages 20 years and older with BMI between 18 and 37 kg/m2 examined in NHANES 2005–2008 lacked data for TBS and LSBMD, and this nonresponse is not addressed by the sample weight adjustments. Results from the analyses that were re-weighted to address this additional nonresponse were similar to those obtained when the publicly released sample weights were used, which suggests that major nonresponse bias is unlikely, however. An additional study limitation is the exclusion of institutionalized persons, an important at-risk group for osteoporosis [45], from the NHANES sampling frame by design. Finally, findings from the present study also apply only to the non-institutionalized US population with BMI in the optimal range for TBS measurements (e.g., 15–37 kg/m2). However, sensitivity analysis results suggested that the BMI exclusion probably did not introduce major nonresponse bias, as TBS estimates for sample created after making the BMI exclusions were only 1–2 % higher than those observed for the examined sample prior to making the BMI exclusions, and conclusions regarding demographic patterns in TBS were unchanged, most likely because only 8 % of the population had BMI values above that BMI threshold. This should not be interpreted, however, to indicate that it is appropriate to disregard the recommendation from the TBS manufacturer regarding the appropriate BMI range for TBS calculation, since mean TBS for the respondents with BMI >37 kg/m2 was significantly lower than mean TBS of respondents with BMI between 15 and 37 kg/m2.
In conclusion, demographic patterns in TBS in US adults with BMI in the optimal range for these measurements were complex and differed from those seen in LSBMD in several ways. In some cases, results for the two bone variables suggested different conclusions regarding the group with the lowest values, and hence higher fracture risk. The at-risk demographic group identified by TBS differed from observed patterns in vertebral fracture occurrence by these demographic variables in some cases as well. TBS and LSBMD also had different relationships with body size variables, with TBS being negatively related to these variables, while LSBMD was positively related. More work is needed to understand the basis for these observed differences in demographic and body size patterns between TBS and LSBMD.
References
Silva BC, Leslie WD, Resch H, Lamy O, Lesnyak O, Binkley N, McCloskey EV, Kanis JA, Bilezikian JP (2014) Trabecular bone score: a noninvasive analytical method based upon the DXA image. J Bone Miner Res 29:518–530
McCloskey EV, Oden A, Harvey NC, Leslie WD, Hans D, Johansson H, Kanis JA (2015) Adjusting fracture probability by trabecular bone score. Calcif Tissue Int 96:500–509
Silva BC, Broy SB, Boutroy S, Schousboe JT, Shepherd JA, Leslie WD (2015) Fracture risk prediction by non-BMD DXA measures: the 2015 ISCD official positions part 2: trabecular bone score. J Clin Densitom 18:309–330
Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. (2013) National Health and Nutrition Examination Survey: plan and operations, 1999–2010. National Center for Health Statistics, Hyattsville, MD
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S (2013) Executive summary of the 2013 International Society for Clinical Densitometry position development conference on bone densitometry. J Clin Densitom 16:455–466
Centers for Disease Control and Prevention National Center for Health Statistics (2007) Dual energy X-Ray absorptiometry (DXA) procedures manual. Centers for Disease Control and Prevention, National Center for Health Statistics. http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_dexa.pdf
Centers for Disease Control and Prevention National Center for Health Statistics (2000) Anthropometry procedures manual. Centers for Disease Control and Prevention National Center for Health Statistics, Hyattsville MD
Centers for Disease Control and Prevention National Center for Health Statistics (2004) Body composition procedure manual. Centers for Disease Control and Prevention, National Center for Health Statistics. http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/bc.pdf
Centers for Disease Control and Prevention National Center for Health Statistics (2008) Technical documentation for the 1999–2004 dual-energy x-ray absorptiometry (DXA) multiple imputation data files. . http://www.cdc.gov/nchs/data/nhanes/dxa/dxa_techdoc.pdf
Seeman E, Delmas PD (2006) Bone quality—the material and structural basis of bone strength and fragility. New Engl J Med 354:2250–2261
Taylor AJ, Gary LC, Arora T et al (2011) Clinical and demographic factors associated with fractures among older Americans. Osteoporosis Int 22:1263–1274
Jacobsen SJ, Cooper C, Gottlieb MS, Goldberg J, Yahnke DP, Melton LJ (1992) Hospitalization with vertebral fracture among the aged—a national population-based study, 1986–1989. Epidemiology 3:515–518
Tracy JK, Meyer W, Grigoryan M, Fan B, Flores R, Genant H, Resnik C, Hochberg M (2006) Racial differences in the prevalence of vertebral fractures in older men: the Baltimore Men’s Osteoporosis Study. Osteoporosis Int 17:99–104
Cauley JA, Palermo L, Voot M, Ensrud KE, Ewing S, Hochberg M, Nevitt MC, Black DM (2008) Prevalent vertebral fractures in black women and white women. J Bone Miner Res 23:1458–1467
O’Neill TW, McCloskey EV, Kanis JA, Bhalla AK, Reeve J, Reid DM, Todd C, Woolf AD, Silman AJ (1999) The distribution, determinants, and clinical correlates of vertebral osteophytosis: a population based survey. J Rheumatol 26:842–848
Kolta S, Briot K, Fechtenbaum J, Paternotte S, Armbrecht G, Felsenberg D, Glüer CC, Eastell R, Roux C (2014) TBS result is not affected by lumbar spine osteoarthritis. Osteoporosis Int 25:1759–1764
Orwoll ES, Oviatt SK, Mann T (1990) The impact of osteophytic and vascular calcifications on vertebral mineral density measurements in men. J Clin Endocrinol Metab 70:1202–1207
Yu W, Gluer CC, Fuerst T, Grampp S, Li J, Lu Y, Genant HK (1995) Influence of degenerative joint disease on spinal bone mineral measurements in postmenopausal women. Calcif Tissue Int 57:169–174
Rand T, Seidl G, Kainberger F, Resch A, Hittmair K, Schneider B, Gluer CC, Imhof H (1997) Impact of spinal degenerative changes on the evaluation of bone mineral density with dual energy X-ray absorptiometry (DXA). Calcif Tissue Int 60:430–433
Borrud LG, Flegal KM, Looker AC, Everhart JE, Harris TB, Shepherd JA (2010) Body composition data for individuals 8 years of age and older: US population, 1999–2004. Vital Health Stat 11:1–87
Nevitt MC, Cummings SR, Stone KL et al (2005) Risk factors for a first-incident radiographic vertebral fracture in women ≥65 years of age: the Study of Osteoporotic Fractures. J Bone Miner Res 20:131–140
Compston JE, Flahive J, Hosmer DW et al (2014) Relationship of weight, height, and body mass index with fracture risk at different sites in postmenopausal women: the Global Longitudinal study of Osteoporosis in Women (GLOW). J Bone Miner Res 29:487–493
Roy DK, O’Neill TW, Finn JD et al (2003) Determinants of incident vertebral fracture in men and women: results from the European Prospective Osteoporosis Study (EPOS). Osteoporos Int 14:19–26
Samelson EJ, Hannan MT, Zhang Y, Genant HK, Felson DT, Kiel DP (2006) Incidence and risk factors for vertebral fracture in women and men: 25-year follow-up results from the population-based Framingham study. J Bone Miner Res 21:1207–1214
Johnell O, O’Neill T, Felsenberg D, Kanis J, Cooper C, Silman AJ (1997) Anthropometric measurements and vertebral deformities. European Vertebral Osteoporosis Study (EVOS) Group. Am J Epidemiol 146:287–293
Melton LJ 3rd, Atkinson EJ, Khosla S, O’Fallon WM, Riggs BL (1999) Secondary osteoporosis and the risk of vertebral deformities in women. Bone 24:49–55
Holmberg AH, Johnell O, Nilsson PM, Nilsson J, Berglund G, Akesson K (2006) Risk factors for fragility fracture in middle age. A prospective population-based study of 33,000 men and women. Osteoporos Int 17:1065–1077
Tanaka S, Kuroda T, Saito M, Shiraki M (2013) Overweight/obesity and underweight are both risk factors for osteoporotic fractures at different sites in Japanese postmenopausal women. Osteoporos Int 24:69–76
Laslett LL, Just Nee Foley SJ, Quinn SJ, Winzenberg TM, Jones G (2012) Excess body fat is associated with higher risk of vertebral deformities in older women but not in men: a cross-sectional study. Osteoporos Int 23:67–74
Pirro M, Fabbriciani G, Leli C, Callarelli L, Manfredelli MR, Fioroni C, Mannarino MR, Scarponi AM, Mannarino E (2010) High weight or body mass index increase the risk of vertebral fractures in postmenopausal osteoporotic women. J Bone Miner Metab 28:88–93
Gallagher D, Visser M, Sepúlveda D, Pierson RN, Harris T, Heymsfield SB (1996) How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol 143:228–239
Flegal KM, Shepherd JA, Looker AC, Graubard BI, Borrud LG, Ogden CL, Harris TB, Everhart JE, Schenker N (2009) Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr 89:500–508
Fernández JR, Heo M, Heymsfield SB, Pierson RN, Pi-Sunyer FX, Wang ZM, Wang J, Hayes M, Allison DB, Gallagher D (2003) Is percentage body fat differentially related to body mass index in Hispanic Americans, African Americans, and European Americans? Am J Clin Nutr 77:71–75
Deurenberg P, Yap M, van Staveren WA (1998) Body mass index and percent body fat: a meta analysis among different ethnic groups. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity 22:1164–1171
Camhi SM, Bray GA, Bouchard C, Greenway FL, Johnson WD, Newton RL, Ravussin E, Ryan DH, Smith SR, Katzmarzyk PT (2011) The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obesity (Silver Spring, Md) 19:402–408
Carroll JF, Chiapa AL, Rodriquez M, Phelps DR, Cardarelli KM, Vishwanatha JK, Bae S, Cardarelli R (2008) Visceral fat, waist circumference, and BMI: impact of race/ethnicity. Obesity (Silver Spring, Md) 16:600–607
Leslie W WR, Majumdar S, Lix L, Hans D (2014) Clinical performance of an updated version of trabecular bone score in men and women: the Manitoba BMD Cohort. J Bone Miner Res 29 (Suppl 1):
Leib E, Winzenrieth R, Aubry-Rozier B, Hans D (2014) Vertebral microarchitecture and fragility fracture in men: a TBS study. Bone 62:51–55
Aloia JF, Mikhail M, Usera G, Dhaliwal R, Islam S (2015) Trabecular bone score (TBS) in postmenopausal African American women. Osteoporosis Int 26:1155–1161
Leslie WD, Krieg MA, Hans D (2013) Clinical factors associated with trabecular bone score. J Clin Densitom 16:374–379
Iki M, Tamaki J, Sato Y, Winzenrieth R, Kagamimori S, Kagawa Y, Yoneshima H (2015) Age-related normative values of trabecular bone score (TBS) for Japanese women: the Japanese Population-based Osteoporosis (JPOS) study. Osteoporosis Int 26:245–252
Dufour R, Winzenrieth R, Heraud A, Hans D, Mehsen N (2013) Generation and validation of a normative, age-specific reference curve for lumbar spine trabecular bone score (TBS) in French women. Osteoporosis Int 24:2837–2846
Simonelli C, Leib E, Mossman N, Winzenrieth R, Hans D, McClung M (2014) Creation of an age-adjusted, dual-energy x-ray absorptiometry-derived trabecular bone score curve for the lumbar spine in non-Hispanic US White women. J Clin Densitom 17:314–319
Centers for Disease Control and Prevention National Center for Health Statistics (2010) 2005–2008 Data documentation, codebook, and frequencies: dual-energy X-ray absorptiometry -- Spine (DXXSPN_D). http://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/DXXSPN_D.htm, http://wwwn.cdc.gov/Nchs/Nhanes/2007-2008/DXXSPN_E.htm
Zimmerman SI, Girman CJ, Buie VC, Chandler J, Hawkes W, Martin A, Holder L, Hebel JR, Sloane PD, Magaziner J (1999) The prevalence of osteoporosis in nursing home residents. Osteoporos Int 9:151–157
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures in NHANES 2005–2008 were approved by the NCHS Research Ethics Review Board, and written informed consent was obtained from all subjects.
Conflicts of interest
None.
Required disclaimer
The findings and conclusions in this report are those of the authors and not necessarily those of the Centers for Disease Control and Prevention.
Rights and permissions
About this article
Cite this article
Looker, A.C., Sarafrazi Isfahani, N., Fan, B. et al. Trabecular bone scores and lumbar spine bone mineral density of US adults: comparison of relationships with demographic and body size variables. Osteoporos Int 27, 2467–2475 (2016). https://doi.org/10.1007/s00198-016-3550-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3550-6




 Non-Hispanic white (NHW).
Non-Hispanic white (NHW).  Non-Hispanic black (NHB).
Non-Hispanic black (NHB).  Mexican American (MA)
Mexican American (MA)
 Non-Hispanic white (NHW)
Non-Hispanic white (NHW)  . Non-Hispanic black (NHB).
. Non-Hispanic black (NHB).  Mexican American (MA)
Mexican American (MA)