Abstract
Summary
Despite the high burden of hip fracture in China, there is limited information on its management. This study investigated the management of hip fractures in a Beijing tertiary hospital and compared practice with that in 180 hospitals in the UK. The findings show a significant gap exists between the countries.
Introduction
The purpose of this study was to determine if the management of older people with hip fractures in a Beijing tertiary hospital is comparable with the UK best practice guidelines for hip fracture management and the UK National Hip Fracture Database 2012, obtained from 180 hospitals.
Methods
A retrospective audit was undertaken in a large tertiary care hospital in Beijing. Data were compared with the National Hip Fracture Database 2012 collected in 180 hospitals in the UK on the proportion of patients managed according to the UK Blue Book standards.
Results
Sixty-six percent of patients were admitted to an orthopaedic ward within 24 h of fracture, while 100 % of patients in the UK were admitted to an orthopaedic ward within 24 h of arrival to an accident and emergency department. Only 8 % of patients received surgery within 48 h of admission compared with 83 % in the UK; 10 % received no surgery compared with 2.5 % in the UK; and 27 % received orthogeriatrician assessment compared with 70 % in the UK. New pressure ulcers developed in 2 % of patients compared with 3.7 % of those in the UK; whereas, 0.3 % of patients were assessed for osteoporosis treatment and 3.8 % received falls assessment, and comparable figures for the UK were 94 and 92 %, respectively.
Conclusions
Significant gaps exist in hip fracture management in the Beijing hospital compared with the best practice achieved in 180 UK hospitals, highlighting the need to implement and evaluate proactive strategies to increase the uptake of best practice hip fracture care in China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Improving the management of hip fractures and hip fracture prevention in older people are significant health priorities in the UK [1]. The British Orthopaedic Association and the British Geriatric Society have produced the UK Blue Book, which summarises current evidence and best practice consensus in the care and secondary prevention of fragility fractures [2]. The UK National Hip Fracture Database (NHFD) uses the Blue Book guidelines to audit quality standards of care for individuals hospitalised with hip fractures in the UK [3].
In the UK, six standards of hip fracture care are continually monitored and provide the basis for assessment of quality care: admission to an acute orthopaedic ward within 4 h of presentation to accident and emergency (A&E), surgery within 48 h of admission for those who are medically fit, assessment and access to orthogeriatrician care, care to minimise incidence of pressure ulcers, assessment to determine the need for antiresorptive therapy to prevent future osteoporotic fractures, and assessment and intervention to prevent the future occurrence of falls [4–6]. The adoption of these standards in the UK has led to significant improvements in patient outcomes and produced annual savings of 14 million GBP [1].
In 1990, an estimated 1.66 million hip fractures occurred worldwide [7], with the numbers expected to increase to 3.1 million in 2030 and 6.25 million in 2050 [7, 8]. The projected increases are primarily the result of ageing populations and increased life expectancy in China and India, such that by 2050, it is projected that nearly half of all hip fractures will occur in Asia [9, 10]. In 2003–2006, a survey undertaken by the Chinese Ministry of Health estimated that more than 69.4 million Chinese over 50 had osteoporosis, of which 687,000 were likely to sustain hip fractures each year [11]. However, this may be an underestimate as hip fractures in individuals over 70 years in Beijing increased 3.4 times for women and doubled for men in the years between 1992 and 2006 [12].
Despite the current and projected burden of hip fracture in China, there is currently no reliable information on the management of hip fractures amongst older people in China. We therefore undertook a study to document the current management of hip fractures for individuals seeking care in a major orthopaedics hospital in Beijing and to determine whether the pathways of care identified were consistent with the Blue Book guidelines and with current practice in 180 UK hospitals as recorded in NHFD.
Methods
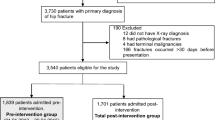
We retrospectively reviewed the electronic medical records of all patients aged 60 years and older with an X-ray-confirmed hip fracture admitted to Ji Shui Tan Hospital (JSTH) within 30 days of a fracture during the period from 1 December 2009 to 31 December 2011. Patients with pathological fractures and with terminal malignancies were excluded. JSTH is the leading tertiary care facility for orthopaedics in China and the 4th medical college of Peking University with an estimated total of 1000 orthopaedic beds. Since 1 December 2009, all patients were required to be registered in the JSTH electronic medical record system.
The data collection format for the study was similar to that used for the UK NHFD audit. The data fields include demographic profile, pre-fracture mobility status, fracture to admission time, time from admission to surgery, orthogeriatrician care, type of fracture and surgical procedure, mortality, complications including pressure ulcers, medication for bone health, falls prevention, and length of stay in the orthopaedics acute care service.
Two researchers independently reviewed the electronic medical records using the same patient inclusion and exclusion criteria to ensure all registered patients were included in the study. Data were entered into Epidata software (version 3.1, Denmark) in Chinese and later translated into English for analysis. To assess the reliability of the collected data, 10 % of the reviewed electronic records were randomly selected and errors in transcription were corrected by the study researcher.
Data from the JSTH patients were then compared with the UK NHFD 2012 data, obtained from 180 hospitals between 1 April 2011 and 31 March 2012 [1].
Results
A total of 780 hip fractures in 497 (64 %) women and 283 men, with a mean age of 74.5 years (SD 7.7) were included in the JSTH audit (Table 1). The UK NHFD audit included a total of 59,365 hip fractures, of which 74 % were in women [1]. Seventy-six percent of JSTH patients with hip fracture were less than 80 years of age, compared with 30 % of the UK patients (Table 1). Nine percent of patients with hip fracture admitted to JSTH used aids for mobility pre-fracture compared with 54 % in the UK (Table 1). A fall, inside or outside the house was the cause of hip fracture in 91 % of patients admitted to JSTH, and the remainder were caused by road traffic crashes. There were no comparable data on the cause of hip fracture in the NHFD report [1].
The types of hip fractures sustained were similar in JSTH and the UK. However, the implant selection varied, with a higher proportion of intramedullary nails being used for trochanteric fractures in JSTH (77 %) compared with the UK (11 %) and a higher proportion of hemiarthroplasty being performed for intra-capsular fractures in the UK (72 %) compared with JSTH (42 %) (Table 2). Regional anaesthesia was used in 87 % of patients in JSTH compared with 40 % in the UK (Table 2). About 10 % of hip fractures admitted to JSTH were managed without surgery compared with 2.5 % in the UK (Table 2).
Almost all patients with hip fracture in the UK are initially admitted in the A&E Department and then transferred to an orthopaedics ward. In JSTH, 80 % of people with hip fractures are admitted through A&E and the remainder are first seen in the outpatient department. Two-thirds of patients in JSTH were admitted to an orthopaedic ward within 24 h of fracture. In the UK, 50 % of hip fracture patients were admitted to an orthopaedic ward within 4 h of arrival in A&E and 100 % within 24 h (Table 3). Assessment by an orthogeriatrician was undertaken for 27 % of patients in JSTH compared with 70 % in the UK (Table 3).
Eight per cent of hip fractures in JSTH were operated within 48 h of arrival in hospital compared with 83 % in the UK, and all hip fractures were operated within the first week in the UK compared with 70 % in JSTH (Table 3). New pressure ulcers developed in 2 % of admitted patients in JSTH compared with 3.7 % in the UK. Only 0.3 % of patients in JSTH were assessed for osteoporosis treatment and 3.8 % received falls assessment, compared with 94 and 92 %, respectively, in the UK (Table 3). Calcium and vitamin D were the only medications prescribed for osteoporosis treatment in JSTH.
The average length of acute hospital stay in JSTH was 13.7 days compared with 20.2 days in the UK. There were no reported in-hospital deaths in JSTH compared with a 9 % death rate in people admitted with hip fracture in the UK.
Discussion
Our study has identified major differences in the management of hip fracture in JSTH compared with practice in the UK and gaps with respect to recommended evidence-based guidelines, as outlined in the UK Blue Book. Importantly, less than 10 % of hip fracture patients receive surgery within the recommended period of 48 h comparing with over 80 % in the UK, the latter percentage being much higher also than in other European countries, such as Spain, where the figure is only 35 % [3, 13]. Post-operatively, negligible numbers receive assessment for osteoporosis and falls, in contrast to almost all receiving both in the UK. By comparison, the use of osteoporosis medication after hospitalisation for hip fracture is 39 % in South Korea and 25 % in Spain [14]. The incidence of pressure ulcers is low and similar in both audits. Only a small proportion of patients are assessed by an orthogeriatrician in JSTH, and this may reflect the lack of this service in the hospital.
In addition, the JSTH hip fracture audit shows that the hip fracture population in this hospital comprises a higher proportion of men, is about a decade younger, and has more independent mobility than the UK patient population. Notwithstanding the types of hip fractures sustained are similar, the incidence of non-surgical management is four times higher in JSTH compared with the UK. In JSTH, surgery for trochanteric fractures mostly involves the use of intramedullary nails—a more expensive treatment option than that used in the UK—and while in both audits, hemiarthroplasty was the most common choice of surgery for patients with intracapsular fractures, screw fixation and total hip replacement were reported for a higher proportion of patients in JSTH. In JSTH, there was greater use of regional anaesthesia than in the UK, consistent with best practice guidelines. Notably, the documented length of acute hospital stay was considerably shorter in JSTH than in the UK, and whereas almost one in 10 individuals in the UK died during their hospital stay, there were no recorded deaths in the JSTH audit. The higher mortality, longer length of stay in hospital, and frequent orthogeriatrician assessment is expected in the UK due to a considerable higher mean age than amongst the Chinese hip fracture patients.
Notwithstanding some limitations in the nature of the data collected, the JSTH audit provides a systematic overview of the management of all hip fracture patients in one of the largest and most influential orthopaedic facilities in Beijing, over a period of almost 2 years. However, given the retrospective nature of the data collection, the quality of data collected was dependent on the information having been recorded. For example, it was not possible to compare the times from A&E admission to orthopaedic ward admission at JSTH as these data were not collected. Additionally, the prevalence of pressure ulcers, the extent of orthogeriatrician involvement, osteoporosis management, and specialist falls assessment may be underestimates. Finally, as the data captured only related to information collected on the orthopaedic ward, the true length of hospital stay and the true extent of in-hospital mortality are unknown and may be underestimated.
The demographic profile of patients with hip fracture recorded in the JSTH audit is comparable with previous reports from China, which have shown male-to-female ratios of 1:1.78 [12] and 1:2 [15] compared with 1:1.2 in the JSTH population. However, the extent to which the findings on care observed in JSTH might be comparable with practice in other major urban hospitals in China or hospitals in smaller urban settings is uncertain. There are a few reported studies on the management of hip fracture in China and data on the patient profiles of individuals with hip fractures in other hospitals. Nevertheless, as one of the largest and most influential orthopaedics hospitals in China, it might be expected that the quality of care elsewhere in China might be less than that observed in JSTH. However, it could also be that the length of time to surgery is longer than in other hospitals, given the reputation of JSTH and consequently the potentially higher proportions of sicker patients admitted to the hospital, from a wide geographic area.
The marked differences between care observed in JSTH and the UK Blue Book guidelines suggest there is a need to better understand the reasons for these differences and the barriers and facilitators to changing practice. The findings also suggest there is a need to raise awareness in the community and amongst care-providers that hip fractures should be regarded as an emergency requiring early admission and early surgery. Few admitted hip fracture patients in JSTH received orthogeriatrician care, and this may have also contributed to the delays in surgery, given that patients with medical problems had to be referred to different specialities. As a consequence, early orthogeriatrician participation in the management of hip fractures needs to be encouraged by appropriate training of such specialists within the Chinese health system. The finding also that secondary prevention activities were not part of routine hip fracture management suggests that they too need to be incorporated into training and care pathways.
To date, there is limited published information on care pathways for the management of older people with hip fractures in China. Our retrospective study in a single urban tertiary hospital in Beijing suggests there may be important evidence-practice gaps in China. However, there is a need to confirm our findings through the conduct of prospective studies in a much larger number of hospitals, not only in major urban centres but also in smaller regional areas. The development and implementation of a standardised data collection tool will facilitate the latter as well as the formation of a China national hip fracture registry, which, in combination with best practice tariff incentives (as in the UK), has the potential to transform the management of hip fracture care in the country. In summary, health policy makers in China have the potential to prevent the looming social and financial burden of hip fractures in the burgeoning older population, by learning from the NHFD experience in managing a similar challenge in the UK.
References
National report 2012 [http://www.nhfd.co.uk/20/hipfractureR.nsf/vwcontent/2012ReportDownload/$File/NHFD+National+Report+2012.pdf?openelement]
Annual report 2011 [http://rikshoft.se/wp-content/uploads/2013/07/Arsrapport2001.pdf]
The care of patients with fragility fracture (“Blue Book”) [http://www.bgs.org.uk/pdf_cms/pubs/Blue%20Book%20on%20fragility%20fracture%20care.pdf]
Hip fracture: the management of hip fracture in adults [http://www.nice.org.uk/guidance/cg124/resources/guidance-hip-fracture-pdf]
Rosengren BE, Ahlborg HG, Mellstrom D, Nilsson JA, Bjork J, Karlsson MK (2012) Secular trends in Swedish hip fractures 1987-2002: birth cohort and period effects. Epidemiology 23(4):623–630
Scottish hip fracture audit report 2008 [http://www.shfa.scot.nhs.uk/AnnualReport/SHFA_Report_2008.pdf]
Cooper C, Campion G, Melton LJ 3rd (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2(6):285–289
Johnell O, Kanis JA (2004) An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 15(11):897–902
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA, Epidemiology ICWGoF (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22(5):1277–1288
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733
The Asian audit: epidemiology, costs and burden of osteoporosis in Asia 2009 [http://www.iofbonehealth.org/sites/default/files/PDFs/Audit%20Asia/Asian_regional_audit_2009.pdf]
Xia WB, He SL, Xu L, Liu AM, Jiang Y, Li M, Wang O, Xing XP, Sun Y, Cummings SR (2012) Rapidly increasing rates of hip fracture in Beijing, China. J Bone Miner Res 27(1):125–129
Vidan MT, Sanchez E, Gracia Y, Maranon E, Vaquero J, Serra JA (2011) Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med 155(4):226–233
Kim SC, Kim MS, Sanfelix-Gimeno G, Song HJ, Liu J, Hurtado I, Peiro S, Lee J, Choi NK, Park BJ, Avorn J (2015) Use of osteoporosis medications after hospitalization for hip fracture: a cross-national study. Am J Med 128(5):519–526, e511
Dai K, Zhang Q, Fan T, Sen SS, Osteoporotic Hip Fracture in China Study T (2007) Estimation of resource utilization associated with osteoporotic hip fracture and level of post-acute care in China. Curr Med Res Opin 23(12):2937–2943
Conflicts of interest
Maoyi Tian, Xiaofeng Gong, Santosh Rath, Jie Wei, Lijing L. Yan, Sarah E. Lamb, Richard I. Lindley, Catherine Sherrington, Keith Willett, and Robyn Norton declare that they have no conflict of interest.
Funding
Funding was provided by The George Institute for Global Health at Peking University Health Science Center, in collaboration with the Australian and UK offices.
Author information
Authors and Affiliations
Corresponding author
Additional information
Maoyi Tian and Xiaofeng Gong contributed equally to this work.
Rights and permissions
About this article
Cite this article
Tian, M., Gong, X., Rath, S. et al. Management of hip fractures in older people in Beijing: a retrospective audit and comparison with evidence-based guidelines and practice in the UK. Osteoporos Int 27, 677–681 (2016). https://doi.org/10.1007/s00198-015-3261-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3261-4