Abstract
Summary
Hip fractures continue to be one of the most serious and costly injuries suffered by older people globally. This paper describes the development of a national hip fracture audit and summarises the first 6 years of data from the Republic of Ireland. This can help inform care, standards and outcomes of hip fracture patients.
Introduction
Ireland has one of the highest standardised rates of hip fracture in the world behind northern European countries. The Irish Hip Fracture Database (IHFD) was established in 2012 to drive clinical and organisational improvements in quality and effectiveness of hip fracture care. This paper describes the progression of the IHFD between 2013 and 2018 and identifies trends and areas for improvement.
Methods
The IHFD is a clinically led, web-based audit, with data collected through the national Hospital Inpatient Enquiry (HIPE) electronic system, the principal source of information from publicly funded acute hospitals in Ireland. Eligible cases are aged ≥ 60 years with hip fracture as defined by IHFD or with other specified hip fracture excluding periprosthetic fractures. As of 2015, all 16 trauma-receiving hospitals within Ireland submitted data. Demographics and adherence to six national quality standards are described.
Results
A total of 17,983 cases were included in the analysis. National coverage has increased from 63% in 2013 to 99% in 2018. Demographic characteristics are unchanged, but higher levels of comorbidity are seen. Internal fixation and hemiarthroplasty are the most common modes of surgical repair with two-thirds of cases receiving spinal rather than general anaesthesia. Increasingly patients are being assessed by a geriatrician (11% in 2013 to 69% in 2018) and receive a bone health assessment (65% in 2013 to 84% in 2018).
Conclusion
While some hip fracture standards have improved, further improvements are required to compare favourably internationally. Reduction of surgical delay and ensuring early mobilisation post-operatively are immediate priorities for the IHFD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hip fracture is a common and serious consequence of falls among older people, with one in five dying in the first year [1]. In Ireland, approximately 3700 hip fractures occur annually due to injury in individuals over the age of 60 [2], and the age-standardised incidence rate is 4.4 and 1.8 per 1000 population in women and men, respectively. This is one of the highest rates in the world only slightly lower than the Scandinavian countries, Denmark, Sweden and Norway [3]. While the age-standardised incidence rate has declined since the year 2000 for females, the absolute number of all fragility fracture admissions increased in Ireland by 30% between 2000 and 2014 for men (40% increase) and women (27% increase), which is largely attributable to an ageing population. The number of hospitalisations for hip fractures is projected to increase threefold by 2046 with the proportion over the age of 85 projected to increase to 58% [4].
Over a 2-year period in Ireland, in comparison with their female peers, women with hip fracture have been found to have higher mortality, much higher institutionalisation rates and increased use of health and social care services [5]. Hip fracture also leads to dependence for many, with less than half regaining their previous level of function [6]. These injuries also have a significant economic burden. In Ireland, the estimated cost of one admission for hip fracture was €12,687 in 2014 [4].The costs of falls and fractures for people aged 65 years and older were estimated to be €404 million in 2004, making up an estimated 4.2% of all public health expenditure [7]. Efficient and high quality care has the potential to reduce the overall societal cost of hip fractures and reduce the rate of reoccurrence. Furthermore, evidence from the UK National Hip Fracture Database (NHFD; data collected from England, Wales and Northern Ireland) has shown that driving clinical improvement through national auditing of services can improve clinical outcomes and mortality after hip fracture [8].
The Irish Hip Fracture Database (IHFD) was established in 2012 with the goal of driving clinical and organisational improvements in the quality and effectiveness of hip fracture care locally and nationally and to monitor outcomes against international standards. It is a clinically led, web-based national audit, which is supported by the Irish Gerontological Society (IGS) and the Irish Institute of Trauma and Orthopaedic Surgery (IITOS) and is under the governance of the National Office of Clinical Audit (NOCA) [9]. In a European context, it built on the success of national hip fracture audits in Scandinavia and the UK and aligns itself with the minimum common dataset supported by the international Fragility Fracture Network (FFN) [10]. Currently, Ireland is one of at least 13 national hip fracture audit initiatives worldwide joining Sweden, Denmark, Finland, Norway, Germany, Netherlands, Italy, Spain, England, Wales and Northern Ireland (NHFD), Scotland (not included in the NHFD), the USA and (jointly) Australia and New Zealand [11]. The Irish audit has now published six annual reports and is comparable on the international stage with other national hip fracture audits [9].
Since the first report of the IHFD was published in 2013 [12], data coverage has improved every year. All 16 trauma-accepting acute hospitals in the country now submit data, and the coverage is 99% [9]. A Best Practice Tariff (BPT) system was introduced in 2018 to give financial imbursements to hospitals for meeting the clinical, data quality and governance standards for hip fracture care [2]. The aim of this paper is to describe the progression of the Irish Hip Fracture Database between the years 2013 and 2018 and to identify important trends and areas for improvement.
Methods
Irish Hip Fracture Standards
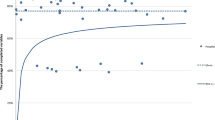
The Irish Hip Fracture Standards (IHFS) are the standards against which Irish hip fracture services are benchmarked. These standards evolved over time from the British Orthopaedic Association (BOA) and British Geriatric Society (BGS) “Blue Book” guidelines [13]. The IHFS are in alignment with the BPT for hip fractures, which focus on eight core measures; six clinical and two data quality and governance measures. These parameters are designed to improve the quality of care, clinical outcomes and cost-effectiveness of care post hip fracture (Fig. 1).
Identification of cases and data entry
The IHFD is a clinically led, web-based audit, whereby data is collected through an additional portal on the Hospital Inpatient Enquiry (HIPE) electronic system. The HIPE system is the principal source of demographic, clinical and administrative information on all discharges and deaths from publicly funded acute hospitals in Ireland and is managed by the national Healthcare Pricing Office (HPO) [14]. Each participating hospital in the IHFD has an audit coordinator and a clinical lead. The local audit coordinator identifies eligible cases by running a discharge report in the IHFD Portal. Additional cases may be identified manually.
Eligible cases include:
-
(i)
Cases diagnosed, on HIPE, with either a hip fracture due to injury specified by ICD-10-AM diagnosis codes S72.00 to S72.2 or with a specified type of fracture (e.g. intracapsular displaced, intracapsular undisplaced, intertrochanteric or subtrochanteric) other than periprosthetic
-
(ii)
Cases aged 60 years and over
At each hospital, the local audit co-coordinator enters data into the IHFD portal retrospectively based on individual patient records and in accordance with quarterly data collection targets (3 to 6 months after discharge). Comorbidity and physical status preoperatively are determined using the American Society of Anesthesiologists (ASA) physical status classification [15], and pre-fracture function is recorded with the New Mobility Score (NMS) [16, 17]. The timeline of events in hospital, time to orthopaedic ward, time to surgery and length of stay are also recorded. In cases where surgery was not performed within 48 h, a reason for delay is required, chosen from a pre-specified list of potential reasons. Data provided on post-operative care includes access to physiotherapy, specialist falls assessment and prescription of bone protection medication. The full list of variables collected in the audit including the year they were introduced is available in Supplemental Table 1.
Data anonymisation and quality
Data from the HIPE system are merged with additional IHFD data, and an extract is sent to the National Office of Clinical Audit from the HPO, with the cases anonymised. In the absence of a unique health identifier in Ireland, these records represent hospital encounters rather than individual patients. The IHFD data is assessed within the National Office of Clinical Audit using internationally agreed dimensions of data quality [18]. The IHFD updates the dataset annually to ensure that all data fields are relevant to the audit. Difficulty with specific data fields is addressed and monitored through continuous local and national data validation, monthly teleconferences and workshops with the audit coordinators and use of a data dictionary.
Analysis
Each of the 16 eligible hospitals within Ireland registered with the IHFD is currently submitting data. The descriptive analysis includes patients discharged from 1 January 2013 to 31 December 2018 inclusive. Data coverage is calculated as the proportion of cases identified as being eligible from HIPE records that are included in the audit.
Results
Coverage and demographics
A total of 17,983 cases were included in the analysis between 2013 and 2018. Table 1 shows how the coverage and demographics have changed over the audit period. National coverage of the audit has increased from 63% with 12 hospitals participating in 2013 to 99% with all 16 hospitals participating in 2018. There has therefore been a 92% increase in the number of cases included in the audit over 6 years and a 21% increase in hip fracture cases admitted nationally.
In total, 70% of cases were females. Overall, 13% of cases included in the audit were aged 60–69 years, 28% aged 70–70 years, 43% aged 80–89 and 15% aged 90 and older. The demographic characteristics of cases have not changed significantly within the 6 years of the audit. In total, 82% of cases were residing at home before their fracture. Table 1 shows how the proportion of patients admitted to another hospital prior to being transferred to the operating hospital has decreased from 13% in 2013 to just 6% in 2018. There was a high percentage of preoperative comorbidity among the patient population with 51% of patients with ASA scores recorded having an ASA grade of III (severe systemic disease that limits activity but is not incapacitating). There has been a trend towards increasing preoperative comorbidity among cases captured by the audit over 6 years; however, it must be noted that between 11 and 17% of cases did not have reported ASA scores in the IHFD.
Table 2 shows further clinical details of fractures and surgeries across the 6-year audit period. Most fractures (93%) were due to low energy trauma, which include falls from a height of less than 2 m, and at least 23% of cases had experienced a previous fracture. Figure 2 shows the frequency of the different fracture types, with intracapsular being the most common (50%). Of intracapsular fractures, over three quarters of them (76%) were displaced. Extracapsular fractures accounted for 44% of cases with 37% being intertrochanteric and 7% classed as subtrochanteric. The majority of cases were treated surgically (96%) with most receiving either internal fixation (48%) or hemiarthroplasty (47%) and almost two-thirds of cases receiving a spinal rather than general anaesthetic. Of cases with more than 48 h to surgery, 57% were due to medical reasons and a need for stabilisation.
In 2016, the audit began collecting data on pre-fracture functional mobility using the NMS and post-operative mobility using the Cumulative Ambulatory Score (CAS), both validated measures in patients with hip fracture [16, 17, 19, 20]. Over 3 years, 52% of cases with data recorded had low functional mobility (NMS 0–6), while 48% had an NMS score of 7 or more indicating high functional mobility [19]. Reporting of this variable has significantly improved, from 75% in 2016 to 93% in 2018. Over three quarters of cases since 2015 were mobilised on the day of or the day after surgery with the majority of cases being mobilised with a physiotherapist. Although there have been some improvements, there remains significant missing data for the CAS. In 2016, the CAS was completed for 41% of cases increasing to 60% in 2018. Over half of cases with CAS completed on the day after surgery have a score of 3, representing getting in and out of bed, standing and walking with assistance or verbal cueing from one or more persons [20].
Over the 6-year period, the mean length of stay was 19.7 days, decreasing from 21 days in 2013 to 18.7 days in 2018. There has been a decrease in the number of cases reported as been discharged directly to their home from 32% in 2013 to 20% in 2018, despite a slight increase in the number being admitted from home. In order to capture more accurate data on discharge destination, the IHFD introduced a new data field for this in 2016. In 2018, 31% of cases were discharged to a rehabilitation unit. Average inpatient mortality was 4.7% and has not changed over the audit period. Reoperation rate within 30 days is at least 1.4%, but for more than 10% of cases, this information was not recorded.
Hip fracture standards
Figure 3 shows the trend in the number of cases meeting the Irish Hip Fracture Standards over time. The most notable improvements have been seen in the number of cases being assessed by a geriatrician during their hospital stay (from 19% in 2014 to 69% in 2018) and receiving a bone health assessment (from 65 to 84%). The largest fluctuation from year to year has been seen in standard 6 (receiving a specialist falls assessment). The proportion of cases receiving surgery within 48 h ranged from 69 to 73% with 38 to 42% being conducted in the first 24 h. No consistent reduction in the time to surgery was seen over the audit period.
Discussion
This paper provides a summary of changes in hip fracture care and audit in the Republic of Ireland between 2013 and 2018, covering 17,983 individual cases. Using the key quality indicators set out in the Irish Hip Fracture Standards, improvements have been seen during the time period 2013–2018, particularly in relation to assessment of the need for bone protection and review by an orthogeriatrician. International evidence has shown that the synergy of care standards, audit and feedback drives measurable improvements in hip fracture outcomes for patients, including reduction in mortality [8, 21]. In 2018, hip fractures became the first condition to be eligible for a financial reward known as the Best Practice Tariff (BPT) in Ireland. For each patient who received care meeting all eight standards of care, €1000 was offered to the operating hospitals. Financial incentives have shown improvements in other health systems. Metcalfe et al. compared the data from England with that in Scotland, which does not provide BPT payments to hospitals and found that the BPT scheme saved up to 7600 lives in England between 2010 and 2016 and led to a reduction in hospital readmission [21].
Female patients and patients aged 80–89 years make up the majority of cases of hip fracture from a low energy trauma in Ireland. This is in line with international audits where approximately 70% are female and the average age is consistently above 80 years [11]. As the population ages, Ireland has observed a 21% increase over 6 years in the numbers of hip fractures nationally. For those included in the audit, there was an increase in the complexity of patients presenting with hip fracture. ASA grade III (severe systemic disease) admissions increased from 39% in 2013 to 46% in 2018. While this could be accounted for by changes in levels of data completeness and coverage, a large review of hip fracture care in Northern Ireland where there was over 97% completion of ASA grade found a significant increase in the degree of comorbidity over the last 15 years [21]. Currently, in the wider population, 65% of Irish adults over 65 years have two or more chronic conditions [22]. This has serious implications as the presence of three or more comorbidities in older individuals with a hip fracture has been shown to be a strong predictor of mortality (HR 2.5, 95% CI 1.6–3.9, p < 0.05) [23].
In 2018, 72% of patients were operated on within 48 h of admission, which is considerably fewer than in Sweden, Norway, Finland, Denmark and Scotland [11]. During the 6 years, the proportion has remained unchanged. This is despite the introduction of national bypass for hip fracture in 2017, whereby patients are brought directly to a hospital with an orthopaedic service that can provide surgery instead of to the nearest geographical hospital, which may not have that service [24]. This bypass has resulted in a steady reduction in admissions from other hospitals from 13% in 2013 to 6% in 2018. The lack of reduction in time to surgery is an ongoing challenge in Ireland, as adverse effects of delayed surgery in hip fracture are well established in the literature. The Danish National Indicator Project, which included 38,000 patients with hip fracture from 2003 to 2009, showed that after adjusting for age, sex, ASA grade and type of fracture, the risk of death in hospital and 30-day mortality increased with surgical delay (OR 1.30 per 24 h of delay) [25]. Similarly, a 2012 systematic review and meta-analysis reported that surgery within 48 h was associated with a lower risk of death (OR 0.74, 95% CI 0.67–0.81; p < 0.001) [26]. Early surgery has also been found to be associated with lower incidence of post-operative complications including pneumonia (RR 0.59, 95% CI 0.37–0.93, p < 0.02) and pressure sores (RR 0.48, 95% CI 0.34–0.69, p < 0.001) [27]. Work is continuing both nationally and locally within Irish hospitals to decrease surgical delays. Time to admission to an orthopaedic ward is a related standard to time to surgery. While 17% of cases were admitted or transferred to theatre within 4 h in 2018, this rate has not seen an improvement. It compares to 36% in the UK in 2018, where there has been a fall in this standard since 2015 [28]. Policies around prioritising direct operating theatre transfer from the emergency department have been introduced in several hospitals in Ireland in recent years, and this is an area for further development. Barriers to achievement of this standard locally, nationally and internationally require further investigation.
Surgical practices vary internationally, and the audit allows useful comparisons of standards. Most patients with hip fracture in Ireland receive spinal anaesthesia, but this practice varies internationally. Ireland’s pattern is similar to Norway and Spain, while in Australia, New Zealand and Germany, a larger proportion of general anaesthetics are administered [11]. Similarly, procedure types vary internationally according to other published audits, and Ireland’s practice appears most aligned with Norway and the UK. Other European countries and Australia and New Zealand report using intramedullary nails more frequently than other procedures [11]. Work is underway in the Irish audit to build a more detailed implant list into the database to facilitate further research.
As per recommendations from the International Fragility Fracture Network, prompt surgery should also allow immediate weight bearing in lower extremities and activities of daily living in upper extremities, to support optimal recovery of function [41]. The IHFD encourages and records data on early mobilisation. A recent analysis of the data from the IHFD showed that patients who were not mobilised on the day of or after surgery were 46% more likely to die in hospital than those patients who were mobilised early (OR 1.46, 95% CI 1.25–1.70, p < 0.001). In addition, patients who were independent in their mobility prior to hip fracture had a 16% reduction in odds of in-hospital mortality (OR 0.84, 95% CI 0.79–0.89, p < 0.001) [29]. While the proportion of patients recorded as having mobilised on the first post-operative day in Ireland is broadly in line with data from the NHFD and other European countries, it lags behind Australia and New Zealand [11, 28]. Furthermore, our interpretation of this variable is limited by high levels of missing data in the CAS score, which would quantify and ensure standardisation of the definition of “mobilisation”. From 2020, first-day mobilisation and CAS score recording will be prioritised as a new hip fracture standard in the IHFD. Prioritisation of post-operative mobility and recording of this measure will provide important information about potential barriers to early rehabilitation.
There is evidence that outcomes are improved for patients with hip fracture when their care is co-managed by an orthogeriatric team [30, 31]. Orthogeriatric assessment focuses on the rapid optimisation of patients’ pre- and post-operative repair, early identification of rehabilitation goals, secondary prevention of falls and fractures and integration with community services [32]. A recent UK population-based longitudinal study of more than 33,000 patients with hip fracture over 60 years of age showed the beneficial effect of orthogeriatric care on 30-day mortality (HR 0.73, 95% CI 0.65–0.82, p < 0.001) and 1-year mortality (HR 0.81, 95% CI 0.75–0.87, p < 0.001) [33]. A 2014 systematic review and meta-analysis also found that orthogeriatric care was associated with a significant reduction in time to surgery, in-hospital mortality and length of stay (standardised mean difference, − 0.25, 95% CI − 0.44–0.05, p < 0.001) [34]. Despite this evidence, in 2014, there was only one consultant orthogeriatrician appointed in Ireland. In 2020, there has been an increase in orthogeriatric service development to at least thirteen hospitals. The configuration of each of these services varies, and work is underway to further develop a minimum criterion for an orthogeriatric service definition. This has likely had an impact on improvements in several IHFS as observed in the audit most notably IHFS 4, 5 and 6. Orthogeriatric services are frequently linked to secondary prevention of falls and fractures. Given that 8.5% of patients with hip fracture go on to have a second hip fracture, frequently within the first year [35], these secondary prevention activities form part of essential care. While 70% of patients with hip fracture in Ireland received a specialist falls assessment in 2018, only 50% received this service between 2015 and 2017. This compares to 98% in England and 95% in Northern Ireland receiving a specialist falls assessment in 2018 [28]. Similarly the rate receiving a bone health assessment has improved from 65% in 2013 to 84% in 2018 but compares to over 95% in Northern Ireland [28]. Assessment of fracture risk and treatment of osteoporosis remains opportunistic in both primary and secondary care in the Republic of Ireland. Assessment with dual-energy X-ray absorptiometry (DXA) is not routinely available, and only seven of the 16 trauma units receiving fractures have a dedicated fracture liaison service [36]. Improvements are needed in fracture risk assessment and treatment in the general older population nationally to target both primary and secondary prevention.
Currently, the IHFD only reports data collected within the acute care setting. Collection of longer-term outcomes has been hindered to date by the absence of a unique health identifier or formal linkage between population datasets in Ireland [37]. This makes the interpretation of outcomes such as 1-year mortality, functional status and quality of life particularly challenging. However, in-hospital mortality can be accurately measured and has remained constant at approximately 5% in the IHFD cohort, which is comparable with Scotland (5%), Germany (5%), Australia (6%) and New Zealand (4%) [11]. In the NHFD, Norwegian and Danish databases, mortality is collected through death register linkage, and the 2016 reported 30-day mortality rates were 6.7%, 7.7% and 10%, respectively [1]. A recent systematic review found 22 individual studies conducted in Europe that reported 1-year mortality and calculated a mean of 23.3% (SD = 6.3%) [1], which is in line with the 1-year rate reported by the Norwegian database of 24%. The only study from Ireland included in this review was small and reported a low mortality rate of 9.7% [38]. A more recent analysis of local Irish data has reported a 1-year mortality rate of 24.7% among 541 patients followed up [39]. Reliable national longer-term mortality data in Ireland is required, and pursuing methods of collection is a priority for the IHFD [2]. Between 2013 and 2018, there was a decrease in the average acute length of stay for patients with hip fracture in Irish hospitals from 20 to 18.7 days. This remains long compared with other European countries [11]. Despite 71% of patients being admitted from home in 2018, only 20% were discharged directly home with the majority (31%) being transferred to a rehabilitation unit. Comparability of this data is affected by different rehabilitation pathways nationally, as well as internationally. Information on patients’ final discharge destination is not available although it is very important to patients. The perception of disability from falls, fractures or osteoporosis in older persons has been shown to result in individuals being willing to sacrifice approximately 9 months of life in order to return home rather than go to a nursing home [40]. More recently, a large cohort study in the UK (the WHiTE study) showed that routine collection of patient-reported outcomes is feasible and acceptable to patients and families [41]. Follow-up of patients’ functional ability, mobility and quality of life at fixed time points is essential to ensure equity of recovery. Collection of longer-term outcomes is a priority for the IHFD in line with international efforts [9].
Study limitations
This paper reports descriptive data on a national cohort of older patients with hip fracture in the Republic of Ireland. Suboptimal coverage and missing data in earlier years of the audit limit our ability to make strong conclusions about observed trends over the full 6-year period. Furthermore, as data is collected by multiple professionals across 16 sites in Ireland, there is the potential for variation in interpretation of variables in the context of local practices. This is minimised through central co-ordination of the audit, data validation protocols and continual education and support for data collectors. Rates and percentages reported are not adjusted for patient characteristics.
Conclusion
This paper describes key trends hip fracture care in Ireland from 2013 to 2018 using the IHFD. Ireland has observed a 21% increase in hip fracture numbers nationally, significant improvement in coverage of the audit and an increase in the complexity of cases recorded. Hip fracture standards including access to orthogeriatric care, falls and bone health assessments have improved over the course of the audit, but these require continued improvement to compare favourably internationally. Minimising surgical delay and ensuring early mobilisation post-operatively are immediate priorities for the IHFD. Future research will focus on the collection of information pertaining to longer-term mortality, functional status and health-related quality of life after hip fracture. In turn, this will allow the IHFD to monitor equity of outcomes for all patients with hip fracture in Ireland and will help inform future health policy.
Data availability
Data from the Irish Hip Fracture Database can be requested from the National Office of Clinical Audit, Ireland.
References
Downey C, Kelly M, Quinlan JF (2019) Changing trends in the mortality rate at 1-year post hip fracture - a systematic review. World J Orthop 10:166–175. https://doi.org/10.5312/wjo.v10.i3.166
National Office of Clinical Audit (2019) Irish Hip Fracture Database National Report 2018. National Office of Clinical Audit, Dublin
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C, on behalf of the IOF Working Group on Epidemiology Quality of Life (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256. https://doi.org/10.1007/s00198-012-1964-3
Kelly MA, McGowan B, McKenna MJ, Bennett K, Carey JJ, Whelan B, Silke C (2018) Emerging trends in hospitalisation for fragility fractures in Ireland. Ir J Med Sci 187:601–608. https://doi.org/10.1007/s11845-018-1743-z
Kirke PN, Sutton M, Burke H, Daly L (2002) Outcome of hip fracture in older Irish women: a 2-year follow-up of subjects in a case-control study. Injury. 33:387–391. https://doi.org/10.1016/s0020-1383(02)00025-6
Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE (1990) Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol 45:M101–M107. https://doi.org/10.1093/geronj/45.3.m101
Gannon B, O'Shea E, Hudson E (2008) Economic consequences of falls and fractures among older people. Ir Med J 101:170–173
Neuburger J, Currie C, Wakeman R, Tsang C, Plant F, De Stavola B, Cromwell DA, van der Meulen J (2015) The impact of a national clinician-led audit initiative on care and mortality after hip fracture in England: an external evaluation using time trends in non-audit data. Med Care 53:686–691. https://doi.org/10.1097/mlr.0000000000000383
Johansen A, Golding D, Brent L, Close J, Gjertsen JE, Holt G, Hommel A, Pedersen AB, Rock ND, Thorngren KG (2017) Using national hip fracture registries and audit databases to develop an international perspective. Injury. 48:2174–2179. https://doi.org/10.1016/j.injury.2017.08.001
Fragility Fracture Network (FFN) hip fracture audit database Minimum Core Dataset for hip fracture audit. Available from: http://web1.crownaudit.org/ffn/info.nsf/. Accessed 8th October 2019
Ojeda-Thies C, Saez-Lopez P, Currie CT et al (2019) Spanish National Hip Fracture Registry (RNFC): analysis of its first annual report and international comparison with other established registries. Osteoporos Int 30:1243–1254. https://doi.org/10.1007/s00198-019-04939-2
Ellanti P, Cushen B, Galbraith A, Brent L, Hurson C, Ahern E (2014) Improving hip fracture care in Ireland: a preliminary report of the irish hip fracture database. J Osteoporos 2014:656357–656357. https://doi.org/10.1155/2014/656357
British Orthopaedic Association (2007) The care of patients with fragility fracture (Blue Book). London, pp 8–11. Available from: https://www.bgs.org.uk/resources/care-of-patients-with-fragility-fracture-blue-book. Accessed 26th August 2020
Healthcare Pricing Office (2020) Hospital in-patient enquiry scheme (HIPE). Available from: www.hpo.ie. Accessed 26th March 2020
Dripps R, Lamont A, Eckenhoff J (1961) The role of anesthesia in surgical mortality. JAMA. 178:261–266. https://doi.org/10.1001/jama.1961.03040420001001
Fitzgerald M, Blake C, Askin D, Quinlan J, Coughlan T, Cunningham C (2018) Mobility one week after a hip fracture - can it be predicted? Int J Orthop Trauma Nurs 29:3–9. https://doi.org/10.1016/j.ijotn.2017.11.001
Parker MJ, Palmer CR (1993) A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg (Br) 75-B:797–798. https://doi.org/10.1302/0301-620X.75B5.8376443
Health Information and Quality Authority (2018) Guidance on a data quality framework for health and social care. Health Information and Quality Authority, Dublin
Kristensen MT, Bandholm T, Foss NB, Ekdahl C, Kehlet H (2008) High inter-tester reliability of the new mobility score in patients with hip fracture. J Rehabil Med 40:589–591. https://doi.org/10.2340/16501977-0217
Kristensen MT, Jakobsen TL, Nielsen JW, Jorgensen LM, Nienhuis RJ, Jonsson LR (2012) Cumulated ambulation score to evaluate mobility is feasible in geriatric patients and in patients with hip fracture. Dan Med J 59:A4464
Metcalfe D, Zogg CK, Judge A, Perry DC, Gabbe B, Willett K, Costa ML (2019) Pay for performance and hip fracture outcomes: an interrupted time series and difference-in-differences analysis in England and Scotland. Bone Joint J 101-b:1015–1023. https://doi.org/10.1302/0301-620x.101b8.Bjj-2019-0173.R1
Smyth B, Marsden P, Donohue F et al (2017) Planning for health: trends and priorities to inform health service planning 2017. Health Service Executive, Dublin
Roche JJ, Wenn RT, Sahota O, Moran CG (2005) Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 331:1374. https://doi.org/10.1136/bmj.38643.663843.55
Hughes AJ, Brent L, Biesma R, Kenny PJ, Hurson CJ (2019) The effect of indirect admission via hospital transfer on hip fracture patients in Ireland. Ir J Med Sci 188:517–524. https://doi.org/10.1007/s11845-018-1854-6
Mainz J, Krog BR, Bjornshave B, Bartels P (2004) Nationwide continuous quality improvement using clinical indicators: the Danish National Indicator Project. Int J Qual Health Care 16(Suppl 1):i45–i50. https://doi.org/10.1093/intqhc/mzh031
Moja L, Piatti A, Pecoraro V, Ricci C, Virgili G, Salanti G, Germagnoli L, Liberati A, Banfi G (2012) Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS One 7:e46175. https://doi.org/10.1371/journal.pone.0046175
Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, Debeer J, Bhandari M (2010) Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 182:1609–1616. https://doi.org/10.1503/cmaj.092220
HQIP/RCP Falls & Fragility Fracture Audit Programme (2020) National Hip Fracture Database - charts & reports. available from: https://www.nhfd.co.uk/20/NHFDcharts.nsf/fmDashboard?readform. Accessed 26th March 2020
Ferris H, Brent L, Coughlan T (2020) Early mobilisation reduces the risk of in-hospital mortality following hip fracture. Eur Geriatr Med 11:527–533. https://doi.org/10.1007/s41999-020-00317-y
Brent L, Hommel A, Maher AB, Hertz K, Meehan AJ, Santy-Tomlinson J (2018) Nursing care of fragility fracture patients. Injury. 49:1409–1412. https://doi.org/10.1016/j.injury.2018.06.036
Pioli G, Bendini C, Pignedoli P, Giusti A, Marsh D (2018) Orthogeriatric co-management - managing frailty as well as fragility. Injury. 49:1398–1402. https://doi.org/10.1016/j.injury.2018.04.014
Nicholas JA (2014) Preoperative optimization and risk assessment. Clin Geriatr Med 30:207–218. https://doi.org/10.1016/j.cger.2014.01.003
Hawley S, Javaid MK, Prieto-Alhambra D, Lippett J, Sheard S, Arden NK, Cooper C, Judge A (2016) Clinical effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: population-based longitudinal study. Age Ageing 45:236–242. https://doi.org/10.1093/ageing/afv204
Grigoryan KV, Javedan H, Rudolph JL (2014) Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma 28:e49–e55. https://doi.org/10.1097/BOT.0b013e3182a5a045
Zhu Y, Chen W, Sun T, Zhang Q, Liu S, Zhang Y (2014) Epidemiological characteristics and outcome in elderly patients sustaining non-simultaneous bilateral hip fracture: a systematic review and meta-analysis. Geriatr Gerontol Int 15:11–18. https://doi.org/10.1111/ggi.12368
National Office of Clinical Audit (2017) Irish Hip Fracture Database National Report 2016. National Office of Clinical Audit, Dublin
Department of Health (2013) eHealth strategy for Ireland. Available from: https://assets.gov.ie/16174/092e7c62f97b472b83cdb6dfdcdfd5c7.pdf. Accessed 9th April 2020
Henderson CY, Shanahan E, Butler A, Lenehan B, O'Connor M, Lyons D, Ryan JP (2017) Dedicated orthogeriatric service reduces hip fracture mortality. Ir J Med Sci 186:179–184. https://doi.org/10.1007/s11845-016-1453-3
Small C, Kneafsey S, McFeely A, O'Hanlon S, Cooney MT, Doyle R (2019) Hip fracture outcomes in the frail older person. Age Ageing 48:iii17–iii65. https://doi.org/10.1093/ageing/afz103.11
Robinson SM, Ni Bhuachalla B, Ni Mhaille B, Cotter PE, O'Connor M, O'Keeffe ST (2015) Home, please: a conjoint analysis of patient preferences after a bad hip fracture. Geriatr Gerontol Int 15:1165–1170. https://doi.org/10.1111/ggi.12415
Costa ML, Griffin XL, Achten J, Metcalfe D, Judge A, Pinedo-Villanueva R, Parsons N (2016) World hip trauma evaluation (WHiTE): framework for embedded comprehensive cohort studies. BMJ Open 6:e011679. https://doi.org/10.1136/bmjopen-2016-011679
Acknowledgements
We would like to acknowledge the Healthcare Pricing Office for facilitating and maintaining the IHFD dataset; the National Office of Clinical Audit for managing the IHFD, analysing data and producing annual reports; the Irish Gerontological Society and the Irish Institute of Trauma and Orthopaedic Surgery for their continued support of the audit, to the clinical leads, local hospital governance committees and especially to the audit co-ordinators at each hospital site for collecting the data and the National Irish Hip Fracture Database Governance committee.
Funding
The Irish Hip Fracture Database is supported by the National Office of Clinical Audit, which is funded by the Quality Improvement Team of the Health Service Executive. No additional funding supported the preparation of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethics approval
This study involved analysis of anonymous IHFD data which have been described in previously published annual reports. Formal ethical approval was not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 17.7 kb)
Rights and permissions
About this article
Cite this article
Walsh, M., Ferris, H., Coughlan, T. et al. Trends in hip fracture care in the Republic of Ireland from 2013 to 2018: results from the Irish Hip Fracture Database. Osteoporos Int 32, 727–736 (2021). https://doi.org/10.1007/s00198-020-05636-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05636-1