Abstract
New assessment guidelines for osteoporosis in Japan include the use of the WHO risk assessment tool (FRAX) that computes the 10-year probability of fracture. The aim of this study was to determine the distribution of fracture probabilities and to assess the impact of probability-based intervention thresholds in women from Japan aged 50 years and older. Age-specific simulation cohorts were constructed from the prevalences of clinical risk factors and femoral neck bone mineral density to determine the distribution of fracture probabilities as assessed by FRAX. These data were used to estimate the number and proportion of women at or above a 10-year fracture probability of 5, 10, 15, 20, 25, and 30 %. In addition, case scenarios that applied a FRAX probability threshold of 15 % were compared with current guidance. In the absence of additional criteria for treatment, a 15 % fracture probability threshold would identify approximately 32 % of women over the age of 50 years (9.3 million women) as eligible for treatment. Because of expected changes in population demography, the 15 % fracture probability threshold would capture approximately 38 % of women over the age of 50 years (12.7 million women), mainly those aged 80 years or older. The introduction of a FRAX threshold of 15 % would permit treatment in women with clinical risk factors that would otherwise fall below previously established intervention thresholds. The incorporation of FRAX into assessment guidelines is likely to redirect treatments for osteoporosis from younger women at low risk to elderly women at high fracture risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
FRAX® is a computer-based algorithm (http://www.shef.ac.uk/FRAX) that provides models for the assessment of fracture probability in men and women [1, 2]. FRAX uses easily obtained clinical risk factors to estimate fracture risk. The estimate can be made with the input of clinical risk factors alone or with bone mineral density (BMD). In addition to fracture risk, FRAX uses Poisson regression to derive hazard functions of death. These hazard functions, which are continuous as a function of time, permit the calculation of the 10-year probability of hip, clinical spine, humerus, or wrist fracture and the 10-year probability of hip fracture. Models need to be calibrated to the epidemiology of fracture and death in the intended country of use, and a FRAX model has been available in Japan since 2008 [3]. About 45,000 calculations of probability are made in Japan yearly on the website and many more on handheld calculators and from the output of densitometers.
A major application of FRAX® has been in the clinical assessment of patients and has prompted the revision of guidelines that are based wholly or partly on fracture probability [4, 5]. The use of FRAX in clinical practice demands a consideration of the fracture probability at which to intervene, both for treatment (an intervention threshold) and, in some countries, for BMD testing (assessment thresholds) [6]. Many approaches have been used to set intervention thresholds that depend critically on local factors such as reimbursement issues, health economic assessment, willingness to pay for health care in osteoporosis, and access to BMD [2, 6–15]. For this reason it is not possible or desirable to recommend a unified intervention strategy. Thus, the incorporation of FRAX into guidelines and the provision of intervention thresholds has been approached differently in different regions of the world, variously using a fixed probability threshold (e.g., USA, Canada, Sweden) or an age-dependent threshold (e.g., UK, Switzerland).
The Japanese Osteoporosis Society has recently revised its clinical guidelines for the assessment of osteoporosis; these include the use of FRAX thresholds [16]. A threshold probability of 15 % for a major osteoporotic fracture was included as one of several intervention thresholds. Against this background, the aim of the present report was to examine the potential burden of disease in the female population designated to be at high risk on the basis of FRAX probabilities of fracture.
Materials and methods
The probability calculations were made using FRAX (version 3.4) calibrated to the epidemiology of Japan [3]. All estimates were for the probability of a major osteoporotic fracture (clinical spine, hip, forearm, or humerus fracture). Femoral neck BMD was included in the calculations. Body mass index was set at 24 kg/m2, corresponding to the mean BMI of the Japanese cohorts used in the construction and validation of FRAX.
The distribution of probabilities in the postmenopausal Japanese population was undertaken using simulation samples of 10,000 women in each 5-year age interval from the age of 50 years. Simulations were used to provide age-specific data that reproduced the prevalences of the clinical risk factors (e.g., at the age of 65 years rather than in women aged 65 years or more). The estimates assumed that the distribution of the risk score and BMD was the same in Japanese women as that of the population-based cohorts used to synthesise the FRAX algorithms [17, 18]. Femoral neck BMD was converted to a T-score using the young female reference data published in the third National Health and Nutrition Examination Survey (NHANES III) [19].
These distributions were used to estimate the number and proportion of women at or above a 10-year fracture probability of 5, 10, 15, 20, 25, and 30 %. Simulations of greater numbers of women (up to 100,000) indicated that a population size of 10,000 at each age interval was robust in terms of comparing populations. The results for each age were then applied to the population of Japan. For population demography, we used data for 2010 supplied by the UN using the medium variant [20]. The same source was used to determine the extent that changes in the demography of the Japanese population over the next 25 years would affect the number of women designated to be at high risk as judged by FRAX probabilities.
We additionally estimated fracture probabilities in individual patient scenarios in the context of the existing assessment guidelines revised in the year 2000. In Japan, the criteria for the diagnosis of osteoporosis prepared by the Japanese Society for Bone and Mineral Research were based on BMD measurements expressed as a percentages of the young adult mean (YAM) for women [21, 22]. In women with no prior fragility fracture, a diagnosis of osteoporosis is made when BMD is <70 % of YAM. In patients with a previous fracture, osteoporosis is diagnosed when the BMD is <80 % of YAM. These diagnostic thresholds, derived by maximizing sensitivity and specificity for fracture detection, are also used as intervention thresholds. To compare intervention thresholds using YAM with probabilities derived from the FRAX algorithm, T-score equivalents were used. The T-score equivalent to 70 and 80 % of YAM for Japanese women was −2.7 SD and −1.8 SD, respectively, based on the NHANES III reference values for BMD at the femoral neck.
Results
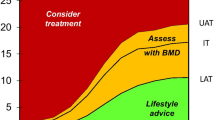
The impact of using different intervention threshold is shown in Fig. 1 for postmenopausal women in Japan. At high thresholds, e.g., ≥20 % fracture probability, 18.5 % of postmenopausal women would be eligible for treatment. A problem that arises is that very few women under the age of 60 years would ever attain this threshold (<1 %). On the other hand, if a less stringent threshold were chosen, such as 10 %, then approximately 5 % of women at the age of 50 years would exceed this threshold, and a majority of women over the age of 65 years would be eligible and the treatment threshold would be exceeded in 46 % of all postmenopausal women. Both scenarios are counterintuitive to clinical practice. In the absence of additional criteria for treatment, the 15 % threshold would identify approximately 32 % of women over the age of 50 years as eligible for treatment.
The impact of a fixed treatment threshold in postmenopausal women in the Japan according to threshold values for the probability of a major osteoporotic fracture. The left-hand panel shows the proportion of the postmenopausal population exceeding the threshold shown at each age. The right-hand panel shows the proportion of the total postmenopausal population that exceed a given threshold
The number of women with FRAX probabilities exceeding 15 % from the age of 50 years in 5-year age intervals is shown in Table 1. Of 29.7 million women aged 50 years or more, 9.3 million (31.5 %) had a FRAX probability of fracture that exceeded the 15 % threshold.
Future projections
In 2010, there were estimated to be 29.7 million women in Japan over the age of 50 years, representing 46 % of the total female population. The female population aged 50 years or more is projected to increase by 13 % to 33.7 million by the year 2035. However, the population growth is predominantly confined to the elderly. The growth in the female population aged 65 years or more is set to increase from 16.5 million in 2010 to 21.2 million in 2035, an increment of 29 %. The incremental increase will be even more marked for women over the age of 80 years (+90 %).
The increase in the mean age of the female population and the increase in the size of the elderly population are expected to increase the number of women with a fracture probability that exceeds 15 % in 2035. The total number of women aged 50 years or more above this threshold will rise by 3.3 million, from 9.3 million to 12.7 million. Most of the increase in number will be in the population aged 80 years or more.
Clinical scenarios
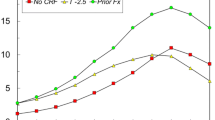
Fracture probabilities equivalent to intervention thresholds given in the year 2000 guidelines are shown in Fig. 2. Probabilities at the two intervention thresholds were very similar; they rose progressively with age up to the age of 80 years and then decreased because of the competing death hazard in the very elderly. From the age of 70 years, women eligible for treatment under the 2000 guidelines also had a fracture probability that exceeded 15 %. In contrast, below the age of 70 years women with no prior fracture and a less stringent T-score would be eligible for treatment if their fracture probability exceeded 15 %.
The 10-year probability of a major osteoporotic fracture at the intervention thresholds used in Japan. Intervention is recommended at a YAM of 70 % (a T-score of −2.7 SD at the femoral neck) or, in the presence of a prior fragility fracture, at a YAM of 80 % (a T score of −1.8 SD at the femoral neck). The horizontal line indicates a fracture probability of 15 % (FRAX 3.4, BMI set at 24 kg/m2, no additional clinical risk factors)
Table 2 shows some examples of the 10-year probabilities for a major fracture in women who would not be eligible for treatment under the 2000 guidelines. In women without a prior fracture and a YAM of 80 %, fracture probability did not exceed 15 % except at the age of 80 years. In contrast, in women with the same BMD and fracture status but in the presence of strong risk factors for fracture, a probability of 15 % or more was seen in all women from the age of 70 years. Thus, the introduction of a FRAX threshold of 15 % would permit treatment in women with clinical risk factors that would otherwise fall below an intervention threshold.
Discussion
The major application of FRAX is to assess fracture probability in individuals so that recommendations can be more accurately made with regard to the treatment of high-risk individuals, with unnecessary treatment avoided in those at low risk. The FRAX algorithms, particularly when used with BMD, improve the sensitivity of fracture prediction without sacrificing specificity over that provided by the use of BMD tests alone [18]. Notwithstanding, the application of FRAX to clinical practice requires the development of probability-based intervention thresholds, i.e., the 10-year fracture probability over which treatment can be recommended. As noted in the Introduction, there is no invariant method for their development because this will depend upon many local factors unique to each national setting. In the case of Japan, the Japanese Osteoporosis Society has adopted a fixed probability threshold in line with several other recent guidelines [8, 9, 13].
The present study quantifies the burden of disease in the Japanese female population according to FRAX and the implications of using a fixed intervention threshold. The principal finding is that with stringent thresholds (20 % probability or above), very few patients would be treated before the age of 65 years. At the other extreme, if a lax threshold is chosen, say 5 %, then 40 % of women at the aged 50–54 years would exceed this threshold, all women over the age of 75 years would be eligible, and the treatment threshold would be exceeded in nearly 80 % of all postmenopausal women. Both extremes are counterintuitive to clinical practice. Thus, the 15 % threshold provides a compromise between the undertreatment of younger individuals and the overtreatment of the elderly.
The present study estimates that there were 9.3 million women in Japan with a 10-year fracture probability that was 15 % or higher. The number is set to increase to 12.7 million by 2035. The estimate is conservative because this was based only on population demography and assumes, therefore, that the age- and sex-specific incidence remains unchanged in this interval. Empirical studies have shown that the hip fracture rates continue to increase in Japan [23, 24], whereas age- and sex-specific incidence has fallen in the past decade in several countries [25]. It is important to recognize that the proportion of the population with FRAX probabilities >15 % should not be misinterpreted to mean that this represents the population that would be targeted for treatment only on the basis of FRAX, because this will depend upon additional factors in the guidance provided, such as the T-score for BMD, prior fracture, and other eligibility criteria for assessment as provided in the new Japanese guidelines. Thus, the impact of new guidelines needs to take account of these additional criteria.
The present study also highlights the fact that populations eligible for treatment will differ when individuals are selected on the basis of densitometric criteria or on the basis of fracture probability. For example, women under the age of 70 years without clinical risk factors who are eligible for treatment by virtue of BMD have fracture probabilities that are less than the intervention threshold chosen of 15 % probability (see Table 2). Conversely, fracture probability will exceed 15 % in some women who would be ineligible for treatment using densitometric criteria alone. Such anomalies arise because of the imperfection of all assessment strategies. Nevertheless, the introduction of FRAX to guidelines is likely to improve the current strategy in targeting treatment to women at higher risk than before.
An important consideration in the use of FRAX is to determine whether patients identified to be at high risk with this tool are responsive to intervention. There is now increasing evidence for the reversibility of risk [26]. One line of evidence is from the phase III trials in which FRAX-based probabilities were calculated in post hoc analyses. These studies examined the interaction between FRAX-based probabilities with effectiveness. Two of these re-analyses of clinical trials data have shown greater efficacy against fracture in individuals at higher risk treated with clodronate or bazedoxifene [27, 28]. In a pre-planned analysis of the FREEDOM trial, greater efficacy against fracture was also shown in individuals at higher risk treated with denosumab [29]. In contrast, other studies have shown benefit of strontium ranelate or raloxifene across a range of fracture probabilities (with greater absolute risk reductions in those at higher risk) [30, 31]. For example, the efficacy of raloxifene does not change with fracture probability and reduces the risk of a clinical vertebral fracture by 50 % (95 % confidence intervals, 46–60), an effect comparable to that at a probability of 10 % (52 %: 95 % CI, 36–64) or 20 % (46 %: 95 % CI, 35–57). These randomized controlled trial (RCT) data strongly suggest that FRAX (with and without BMD) identifies high-risk patients who respond to pharmaceutical interventions.
These data are modeled on the demography and epidemiology of Japan, and the distribution of probabilities will vary from country to country. Thus, the present findings cannot be directly applied to other countries because of the large heterogeneity in demography, fracture risk, and mortality.
We conclude that a FRAX threshold of 15 % as an intervention threshold provides a compromise between the undertreatment of younger individuals and the overtreatment of the elderly. The incorporation of FRAX into assessment guidelines is likely to redirect treatments for osteoporosis from younger women at low risk to elderly women at high fracture risk.
References
Kanis JA on Behalf of the World Health Organization Scientific Group (2008) Assessment of osteoporosis at the primary health-care level. Technical Report. WHO Collaborating Centre, University of Sheffield, UK. http://www.shef.ac.uk/FRAX
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgström F, Odén A; National Osteoporosis Guideline Group (2008) Case finding for the management of osteoporosis with FRAX®: assessment and intervention thresholds for the UK. Osteoporos Int 19:1395–1408 (erratum 2009 Osteoporos Int 20:499–502)
Fujiwara S, Nakamura T, Orimo H, Hosoi T, Gorai I, Odén A et al (2008) Development and application of a Japanese model of the WHO fracture risk assessment tool (FRAX™). Osteoporos Int 19:429–448
Kanis JA, Oden A, Johansson H, Borgström F, Ström O, McCloskey E (2009) FRAX® and its applications to clinical practice. Bone (NY) 44:734–743
Kanis JA, Hans D, Cooper C, Task Force of the FRAX Initiative et al (2011) Interpretation and use of FRAX in clinical practice. Osteoporos Int 22:395–411
Compston J, Cooper A, Cooper C et al, on Behalf of the National Osteoporosis Guideline Group (NOGG) (2009) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas 62:105–108
Grossman JM, Gordon R, Ranganath VK et al (2010) American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken) 62:1515–1526
Papaioannou A, Morin S, Cheung AM et al (2010) 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ 182:1864–1873
Socialstyrelsen (2010) Nationella riktlinjer för rörelseorganens sjukdomar 2010—stöd för styrning och ledning. Preliminär version. Artikelnr 2010-11-15. http://www.socialstyrelsen.se
Czerwinski E, Kanis JA, Trybulec B, Johansson H, Borowy P, Osieleniec J (2009) The incidence and risk of hip fracture in Poland. Osteoporos Int 20:1363–1368
Kanis JA, Burlet N, Cooper C et al, on Behalf of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) (2008) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 19:399–428
Association Suisse contre l’Ostéoporose (2010) Ostéoporose: Recommandations 2010. ASCO http://www.svgo.ch/content/documents/SVGO_Empfehlungen2010_V19April2010.pdf
Dawson-Hughes B, National Osteoporosis Foundation Guide Committee (2008) A revised clinician’s guide to the prevention and treatment of osteoporosis. J Clin Endocrinol Metab 93:2463–2465
Neuprez A, Johansson H, Kanis JA et al (2009) Rationalisation du remboursement des médicaments de l’ostéoporose: de la mesure isolée de la densité osseuse à l’intégration des facteurs cliniques de risque fracturaire. Validation de l’algorithme FRAX®. La Revue Médicale de Liège 64:612–619
Lippuner K, Johansson H, Kanis JA, Rizzoli R (2010) FRAX® assessment of osteoporotic fracture probability in Switzerland. Osteoporos Int 21:381–390
Committee of Japanese Guidelines for the Prevention and Treatment of Osteoporosis (2012) The Japanese guidelines for the prevention and treatment of osteoporosis, 2011 edn. Life Science Publishing, Tokyo (in Japanese)
Johansson H, Kanis JA, Odén A, Johnell O, McCloskey E (2009) BMD, clinical risk factors and their combination for hip fracture prevention. Osteoporos Int 20:1675–1682
Kanis JA, Oden A, Johnell O et al (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18:1033–1046
Looker AC, Wahner HW, Dunn WL et al (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8:468–489
Population Division of the Department of Economic and Social Affairs of the United Nations. World Population Prospects: The 2008 Revision. http://esa.un.org/unpp
Orimo H, Sugioka Y, Fukunaga M et al (1998) Diagnostic criteria of primary osteoporosis. J Bone Miner Metab 16:139–150
Orimo H, Hayashi Y, Fukunaga M et al (2001) Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab 19:331–337
Hagino H, Katagiri H, Okano T, Yamamoto K, Teshima R (2005) Increasing incidence of hip fracture in Tottori Prefecture, Japan: trend from 1986 to 2001. Osteoporos Int 16:1963–1968
Hagino H, Furukawa K, Fujiwara S, Okano T, Katagiri H, Yamamoto K et al (2009) Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos Int 20:543–548
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA, IOF CSA Working Group on Fracture Epidemiology (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22:1277–1288
Kanis JA, McCloskey E, Johansson H, Odén A, Leslie WD (2012) FRAX® with and without BMD. Calcif Tissue Int 90:1–13
Kanis JA, Johansson H, Odén A et al (2009) Bazedoxifene reduces vertebral and clinical fractures in postmenopausal women at high risk assessed with FRAX. Bone (NY) 44:1049–1054
McCloskey EV, Johansson H, Odén A et al (2009) Ten-year fracture probability identifies women who will benefit from clodronate therapy—additional results from a double blind, placebo controlled randomised study. Osteoporos Int 20:811–818
McCloskey EV, Johansson H, Oden A et al (2012) Denosumab reduces the risk of all osteoporotic fractures in postmenopausal women, particularly in those with moderate to high fracture risk as assessed with FRAX®. J Bone Miner Res. doi:10.1002/jbmr.1606
Kanis JA, Jönsson B, Odén A, McCloskey EV (2011) A meta-analysis of the effect of strontium ranelate on the risk of vertebral and non-vertebral fracture in postmenopausal osteoporosis and the interaction with FRAX®. Osteoporos Int 22:2347–2355
Kanis JA, Johansson H, Odén A et al (2010) A meta-analysis of the efficacy of raloxifene on all clinical and vertebral fractures and its dependency on FRAX. Bone (NY) 47:729–735
Acknowledgments
The analysis used in this article was supported by a grant from Lilly, Japan. Lilly, Japan had no input into the analysis plan or in the writing of this report.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kanis, J.A., Johansson, H., Odén, A. et al. The distribution of FRAX®-based probabilities in women from Japan. J Bone Miner Metab 30, 700–705 (2012). https://doi.org/10.1007/s00774-012-0371-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-012-0371-3