Abstract
Summary
A country-specific FRAX® model was developed from the epidemiology of fracture and death in Belgium. Fracture probabilities were identified that corresponded to currently accepted reimbursement thresholds.
Introduction
The objective of this study was to evaluate a Belgian version of the WHO fracture risk assessment (FRAX®) tool to compute 10-year probabilities of osteoporotic fracture in men and women. A particular aim was to determine fracture probabilities that corresponded to the reimbursement policy for the management of osteoporosis in Belgium and the clinical scenarios that gave equivalent fracture probabilities.
Methods
Fracture probabilities were computed from published data on the fracture and death hazards in Belgium. Probabilities took account of age, sex, the presence of clinical risk factors and femoral neck bone mineral density (BMD). Fracture probabilities were determined that were equivalent to intervention (reimbursement) thresholds currently used in Belgium.
Results
Fracture probability increased with age, lower BMI, decreasing BMD T-score and all clinical risk factors used alone or combined. The 10-year probabilities of a major osteoporosis-related fracture that corresponded to current reimbursement guidelines ranged from approximately 7.5% at the age of 50 years to 26% at the age of 80 years where a prior fragility fracture was used as an intervention threshold. For women at the threshold of osteoporosis (femoral neck T-score = −2.5 SD), the respective probabilities ranged from 7.4% to 15%. Several combinations of risk-factor profiles were identified that gave similar or higher fracture probabilities than those currently accepted for reimbursement in Belgium.
Conclusions
The FRAX® tool has been used to identify possible thresholds for therapeutic intervention in Belgium, based on equivalence of risk with current guidelines. The FRAX® model supports a shift from the current DXA-based intervention strategy, towards a strategy based on fracture probability of a major osteoporotic fracture that in turn may improve identification of patients at increased fracture risk. The approach will need to be supported by health economic analyses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The diagnosis of osteoporosis is based on the measurement of bone mineral density (BMD) by dual X-ray absorptiometry (DXA). The World Health Organization has provided an operational definition of osteoporosis given as a BMD that lies 2.5 standard deviations (SDs) or more below the average mean value of young healthy women (T-score ≤ −2.5 SD) [1]. More recently, a standardised reference site (the femoral neck) and a standard reference range (the NHANES III data for women aged 20–29 years) [2] has been provided [3]. The operational definition of osteoporosis has been adopted by many agencies as one of the criteria for treatment [4–7].
Although low BMD is a major risk factor for fracture, many prospective studies have shown that, although fracture risk increases with decreasing BMD, most fractures occur in subjects with a BMD T-score above the operational threshold [8–10]. Recently, the use of clinical risk factors (CRFs) has been shown to enhance the performance of BMD in the prediction of hip and osteoporotic fractures in men and women [11]. In order to identify the CRFs for osteoporotic fracture, data were analysed from nine prospective primary cohorts and 11 prospective validation cohorts, including more than 275,000 persons corresponding to 1.4 million person-years with more than 22,711 reported fractures [11]. In addition to a prior fragility fracture, age, sex body mass index and additional risk factors for fractures were identified including the prior use of glucocorticoids, secondary osteoporosis, rheumatoid arthritis, a parental history of hip fracture, current cigarette smoking and alcohol intake of three or more units per day.
These analyses form the basis for the development of FRAX®, a computer-based algorithm (http://www.shef.ac.uk/FRAX) that provides models for assessment of fracture probability in men and women from the information provided from the CRFs [5, 12]. The 10-year fracture probability can be derived from the CRFs alone or with femoral neck BMD to enhance fracture risk prediction. In addition to the clinical risk factors, fracture probability varies markedly in different regions of the world [13]. Thus, the FRAX® models need to be calibrated to those regions where the epidemiology of fracture and death is known. At present, FRAX® models are available for Argentina, Austria, Belgium, China, Finland, France, Germany, Hong Kong, Italy, Japan, Lebanon, New Zealand, Spain, Sweden, Switzerland, Turkey, the UK and USA [12, 14–16], and several others are being developed.
In an earlier publication, the elements required to populate a Belgian-specific FRAX® model were reported [17]. The aim of this study was to describe a fracture probability model for Belgium. Given the current recommendations for treatment in Belgium, an additional aim was to determine which clinical risk factors, alone or in combination, and with or without a BMD measurement, might qualify for treatment in a Belgian environment.
Methods
Models were constructed to compute the 10-year probability of hip fracture and a major osteoporosis-related fracture in Belgium using the methodology previously described for the development of the FRAX® in the UK [12]. A major osteoporosis-related fracture was defined as a clinical spine, hip, proximal humeral or forearm fracture. Poisson models were used to calculate the hazard functions of fracture and death. The relationship between the hazard functions was used to calculate the 10-year probability or fracture for a combination of given risk factors. The mortality estimates for Belgium were those published by the World Health Organization for 1999 [18]. The incidence of hip fracture was taken from a previously published source [17]. Since the incidence of other fractures was not known in Belgium, we assumed that the age- and sex-specific ratio of index fracture to hip fracture in Belgium was the same as found in Sweden. This assumption, used in the development of several FRAX® models [5], appears to hold true for West European countries, the USA and Australia [19].
The relationship of clinical risk factors to fracture outcomes was assumed to be the same as that determined in a large meta-analysis of risk factors derived from prospectively studied population-based cohorts from Europe, Australia, North America and Asia. The independent contribution of each risk factor was used to compute probabilities of fracture in the absence of clinical risk factors or in the presence of any combination [11].
In Belgium, access to reimbursable treatment depends on the intervention envisaged and is largely predicated by price. Generic alendronate has no restriction for reimbursement in men and women. For branded bisphosphonates and raloxifene (in women), patients with a prior vertebral fracture and/or a T-score of less than −2.5 SD at the lumbar spine, total hip or femoral neck qualify for reimbursement using the Belgian normative reference ranges [20, 21]. For strontium ranelate, the same criteria are applied to women aged 80 years or older. More stringent criteria are applied to teriparatide in women. For the purposes of this report, we assessed fracture probabilities that were equivalent to a prior fragility fracture or a T-score of −2.5 SD for BMD at the femoral neck. The T-score was computed using the NHANES III as a reference for BMD at the femoral neck in Caucasian women aged 20–29 years [2]. The calculation of fracture probability was made at a body mass index (BMI) of 25 kg/m2 unless otherwise stated. Changes in BMI have little effect on predictive value for fracture risk assessment in the presence of BMD [22].
Results
Clinical risk factors
The contribution of clinical risk factors to fracture probability is shown in Table 1 for men and women with a BMI of 25 kg/m2. In women without clinical risk factors, the 10-year probability for an osteoporosis-related fracture was 3.4% at the age of 50 years and rose with age to 19% at the age of 90 years. The 10-year probability was higher in the presence of clinical risk factors. Smoking and alcohol were relatively weak risk factors; the use of long-term glucocorticoids of intermediate weight and a parental history of hip fracture or a prior fragility fracture were associated with the highest risks. At the age of 70 years for example, the 10-year probability was 11% for smokers and 18% for women with a prior fracture. Probabilities were consistently lower in men than in women.
BMD
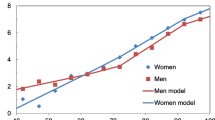
The 10-year probability of a major osteoporotic fracture for women without clinical risk factors is shown in Fig. 1 grouped by age and T-score. In women, the 10-year probability of fracture increased with age and with decreasing T-score up to the age of 80 years and then declined in women with the lower T-scores because of the competing effect of the death risk on fracture probability. At younger ages, the fracture probability was similar in men and women. For example, at the age of 50 years with a T-score of 1.0 SD, the probability of a major fracture was 2.4% in men and 2.9% in women. With advancing age, probabilities in men rose as expected at high T-scores, but decreased above the age of 80 years. At the extreme of T-score (−4.0 SD), probabilities decreased progressively with age because of the more marked competing effect of the death risk on fracture probability.
Intervention thresholds
Table 2 shows the fracture probabilities in women equivalent to the two thresholds for the reimbursement of treatments in Belgium. Thus, the levels of probability were equivalent either to a BMD set at a T-score of −2.5 SD in women without a previous fracture or to that in women with a previous fragility fracture. These probabilities are compared with women with no clinical risk factors in the absence of BMD (Table 2).
In women aged 50, 60, 70 and 80 years without clinical risk factors and with a BMD T-score of −2.5 SD, the 10-year probability of a major osteoporotic fracture was 6.7%, 9.3%, 13% and 15%, respectively. In women with no CRFs and no BMD tests, the equivalent probabilities were 3.4%, 5.7%, 9.6% and 16%, respectively. Thus, the BMD criterion for reimbursement using a fixed T-score became less and less appropriate with advancing age. For example, at the age of 50 years, women with a T-score of −2.5 SD had a two-fold higher probability than women of the same age and no CRFs. In contrast, at the age of 80 years and older, fracture probabilities were lower in women at the threshold of osteoporosis than their counterparts with no risk factors. The phenomenon was even more marked when hip fracture probabilities were considered (see Table 2). The situation arises because of the decrease in T-score that occurs with advancing age. Indeed, the average T-score at the age of 80 years is <−2.5 SD, so that a woman with a T-score of −2.5 SD has a higher-than-average T-score.
In women with a previous fracture, probabilities were consistently greater than in women at the threshold of osteoporosis and rose progressively with age up to the age of 85 years. This suggests that the probabilities equivalent to a prior fracture might be considered as a reference value above which patients could receive reimbursement for treatment in the absence of a prior fracture as indicated in Fig. 2.
Multiple clinical risk factors
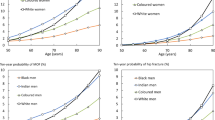
Each of the CRFs had an additive effect on fracture probability. For example, at the age of 65 years, the 10-year probability of hip fracture was 1.5% in the absence of CRFs with a BMI set at 25 kg/m2 (see Table 2). In the presence of one risk factor, this ranged from 2.0–3.7% depending on the weight of the risk factor. The mean and range increased progressively according to the number of CRFs, so that with four CRFs, the hip fracture probability ranged from 7.7–19% with a mean of 13%. Further examples are given in Fig. 3. Figure 3 also shows the effect of multiple risk factors in women of the same age at the threshold of osteoporosis. Mean hip fracture probabilities rose from 3.5% to 17%, depending on the number of CRFs.
10-year probability of hip fracture (%) in women aged 65 years according to the number of clinical risk factors. The left-hand panel shows the probabilities without BMD at a BMI fixed at 25 kg/m2. The right-hand panel illustrates the effects with BMD fixed at the threshold for osteoporosis. The bars indicate the mean value and the vertical lines denote the range of probabilities dependent on the weight of the risk factors [09Ca124]
As expected, probabilities of a major osteoporotic fracture also rose with increasing numbers of CRFs and ranged from 7.4% with no CRF to 54% with a combination of the four strongest risk factors (Fig. 3). The 10-year probability of a major fracture in women aged 65 years with a prior fracture was 15%. If this is taken as a reimbursement or treatment threshold, then, this threshold is exceeded in several scenarios of combinations. Indeed, with three or more CRFs, all possible combinations gave a fracture probability of 15% or more. A comparable effect was seen in the case of hip fracture probabilities using a threshold of 3.7%.
Examples of risk-factor pairs are given in Table 3 for women at the age of 60 and 80 years. At the age of 60 years, the reimbursement threshold was 12% for a major fracture. Several pairs of risk factors exceeded this threshold, despite no information on BMD. The threshold at the age of 80 years (26%) was exceeded in the majority of combinations.
In the presence of BMD, the intervention threshold was exceeded in women with no CRFs and a T-score of less than −2.9, −3.1, −3.5 and −4.2 SD at the ages of 60, 70, 80 and 90 years, respectively.
Discussion
The present study describes the FRAX® model for the assessment of fracture probability in men and women from Belgium. The model has been calibrated to the epidemiology of hip fracture that has recently been characterised for Belgium and has been recently added to the FRAX Web site (version 3.0; http://www.shef.ac.uk/FRAX/index.htm).
The strengths and limitations of FRAX have been extensively reported [5, 23], but the technology permits an estimate of fracture probability that integrates in a quantitative manner the information from multiple risk factors, with or without information on BMD. The inclusion of the risk factors improves the performance of assessment by increasing sensitivity (detection rate of who will fracture) without sacrificing specificity [11, 24].
Several previous studies have developed models to predict fracture risk from the combination of clinical risk factors and BMD [25–40]. The risk factors used include activities of daily living, impaired cognition, liability to falls, poor overall health, history of stroke, seizure disorder and several different medications. A limitation of many of these studies is that they have not been extensively tested in other cohorts. The model described in this paper has been validated in 11 independent prospectively studied cohorts with in excess of 1 million patient years [11]. Moreover, most other risk engines have not incorporated mortality, or incompletely so, and have not considered whether the risk factors used identify a risk that is reversible with intervention.
Many lines of evidence [41, 42] suggest that the FRAX® algorithms identify individuals in whom a high risk is responsive to pharmacological interventions. To test the hypothesis directly that a candidate risk factor identified a risk amenable to treatment, it would be necessary to recruit individuals selected on the basis of the risk factor(s) to a randomised controlled trial (RCT). The risk factor that is best evaluated in this way is BMD; and indeed the majority of therapeutic studies have recruited on the basis of low BMD as recommended by regulatory agencies in Europe [43]. In recent years, other trials have recruited on the basis of age, gender, a prior vertebral fracture and current exposure to glucocorticoids irrespective of BMD, and have shown therapeutic effects similar to those noted in RCTs based on BMD selection [44–46].
For other individual risk factors, comparable data are lacking, but several considerations suggest that the choice of these risk factors is appropriate in the context of identifying a reversible risk. First, several studies have shown that intervention in the general population induces therapeutic results similar to those expected in individuals selected to be at high risk [47–49]. Second, studies have shown no significant interaction between response to treatment and the presence or absence of the risk factors used in the present study including age, height, family history of fracture, low body weight or BMI, smoking, alcohol intake or prior non-vertebral fracture [50–54]. Third, the clinical risk factors are not totally independent of BMD, and when clinical risk factors alone are used in women aged 70 years or more, BMD is approximately 1 SD lower in the high-risk group compared with a low-risk group [55]. Perhaps, the best evidence is that response to intervention in elderly women recruited from the general population is greater, the higher the probability of fracture estimated without the inclusion of BMD in FRAX® [56]. Similar findings are reported for the SERM bazedoxifene. In this phase III intervention study, relative risk reduction compared with placebo was greater in women with the higher baseline fracture probabilities [57]. These considerations suggest that the risk factors chosen are appropriate in that they identify a risk that is amenable to pharmacological intervention.
Any clinical utility of FRAX® will be dependent on the manner by which probabilities are used to make clinical decisions on the management of patients. Practice guidelines or reimbursement criteria have been traditionally based on BMD thresholds [4–7]. However, the majority of fractures occur in individuals who would be considered to be at low risk on the basis of BMD alone [8–10]. If, for example, if it was considered appropriate to identify women in Sweden at the age of 65 years in the highest decile of risk, then 75% of all hip fractures would occur in those women categorised as being at low risk with a test with a gradient of fracture risk of 2.0 [10].
In this paper, we have explored a “translational approach” to guideline development by examining existing guidance and converting thresholds to fracture probabilities. The threshold chosen corresponds to a woman with a prior fragility fracture with an average BMD. This threshold will be marginally lower than the probability of the population with a prior fracture since a small segment of the population will have other FRAX® risk factors [41]. With this caveat, the present study shows that 10-year fracture probabilities equivalent to those currently accepted for reimbursement of treatment in Belgium are achieved with several clinical risk factor profiles and combinations. These include risk factors not (yet) accepted for reimbursement, such as a parental history of fracture, tobacco and/or alcohol abuse and rheumatoid arthritis. Thus, treatment is not equally accessible to all patients presenting with identical fracture risks. In this context, FRAX® represents a unique opportunity for identifying additional individuals who can benefit from treatment. FRAX® may also assist in identifying individuals at low risk but who would be eligible for treatment under existing arrangements. An example is provided in the present study in the use of BMD alone as a treatment threshold. If, for the sake of argument, it was considered appropriate to use the intervention threshold suggested in the present study, as has been recommended in several countries [15, 16, 58, 59], then, intervention would be recommended at the probabilities shown in Fig. 2. Under this scheme, women at the age of 55 years with a T-score of −2.5 SD and no clinical risk factors would have a fracture probability of 8.6% (see Table 2) which is close to the intervention threshold of 9.9%. By contrast, a woman at the age of 80 years with the same T-score would have a fracture probability (15%) very much lower than the intervention threshold (26%). Indeed, in this example, the fracture probability (15%) is similar to that of the general population of women at that age (16% without any CRFs). The reason is that the T-score diminishes with age so that at the age of 55 years, this T-score affords a substantial risk compared with women with an average T-score of the same age. At the age of 80 years, a T-score of −2.5 SD is higher than the average T-score for that age. Thus, the use of FRAX® can aid both in targeting treatments to individuals at high risk and by excluding individuals who would otherwise have received an inappropriate treatment. Both measures will improve the cost-effectiveness of case-finding.
We conclude that the FRAX® tool can be used to identify possible thresholds for therapeutic intervention in Belgium, based on equivalence of risk with current guidelines. The FRAX® model supports a shift from the current DXA-based intervention strategy, towards a strategy based on fracture probability of a major osteoporotic fracture that in turn may improve identification of patients at increased fracture risk. The approach will need to be supported by health economic analyses.
References
Kanis JA, Melton LJ 3rd, Christiansen C et al (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141
Looker AC, Wahner HW, Dunn WL et al (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8:468–489
Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ, Khaltaev N (2008) A reference standard for the description of osteoporosis. Bone 42:467–475
Kanis JA, Delmas P, Burckhardt P, Cooper C, Torgerson D, On behalf of the European Foundation for Osteoporosis and Bone Disease (1977) Guidelines for diagnosis and management of osteoporosis. Osteoporos Int 7:390–406
Kanis on behalf of the World Health Organization Scientific Group. JA (2008) Assessment of osteoporosis at the primary health-care level. Technical Report. WHO Collaborating Centre, University of Sheffield, UK.
European Community. Report on osteoporosis in the European Community. 1998. EC, Strasbourg
Royal College of Physicians (1999) Osteoporosis: clinical guidelines for the prevention and treatment. Royal College of Physicians, London
Kanis JA, Johnell O, Oden A et al (2000) Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone 27:585–590
Schuit SC, van der Klift M, Weel AE et al (2004) Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone 34:195–202
Kanis JA, Johnell O, Oden A et al (2000) Risk of hip fracture derived from relative risks: an analysis applied to the population of Sweden. Osteoporos Int 11:120–127
Kanis JA, Oden A, Johnell O et al (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18:1033–1046
Kanis JA, Johnell O, Oden A et al (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Oglesby A (2002) International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res 17:1237–1244
Dawson-Hughes B, Tosteson AN, Melton LJ 3rd et al (2008) Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int 19:449–458
Fujiwara S, Nakamura T, Orimo H et al (2008) Development and application of a Japanese model of the WHO fracture risk assessment tool (FRAX). Osteoporos Int 19:429–435
Lippuner K, Johansson H, Rizzoli R, Kanis JA (2009) Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporosis Int 20:1131–1140
Hiligsmann M, Bruyère O, Ethgen O, Gathon HJ, Reginster JY (2008) Lifetime absolute risk of hip and other osteoporotic fracture in Belgian women. Bone 43:991–994
United Nations population division (2003). World population prospects: the 2002 revision and world urban prospects. Population Division of the Dept Economic and Social Affairs of the UN Secretariat.
Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A (2001) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12:417–427
Boonen S, Kaufman JM, Reginster JY, Devogelaer JP, on behalf of the Belgian Bone Club (BBC) (2003) Patient assessment using standardized bone mineral density values and a national reference database: implementing uniform thresholds for the reimbursement of osteoporosis treatments in Belgium. Osteoporos Int 14:110–115
Goemaere S, Vanderschueren D, Kaufman JM, On behalf of the Belgian Bone Club (BBC), the Network on Male Osteoporosis in Europe (NEMO) et al (2007) Dual energy x-ray absorptiometry-based assessment of male patients using standardized bone density values and a national reference database. J Clin Densitom 10:25–33
De Laet C, Kanis JA, Oden A et al (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338
Kanis JA, Oden A, Johansson H, Borgström F, Ström O, McCloskey E (2009) FRAX® and its applications to clinical practice. Bone 44:734–743
Johansson H, Kanis JA, Oden A, Johnell O, McCloskey E (2009) BMD, clinical risk factors and their combination for hip fracture prevention. Osteoporos Int 20:1675–1682
Black DM, Steinbuch M, Palermo L et al (2001) An assessment tool for predicting fracture risk in postmenopausal women. Osteoporos Int 12:519–528
Burger H, de Laet CE, Weel AE, Hofman A, Pols HA (1999) Added value of bone mineral density in hip fracture risk scores. Bone 25:369–374
Albrand G, Munoz F, Sornay-Rendu E, DuBoeuf F, Delmas PD (2001) Independent predictors of all osteoporosis-related fractures in healthy postmenopausal women: the OFELY Study. Bone 32:78–85
Carroll J, Testa MA, Erat K, LeBoff MS, El-Hajj Fuleihan G (1997) Modelling fracture risk using bone density, age, and years since menopause. Amer J Prevent Med 13:447–452
Dargent-Molina P, Douchin MN, Cormier C, Meunier PJ, Bréart G, EPIDOS Study Group (2002) Use of clinical risk factors in elderly women with low bone mineral density to identify women at higher risk of hip fracture: the EPIDOS prospective study. Osteoporos Int 13:593–599
Girman CJ, Chandler JM, Zimmerman SI et al (2002) Prediction of fracture in nursing home residents. J Amer Geriatr Soc 50:1341–1347
Honkanen RJ, Honkanen K, Kröger H, Alhava E, Tuppurainen M, Saarikoski S (2000) Risk factors for perimenopausal distal forearm fracture. Osteoporos Int 11:265–270
Leslie WD, Metge C, Salamon EA, Yuen CK (2002) Bone mineral density testing in healthy postmenopausal women: the role of clinical risk factor assessment in determining fracture risk. J Clin Densitom 5:117–130, Erratum in: J Clin Densitom 2002;5:319
Miller PD, Barlas S, Brenneman S et al (2004) An approach to identifying osteopenic women at increased short-term risk of fracture. Arch Int Med 164:1113–1120
Westfall G, Littlefield R, Heaton A, Martin S (2001) Methodology for identifying patients at high risk for osteoporotic fracture. Clin Ther 23:1570–1588
Colón-Emeric CS, Pieper CF, Artz MB (2002) Can historical and functional risk factors be used to predict fractures in community-dwelling older adults? Development and validation of a clinical tool. Osteoporos Int 13:955–961
van Staa T-P, Leufkens H-GM, Cooper C (2002) Utility of medical and drug history in fracture risk prediction among men and women. Bone 31:508–514
van Staa TP, Geusens P, Pols HA, de Laet C, Leufkens HG, Cooper C (2005) A simple score for estimating the long-term risk of fracture in patients using oral glucocorticoids. Quart J Med 98:191–198
McGrother CW, Donaldson MM, Clayton D, Abrams KR, Clarke M (2002) Evaluation of a hip fracture risk score for assessing elderly women: the Melton Osteoporotic Fracture (MOF) study. Osteoporos Int 13:89–96
Walter LC, Lui LY, Eng C, Covinsky KE (2003) Risk of hip fracture in disabled community-living older adults. J Amer Geriatr Soc 51:50–55
Nguyen ND, Frost SA, Center JR, Eisman JA, Nguyen TV (2008) Development of prognostic nomograms for individualizing 5-year and 10-year fracture risks. Osteoporos Int 19:1431–1444
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey EV (2008) FRAX™ and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
Kanis JA, Oden A, Johansson H, Borgström F, Ström O (2009) McCloskey E (2009)FRAX® and its applications to clinical practice. Bone 44:734–743
Committee for Medicinal Products for Human Use (CHMP) (2006) Guideline on the evaluation of Medicinal products in the treatment of primary osteoporosis. Ref CPMP/EWP/552/95Rev.2. London, CHMP. Nov 2006.
Saag KG, Emkey R, Schnitzer TJ, Brown JP, Hawkins F, Goemaere S et al (1998) Alendronate for the prevention and treatment of glucocorticoid-induced osteoporosis. Glucocorticoid-induced Osteoporosis Intervention Study Group. New Engl J Med 339:292–299
Adachi JD, Saag KG, Delmas PD, Liberman UA, Emkey RD, Seeman E et al (2001) Two year effects of alendronate on bone mineral density and vertebral fracture in patients receiving glucocorticoids: a randomised, double-blind, placebo-controlled extension trial. Arthritis Rheum 44:202–211
Reginster JY, Minne HW, Sorensen OH et al (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral efficacy with risedronate therapy (VERT) study group. Osteoporos Int 11:83–91
Roussow JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML et al (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomized controlled trial. JAMA 288:321–333
McCloskey EV, Beneton M, Charlesworth D, Kayan K, deTakats D, Dey A et al (2007) Clodronate reduces the incidence of fractures in community dwelling elderly women unselected for osteoporosis: results of a double-blind, placebo-controlled randomized study. J Bone Miner Res 22:135–141
Chapuy MC, Arlot ME, Delmas PD, Meunier PJ (1994) Effect of calcium and cholecalciferol treatment for three years on hip fractures in elderly women. BMJ 308:1081–1082
Kanis JA, Barton I, Johnell O (2005) Risedronate decreases fracture risk in patients selected solely on the basis of prior vertebral fracture. Osteoporos Int 16:475–482
McCloskey EV, Selby P, Davies M et al (2004) Clodronate reduces vertebral fracture risk in women with post-menopausal or secondary osteoporosis: results of a double blind placebo-controlled 3 year study. J Bone Miner Res 19:728–736
Roux C, Reginster J-Y, Fechtenbaum J, Kolta S, Sawicki A, Tulassay Z et al (2006) Vertebral fracture with reduction with strontium ranelate in women with postmenopausal osteoporosis is independent of baseline risk factors. J Bone Miner Res 21:536–542
Marcus R, Wang O, Satterwhite J et al (2003) The skeletal response to teriparatide is largely independent of age, initial bone mineral density and prevalent vertebral fractures in postmenopausal women with osteoporosis. J Bone Miner Res 18:18–23
Johnell O, Kanis JA, Black DM et al (2004) Association between baseline risk factors and vertebral fracture risk in the Multiple Outcomes of Raloxifene Evaluation (MORE) study. J Bone Miner Res 19:764–772
Johansson H, Oden A, Johnell O, Jonsson B, De Laet C, Oglesby A et al (2004) Optimisation of BMD measurements to identify high risk groups for treatment—a test analysis. J Bone Miner Res 19:906–913
McCloskey EV, Johansson H, Oden A, Vasireddy S, Kayan K, Pande K, Jalava T, Kanis JA (2009) Ten-year fracture probability identifies women who will benefit from clodronate therapy—additional results from a double blind, placebo controlled randomised study. Osteoporos Int 20:811–818
Kanis JA, Johansson H, Oden A, McCloskey EV (2009) Bazedoxifene reduces vertebral and clinical fractures in postmenopausal women at high risk assessed with FRAX®. Bone 44:49–54
Johansson H, Kanis JA, Borgström F, Ström O, Svensson O, Mellström D (2009) FRAX® ett stöd för frakturprevention. Lakar Tidningen
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A, and the National Osteoporosis Guideline Group (2008) Case finding for the management of osteoporosis with FRAX®—assessment and intervention thresholds for the UK. Osteoporos Int 19:1395–1408, Erratum published 2009 Osteoporos Int 20, 499–502
Acknowledgements
This study is supported by a non-restricted grant from the International Osteoporosis Foundation and the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johansson, H., Kanis, J.A., McCloskey, E.V. et al. A FRAX® model for the assessment of fracture probability in Belgium. Osteoporos Int 22, 453–461 (2011). https://doi.org/10.1007/s00198-010-1218-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1218-1