Abstract
Introduction and hypothesis
Urinary incontinence (UI) and pelvic organ prolapse (POP) significantly decrease quality of life and sexual health. This study aimed to evaluate the reliability and validity of a Serbian adaptation of the short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ-12) used in assessing sexual function in women with UI and/or POP.
Methods
This study included 416 women, 310 (74.5%) with UI and/or POP and 106 (25.5%) without UI and/or POP. The adaptation of the PISQ-12 to Serbian language was performed via back-translation. The content validity of the questionnaire was conducted by experts in the field. The reliability and validity of the PISQ-12 were analyzed. Evaluation of the data was performed using Content Validity Index (CVI), Cronbach’s alpha, test-retest reliability, item total correlation and confirmatory factor analysis.
Results
Content validity of the Serbian PISQ-12 was 1.00 (100%). Item total correlations were between 0.459 and 0.819 (P < 0.001). The PISQ-12 had an adequate and high internal consistency (Cronbach’s alpha 0.806) as well as high test-retest reliability (Pearson correlation coefficient r = 0.807; P < 0.001). Factor analysis results revealed strong construct validity. The mean scores of PISQ-12 were significantly better in the control group compared with the women with UI and/or POP. Sexual function was negatively affected by UI and/or POP as assessed with SF-36 and I-QoL questionnaires.
Conclusions
This study showed that the Serbian version of the PISQ-12 is a reliable, consistent, valid and condition-specific instrument to assess sexual function in women with UI and/or POP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic floor disorders (PFDs) include pelvic organ prolapse (POP), stress urinary incontinence (SUI), urgency urinary incontinence (UUI), overactive bladder (OAB) and fecal or anal incontinence (FI, AI) [1]. The reported prevalence of PFD ranges between 23.7–46% in different populations [2, 3]. PFD negatively affects women's physical, psychological, social and sexual well-being. Contemporary results indicate that all urinary incontinence types are associated with low self-esteem and higher probability of psychiatric disease [4]. Multiple and different domains of sexual function were impaired in women with PFD. Between 53–83% of sexually active women with PFD have some form of female sexual dysfunction (FSD) [5, 6]. UI is associated with low libido, vaginal dryness and dyspareunia [5]. Many women may be avoiding sexual intercourse because of fear or shame of coital urinary incontinence [7,8,9].
Interestingly, most women with UI have not required help. Reasons given by women for not seeking help included: not regarding incontinence as abnormal or serious, considering incontinence to be a normal part of aging and having low expectations of treatment [10]. Similarly, women have difficulty speaking about sexual problems [11]. Due to the high frequency of the problem and the reluctance of women to address it, a reliable instrument for FSD assessment in women with UI and/or POP is needed.
Sexual function can be evaluated using generic and disease-specific questionnaires. Generic sexuality questionnaires such as the Female Sexual Function Index (FSFI) and the McCoy Female Sexuality Questionnaire (MFSQ) were designed to evaluate sexual function in a general population and can lack sensitivity in specific populations [12], such as urinary incontinence [13].
Disease-specific questionnaires can be used to assess patients with special medical conditions. The Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire short form (PISQ-12) is a validated, self-reporting, condition-specific quality-of-life questionnaire that investigates sexual function in heterosexual, sexually active women with UI and/or POP as well as sexual function after pelvic floor surgery and conservative treatment [14].
PISQ-12 was developed by Rogers et al. in 2003 with a view to assessing sexual functions that are specific to women with UI and/or POP [14]. In the past years, the PISQ-12 has been validated in French, Spanish, Turkish, Swedish, Portuguese, Chinese, Arabic, Persian and Dutch languages [15,16,17,18,19,20,21,22,23]. Although the psychometric properties of PISQ-12 by Rogers et al. are well documented in many languages [15,16,17,18,19,20,21,22,23], it is not available in Serbia, and since many women in Serbia, as in all societies, experience UI/POP and their negative impact on sexual health and health-related quality of life (HR-QoL) [5,6,7, 24], there is a significant need for a validated and reliable questionnaire. In fact, without condition-specific questionnaires, this problem will remain undetected in the clinical setting.
The aim of this study is to perform a transcultural adaptation and translation of the PISQ-12 to Serbian for use in everyday clinical practice and medical research.
Materials and methods
Questionnaire and scoring
The structure of the PISQ-12 questionnaire has three domains. It consists of 12 items, concerning emotional and behavioral factors (items 1–4), physical (items 5–9) and partner-related aspects (items 10–12). Behavioral-emotive domain includes questions about sexual desire, orgasm, sexual excitement and satisfaction with a variety of sexual activities. The physical domain evaluates frequency of pain during intercourse, coital urinary incontinence, avoiding sexual function because of prolapse and fear of urine or stool incontinence. The partner-related domain assesses erectile dysfunction, premature ejaculation and orgasm intensity. The Likert scale is used to grade responses that range from 0 to 4 indicating “never” to “always,” respectively. For items 1–4, inverse scoring is used. The final score is derived by summing together the responses to all 12 items where the maximum score possible is 48. Higher scores indicate better sexual function. PISQ-12 is a self-administered questionnaire that provides a single sexual function score [14].
Translation procedures
Before using PISQ-12 in this study, the researcher obtained permission from the PISQ author to translate and validate the questionnaire in Serbia. Two bilingual experts independently translated the questionnaire from English to Serbian. The translation was later reviewed by the translators and clinicians to confirm that the questionnaire is appropriate. In addition, ten incontinent women with or without POP were included during the translation phase to exclude semantic ambiguity. Following the translation field, two translators with no knowledge of the original PISQ-12 in English translated the Serbian version back into English, which was later compared with the original PISQ-12 to confirm accuracy and comprehension by another expert with only knowledge of English. Necessary modifications were made.
Study population and data collection
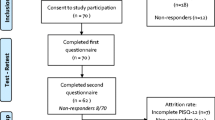
This cross-sectional study was conducted from January 2016 to October 2019 in University Clinic of Urology in Belgrade (a tertiary referral center) and the Department of Urology of the General Hospital in Vrbas (a secondary referral center). The control group included women without UI and/or POP from the University of Belgrade Faculty of Stomatology Clinic and blood donors at the Institute of Transfusion Medicine. A consecutive sample of female patients attending the Department of Urogynecology of the Clinic of Urology and the Department of Urology of the General Hospital was invited to participate in this study, which included 416 patients, 310 (74.5%) with UI and/or POP and 106 (25.5%) without UI and/or POP. Criteria for inclusion in the study were age > 18 years, sexually active within the past 6 months, not pregnant, able to read, write and understand the language and the presence of prolapse, urinary or fecal incontinence (or any combination). All included patients were those having their first visit for UI and/or POP and volunteering to participate in the study. Criteria for exclusion from the study were women with vesicovaginal fistula, history of pelvic/gynecological surgery or radiation, vulvodynia, painful bladder syndrome and chronic pelvic pain syndrome (defined as pelvic pain for > 6 months). In addition, women with functional disability and psychotic disorders including schizophrenia were excluded.
At first, 2 weeks from the initial completion of the questionnaire, 20 patients were asked to return to the clinic and complete the questionnaires again to evaluate internal consistency and test-retest reliability of the Serbian version. During this time, the patients were not given any treatment for symptoms to remain stable. After this pilot study, 416 participants were enrolled in the study. The participants completed the questionnaires in a private environment.
After patients completed the PISQ-12 questionnaire, they were examined by a physician who determined the type of their incontinence and any degree of POP via standardized assessment and POP-Q stage. The physician was blinded from the information obtained by the survey. Women with initial complaints of urinary incontinence underwent standardized assessment that included: history including assessment of bother, physical examination including a pelvic examination with POP-Q stage, objective demonstration of stress urinary incontinence with a comfortably full bladder in supine and standing position, ultrasound examination of the bladder with assessment of post-void residual urine, assessment of voluntary pelvic floor muscle contractility and urinalysis. Cystoscopy and urodynamic investigations were done in some selected cases. The definitions of International Continence Society were used to describe the symptoms, signs, urodynamic observations and conditions associated with lower urinary tract dysfunction [25]. The terminology of the International Urogynecological Association (IUGA)/International Continence Society (ICS) was used for staging prolapse [26]. The patient’s demographics and clinically significant information were collected and recorded.
The generic 12-item short-form health survey (SF-12) was used to assess the criterion validity of the PISQ-12 [27]. The SF-12 is a 12-question quality-of-life survey derived from the widely used health-related QOL questionnaire, the 36-item short-form health survey (SF-36) [28].
Ethics
The study was approved by Ethics Committee of the University Clinical Centre of Belgrade (no. 623/2). All participants provided written consent, and all participant information was kept confidential.
Statistical analysis
Data were described using mean, standard deviation, absolute numbers and percentages. The significance of difference was determined using Student’s t-test and Mann-Whitney U-test for numerical data. Pearson’s chi-square and Fisher’s exact tests were used for categorical data.
Internal consistency and test-retest reliability were evaluated to assess the reliability of the Serbian PISQ-12. The Cronbach’s alpha coefficient and intraclass correlation coefficient (ICC) were used to evaluate the internal reliability and test-retest reliability, respectively. Cronbach’s alpha values ≥ 0.70 were considered significant [29]. An ICC > 0.9 was considered excellent, > 0.8 acceptable, > 0.6 weak and ≤ 0.6 non-existent. A focus group and panel of patients and experts subjectively assessed the questionnaires for face/content validity to confirm that the questionnaire made sense to both the patients and experts and that all of the relevant domains were included. Spearman correlation was done to evaluate the criterion validity between the PISQ-12 and the I-QoL and SF36. SPSS version 26.0 (SPSS, Chicago, IL, USA) was used for statistical analysis, and the significance level was set to 0.05.
Results
The basic characteristics of the study group are presented in Table 1. Patients with incontinence are a few years older on average. Although groups significantly differed in body mass index (BMI), the clinical difference was small. Conversely, menopause and coital incontinence were significantly higher in the incontinence group. The average PISQ scores, total and in all three domains, were significantly lower in the incontinence group (Table 1).
Reliability analysis showed a high Cronbach’s alpha in the total sample, behavioral and emotional, and physical domains; however, a lower Cronbach’s alpha was obtained in the partner-related domain. In the latter, the range of alpha values of items deleted was very high, while in total and other domains was acceptable (Table 2).
The correlation matrix between PISQ (total, behavioral and emotive, physical and partner-related domains) with I-QoL and SF36 revealed a significant correlation between these scales. All correlations had a small to medium effect and were statistically significant (P < 0.001) (Table 3).
Factor analysis was used to assess the construct validity of the questionnaire. Factor analysis was set to eigenvalue > 1. Three factors were extracted, and the highest values in the line are in bold, with the exception of the last one (Table 4). The structure of the questionnaire has three domains, which are the same as described in the methodology. Questions 1–4 belong to the behavioral and emotional domain, 5–9 to the physical domain and three last questions to the partner-related domain. Test-retest was performed on 20 subjects. In total, correlation between PISQ on test and retest was high (r = 0.874; P < 0.001) as well as in each domain, behavioral-emotive (r = 0.918; P < 0.001), physical (r = 0.817; P < 0.001) and partner-related (r = 0.900; P < 0.001).
Discussion
This multicenter study provides greater diversity of patients in sociocultural terms because patients attending other centers may differ in terms of sociocultural conditions. When a quality-of-life instrument in the form of a questionnaire is translated from other previously validated languages, it is important to test the translated version for reliability and validity.
Patients in the study group were older, had higher BMI and parity and rate of complicated vaginal delivery, had a lower rate of cesarean section (CS) and were more frequently in menopause. All these are known risk factors for PFD.
Lower scores in total and in all three dimensions in the study group suggest that POP and UI are associated with higher probability of FSD. Nilsson et al. assessed the impact female UI and urgency on women and their partners's sexual life in sexually active couples. They reported that 22% of the men and 43% of the women stated that the female urinary symptoms impaired their sexual life [7]. Furthermore, Novi et al. reported a higher incidence of FSD in patients with POP with or without UI, but not all studies found this relationship [30].
The study showed that the Serbian version of the PISQ-12 has good internal consistency, with Cronbach’s alpha of 0.806. Studies validating PISQ-12 in other languages reported similar, acceptable values ranging from 0.712 to 0.898 [15,16,17,18,19,20,21,22], with an exception for the Dutch study, showing slightly lower values [23]. The internal consistency of the partner-related domain was lower than that of the total score and two other domains. Other authors reported similar findings in previous translations [17, 20, 23].
The reproducibility of the Serbian PISQ-12 was 0.874 for total score and 0.918, 0.817 and 0.900 within the three domains, behavioral-emotive, physical and partner-related domains, respectively. The ICC was 0.907 for the PISQ12 translated in Serbian. The values were comparable to those obtained in the Dutch and Swedish translations, which were 0.936 and 0.943, respectively. This shows that Serbian PISQ-12 can be used to distinguish the severity of FSD and follow the outcome of therapeutic treatments for PFD between patients.
The study showed a significant, small to medium correlation between PISQ-12 and previously validated Serbian versions of the I-QoL and SF-36.
Factor analysis confirmed the existence of three domains (emotional/behavioral, physical and partner-related). In the present study, item 12 (orgasm intensity) loaded in the emotional-behavioral domain, but had been identified as belonging to the partner-related domain in the original questionnaire [14]. We hypothesize that pain as an unpleasant sensation may influence emotional-behavioral aspects of women’s sexual life. Other studies identified item 12 as part of the emotional/behavioral domain [20, 22]. A possible explanation may be that intensity of orgasms is a complex entity influenced by not only partner-related factors, but also emotional and behavioral.
In conclusion, our study indicates that the Serbian version of the PISQ-12 is a valid tool for assessing sexual function in women with UI and/or POP. Given the results of our study, the Serbian PISQ-12 can be widely used in the Serbian population.
References
Hallock JL, Handa VL. The epidemiology of pelvic floor disorders and childbirth: an update. Obstet Gynecol Clinics. 2016;43(1):1–3.
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ. Pelvic Floor Disorders Network. Prevalence of symptomatic pelvic floor disorders in US women. Jama. 2008;300(11):1311–6.
Gyhagen M, Åkervall S, Milsom I. Clustering of pelvic floor disorders 20 years after one vaginal or one cesarean birth. Int Urogynecol J. 2015 ;26(8):1115–21.
Sinclair AJ, Ramsay IN. The psychosocial impact of urinary incontinence in women. Obstet Gynaecol. 2011;13(3):143–8.
Handa VL, Harvey L, Cundiff GW, Siddique SA, Kjerulff KH. Sexual function among women with urinary incontinence and pelvic organ prolapse. Am J Obstet Gynecol. 2004;191(3):751–6.
Roos AM, Thakar R, Sultan AH, Burger CW, Paulus AT. Pelvic floor dysfunction: women’s sexual concerns unraveled. J Sex Med. 2014;11(3):743–52.
Nilsson M, Lalos O, Lindkvist H, Lalos A. Female Urinary Incontinence and Urgency Impact on Women’s and Their Partners’ Sexual Life. In neurourology and urodynamics 2011 Jan 1 (Vol. 30, No. 6, pp. 940-941). commerce place, 350 main st, malden 02148, MA USA: Wiley-Blackwell.
Rogers GR, Villarreal A, Kammerer-Doak D, Qualls C. Sexual function in women with and without urinary incontinence and/or pelvic organ prolapse. Int Urogynecol J. 2001;12(6):361–5.
Tok EC, Yasa O, Ertunc D, Savas A, Durukan H, Kanik A. The effect of pelvic organ prolapse on sexual function in a general cohort of women. J Sex Med. 2010;7(12):3957–62.
Hägglund D, Walker-Engström ML, Larsson G, Leppert J. Reasons why women with long-term urinary incontinence do not seek professional help: a cross-sectional population-based cohort study. Int Urogynecol J. 2003;14(5):296–304.
Moreira ED, Glasser DB, Nicolosi A, Duarte FG, Gingell C, GSSAB Investigators’ Group. Sexual problems and help-seeking behaviour in adults in the United Kingdom and continental Europe. BJU Int 2008;101(8):1005-1011.
Espuña PM. Sexual health in women with pelvic floor disorders: measuring the sexual activity and function with questionnaires—a summary. Int Urogynecol J. 2009;20(1):65–71.
Omotosho TB, Rogers RG. Shortcomings/strengths of specific sexual function questionnaires currently used in urogynecology: a literature review. Int Urogynecol J. 2009;20(1):51–6.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J. 2003;14(3):164–8.
Fatton B, Letouzey V, Lagrange E, Mares P, Jacquetin B, De Tayrac R. Validation linguistique en français de la version courte du questionnaire sur la sexualité (PISQ-12) chez les patientes présentant un prolapsus génital et/ou une incontinence urinaire. J de gynécologie obstétrique et biologie de la reproduction. 2009;38(8):662–7.
Pons ME, Clota MP, Aguilón MG, Zardain PC, Álvarez PR. Cuestionario para evaluación de la función sexual en mujeres con prolapso genital y/o incontinencia. Validación de la versión española del “Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12)”. Actas Urol Esp. 2008;32(2):211–9.
Cam C, Sancak P, Karahan N, Sancak A, Celik C, Karateke A. Validation of the short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12) in a Turkish population. Eur J Obstet Gynecol Reprod Biol. 2009;146(1):104–7.
Teleman PI, Stenzelius K, Iorizzo L, Jakobsson UL. Validation of the Swedish short forms of the pelvic floor impact questionnaire (PFIQ-7), pelvic floor distress inventory (PFDI-20) and pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Acta Obstet Gynecol Scand. 2011;90(5):483–7.
Santana GW, Aoki T, Auge AP. The Portuguese validation of the short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J. 2012;23(1):117–21.
Zhu L, Yu S, Xu T, Yang X, Lu Y, Lang J. Validation of the Chinese version of the pelvic organ prolapse/urinary incontinence sexual questionnaire short form (PISQ-12). Int J Gynecol Obstet. 2012;116(2):117–9.
Shaaban MM, Abdelwahab HA, Ahmed MR, Shalaby E. Assessment of female sexual function among women with pelvic organ prolapse or urinary incontinence via an Arabic validated short-form sexual questionnaire. Int J Gynecol Obstet. 2014;124(1):24–6.
Zohre M, Minoo P, Ali M. Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12): psychometric validation of the Iranian version. Int Urogynecol J. 2015;26(3):433–9.
t Hoen LA, Utomo E, Steensma AB, Blok BF, Korfage IJ. The pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12): validation of the Dutch version. Int Urogynecol J. 2015;26(9):1293–303.
Asoglu MR, Selcuk S, Cam C, Cogendez E, Karateke A. Effects of urinary incontinence subtypes on women's quality of life (including sexual life) and psychosocial state. Eur J Obstet Gynecol Reprod Biol. 2014;1(176):187–90.
Abrams P. Standardisation Sub-committee of the International Continence Society. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:167–78.
Haylen BT, De Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodynam: Off J Int Continence Soc. 2010;29(1):4–20.
PROQOLID Patient-Reported Outcome and Quality of Life Instruments Database. SF-12v2 Health Survey Serbian version. https://www.qolid.org.
PROQOLID Patient-Reported Outcome and Quality of Life Instruments Database. SF-36 Health Survey Serbian version. https://www.qolid.org.
Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334.
Novi JM, Jeronis S, Morgan MA, Arya LA. Sexual function in women with pelvic organ prolapse compared to women without pelvic organ prolapse. J Urol. 2005;173(5):1669–72.
Author information
Authors and Affiliations
Contributions
Dj. Nale: Project development, Management, Data analysis, Manuscript writing/editing
V. Skoric: Project development, Data collection, Data analysis
P. Nale: Data collection, Data analysis, Manuscript writing
U. Babic: Data collection, Data analysis
M. Petrovic: Interpretation of data, Statistical analysis, Manuscript writing/editing
I. Radovic: Interpretation of data, Statistical analysis, Manuscript writing
J. Markovic: Interpretation of data, Statistical analysis, Manuscript writing
I. Soldatovic: Interpretation of data, Statistical analysis, Manuscript editing
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Nale, D., Skoric, V., Nale, P. et al. Validation of the Serbian version of the Pelvic Organ Prolapse/Urinary Incontinence/Sexual Questionnaire short form (PISQ-12). Int Urogynecol J 33, 3177–3184 (2022). https://doi.org/10.1007/s00192-022-05288-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05288-1