Abstract
Introduction and hypothesis
We have previously reported on laparoscopic hysteropexy for uterine prolapse. We now report a pilot randomized study comparing laparoscopic hysteropexy (LH) with vaginal hysterectomy (VH) for the surgical management of uterine prolapse.
Methods
Women with symptomatic uterine prolapse requiring surgery for uterine prolapse were recruited. The data were analyzed for those who had completed a 1-year follow-up. As this is a pilot randomized study, no power calculation was available. The main primary outcome measure was repeat apical prolapse. Secondary outcomes included operation data, complications, recovery time, functional and QoL outcomes, and anatomical outcomes. Wilcoxon signed rank and Mann–Whitney tests compared pre-operative with post-operative data and the difference between the two groups respectively.
Results
One hundred and thirty-two women were recruited. Of these, 101 were randomized. Eighty percent of the 31 women who dropped out preferred LH. One-year follow-up data were analyzed for 37 women in the LH and 35 women in the VH group. Time before return to normal activity was significantly shorter, estimated blood loss was significantly less, pain score 24 h post-operatively was significantly lower, and hospital stay was significantly shorter in the hysteropexy group compared with the vaginal hysterectomy group. Operation time was significantly longer in the hysteropexy group. Both procedures showed significant improvement in prolapse symptoms. Hysteropexy was associated with better apical support; point C and total vaginal length were significantly improved. More vaginal repairs were subsequently required post-hysteropexy.
Conclusions
Laparoscopic hysteropexy is a safe surgical alternative to vaginal hysterectomy with a similar risk of repeat apical surgery at 1 year. Longer follow-up data from larger studies are required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse is prevalent and is one of the most common reasons for gynecological surgery [1, 2]. Surgical outcomes are frequently poor with high rates of recurrent surgery [3, 4].
The surgical option for uterine prolapse has traditionally been vaginal hysterectomy, with and without vault suspension. However, hysterectomy removes a healthy, albeit poorly supported organ. It fails to tackle pathological connective tissue weakness, primarily the uterosacral and cardinal ligaments, and this contributes to the subsequent high apical prolapse rates seen with this operation [3–5].
The concept of uterine preservation at the time of uterovaginal prolapse surgery has become more popular. A variety of vaginal, abdominal, and laparoscopic techniques have been described with varying success rates [6]. These procedures preserve fertility in women of reproductive age, but also have the potential to significantly improve the symptoms of prolapse, psychological wellbeing, and sexual function. Furthermore, they may also have the potential to reduce the risk of apical prolapse recurrence by using non-absorbable materials to reinforce weakened connective tissues and ligaments.
Laparoscopic uterine preservation surgery has developed with advances in laparoscopic surgery. The Oxford laparoscopic hysteropexy technique used in this study has been previously reported; early and intermediate observational prospective studies have shown that it is an effective and safe operation for uterine prolapse preservation surgery [7–9].
To date, there have been no randomized studies comparing the outcomes of laparoscopic uterine suspension (hysteropexy) with conventional vaginal hysterectomy. We now report 1-year follow-up data from a randomized study comparing the rates of recurrent prolapse surgery of the two procedures. We also report data comparing subjective and objective outcome in addition to complications and recovery from surgery.
Materials and methods
Trial design
This was a single-center, pilot balanced, randomized controlled study of two parallel groups, conducted in the United Kingdom.
Participants
Women attending the gynecology clinic at a tertiary referral urogynecology unit in Oxford, UK, requesting surgical treatment for grade 2–4 symptomatic uterine prolapse were offered participation in a randomized trial, over a 3-year period between May 2009 and September 2012. Requirements for women recruited were that they were over 18 years of age with no desire to preserve fertility. Women with abnormal cervical cytology and abnormal uterine bleeding were excluded. Women with a significantly enlarged fibroid uterus or concomitant medical problems precluding general anesthesia or the use of a steep Trendelenberg position were also excluded. Subjects who agreed to participate in principle were given further information about the trial and consent was obtained either in an outpatient clinic or at the next visit for pre-operative assessment.
Interventions
Subjects participating in the study were randomly assigned to either of two groups: group A, laparoscopic hysteropexy (LH), or group B, vaginal hysterectomy (VH).
Those recruited who subsequently had a strong preference for either operation, and consequently declined to continue in the study, were excluded and were not randomized. On the day of the operation allocation was confirmed and appropriate consent was obtained for the specific surgical procedure.
Surgery was performed under general anesthesia by the senior authors or by the urogynecology sub-specialty trainee under their direct supervision. All surgeons, including the trainee, had extensive prior experience of performing both operations, having performed over 50 cases of either procedure prior to performing surgery in the trial. Vaginal hysterectomy and laparoscopic hysteropexy were combined with anterior and/or posterior repair depending on the judgment of the surgeon at the time of the operation. In the vaginal hysterectomy group, the uterosacral ligaments were reattached with re-absorbable sutures (Vicryl 1; Ethicon, Somerville, NJ, USA) to the vaginal vault after hysterectomy at the time of vault closure. This was chosen as the method of vault support as it is the most common technique employed in the UK [10]. In cases of complete procidentia, additional vault support was obtained by sacrospinous fixation with re-absorbable sutures (PDS II 0; Ethicon), again mirroring common UK practice and complying with Royal College of Obstetrician and Gynaecologist (RCOG) recommendations [11].
Laparoscopic hysteropexy was performed, after creating a pneumoperitoneum, via four laparoscopic ports. The peritoneum was opened over the sacral promontory and right pelvic sidewall between the ureter and rectum toward the pouch of Douglas [7]. Each broad ligament at the level of the cervico-uterine junction was also opened through the avascular area and the bladder dissected distally. Then, the uterus was suspended from the sacral promontory using a bifurcated polypropylene type-1 monofilament macroporous non-absorbable mesh (ProLiteTM Atrium Medical Corporation, Hudson, NH, USA), which, prior to sacral fixation, was wrapped around the cervix, via the broad ligament windows created. The two arms of the mesh were transfixed anterior to the cervix with three non-absorbable polyester 2–0 sutures (Ethibond ExcelTM; Ethicon). The mesh is completely re-peritonealized to reduce the risk of bowel adhesions. The procedure was fully described and also presented as a video article in previous publications [7–9].
Outcomes
The women’s prolapse symptoms and their impact were evaluated before surgical treatment. A subjective assessment of the prolapse was made using the International Consultation on Incontinence Questionnaire for Vaginal Symptoms (ICIQ-VS) [12]. This is a validated questionnaire measuring vaginal prolapse symptoms and their impact. The ICIQ-VS has been shown to effectively measure change in symptoms pre- and post-treatment [12].
Objective assessment of pelvic organ prolapse was performed during a Valsalva maneuver, in the left lateral position, using a Sims’ speculum. The pelvic organ prolapse quantification (POP-Q) [13] scale was used to grade the degree of prolapse at all sites. Where indicated, further assessments of pelvic organ function, such as urodynamic bladder studies, were performed.
Each woman was followed up initially in the clinic 2–3 months post-surgery as part of departmental routine. They were then invited for review, as part of the trial, at a dedicated clinic, 1 year following surgery. Vaginal prolapse was assessed again using the ICIQ-VS questionnaire and the POP-Q examination.
During the interview, further questions were asked regarding post-operative recovery, current urinary symptoms, and their satisfaction with the operation. Subjective surgical outcome was measured using the Patient Global Impression of Improvement (PGI-I), which is a validated tool as a global index of response to prolapse surgery [14]. The PGI-I is a seven-scale response for women comparing the post-operative condition with the pre-operative state, 1 being very much better and 7 being very much worse [14]. The PGI-I score is recommended by the IUGA/ICS joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse [15].
The measure for primary outcome was treatment failure defined as recurrent apical prolapse surgery required within the first year post-operatively. The secondary outcome measures were change in anatomy quantified by POP-Q and symptoms quantified using the ICIQ-VS questionnaire scores for prolapse, sexual wellbeing, quality of life, and PGI-I score. Other secondary outcome measures were operation time, blood loss, hospital stay, and time before return to normal activity.
Randomization
The trial protocol was approved by the National Research Ethics committee (reference number: 09/H0606/28). All participants were given written information on the study, and gave informed signed consent before random assignment to either of the two operations. Simple randomization was performed by blind envelopes to allocate the patient into group A for LH or group B for VH. This was performed prior to admission for surgery. As this is a first randomized study, no power calculation was available.
Statistical analysis
Descriptive statistics were used for the whole population. To compare the difference between the means of scores pre- and post-operatively, a Wilcoxon signed rank test was used. A Mann–Whitney test was used to compare the difference between the two surgical groups. The significance level was set as p < 0.05. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) 20.0 for Mac. All method definitions and units conform to the standards jointly recommended by the IUGA and the ICS, except where specifically noted [16, 17].
Results
A total of 481 women seen with symptomatic uterine prolapse stages 2–4 who desired surgery during the period May 2009 to September 2012 were approached to participate in the study. One hundred and thirty-two women were recruited. Some women met the exclusion criteria, but many women declined participation as they had a strong desire for one type of surgery, usually hysteropexy.
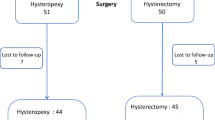
A further 31 women dropped out after recruitment, but prior to randomization as they also had a strong desire for one type of surgery. Of these 31 women, 6 preferred VH and 25 women wanted LH. The trial profile of enrolment and randomization is summarized in Fig. 1.
One woman who was randomized to LH had to be converted to VH owing to low bifurcation of the aorta, which made access to the sacral promontory unsafe. She was excluded from the trial.
Patient demographics, degree of uterine prolapse, and concomitant surgery in each group are summarized in Table 1. There were no significant differences in the demographics between the two groups. In women undergoing VH, 98 % had a concomitant vaginal pelvic floor repair, compared with 82 % in the LH group. Those with stage 4 prolapse had a sacrospinous fixation with VH (Table 1).
There were no major intraoperative complications in either of the groups. Duration of operation was significantly shorter in the VH group with a mean difference of 11.4 min (p < 0.001). The time did not include any concomitant surgery such as pelvic floor repair or sacrospinous fixation, but includes vault closure in the VH group. The estimated blood loss was significantly less, number of nights in hospital significantly fewer, 24-h post-operative pain score was significantly lower, and time before return to normal activity was significantly shorter in the LH group compared to with the VH group (p < 0.05; Table 2).
Data on repeat prolapse surgery following the initial primary prolapse repair are presented in Table 3. Those who did not attend the 1-year follow-up had their hospital notes reviewed for evidence of repeat surgery during the 1st year post-operatively. At the time of review 4 women had undergone laparoscopic sacrocolpopexy in the VH group and another 3 were booked to have the operation. In the LH group, 3 women had undergone a further apical operation in the form of laparoscopic plication of the mesh or cervical amputation (Table 3). Laparoscopic plication of mesh involves shortening the mesh by folding it onto itself with nonreabsorbing sutures. None of the women having a VH needed further vaginal repair, but there were 2 who had undergone a subsequent repair and a further 3 were booked for repair in the LH group. p values for repeat operation, and combined repeat and requiring further operation at 1-year review were obtained (Table 3).
Excluding those women who had repeat apical surgery, 1-year follow-up data were obtained for 37 women in the LH group and 35 women in the VH group. One-year data for ICIQ-VS and POP-Q assessment of prolapse are summarized in Table 4. There was a significant improvement of all parameters when comparing pre-operative with post-operative data for the two groups. There was no significant mean difference in ICIQ-VS between the two groups. A significant difference was noted in two of the POP-Q parameters; point C was more elevated in the LH group and the total vaginal length was shorter in the VH group (Table 4).
The PGI-I was very similar in both groups, with 82 % of subjects in the LH group very much/much better with their prolapse symptoms, compared with 87 % in the VH group at 1-year follow-up. Of those who completed 1-year follow-up, 89 % of women in the VH group recommended their primary prolapse operation to other women with prolapse, whereas 78 % in the LH group recommended the operation.
Although it was not part of the study methodology, the author assessing patients at 1 year evaluated subjects about their urge and stress urinary incontinence symptoms. Women who had symptoms of stress incontinence in the LH group (n = 14) and VH group (n = 13), and did not undergo concomitant continence surgery, reported subjective improvement or cure of their stress incontinence in 86 % of the LH group compared with 39 % in the VH group. As regards urge incontinence in the LH group (n = 24) and VH group (n = 26), subjective improvement of urge incontinence was reported in 58 and 31 % respectively. The urinary questions were asked post-operatively and not verified with pre- and post-operative validated questionnaires.
There were no major intraoperative complications in either of the groups. No vaginal mesh exposure or any other mesh complications were observed in any of the women undergoing LH. In the VH group one of the women without post-menopausal bleeding was found to have a coincidental stage 1A mucinous endometrial carcinoma.
Discussion
Main findings
Both laparoscopic hysteropexy (LH) and vaginal hysterectomy (VH) result in significant objective and subjective improvement at the 1-year follow-up. LH was associated with better apical support; the mean difference for point C was significantly higher compared with women who underwent VH. The mean difference in total vaginal length was also significantly higher in women having LH.
At 1 year, there is more chance of requiring apical surgery in the VH group (14 %) compared with the LH group (6 %). However, significantly more repeat vaginal repairs are required post-hysteropexy (10 %). This may be explained by fewer concomitant vaginal repairs performed at the time of the initial operation. The rate of anterior repair was 50 % less in the LH group at the time of primary operation as adequate elevation of the anterior prolapse appeared to be achieved at the time of initial surgery, once apical support had been re-established.
Both operations appear to be safe, with LH having significantly less blood loss, fewer nights in hospital, shorter time before return to normal activity, and lower post-operative pain score compared with VH, but the operation took longer to perform.
Strengths and limitations
To our knowledge, this is the first study comparing laparoscopic uterine preservation surgery with conventional hysterectomy surgery for uterine prolapse. A recent survey in the United Kingdom confirmed that vaginal hysterectomy with uterosacral ligament suspension is the most common procedure performed for uterine prolapse with mild to moderate apical vaginal prolapse [10]. Although other procedures for concomitant vaginal vault support are described in the literature, over 50 % of gynecologists routinely employ this method in the UK. However, when there is procidentia it is thought that this method is insufficient [11]. In this study, 3 women with procidentia underwent additional sacrospinous suture vault fixation, as recommended by the RCOG [11].
Our study randomized women to try and eliminate bias. However, we struggled to recruit, many women preferring uterine preservation when offered this option. This patient preference also led to a high drop-out rate post-recruitment, prior to surgery. The surgeons performing the procedures had extensive experience performing both operations and each had carried out many hundreds of VHs and over 50 LHs prior to starting the trial; thus, there was no learning curve. The data from this study can be used to counsel women undergoing prolapse surgery and is a platform for designing a more robust multi-center study. According to our data for a binary outcome superiority trial, with an 80 % chance of detecting significance at the 5 % level, 434 patients are required to show a significant difference in rates of recurrent apical prolapse surgery 1 year post-operatively.
Our study had some limitations. This was a pilot study and not adequately powered for the rate of recurrent apical prolapse; longer-term follow up will be required. The study was randomized; consequently, patients could not choose their operation method. As a result, recruitment was much more difficult than anticipated as many preferred to retain choice and declined recruitment. Thirty-one women declined to continue with the study once recruited, as they did not wish to undergo the surgery allocated. There were 11 women in the VH group and 10 in LH who did not attend the 1-year follow-up. For these women, case notes were examined to confirm whether recurrent prolapse surgery had been performed. However, this method is only valid on the assumption that repeat surgery had been performed in the same hospital. If they had undergone surgery elsewhere, this would not have been detected, although there are no other hospitals within Oxfordshire, and the population is relatively stable.
No urinary symptom validated questionnaires were completed pre- and post-procedure and the change in urinary symptoms was obtained by direct questioning at the time of review.
Interpretation
Hysteropexy appears to show comparable repeat apical re-operation compared with vaginal hysterectomy at the 1-year follow-up. Objective assessment showed significant improvement in point C, which was elevated by a mean of 6.8 cm. This was very similar to our previous observational study of a larger cohort [9]. We suspect that the polypropylene mesh used will provide more durable long-term apical support in the LH group. Consequently, we anticipate higher rates of apical recurrent prolapse in the VH group with longer follow up, there appeared to be a trend supporting this, but the hypothesis can only be tested with a larger and longer follow-up study.
Contrary to the belief that prolapse repair can worsen urinary incontinence and unmask urethral sphincter weakness [18], it seems that a considerable number of women had improvement of their urinary incontinence without any continence procedure. This concurs with previous studies showing up to 40 % recovery from urinary incontinence after prolapse surgery [19]. However, urinary symptoms need to be further investigated with larger and longer studies. This finding, however, along with the similar findings of prior studies, has led the authors to change their clinical practice: we now correct anatomical defects in the first instance when patients present with combined prolapse and bladder symptoms. We evaluate urinary symptoms if they persist post-prolapse surgery, rather than performing concurrent prolapse and continence surgery.
Of the data analyzed, lower numbers of women recommended LH rather than VH (89 % vs 78 %). Those who were less satisfied with hysteropexy tended to cite further anterior prolapse as the reason for dissatisfaction.
While concurrent vaginal surgery at the time of vaginal hysterectomy tends to be routine among many urogynecology centers, whether or not it is performed at the time of laparoscopic prolapse correction is contentious. Restoring apical support will frequently, in the authors’ experience, also correct cystocele and enterocele. We find that morbidity and risk of vaginal dysfunction are reduced if vaginal surgery is minimized; however, repeat surgery is a source of dissatisfaction. Currently, in our unit, we try to avoid concurrent vaginal surgery if possible, as witnessed by the lower rates seen in the LH group, and this rate has reduced still further since this study was performed.
Subsequent malignancy
One of the women in the VH group was found to have a coincidental uterine cancer despite being asymptomatic. The risk of an asymptomatic woman being diagnosed with coincidental endometrial carcinoma at the time of vaginal hysterectomy is thought to be less than 1 % [20, 21]. Women undergoing a uterine preservation procedure need to be warned of potential uterine and cervical cancer and need to continue with cervical screening. They are also advised to seek medical advice for any abnormal vaginal bleeding, as with any other non-hysterectomized woman. Women undergoing hysterectomy post-hysteropexy require division of prolene mesh at the level of the right uterosacral ligament. The authors have performed hysterectomy subsequent to hysteropexy for bleeding in other non-trial patients and have not encountered any technical difficulty with mesh division or hysterectomy.
Conclusion
In conclusion, laparoscopic hysteropexy is a safe and effective surgical alternative to vaginal hysterectomy. At 1 year, both operations have similar recurrent apical prolapse. However, longer follow-up data from larger multicenter studies are required.
References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501–506. doi:10.1016/S0029-7844(97)00058-6
Handa VL, Garrett E, Hendrix S, Gold E, Robbins J (2004) Progression and remission of pelvic organ prolapse: a longitudinal study of menopausal women. Am J Obstet Gynecol 190(1):27–32. doi:10.1016/j.ajog.2003.07.017
Dallenbach P, Kaelin-Gambirasio I, Dubuisson JB, Boulvain M (2007) Risk factors for pelvic organ prolapse repair after hysterectomy. Obstet Gynecol 110(3):625–632. doi:10.1097/01.AOG.0000278567.37925.4e
Abdel-Fattah M, Familusi A, Fielding S, Ford J, Bhattacharya S (2011) Primary and repeat surgical treatment for female pelvic organ prolapse and incontinence in parous women in the UK: a register linkage study. BMJ Open 1(2), e000206. doi:10.1136/bmjopen-2011-000206
Dallenbach P, Kaelin-Gambirasio I, Jacob S, Dubuisson JB, Boulvain M (2008) Incidence rate and risk factors for vaginal vault prolapse repair after hysterectomy. Int Urogynecol J Pelvic Floor Dysfunct 19(12):1623–1629. doi:10.1007/s00192-008-0718-4
Zucchi A, Lazzeri M, Porena M, Mearini L, Costantini E (2010) Uterus preservation in pelvic organ prolapse surgery. Nat Rev Urol 7(11):626–633. doi:10.1038/nrurol.2010.164
Rahmanou P, Price N, Jackson S (2014) Laparoscopic hysteropexy: a novel technique for uterine preservation surgery. Int Urogynecol J 25(1):139–140. doi:10.1007/s00192-013-2129-4
Price N, Slack A, Jackson SR (2010) Laparoscopic hysteropexy: the initial results of a uterine suspension procedure for uterovaginal prolapse. BJOG: Int J Obstet Gynaecol 117(1):62–68. doi:10.1111/j.1471-0528.2009.02396.x
Rahmanou P, White B, Price N, Jackson S (2014) Laparoscopic hysteropexy: 1- to 4-year follow-up of women postoperatively. Int Urogynecol J 25(1):131–138. doi:10.1007/s00192-013-2209-5
Jha S, Moran P (2011) The UK national prolapse survey: 5 years on. Int Urogynecol J 22(5):517–528. doi:10.1007/s00192-011-1379-2
RCOG (2007) Green-top guideline no. 46: the management of post hysterectomy vaginal vault prolapse. http://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg46/
Price N, Jackson SR, Avery K, Brookes ST, Abrams P (2006) Development and psychometric evaluation of the ICIQ vaginal symptoms questionnaire: the ICIQ-VS. BJOG 113(6):700–712. doi:10.1111/j.1471-0528.2006.00938.x
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175(1):10–17
Srikrishna S, Robinson D, Cardozo L (2010) Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J 21(5):523–528. doi:10.1007/s00192-009-1069-5
Toozs-Hobson P, Freeman R, Barber M, Maher C, Haylen B, Athanasiou S, Swift S, Whitmore K, Ghoniem G, de Ridder D (2012) An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse. Int Urogynecol J 23(5):527–535. doi:10.1007/s00192-012-1726-y
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21(1):5–26. doi:10.1007/s00192-009-0976-9
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, Dwyer PL, Fatton B, Kocjancic E, Lee J, Maher C, Petri E, Rizk DE, Sand PK, Schaer GN, Webb RJ (2011) An international urogynecological association (IUGA) / international continence society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) & grafts in female pelvic floor surgery. Int Urogynecol J 22(1):3–15. doi:10.1007/s00192-010-1324-9
Grody MH (1998) Urinary incontinence and concomitant prolapse. Clin Obstet Gynecol 41(3):777–785
Lensen EJ, Withagen MI, Kluivers KB, Milani AL, Vierhout ME (2013) Urinary incontinence after surgery for pelvic organ prolapse. Neurourol Urodyn 32(5):455–459. doi:10.1002/nau.22327
Renganathan A, Edwards R, Duckett JR (2010) Uterus conserving prolapse surgery–what is the chance of missing a malignancy? Int Urogynecol J 21(7):819–821. doi:10.1007/s00192-010-1101-9
Wan OY, Cheung RY, Chan SS, Chung TK (2013) Risk of malignancy in women who underwent hysterectomy for uterine prolapse. Aust N Z J Obstet Gynaecol 53(2):190–196. doi:10.1111/ajo.12033
Acknowledgements
We are grateful to all clerical and nursing staff, especially Bev White and Tiana Howard, for assisting with patient assessment and data collection.
Conflicts of interest
None.
Details of ethics approval
The trial protocol was approved by the National Research Ethics committee (reference number: 09/H0606/28).
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rahmanou, P., Price, N. & Jackson, S.R. Laparoscopic hysteropexy versus vaginal hysterectomy for the treatment of uterovaginal prolapse: a prospective randomized pilot study. Int Urogynecol J 26, 1687–1694 (2015). https://doi.org/10.1007/s00192-015-2761-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2761-2