Abstract
Introduction and hypothesis
Uterosacral ligament suspension (USLS) is a common procedure for apical pelvic organ prolapse. The procedure has been described using only permanent suture, only absorbable suture and a combination of permanent and absorbable suture. We hypothesized that the use of absorbable suture is not inferior to the use of permanent suture.
Methods
All women undergoing USLS between October 2016 and November 2017 were approached. Subjects were randomized to permanent or absorbable suture. The primary outcome was POP-Q point C 12 months after surgery (non-inferiority limit = 2 cm). A composite outcome of success at 12 months was defined as no apical prolapse ≥ 1/2 TVL, no prolapse beyond the hymen, no prolapse retreatment and no bulge symptoms.
Results
Forty-four subjects with mean (SD) age 62.9 (12.0) years and body mass index 29.1 (5.4) kg/m2 were enrolled and underwent USLS. Fifteen (34.1%) had POP-Q stage II and 29 (65.9%) stage III prolapse. Twenty-two were randomized to permanent and 22 to absorbable suture. Forty (90.9%) completed the 12-month follow-up. Median (IQR) POP-Q point C at 12 months was −7 (−10, -6) for the permanent and − 7 (−9, -5.5) for the absorbable suture groups (p = 0.65, non-inferiority p < 0.0002). Four (20%) in the permanent and one (5%) in the absorbable suture group reported bulge symptoms (p = 0.34). Fifteen (75%) in the permanent and 18 (90%) in the absorbable suture groups met criteria for composite success (p = 0.41). Intervention-related adverse outcomes were uncommon and not different between groups.
Conclusion
Absorbable suture for USLS is not inferior to permanent suture for apical anatomic outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The lifetime risk of surgery for pelvic organ prolapse (POP) or stress urinary incontinence (SUI) has been estimated to be as high as 20% [1]. Uterosacral ligament suspension (USLS) is a commonly performed vaginal approach surgical procedure for correction of apical vaginal prolapse. Anatomic cure rates for apical prolapse following USLS have recently been shown to be 89.7% [2]. The original description of the USLS procedure by Shull included the use of permanent sutures for the apical suspension [3]. Subsequent, high-quality trials evaluating USLS, such as the OPTIMAL trial, have also included the use of permanent sutures [2]. Thus, permanent apical sutures can be considered the “gold standard.” Nonetheless, debate persists as to the optimal suture selection for this procedure.
Some have advocated choosing an absorbable suture [4]. This allows a full-thickness incorporation of the vaginal wall with the apical suture and may reduce suture-related complications. The procedure was initially described using permanent suture to suspend the fibromuscular apical vaginal tissue to the uterosacral ligaments. Symptomatic suture erosion rates of 22% in the permanent suture group were noted in one retrospective comparison of permanent and absorbable sutures [4]. No suture erosions were noted in the absorbable suture group. However, others have advocated continued use of permanent suture, citing increased failure rates with absorbable sutures [5]. The evidence for either approach is limited by having just a few retrospective studies [4, 5].
This primary aim of this trial was to compare absorbable suture to permanent suture for USLS as measured by Pelvic Organ Prolapse Quantification (POP-Q) point C at 12-month follow-up [6]. We hypothesized that absorbable suture is not inferior to permanent suture. Secondary aims included comparing subjective prolapse outcomes and suture-related complications between groups.
Materials and methods
The design of the trial was made available on ClinicalTrials.gov (NCT02888093) prior to recruitment. The study was conducted at the University of Iowa Hospitals and Clinics (Iowa City, IA, USA). The study protocol was approved by the University of Iowa institutional review board, and all subjects provided written informed consent. Reporting is consistent with the CONSORT guidelines.
Adult women scheduled for USLS were eligible for study inclusion and were approached prior to surgery. Exclusion criteria included inability to provide informed consent in English, prisoners, cognitive impairment precluding informed consent and planned hysteropexy. Post-hysterectomy USLS and USLS with concomitant hysterectomy were included. Demographics, relevant histories and baseline physical examination including POP-Q and Pelvic Floor Distress Inventory-20 (PFDI-20) data were abstracted from the electronic medical record following enrollment [7].
Randomization occurred once the subject was in the operating room and the surgical plan was confirmed. Subjects were assigned to receive either absorbable 0 polydioxanone (PDS, Ethicon, Somerville, NJ, USA) suture or permanent polytetrafluoroethylene (CV-2 Gore-Tex, WL Gore and Associates, Flagstaff, AZ, USA) suture for the USLS. Randomization was carried out using a web-based service (www.randomize.net, Ottawa, ON, Canada) that allows for allocation concealment until the time of randomization in the operating room. The randomization sequence was 1:1 with random permuted blocks of four and was stratified by surgeon. Subjects, outcomes assessors and statisticians were blinded to the randomization groups. Surgeons, by necessity, were not blinded.
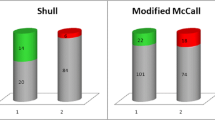
USLS was performed as described by Shull et al with two important differences in technique [3]. First, two sutures were placed through the intermediate portion of each uterosacral ligament instead of three. Second, when absorbable suture was used, the suture was placed through the full thickness of the anterior and posterior vaginal walls. Hysterectomy was performed concomitantly on women who had not had a prior hysterectomy. Anterior colporrhaphy, posterior colporrhaphy and perineorrhaphy were performed at the discretion of the surgeon. Mid-urethral sling procedures were performed as indicated for treatment of stress urinary incontinence or for prevention of de novo stress urinary incontinence.
Postoperative follow-up and data collection occurred 6 weeks and 12 months after surgery. Follow-up appointments were conducted by one of two nurse practitioners with experience in the care of female pelvic floor disorders and who were blinded to the type of suture used. Both nurse practitioners also had extensive experience in performing POP-Q examinations and underwent additional training prior to beginning study procedures to ensure that POP-Q measurements were obtained accurately and systematically. Both follow-up appointments included a complete pelvic examination with POP-Q measurements, a Patient Global Impression of Improvement (PGI-I) for prolapse and several standardized questions about symptoms that could potentially be related to the type of suture used for the USLS [8]. All subjects were also assessed for any suture-related complications, such as erosion or granulation tissue. The 12-month follow-up appointment also included a PFDI-20.
The primary outcome was measured by POP-Q point C. Specifically, the preferred method for measuring point C was to identify point C visually with a speculum and to visually follow that point with the woman performing a Valsalva maneuver while simultaneously releasing pressure on the speculum. Should this method prove not to be feasible for any individual woman because of anatomy or other reasons, the examiner had the option to identify point C visually with the speculum in place, leave the Q-tip in place lying against point C, remove the speculum and have the woman perform a Valsalva maneuver while allowing the Q-tip to descend against point C. As a last alternative, the provider may identify point C digitally, follow point C digitally while the woman performs a Valsalva maneuver and then measure the distance from the hymen to the tip of the finger with a Q-tip.
Secondary outcomes included a composite prolapse outcome, comparison of PGI-I and comparison of suture-related complications. The composite outcome included anatomic, subjective and retreatment components. A composite outcome of failure at 12 months was defined as apical prolapse ≥ 1/2 TVL, prolapse (any POP-Q point) beyond the hymen, any prolapse retreatment and the presence of bulge symptoms. Bulge symptoms were defined as a positive response to PFDI-20 question 3 with “somewhat,” “moderately” or “quite a bit” of bother.
The trial was designed as a non-inferiority trial. Non-inferiority trials aim to show that an experimental treatment (absorbable suture in this case) is not worse than an active control (permanent suture) by more than a specified equivalence margin [9]. Eighteen women per group were required to demonstrate that absorbable suture is not inferior to permanent suture at an alpha 0.05, beta 0.90, SD 2.0 and non-inferiority limit (d) of 2.0 [10]. In other words, if there is truly no difference between absorbable and permanent suture, then 36 women are required to be 90% sure that the lower limit of a one-sided 95% confidence interval (or equivalently a 90% two-sided confidence interval) will be above the non-inferiority limit of −2 cm for POP-Q point C. The standard deviation cited here for measuring point C was obtained from the Kasturi et al. retrospective analysis of absorbable vs permanent suture for USLS [4]. The non-inferiority limit of −2 cm for POP-Q point C was chosen as this represents both a clinically meaningful difference and is large enough that the margin of error in measuring the POP-Q is unlikely to influence the results. Total study recruitment was continued until 44 women were enrolled, randomized and completed USLS. This recruitment number was chosen to allow for an attrition rate of about 20%.
Variable distributions are expressed as proportions for categorical variables and medians (interquartile ranges) or means (standard deviations) for continuous variables, depending on the distribution. Differences between the two treatment arms were assessed using Fisher’s exact test for categorical variables and the Wilcoxon rank sum test for continuous variables.
Results
Between October 2016 and November 2017, 44 subjects with mean (SD) age 62.9 (12.0) years and body mass index 29.1 (5.4) kg/m2 were enrolled (Table 1). There were no significant differences between groups in any baseline variable. Twenty-two were randomized to permanent and 22 to absorbable suture (Fig. 1). Fifteen (34.1%) had POP-Q stage II and 29 (65.9%) stage III prolapse (Table 2). Baseline characteristics were similar in the permanent and absorbable groups, including prior prolapse surgery (9.1 vs 4.6%, p = 1.00) and baseline POP-Q point C measurement (0 vs −1.5 cm, p = 0.27). All subjects underwent USLS. Most underwent concomitant hysterectomy (90.9%) and at least one additional prolapse or urinary incontinence procedure (86.4%) (Table 3). Forty (90.9%) subjects completed 12-month follow-up. Three subjects declined to return for follow-up after being contacted, and one subject could not be contacted. The number of subjects lost to follow-up was the same in each group.
Median (IQR) POP-Q point C at 12 months was −7 (−10, -6) for permanent and − 7 (−9, -5.5) for the absorbable suture groups (p = 0.65, non-inferiority p < 0.0002) (Table 4). Four (20%) in the permanent and one (5%) in the absorbable suture groups reported bulge symptoms (p = 0.34). Five (25%) in the permanent and two (10%) in the absorbable suture groups met criteria for composite failure (p = 0.41). No differences were seen in any outcome measure. No subjects underwent re-treatment of prolapse.
Seven women (2 in the permanent group, 5 in the absorbable group) provided PGI-I scores other than 1 (very much better) or 2 (much better). Only one of those seven women also gave a positive response to PFDI #3. For the six women who did not have recurrent bulge symptoms but had poor PGI-I scores, one had significant de novo SUI, one had persistent SUI requiring urethral bulking injection, one had persistent urgency incontinence, one had worsened urgency incontinence and recurrent UTIs, and two had no apparent complaints in the medical records.
Intervention-related adverse outcomes were relatively common at 6-week follow-up. One subject with permanent suture had granulation tissue treated with silver nitrate at 6 weeks. One subject with absorbable suture had a suture exposure treated with topical estrogen at 6 weeks. By 12 months after surgery, all intervention-related adverse outcomes were uncommon (all 0–10%) and not different between groups (Table 5). No subjects required treatment of any suture-related complications at 12 months. No subjects required suture excision in the office or in the operating room at any time point during the study.
Discussion
In women with apical prolapse undergoing vaginal approach USLS, this trial demonstrates that use of absorbable suture is non-inferior to permanent suture for prolapse outcomes at 12-month follow-up. Additionally, there were no differences in adverse outcomes related to the suture type.
Our findings are consistent with prior retrospective reports comparing absorbable and permanent suture [4, 11]. These authors both found that absorbable suture resulted in similar outcomes to permanent suture. In contrast, our results differ from those of Chung et al. who concluded that permanent suture resulted in fewer prolapse recurrences [5]. However, all of these prior studies are limited by their retrospective design and outcome definitions based only on anatomic findings or retreatment.
The presence of composite failure at 12 months in our study is similar to previously reported randomized trials evaluating USLS. The recently reported Study of Uterine Prolapse Procedures Randomized Trial compared uterosacral ligament suspension using a combination of absorbable and permanent suture to vaginal approach mesh hysteropexy [12]. They used a composite definition of surgical failure very similar to that used in our study and reported a 25.9% composite failure at 12-month follow-up in the USLS group. Another randomized trial comparing native tissue sacrospinous hysteropexy to vaginal hysterectomy with USLS demonstrated a composite failure rate of 17–22% at 12 months for USLS [13].
The primary strength of our randomized trial is the rigorous methodology used. To our knowledge, this is also the first randomized trial to evaluate absorbable and permanent suture for USLS. However, we do have some limitations. The study population was largely women with stage II and III prolapse and fewer than 10% had prior hysterectomy or prolapse surgery. We only evaluated two specific types of suture. Thus, our conclusions should not be extrapolated to apply to other sutures. Follow-up was limited to 12 months. Although the prolapse recurrence rate would be expected to increase with longer follow-up, we suspect that this would be unlikely to result from suture choice. The absorbable suture used in this study is expected to be completely absorbed in about 180 days. Therefore, any change in apical support (i.e., POP-Q point C) due to suture absorption would be expected to occur within 12 months. Finally, the study was designed as a non-inferiority study and has a smaller study population. Larger studies are warranted to confirm our findings.
In conclusion, this study demonstrates that absorbable suture is non-inferior to permanent suture for prolapse outcomes at 12-month follow-up. Additionally, there were no differences in intervention-related adverse outcomes.
References
Wu JM, et al. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6.
Barber MD, et al. Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vaginal prolapse: the OPTIMAL randomized trial. JAMA. 2014;311(10):1023–34.
Shull BL, et al. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol. 2000;183(6):1365–73. discussion 1373-4.
Kasturi S, et al. High uterosacral ligament vaginal vault suspension: comparison of absorbable vs. permanent suture for apical fixation. Int Urogynecol J. 2012;23(7):941–5.
Chung CP, et al. Permanent suture used in uterosacral ligament suspension offers better anatomical support than delayed absorbable suture. Int Urogynecol J. 2012;23(2):223–7.
Bump RC, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13.
Srikrishna S, Robinson D, Cardozo L. Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21(5):523–8.
Snapinn SM. Noninferiority trials. Curr Control Trials Cardiovasc Med. 2000;1(1):19–21.
Available from: Sealed Envelope Ltd. 2012. Power calculator for continuous outcome non-inferiority trial. [Online] Available from: https://www.sealedenvelope.com/power/continuous-noninferior/ [Accessed May 31 2016].
Bradley MS, et al. Vaginal uterosacral ligament suspension: a retrospective cohort of absorbable and permanent suture groups. Female Pelvic Med Reconstr Surg. 2018;24(3):207–12.
Nager CW, et al. Effect of vaginal mesh Hysteropexy vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with Uterovaginal prolapse: a randomized clinical trial. JAMA. 2019;322(11):1054–65.
Detollenaere RJ, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ. 2015;351:h3717.
Funding
IUGA 2016 Clinical Research Grant.
The University of Iowa Clinical and Translational Science Award-NIH (UL1TR002537).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kowalski, J.T., Genadry, R., Ten Eyck, P. et al. A randomized controlled trial of permanent vs absorbable suture for uterosacral ligament suspension. Int Urogynecol J 32, 785–790 (2021). https://doi.org/10.1007/s00192-020-04244-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04244-1