Abstract
Introduction and hypothesis
The objective of this study was to compare the outcomes of uterosacral ligament suspension (USLS) procedures in relation to suture material used for apical suspension.
Methods
A retrospective chart review was performed for two senior surgeons who supervised and performed USLS with both suture types in 2008–2009. Permanent and delayed absorbable sutures were compared for failure of anatomical support. Failure, defined as recurrent prolapse beyond the hymen, was evaluated using survival analysis.
Results
Two hundred forty-eight procedures were performed. One percent in the permanent group had a loss of support beyond the hymen compared to 6% in the delayed absorbable group (p = 0.034). The preoperative prolapse stage and duration of follow-up did not differ between the two groups. The number of sutures used did not differ between patients who failed and those who did not fail.
Conclusions
The use of permanent sutures for USLS of the vaginal apex was associated with a lower failure rate than delayed absorbable sutures in the short-term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) affects millions of women. Approximately 200,000 POP surgeries are performed annually [1, 2]. The vaginal approach to correct POP with the use of native tissue is minimally invasive. Patients are often discharged home the day after surgery. In our institution, uterosacral ligament suspension (USLS) is the most common type of vaginal surgery to correct apical POP. Shull et al. described a transvaginal approach to repair apical and other associated sites of POP with uterosacral ligaments and 5% of his patients had grade 2 or greater persistent or recurrent support defects in follow-up lasting up to 4 years [3]. The suture material used in these patients was permanent braided suture [3]. Technically, the suture closest to the surgeon, next to the ischial spine, is delayed absorbable polydioxanone suture (0-Maxon, Covidien, Dublin, Ireland), followed by two permanent polyester sutures (2-0 Ti-Cron, Covidien, Dublin, Ireland) in the uterosacral ligaments on one or both sides of the pelvis. From 2008 to 2009, two to four delayed absorbable sutures on each side and no permanent sutures were used for uterosacral ligaments suspension in a group of consecutive patients. The switch to delayed absorbable sutures occurred because one senior surgeon (BLS) broke a needle on a 2-0 polyester suture and could not find the missing part intraoperatively. That patient has had no postoperative sequelae. The needle on the 0-polydioxanone suture is larger and easier to use in the suspension. Also, other surgeons had informally reported using only delayed absorbable sutures and their patients had good surgical outcomes regarding anatomic support.
Our subsequent clinical experience has suggested that the failure rate (recurrent POP beyond the hymen) is higher in those patients who had USLS with only delayed absorbable sutures compared to those who had permanent sutures. The objective of this study was to compare outcomes for pelvic support following surgery utilizing the two types of suture materials used in apical support during the USLS procedure.
Methods
A retrospective chart review of two cohorts of patients who underwent USLS from January 2008 through December 2009 was performed. Approval was obtained from the Scott and White Institutional Review Board prior to initiation of the chart review. Medical records of patients who underwent USLS by two senior surgeons (BLS and PMY) during the study interval were reviewed.
A database without patient identifiers was developed. Patients were divided into two groups: permanent sutures and delayed absorbable sutures used for apical suspension. Permanent (polyester) and delayed absorbable (polydioxanone) sutures were compared for failure of support during follow-up exams. USLS cases were performed according to the technique published by Shull et al. [3]. Permanent braided sutures were used to plicate the pubocervical fascia.
In all patients, the remnants of uterosacral ligaments were identified posterior and medial to the ischial spines at the 4 o’clock and 8 o’clock positions [3]. In the permanent group, the first suture used is delayed absorbable polydioxanone suture, followed by two permanent polyester sutures in the uterosacral ligaments on one or both sides of the pelvis. In the delayed absorbable group, two to four delayed absorbable sutures and no permanent sutures were used in uterosacral ligaments on one or both sides of the pelvis.
The data elements collected included age at the time of surgery, parity, body weight, height, BMI, types of suture used, numbers of suture used, preoperative and postoperative pelvic exam findings, history of prior prolapse surgery, and numbers of postoperative follow-up visits and duration in days since surgery. Failure was defined as recurrent prolapse beyond the hymen. Factors that were analyzed were failure rate, age, BMI, number of sutures, preoperative prolapse stage, history of prior prolapse surgery, and duration of follow-up. Group comparisons were performed to identify factors that are associated with failure rate and whether other patient factors predicted failure using Student’s t tests for univariate comparisons and multiple regression analysis. The distributions of number of sutures and preoperative prolapse staging were compared using Pearson’s chi-square test. Survival analysis with Gehen’s Wilcoxin test was used to compare the difference between the different suture materials using a p level <0.05 as significant.
Results
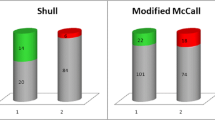
During the study interval, 287 USLS procedures were performed. Nineteen patients had no documentation of types of suture used. Twenty patients did not see us for follow-up after surgery. These 39 cases were excluded from the analysis. In all, 248 cases were analyzed. Of these cases, patients averaged (mean ± SD) 62 ± 12 years of age with BMI of 27.8 ± 5.1 kg/m2 at the time of surgery (Table 1). One of 105 (1%) patients in the permanent suture group had a loss of support beyond the hymen, while 8 of 141 (6%) patients in the delayed absorbable suture group had recurrent prolapse beyond the hymen. Using survival analysis, the groups differed (p = 0.034) in anatomic outcome during a relatively short average follow-up interval of 160 days (Fig. 1). Duration of follow-up (average of 157 versus 162 days, respectively; p = 0.86, using Student’s t test) was similar between groups as was BMI (p = 0.15). The patients who failed were older (70 versus 61 years, p = 0.041). However, the permanent suture group patients were also older (65 versus 60 years, p = 0.003) than those with delayed absorbable sutures; so age was not a confounding factor in this analysis.
Analysis of outcome by surgeon was performed. The first surgeon (BLS) had 73 patients in the permanent group and 63 patients in the delayed absorbable group (with 1 failure in the permanent group and 6 in the delayed absorbable group). The second surgeon (PMY) had 33 patients in the permanent group and 79 patients in the delayed absorbable group (with 0 failure in the permanent group and 2 in the delayed absorbable group). Surgeons do not differ in failure rates within suture types (p = 0.5 in the permanent group and p = 0.07 in the delayed absorbable group, using chi-square test).
Number of sutures used did not differ between patients who failed and those who did not fail (p > 0.24). Eleven patients had unilateral suspension, and 237 patients had bilateral suspension. The majority of patients who failed had six sutures placed (one in the permanent group and six in the delayed absorbable group, p = 0.0037). The preoperative prolapse stage did not differ between the two groups (p = 0.10 using chi-square test; Table 2). Within the delayed absorbable group, preoperative stage did not differ between patients who failed and those who did not fail (p = 0.89 using chi-square test; Table 3). In the nine patients who failed (one from the permanent group and eight from the delayed absorbable group), all had recurrent anterior and apical prolapse. None of these patients had a prior history of pelvic reconstructive surgery.
The one patient who failed in the permanent group used a pessary to treat her recurrent POP. Three of the eight patients who failed in the delayed absorbable group underwent repeat surgery for POP 9 to 10 months after the index surgery. The other five patients in this group chose to be observant or use a pessary. During the postoperative visit, nine patients in the permanent group and seven patients in the delayed absorbable group had permanent suture exposure that required removal in office. The majority of these patients had suture exposure from the permanent sutures used in anterior compartment plication. No patients returned to the operating room for removal of permanent sutures.
Discussion
There are many ways to correct apical POP. In our institution, USLS is the procedure used most commonly to correct apical POP. Shull et al. described a transvaginal approach to repair apical and other associated sites of POP with uterosacral ligaments [3]. The suture material used as described in his paper was permanent braided suture [3]. There are many variances in surgical technique. Wheeler et al. showed that USLS can be performed with bilateral single sutures [4]. In our institution, three sutures (first with delayed absorbable polydioxanone suture, followed by two permanent polyester sutures) are usually placed in each uterosacral ligament. If pelvic adhesions are encountered or there is difficulty in placing sutures on one side of the pelvis, then two to four sutures are usually placed on the contralateral side. In 2008 and 2009, a group of patients received only delayed absorbable polydioxanone sutures during USLS. Our clinical experience suggested that the anatomical failure rate was higher in these patients. Hence, this retrospective study was carried out to determine if there was a difference in the surgical outcomes.
The reported failure rate of USLS varies. Most authors define failure as stage 2 prolapse or greater in one or more segments, with failure rates ranging from 5% to 19% [3, 5–8]. Our failure rate, when defined as recurrent prolapse beyond the hymen, is 1% in the permanent suture group and 6% in the delayed absorbable suture group. The average follow-up interval of 160 days is less than the multiple year interval typically reported in other studies. One reason for our lower failure rate could be the number of suspensory sutures placed in the uterosacral ligaments. We usually place three sutures on each side because we believe suture redundancy provides durability and may reduce surgical failure. Another reason for our low failure rate could be the relatively short follow-up of 160 days in our study compared to the 4-year follow-up period used in the original report from our group [3]. The durability of all reconstructive surgery is a function of time. The longer the follow-up, the greater the recurrence rate. The purpose of our study was to compare the failure rates with two different suture materials. Using survival analysis, permanent suture seems to be associated with a more durable surgical outcome compared to delayed absorbable sutures (p = 0.034).
We also examined other variables which could confound our retrospective results. The duration of follow-up was similar between groups so this did not account for the difference. The patients’ BMI values were similar. The number of sutures used in the delayed absorbable suture group did not differ in patients who failed versus those who did not fail. Interestingly, patients who failed were older. However, the permanent suture group patients who had a lower anatomical failure rate were also older than those with delayed absorbable sutures. Therefore, it seems unlikely that age itself was the major contributor to the observed difference in failure rates. Preoperative prolapse stage and history of prior pelvic reconstructive surgery have been shown to be risks factors for developing recurrent POP [9, 10]. In our study, the preoperative stage did not differ between the two groups. Within the delayed absorbable group, the preoperative stage did not differ between those who failed and those who did not fail. Moreover, none of the nine patients who failed had a history of prior pelvic reconstructive surgery. These results suggest that two of the potential risk factors for recurrent POP, advance preoperative stage and history of prior pelvic reconstructive surgery, were not confounders in this study. We also examined the number of sutures placed in the uterosacral ligaments. Six of eight patients who failed in the delayed absorbable group and one patient who failed in the permanent group had six uterosacral ligament sutures placed. This implies that suture material, and not suture numbers, contributed to the failure. No patient had recurrent POP (defined as POP beyond the hymen) on their 6-week follow-up visit. Failure was not documented until after 180 days. Therefore, we infer that the index surgery was executed correctly. Absorption of these delayed absorbable suspensory sutures after 3 to 6 months could contribute to failure of the repair. Our data imply that the use of delayed absorbable sutures contributed to the onset of support defect >180 days following surgery.
Three of the nine patients who failed have subsequently had repeat surgery for recurrent POP. In addition, nine patients in the permanent group and eight patients in the delayed absorbable group had asymptomatic suture exposure that was treated by removal in office. No patients returned to the operating room for removal of exposed permanent sutures. The two primary weaknesses of this study are the bias that may arise from retrospective studies and the fact that the two senior surgeons who evaluated the postoperative outcomes were not blinded. However, their evaluations were performed prior to performing this retrospective study.
A PubMed search revealed no retrospective or prospective trials that examined the effect of suture materials on the outcome of USLS procedures. An abstract was presented at the American Urogynecologic Society meeting in 2009 which showed that polyglactin 910 suture used for USLS had the lowest success rate when compared to polydioxanone, polytetrafluoroethylene, polypropylene, and polyester at 3 to 6 months follow-up [11]. However, information such as numbers of suture placed was not available from this abstract. In conclusion, based on our findings, permanent suture for the apical suspension component of USLS procedures offers better anatomical support than delayed absorbable suture.
References
Tegerstedt G, Maehle-Schmidt M, Nyrén O, Hammarström M (2005) Prevalence of symptomatic pelvic organ prolapse in a Swedish population. Int Urogynecol J Pelvic Floor Dysfunct 16:497–503
Rortveit G, Brown JS, Thom DH, Van Den Eeden SK, Creasman JM, Subak LL (2007) Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol 109:1396–1403
Shull BL, Bachofen C, Coates KW, Kuehl TJ (2000) A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol 183:1365–1373
Wheeler TL 2nd, Gerten KA, Richter HE, Duke AG, Varner RE (2007) Outcomes of vaginal vault prolapse repair with a high uterosacral suspension procedure utilizing bilateral single sutures. Int Urogynecol J Pelvic Floor Dysfunct 18:1207–1213
Lin LL, Phelps JY, Liu CY (2005) Laparoscopic vaginal vault suspension using uterosacral ligaments: a review of 133 cases. J Minim Invasive Gynecol 12:216–220
Silva WA, Pauls RN, Segal JL, Rooney CM, Kleeman SD, Karram MM (2006) Uterosacral ligament vault suspension: five-year outcomes. Obstet Gynecol 108:255–263
Rardin CR, Erekson EA, Sung VW, Ward RM, Myers DL (2009) Uterosacral colpopexy at the time of vaginal hysterectomy: comparison of laparoscopic and vaginal approaches. J Reprod Med 54:273–280
Margulies RU, Rogers MA, Morgan DM (2010) Outcomes of transvaginal uterosacral ligament suspension: systematic review and metaanalysis. Am J Obstet Gynecol 202:124–134
Whiteside JL, Weber AM, Meyn LA, Walters MD (2004) Risk factors for prolapse recurrence after vaginal repair. Am J Obstet Gynecol 191:1533–1538
Swift SE, Pound T, Dias JK (2001) Case-control study of etiologic factors in the development of severe pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 12:187–192
Patterson D, Sanses TV, Gamble TL, Abbasy S, Nguyen AL, Shahryarinejad A, Saks EK, Hoskey KA, Weber-Lebrun EE, Molden S, Lowenstein L, Young SB (2009) Abdominal sacrocolpopexy and uterosacral ligament suspension for pelvic organ prolapse: does a choice of suture material at the vaginal cuff affect anatomic outcomes? J Pelvic Med Surg 15:243
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chung, C.P., Miskimins, R., Kuehl, T.J. et al. Permanent suture used in uterosacral ligament suspension offers better anatomical support than delayed absorbable suture. Int Urogynecol J 23, 223–227 (2012). https://doi.org/10.1007/s00192-011-1556-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1556-3