Abstract
Purpose
Tibiofemoral synchronization technique matches the rotational alignment of the tibial component to the femoral component during the total knee arthroplasty (TKA). The rotational axis of the proximal tibia can be changed by this technique, which affects tibial torsion postoperatively. The purpose of this study was to investigate whether the tibiofemoral synchronization technique affect the tibial torsion, and the lower limb rotation after primary TKA. It was hypothesised that the tibial torsion would change after primary TKA.
Methods
Ninety-three posterior stabilised TKAs from 89 patients were included from January 2017 to December 2018. Mechanical hip–knee–ankle axis (mHKA), in plain radiographs, femoral anteversion, tibial torsion, femoral neck-malleolar angle (FNMA), and rotational alignment of the femoral and the tibial components in pre- and postoperative CT scans were measured by two blinded observers. The primary outcome was a postoperative change in femoral anteversion, tibial torsion and FNMA. Clinical outcomes were evaluated using the American Knee Society Knee Score (AKSKS)/Function Score (AKSFS), and Oxford Knee Score (OKS) preoperatively and at 1 year after TKA. Patients’ perception of changes in the foot progression angle after TKA was investigated. Statistical significance was set at p < 0.05.
Results
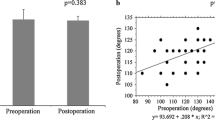
The mean rotational mismatch between the femoral and the tibial component was 0.6 ± 3.2°. There was a significant decrease in femoral anteversion (9.5 ± 6.7° vs. 5.2 ± 6.6°, p < 0.001), and a significant increase in the FNMA (17.6 ± 9.7° vs. 21.8 ± 10.5°, p = 0.005) after TKA, while no significant change in tibia torsion was observed (25.4 ± 8.8° vs. 24.9 ± 9.3°, p = 0.739). AKSS (37.8 ± 15.1 vs. 92.8 ± 8.8, p < 0.001), AKSFS (53.9 ± 18.1 vs. 89.9 ± 5.3, p < 0.001), and OKS (18.0 ± 7.3 vs. 39.9 ± 4.8, p < 0.001) were significantly improved at 1 year after TKA. Ten knees (11%) had changes in tibial torsion greater than ± 10° postoperatively. Four of five patients who had changes in FNMA greater than 15° perceived the external rotation of the foot progression angle after TKA. All four patients had an increase in tibial torsion larger than 10°.
Conclusion
Our study shows that the tibiofemoral synchronization technique less likely affects the tibial torsion after primary TKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Various surgical techniques are used to determine the rotational alignment of the tibial component during total knee arthroplasty (TKA) [1, 3, 7, 10, 11, 16, 24]. Possible anatomical landmarks for determining rotational alignment are tibial tuberosity, anterior tibia crest, tibial eminence, anterior or posterior tibial condylar line, patellar tendon, and second metatarsal bone. However, fixed landmarks may cause a rotational mismatch between the femur and tibia, potentially leading to suboptimal outcomes [25, 26]. This problem can be overcome using tibiofemoral synchronization techniques, such as self-alignment and the linker technique [4, 5, 11, 13, 17].
Tibiofemoral synchronization technique matches the rotational alignment of the tibial component to the femoral component. Moreover, tibiofemoral synchronization technique provides adequate tibiofemoral rotational alignment, which may prevent impingement of polyethylene bearing and improve patellar tracking. However, the tibiofemoral synchronization technique is independent of proximal tibial anatomy, and therefore, the tibial component can be placed in an external or internal position relative to the native rotational axis of the proximal tibia. As a result, the rotational axis of the proximal tibia after TKA may be changed according to the tibia component rotation. Postoperative changes in the rotational axis of the proximal tibia cause compensatory inverse tibial rotation in TKA with a fixed-bearing design [19], which affects the foot progression angle distally and the patellofemoral alignment proximally. Tibial component internal rotation relative to native anteroposterior axis of the proximal tibia causes the external torsion of the tibia, increasing the external rotation of the foot progression angle and Q-angle, and vice versa. A previous study investigated the effect of the rotational alignment of the femur and the tibia on lower limb rotational alignment using cadavers [19]. However, in vivo data are lacking.
The primary purpose of this study was to investigate whether the tibiofemoral synchronization technique affect the tibial torsion, and the lower limb rotation after primary TKA. It was hypothesised that the tibial torsion would change after primary TKA using a tibiofemoral synchronisation technique.
Methods
Patients
This prospective observational study was conducted after obtaining the approval of the institutional ethical review board (IRB No: 2016GR0311) and informed consent from patients. Patients who scheduled to undergo primary TKA (posterior cruciate ligament stabilised, cemented, fixed-bearing, ATTUNE, DePuy Synthes, USA) were screened from January 2017 to December 2018. The exclusion criteria were preoperative flexion contracture > 10° or flexion < 90°; mechanical hip–knee–ankle axis (mHKA) varus > 15° or valgus > 5°; extra-articular deformity of the involved limb, including hip or ankle joints affecting limb alignment or rotation; previous fractures or previous high tibial osteotomy on the operated knee, use of cemented intramedullary stems, and patellar resurfacing. A total of 168 knees from 132 patients were screened and 75 knees were excluded (Fig. 1). Finally, 93 knees from 89 patients were enrolled in this study (Table 1).
Surgical techniques
All TKAs with a medial parapatellar approach were performed by a senior surgeon. The measured resection technique for reproducing the implant thickness (distal 9 mm, symmetric posterior condyle 9 mm) was used in all patients. Distal femoral resection was performed using an intramedullary guide in 6° valgus relative to the anatomical axis of the femur. Femoral component rotation was aligned 3–5° external rotation relative to the posterior condylar axis according to preoperative measurement on CT. Proximal tibial cut was made perpendicular to the mechanical axis of the tibia with 3° posterior slope using an extramedullary guide. With the femoral trial in place, the tibial tray with a PS insert was placed. After the center of tibial tray was aligned to the center of femoral trial box in extension, the orientation was marked on the edge of proximal tibia. The keel was cut into the tibia according to this orientation. Full extension (< 5° flexion) was achieved in all patients intraoperatively.
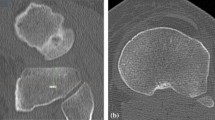
Computed tomography
Multidetector row computed tomography CT (64 channels) (Brilliance 64, Philips Medical System, Cleveland, USA) was used with detector collimation of 16 × 0.75 mm, tube energy and current of 100 kV and 70 mA s, respectively, beam pitch of 0.7 mm, and osteo-scanning mode. Slice thickness was 3 mm. During CT scans, each subject was in supine position with the patella forward, and hip, knee in extension. Axial CT scans of the proximal femur were obtained from the superior acetabulum to the lower border of the lesser trochanter. In the distal femur and proximal tibia, CT scans were taken from the supracondylar region to the tibial tuberosity. In the distal tibia, CT scans were obtained from the supramalleolar region to the upper talus. The following image sections were analysed (Fig. 2); the section showing (1) greater trochanter, femoral neck, and femoral head; (2) surgical transepicondylar axis (sTEA); (3) above the tip of the fibular head showing the entire anterior and posterior border of the proximal tibial condyle; and (4) immediately above the joint line showing the medial and lateral malleoli.
Radiologic evaluation
Preoperative (1 day before TKA) and postoperative (1 year after TKA) full-length lower leg weight-bearing anteroposterior radiographs were used to measure the mechanical hip–knee–ankle axis (mHKA). Preoperative (1 day before TKA) and postoperative (5–7 days after TKA) CT scans were obtained to measure axial parameters (Table 2) [9]. In cases in which the distal axis was externally rotated relative to the proximal axis, tibial torsion and femoral neck-malleolar angle (FNMA) values were expressed as positive and vice versa. The primary outcome of this study was a postoperative change in femoral anteversion, tibial torsion, and FNMA. To validate the accuracy of tibiofemoral synchronization technique, the rotational mismatch between femoral component and tibial component was measured (Table 2). The sTEA was used as a reference line for rotational alignment of femoral component and tibial component because it is considered the flexion–extension axis of the knee joint. The rotational angle of the femoral component was defined as the angle between the femoral component transverse axis (FCTA) and the sTEA. The rotational angle of the tibial component was defined as the angle between the tibial component transverse axis (TCTA) and the projected sTEA on the cut surface of the tibia. Preoperative rotation of the 90° angle line to the sTEA was measured relative to Akagi’s line [Fig. 3]). Positive values indicated that the axis was in external rotation relative to the reference line and vice versa. Measurements were recorded to the nearest 0.1° using a picture archiving and communication system (PACS) (STARPACS, INFINITT Healthcare, Seoul, South Korea), and the magnification factor was automatically corrected. The measurement accuracy of the PACS is within 0.1 mm and 0.1° [8]. The radiologic parameters were measured by two orthopaedic surgeons who did not participate in the operation.
Clinical outcomes
The clinical outcomes were evaluated using the American Knee Society Knee Score (AKSKS), American Knee Society Function Score (AKSFS), and Oxford Knee Score (OKS) preoperative and 1 year after TKA [6]. The patients’ subjective perception of changes in the foot progression angle after TKA was also analysed. The patients were asked to answer the question “Did you perceive changes in the foot progression angle during walking after TKA?” A negative answer indicated no clinically relevant changes in the foot progression angle after TKA, whereas a positive answer indicated clinically relevant changes in the foot progression angle after TKA and then asked about the direction “internally or externally compared to preoperative foot progression angle?” The clinical outcomes were collected by the orthopaedic surgeons who were not involved in the operation.
Statistical analysis
For descriptive analysis, values were presented as mean and standard deviation. The Kolmogorov–Smirnov statistic was used to test the normality assumption. A paired t test for continuous variables was used to compare the preoperative and postoperative values. The Pearson correlation coefficient was used to determine the relationship between the amount of change in femoral anteversion, tibial torsion, and FNMA after TKA. Radiographic parameters were measured twice at a 2-week interval. Intra- and inter-observer reliability was assessed using intraclass correlation coefficients. SPSS software version 20.0 was used for statistical analysis (IBM, USA). Differences were considered statistically significant at P values of less than 0.05.
Results
There was a significant decrease in femoral anteversion, and a significant increase in the FNMA after TKA (p < 0.001, p = 0.005), while no significant change in tibia torsion was observed (p = 0.739, Table 3). Changes in femoral anteversion, tibial torsion, and FNMA were within ± 10° in 83%, 89%, and 71% of knees, respectively, after TKA. Postoperative FNMA was externally rotated (24% of cases) or internally rotated (5% of cases) more than ± 10° compared to before TKA. Changes in FNMA were weakly correlated with changes in femoral anteversion (r = − 0.481, p < 0.001), and there was no significant correlation between changes in tibial torsion and FNMA (r = 0.029, p = 0.777). The mean rotational mismatch between the FCTA and TCTA was 0.6 ± 3.2°. In preoperative CT scans, all knees had an external or neutral rotation from the sTEA to Akagi’s line (mean 9.2 ± 3.9°, range 0.1–19.1°). Intra-observer and inter-observer agreement was excellent (> 0.8) for all measured radiologic parameters.
Clinically, preoperative mHKA, AKSKS, AKSFS, and OKS were significantly improved at 1 year after TKA (Table 1). Four of five patients who had changes in FNMA greater than 15° perceived changes in the foot progression angle postoperatively. All these patients had an increase in tibial torsion larger than 10° and perceived the external rotation of the foot progression angle after TKA.
Discussion
The most important finding of the present study was that the tibia torsion was not significantly changed after TKA using the tibiofemoral synchronization technique. This finding suggests that the tibial component can be placed near to natural rotational axis of proximal tibia by the tibiofemoral synchronization technique. In addition, this technique provided good rotational alignment between the femoral and tibial component, which may improve tibiofemoral and patellofemoral tracking in primary TKA. The lower limb rotation as determined by the FNMA increased, which was found to be weakly correlated with a decrease in femoral anteversion. Our study did not support our hypothesis that the tibial torsion would change significantly after TKA because the tibiofemoral synchronization technique sets the rotational alignment of the tibial component regardless of proximal tibial anatomy.
Theoretically, if the femoral component is well aligned to the sTEA, synchronization of the rotational alignment of the tibial baseplate with the femoral component in extension reproduces the sTEA on the cut surface of the tibia intraoperatively. Our results showed that the mismatch between the sTEA and the mean rotational alignment of the tibial component established by the tibiofemoral synchronization technique was 1.5 ± 3.8°, which demonstrates that this technique can reproduce the sTEA on the tibia. Similarly, Berhouet et al. [4] reported that the tibial baseplate was placed in 1.9 ± 4.9° of internal rotation from the anatomic TEA using the self-alignment technique. Jung et al. [13] also reported that synchronization using a Liker system allowed rotational alignment of 0.6 ± 1.9° between the tibial component and the sTEA. Our study confirms that tibiofemoral synchronization technique accurately reproduces the sTEA on the cut surface of the tibia in cases in which the femoral component is well aligned to the sTEA.
Given the high variability in proximal tibial morphology, we assumed that it is difficult to expect whether the tibial component is positioned externally or internally using the tibiofemoral synchronization technique. Berhouet et al. [4] found that the tibial component was placed from − 4.1° to 22.5° relative to the native posterior condylar axis of the proximal tibia using the self-alignment technique, which supports our assumption. In our study, a mean value of tibia torsion was not changed significantly after TKA. However, 11% of knees had changes in the tibial torsion greater than ± 10° after TKA, suggesting that the tibial component can be placed by the tibiofemoral synchronization technique in large amount of external or internal rotation from the native posterior condylar axis of the proximal tibia (proximal reference of tibia torsion in this study) in some patients. Therefore, the rotational alignment of the tibial baseplate should be double-checked using several anatomical landmarks intraoperatively.
The lower limb rotation can be affected by external or internal rotation of the tibial component in combination with a 3–5° external rotation of the femoral component—a combination often used in TKA [9, 19]. If both components are rotated externally, the lower limb rotational change would be small because the external rotation of the tibial component would decrease tibial torsion (compensatory effect of both components on lower limb rotation). However, lower limb rotation would be more externally rotated after TKA in cases in which the tibial component was rotated internally (increase in tibial torsion) in combination with the external rotation of the femoral component (synergic effect of both components on lower limb rotation). In our study, four of five patients who had changes in FNMA greater than 15° perceived changes in the foot progression angle postoperatively. All these patients had an increase in tibial torsion larger than 10°. Given that the femoral component was rotated externally after TKA, the amount of limb rotational change might be additionally affected by the large amount of internal rotation of the tibial component (increase in tibia torsion) in these patients. Even though our study showed that changes in FNMA were correlated with changes in femoral anteversion, it should be kept in mind that a synergic effect of increase in the tibial torsion by the internal rotation of the tibia component can affect the patients’ perception about the lower limb external rotation after TKA.
A systematic review has shown that Akagi’s line is the most reliable landmark for the rotational alignment of the TC in TKA [20]. However, it has been reported that the angles between Akagi’s line and the perpendicular line to the sTEA ranged from − 19.7° (internal rotation) to 15° (external rotation) [1, 2, 12, 14,15,16, 22, 23]. Furthermore, our study showed that the variation in rotational mismatch between the projected sTEA on the tibia and Akagi’s line was large (0.1–19.1°). Given the high interindividual variability in proximal tibial anatomy, using Akagi’s line alone is not recommended for determining the rotational alignment of the tibial component. Fixed anatomic landmarks may cause tibial component malrotation in some patients. CT is useful to determine the projected sTEA on the tibia but it may not be available routinely because of its high cost. We believe that the tibiofemoral synchronization technique reproduces the sTEA on the cut surface of the proximal tibia regardless of individual tibial anatomy and may help surgeons identify the location of the projected sTEA on the tibia.
This study has a number of limitations. First, our results may not be applicable to other conditions beyond the inclusion criteria and different implant designs. In addition, axial parameters were measured in fully extended knees. Therefore, FNMA, foot progression angle, and the rotational mismatch between the femoral component and tibial component may be different at other flexion angles. Second, several methods to measure the femoral anteversion and the tibial torsion have been reported [21]. Therefore, our results might be affected by the measurement method. We selected methods showing high inter- and intra-observer reliability for each parameter. In addition, our primary interest was determining the amount of change between before and after TKA because this approach was less likely to be affected by measurement methods than determining absolute values. Third, the foot progression angle was not measured objectively. Instead, total lower limb rotation was assessed by measuring the FNMA [18]. Furthermore, the question on patients’ perception of changes in the foot progression angle was not validated, which may be affected by patients’ psychometric status. Fourth, most enrolled patients were female (89%). Anatomic differences between male and female could affect the results. Further study will be needed to investigate whether there is a gender difference regarding a change in limb rotation after TKA. Finally, no comparison group using other techniques, lack of power analysis for sample size calculation, and short-term clinical outcomes are also limitations of this study. Notwithstanding these limitations, we believe that our study provides clinically important information on changes in tibial torsion and lower limb rotation after TKA using the tibiofemoral synchronization technique.
Conclusions
Our study shows that the tibiofemoral synchronization technique less likely affects the tibial torsion after primary TKA. The limb rotation as determined by the FNMA can increase, which is more likely correlated with changes in femoral anteversion.
References
Aglietti P, Sensi L, Cuomo P, Ciardullo A (2008) Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res 466:2751–2755
Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C (2005) Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res 436:172–176
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Berhouet J, Beaufils P, Boisrenoult P, Frasca D, Pujol N (2011) Rotational positioning of the tibial tray in total knee arthroplasty: a CT evaluation. Orthop Traumatol Surg Res 97:699–704
Dalury DF (2001) Observations of the proximal tibia in total knee arthroplasty. Clin Orthop Relat Res 389:150–155
Eun IS, Kim OG, Kim CK, Lee HS, Lee JS (2013) Validation of the Korean version of the Oxford knee score in patients undergoing total knee arthroplasty. Clin Orthop Relat Res 471:600–605
Fang CH, Cheng CK, Qu TB, Zhang JH, Zhang B, Hua Q, Yan SG (2019) The posterolateral corner-locked technique Is applicable in a Chinese population regarding the tibial component rotation alignment in total knee arthroplasty. J Knee Surg 5:466–473
Fowler JR, Ilyas AM (2011) The accuracy of digital radiography in orthopaedic applications. Clin Orthop Relat Res 469:1781–1784
Hauschild O, Muenzberg M, Knothe D, Konstantinidis L, Helwig P, Sudkamp NP, Thielemann FW (2013) Rotational limb alignment changes following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2346–2354
Hirakawa M, Miyazaki M, Ikeda S, Matsumoto Y, Kondo M, Tsumura H (2017) Evaluation of the rotational alignment of the tibial component in total knee arthroplasty: position prioritizing maximum coverage. Eur J Orthop Surg Traumatol 27:119–124
Huddleston JI, Scott RD, Wimberley DW (2005) Determination of neutral tibial rotational alignment in rotating platform TKA. Clin Orthop Relat Res 440:101–106
Ikeuchi M, Yamanaka N, Okanoue Y, Ueta E, Tani T (2007) Determining the rotational alignment of the tibial component at total knee replacement: a comparison of two techniques. J Bone Joint Surg Br 89:45–49
Jung WH, Seo JG, Kim DH, Balabadra S, Mandot U, Kumar D (2020) Optimal rotational positioning of tibial component in total knee arthroplasty: determined by linker surgical technique using a high definition CT. Arch Orthop Trauma Surg 140:401–408
Khan MS, Seon JK, Song EK (2012) Rotational profile of lower limb and axis for tibial component alignment in varus osteoarthritic knees. J Arthroplasty 27:797–802
Kim CW, Seo SS, Kim JH, Roh SM, Lee CR (2014) The anteroposterior axis of the tibia in Korean patients undergoing total knee replacement. Bone Joint J 96:1485–1490
Kim JI, Jang J, Lee KW, Han HS, Lee S, Lee MC (2017) Anterior tibial curved cortex is a reliable landmark for tibial rotational alignment in total knee arthroplasty. BMC Musculoskelet Disord 18:252
Lee DH, Seo JG, Moon YW (2008) Synchronisation of tibial rotational alignment with femoral component in total knee arthroplasty. Int Orthop 32:223–227
Liodakis E, Aljuneidi W, Krettek C, Ettinger M, Kenawey M (2011) The neck-malleolar angle: an alternative method for measuring total lower limb torsion that considers the knee joint rotation angle. Skeletal Radiol 40:617–621
Maderbacher G, Baier C, Springorum HR, Maderbacher H, Birkenbach AM, Benditz A, Grifka J, Keshmiri A (2017) Impact of axial component alignment in total knee arthroplasty on lower limb rotational alignment: an in vitro study. J Knee Surg 30:372–377
Saffarini M, Nover L, Tandogan R, Becker R, Moser LB, Hirschmann MT, Indelli PF (2019) The original Akagi line is the most reliable: a systematic review of landmarks for rotational alignment of the tibial component in TKA. Knee Surg Sports Traumatol Arthrosc 27:1018–1027
Shih YC, Chau MM, Arendt EA, Novacheck TF (2020) Measuring lower extremity rotational alignment: a review of methods and case studies of clinical applications. J Bone Joint Surg Am 102:343–356
Shukla S, Upadhyaya V, Goel M, Gupta S (2019) Antero-posterior axis of tibia in patient undergoing total knee replacement in Indian population. J Clin Orthop Trauma 10:96–101
Tao K, Cai M, Zhu Y, Lou L, Cai Z (2014) Aligning the tibial component with medial border of the tibial tubercle–is it always right? Knee 21:295–298
Tsukeoka T, Lee TH, Tsuneizumi Y, Suzuki M (2014) The tibial crest as a practical useful landmark in total knee arthroplasty. Knee 21:283–289
Ueyama H, Minoda Y, Sugama R, Ohta Y, Yamamura K, Nakamura S, Takemura S, Nakamura H (2020) Malrotation of the fixed-bearing posterior stabilized total knee prosthesis causes a postoperative rotational mismatch between the femur and tibia. Knee Surg Sports Traumatol Arthrosc 28:3810–3820
Valkering KP, Breugem SJ, van den Bekerom MP, Tuinebreijer WE, van Geenen RC (2015) Effect of rotational alignment on outcome of total knee arthroplasty. Acta Orthop 86:432–439
Acknowledgements
The authors thank Editage (www.editage.co.kr) for English-language editing.
Funding
We did not receive outside funding related to this study.
Author information
Authors and Affiliations
Contributions
JHB: study concepts/design and manuscript drafting/revision, JWL: data acquisition/analysis, SHK: data acquisition/analysis, SGK: data acquisition/analysis and manuscript revision, YSJ: data acquisition/analysis and manuscript revision, and JSC: data acquisition/analysis and manuscript revision. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he has no commercial associations (e.g. consultancies, stock ownership, equity interest, and patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
Ethical approval
This study was approved by the institutional ethical review board (2016GR0311).
Informed consent
The informed consent was obtained from each patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bae, J.H., Lee, JW., Kim, SH. et al. Femoral matched tibia component rotation has little effect on the tibial torsion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30, 698–704 (2022). https://doi.org/10.1007/s00167-020-06429-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06429-z