Abstract
Introduction
The rotational alignment of femoral and tibial components is an important determinant of the success of Total Knee Arthroplasty (TKA). The optimal rotational position of the tibial component is still unclear. The purpose of this study was (1) to determine the pre-operative S-TEA (surgical-transepicondylar axis) derived tibialanteroposterior (AP) axis angle and postoperative tibial component axis angle using a “Bird’s eye” high-definition CT image in TKA performed by Linker surgical technique; (2) to determine the femorotibial mismatch angle; and (3) to determine the optimal tibial component rotation in a well-aligned femoral and tibial components.
Materials and methods
55 knees in 49 osteoarthritis patients who underwent primary TKA by Linker surgical technique were evaluated. Preoperative tibial AP axis angle, and the postoperative tibial component axis angle were measured. Rotational mismatch between femoral and tibial components was also measured.
Results
The mean angle of the pre-operative tibial AP axis was 17.8° ± 4.0°, ranging from 4.3° to 25.4°. The mean angle of the post-operative tibial component axis was 16.2° ± 4.9°, ranging from 3.8° to 25.2°. The mean postoperative tibial component axis line was at 14.2% ± 11.9%.
Conclusion
Because of the variability of pre-operative S-TEA derived tibial AP axis angle, the tibial component axis angle was also variable among the knees, but the two angles bore a strong correlation to each other. Based on our results, the optimal axis of the tibial component passes about halfway through the medial edge and medial one-third of the tibial tuberosity.
Level of evidence
Level II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The rotational position of the tibial component in TKA has received far less attention than the rotational position of the femoral component [1, 2]. Several authors have advocated the transepicondylar axis (TEA) as a reproducible and reliable reference axis for the femur [3, 4]. However, the optimal rotational position of the tibial component is unclear [5,6,7]. Most commonly used landmarks for tibial component rotation are the TT, posterior condyles of the cut proximal tibial surface or the ankle malleolar axis. Another method is by assessing the rotational position of the femur and tibia when the knee is held in full extension and the ligaments taut [8].
The intrinsic differences in the anatomical landmarks of individual bones of the femur and tibia can cause a rotational mismatch between the femoral and tibial components postoperatively. This can be avoided by realigning the tibial component to match the femoral component [2]. Linker surgical technique is a new method by which femoral rotation can be directly transferred to the tibial side by the use of a special instrument, thus avoiding any rotational mismatch between the femoral and tibial components [9,10,11,12].
While the femoral component rotation may easily be assessed relative to the epicondylar axis by using a single axial computed tomography (CT) image, malrotation of the tibial component has been difficult to define and evaluate. Most of the proposed techniques use multiple transposed axial CT images to compare tibial component rotation either to the femoral TEA or to a variety of tibial landmarks [13,14,15,16,17,18]. As a result of these inconsistent and complicated measurement techniques, it is difficult to draw definitive conclusions about the optimal tibial component rotation.
To address these issues a single axial “Bird’s eye” image of the proximal tibia using a high-definition CT with three-dimensional reconstruction and metal suppression with prosthesis overlay [19] was used. To our knowledge, no prior studies have assessed pre-operative S-TEA derived tibial AP axis angle, and post-operative tibial component rotation angle using these images. This imaging technique was used to establish the optimal position of the tibial component.
The purpose of this study was (1) to determine the pre-operative S-TEA (line connecting medial epicondylar sulcus and lateral epicondyle) derived tibial AP axis angle and postoperative tibial component axis angle using a “Bird’s eye” high-definition CT image in TKA performed by the Linker surgical technique, (2) to determine the femorotibial mismatch angle, and (3) to determine the optimal tibial component rotation in a well aligned TKA.
Materials and methods
Patient selection
Fifty-five knees in 49 patients who underwent primary TKA for the treatment of osteoarthritis were evaluated prospectively. The patients comprised 39 women and 10 men (Table 1), with ages of 71.5 ± 5.9 (range 61–86). All surgeries were performed with a posterior-stabilized design implant (Lospa, Corentec Inc, Cheonan, Korea) by a single surgeon.
Subjects were excluded if they had a flexion contracture or varus of greater than 15°, previous fracture of the distal femur or if the S-TEA could not be measured. Patients with postoperative femoral component rotation greater than 3° in relation to S-TEA, and those with a femorotibial mismatch angle of greater than 3° were also excluded. By this exclusion, optimal rotation of the tibial component could be measured in a knee with ideally placed components. This study was approved by the institutional review board at the author’s institution.
Surgical technique
We calculated the inter-femoral head distance (IFD) pre-operatively on AP radiographs of the pelvis using picture archiving and communication system (PACS, General Electric, Milwaukee, WI, USA). The patient was placed in a supine position. A customized graduated ruler with two mobile pegs with distance corresponding to the IFD was fitted to a pelvic stabilizer. A center rod of the ruler was located on the pelvic midline passing through symphysis pubis (Fig. 1a). When any difficulty in identifying the center of femoral head was encountered, as in the case of obese patients or patients with pelvic obliquity, a portable X-ray machine was used to confirm if the pegs corresponded to the hip center.
a Patient positioned with graduated ruler attached to the pelvic stabilizer. The distance between the mobile pegs is equal to the IFD and a fixed central peg passes along midline. b Distal femoral block attached to the extramedullary guide and placed parallel to S-TEA. c Extramedullary guide with coronal and sagittal alignment rods. d Femoral rotation transferred to tibial side by linker. e Rotational axis for placement of the tibial component: line drawn parallel to the tibial pins and centering the midpoint of PCL attachment posteriorly
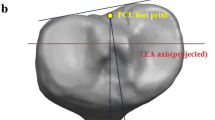
Following a standard medial parapatellar approach and soft tissue balancing, a point for the distal femur was marked about 1 cm superior to the insertion of PCL. The femoral external rotation was determined preoperatively as the angle between the posterior condylar line and S-TEA on a CT scan. A distal femoral block was placed parallel to the S-TEA using an external rotation jig and fixed with two pins (Fig. 1b). An extramedullary guide was mounted on this block. Two alignment rods were then passed through this guide, one corresponding to the coronal axis (from the center of the knee to the center of the hip) and the other corresponding to the sagittal axis (Lateral femoral epicondyle to the anterior margin of Greater trochanter) (Fig. 1c). An anterior skim cut was taken. A distal femur cutting guide was then attached to the Linker and aligned with the tibia [11] (Fig. 1d). S-TEA derived tibial axis was obtained by drawing a line parallel to the tibial pins and centering the PCL attachment posteriorly (Fig. 1e). By this technique, femoral rotation was transferred to the tibia. Patellar resurfacing was done routinely and implants were fixed with cement.
CT evaluation
CT scan images of all patients were obtained before and after surgery, with the limb in a neutral position. We used a helical CT machine (Somatome, Erlangen, Siemens, Germany) to obtain 2-mm slice images. Measurements were performed using advanced visualization software syngo. via a CT Vascular (Siemens, Erlangen, Germany). Three acquisition zones (hip, knee, and ankle) were defined on an AP scout view. The distal femoral and proximal tibial 3D computed tomography cuts were superimposed to measure relative translation and rotation.
Preoperative S-TEA derived tibial AP axis angle, and the post-operative tibial component rotation angle were assessed using a single axial “Bird’s eye” image of the proximal tibia using high-definition CT [19].
Identification of the geometric center on CT images was different from the method used by other authors [2, 15, 20,21,22]. 3D CT cuts of the distal femur and proximal tibia were then superimposed. For the femur, we used a cut in which both femoral epicondyles and the medial sulcus was optimally visualized and for the tibia, we used the cut with the most prominent part of the TT (Fig. 2a, b). The geometric center of the tibia was then identified (Fig. 2c). S-TEA line was first drawn from the sulcus of the medial epicondyle to the lateral epicondyle. Lines were then drawn parallel to the S-TEA at the anterior and posterior margins of the tibial plateau. The mid-points of these lines were then marked. The mid-point of a line perpendicular to the S-TEA connecting these two points was identified as the geometric center of the tibia. S-TEA derived tibial AP axis angle was measured preoperatively using the geometric center as a starting point. The angle was formed by a line perpendicular to the S-TEA and a line passing through the tip of the TT (Fig. 2d). Postoperatively, this angle was compared with the angle of the tibial component axis (Fig. 3). The medial percentage width of the intersection point of the TT was measured (Fig. 4) and the mismatch angle between the posterior femoral condylar line and posterior tibial component line was calculated (Fig. 5). Postoperative femoral component angle was obtained by measuring the angle between the S-TEA and the line along the posterior condyles of the femoral component (Fig 6).
Axial CT scan of the proximal tibia; a projection of S-TEA. b Lines drawn parallel to the S-TEA through the tibial margins anteriorly and posteriorly, and perpendicular to the S TEA, medially and laterally. c Identification of the geometric center of the tibial plateau. d Measurement of S-TEA derived tibial AP axis angle at the geometric center: between a line perpendicular to the derived S-TEA and a line drawn from the most prominent part of TT
Statistical analysis
Statistical analysis was performed using SPSS version 12.0 (SPSS, Chicago, IL, USA). Variables that correlated with the tibial component axis angle were investigated (Table 2).
All axial images were evaluated by two independent observers (HJH, SJH). The entire process was repeated independently, from point gathering to measurement. The reliability of each measurement was then calculated by using interclass correlation coefficients and intraclass correlation coefficients analysis for inter-observer agreement.
Probability values of < 0.05 were considered significant. Pearson’s correlation coefficient r was interpreted as follows: < 0.20, slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and > 0.81, almost perfect agreement.
Results
The measurements on the CT images showed wide variability in pre-operative tibia AP axis angle. The mean angle of the S-TEA derived tibial AP axis angle was 17.8° ± 4.0° (range 4.3°–25.4°). The mean angle post-operative tibial component axis angle was 16.2° ± 4.9° (range 3.8°–25.2°) (p < 0.001, r = 0.685) (Table 1). A strong correlation was found between the tibial component rotation angle and the S-TEA derived tibial AP axis angle (Table 2).
The axis of the tibial component did not intersect the medial border or the medial one-third of the TT. The mean postoperative tibial component axis line was at 14.2% of the width of the TT (Table 1), which is about halfway through the medial border and medial one-third of the TT.
The mismatch angle between the femoral and tibial components was 0.6° ± 1.9° (range − 2.7° to 6.2°) (Table 1).
Discussion
We found the mean pre-operative S-TEA derived tibial AP axis angle to be 17.8° ± 5.3° (range 4.3°–25.4°), and the tibial component axis angle to be 16.2° ± 4.9°, (range 4.3°–25.4°). We also found that the optimal tibial component axis passed about halfway through the medial border and medial one-third of the TT, which is at 14.2% from the medial edge of the TT.
Three distinct intraoperative methods of determining tibial component rotation have been described (1) anatomical placement of an asymmetrical tibial tray on the cut surface; (2) the self-seeking method, in which the tibial component is rotated into alignment following the femoral component during extension; [15] and (3) rotation of the tibial tray relative to the TT (usually using the junction of the medial and central thirds of the TT as anatomical landmarks [2, 23, 24]. Unfortunately, many of these references vary among patients and are difficult to establish.
Several authors have reported the tibial component rotation being a cause of discomfort after TKA. Nicoll and Rowley [22] compared painful and pain-free knees in 740 posterior stabilized TKAs and found that internal rotation of the tibial component by > 9° (in relation to the neutral TT axis) was a major cause of pain and functional deficit following TKA. Bedard et al. [15] investigated preoperative tibial and femoral component rotation in 34 TKAs, revised for stiffness, and found pathological tibial internal rotation in 33 cases, suggesting that excessive internal tibial rotation can lead to poor motion, patellar tracking complications, and anterior knee pain [10].
A review of the literature was undertaken and our results were compared with other studies on tibial component rotation.
Incavo et al. defined the optimal position to be between the midportion of the medial third of the ligament and the midportion of the entire patellar ligament (17–50% of the distance from the medial side of the ligament) [25]. Comparing with our results, the tibial components of Incavo et al. are externally rotated. The use of clinical TEA and patellar tendon instead of S-TEA and TT as a reference may be the cause.
Berger et al. reported that the normal rotational value for the tibial component, corresponding to the native articular surface, was 18° ± 2.6° of internal rotation from the tip of the TT [26]. Our data’s pre-operative S-TEA derived tibial AP axis angle was 17.8° ± 4.0°, which is similar to Berger’s result. But we were unable to establish the methodological details of Berger’s report. Berger may have used the posterior condylar line of the tibial plateau.
Our results showed that the mean tibial component axis is more externally rotated than the Akagi line. The difference could be due to the fact that our study assessed Osteoarthritic knees whereas Akagi studied normal ones. In a similar study, Joong II Kim et al. [27] compared normal knees with osteoarthritic knees and concluded that the proximal tibial AP axes of the osteoarthritic knee showed greater internal rotation.
Khan et al. [28] mentioned the posterior tibial condylar axis as more reliable and accurate for tibial component placement than TEA in varus osteoarthritic knees because of the change in tibial torsion and knee rotation with OA progression. However, they have not assessed the postoperative tibiofemoral component mismatch angle, which is significant.
Range of motion (ROM) technique remains the only method described to transfer the femoral rotation to tibia. Ikeuchi et al. reported that this method left the tibial component more internally rotated [29]. Other authors have reported that the ROM method is reliable only if the femoral component is well aligned and the soft tissues balanced [14]. We think the ROM method is an effective way to reproduce the femoral TEA axis to the tibia, with these two prerequisites. In comparison, the Linker system is a more easily reproducible and reliable instrument to transfer femoral rotation to the tibia. Using the Linker technique our mean mismatching angle was 0.6°, the standard deviation 1.9° (range − 2.7° to 6.2°). When comparing to Uehera et al. [2], 96% of our patients had an angle of 5° or less.
A limitation of the current study is the reproducibility of imaging and measurement techniques in knees with deformities. Because the direction of scanning was aligned to the longitudinal axis of the tibia, the direction of the CT slice for the femur varied according to the varus and flexion contracture. Our study excluded patients with more than 15° flexion contracture and varus. Therefore variation in slice direction could have little impact on the results. Our method of CT evaluation cannot be used for TKA performed using asymmetric tibial components.
The Linker system can be a helpful tool to transfer femoral rotation to the tibia and to reduce rotational mismatch after TKA. To assess the tibial component rotation, the use and comparison of the preoperative S-TEA derived tibial AP axis angle and the postoperative tibial component rotation angle using high-definition CT “Bird’s eye” imaging is recommended.

Conclusion
The variability of the pre-operative S-TEA derived tibial AP axis angle was reflected in the tibial component axis angle, and the two showed a strong correlation. Based on our results, the optimal axis of the tibial component passes about halfway through the medial edge and medial one-third of the TT. The Linker system is an effective method to transfer the femoral rotation to the tibia, thereby reducing the incidence of femorotibial rotational mismatches.
References
Baldini A, Indelli PF, De Luca L, Mariani PC, Marcucci M (2013) Rotational alignment of the tibial component in total knee arthroplasty: the anterior tibial cortex is a reliable landmark. Joints 1(4):155–160
Uehara K, Kadoya Y, Kobayashi A et al (2002) Bone anatomy and rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 402:196–201
Franceschini V, Nodzo SR, Gonzalez Della Valle A (2016) Femoral component rotation in total knee arthroplasty: a comparison between transepicondylar axis and posterior condylar line referencing. J Arthroplast 31(12):2917–2921
Jabalameli M, Moradi A, Bagherifard A, Radi M, Mokhtari T (2016) Evaluation of distal femoral rotational alignment with spiral CT scan before total knee arthroplasty (a study in Iranian population). Arch Bone Jt Surg 4(2):122–127
Indelli PF, Graceffa A, Marcucci M, Baldini A (2016) Rotational alignment of the tibial component in total knee arthroplasty. Ann Transl Med 4(1):3
Saffi M, Spangehl MJ, Clarke HD, Young SW (2019) Measuring tibial component rotation following total knee arthroplasty: what is the best method? J Arthroplast 7S:S355–S360
Kim JI, Jang J, Lee KW, Han HS, Lee S, Lee MC (2017) Anterior tibial curved cortex is a reliable landmark for tibial rotational alignment in total knee arthroplasty. BMC Musculoskelet Disord 18(1):252
Eckhoff DG, Piatt BE, Gnadinger CA, Blaschke RC (1995) Assessing rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 318:176–181
Seo JG, Moon YW, Lim JS et al (2012) Mechanical axis-derived femoral component rotation in extramedullary total knee arthroplasty: a comparison between femoral transverse axis and transepicondylar axis. Knee Surg Sports Traumatol Arthrosc 20:538
Lee DH, Seo JG, Moon YW (2008) Synchronisation of tibial rotational alignment with femoral component in total knee arthroplasty. Int Orthop 32:223–227
Seo JG, Moon YW, Kim SM, Park SH (2015) How to minimize rotational conflict between femoral and tibial component in total knee arthroplasty-the use of femoro-tibial axial synchronizer (linker). Yonsei Med J 56(2):454
Jung WH, Chun CW, Jeong JH (2013) The accuracy of the extramedullary and intramedullary femoral alignment system in total knee arthroplasty for varus osteoarthritic knee. Knee Surg Sports Traumatol Arthrosc 21(3):629–635
Mitsuhashi S, Akamatsu Y, Kobayashi H, Kusayama Y, Kumagai K, Saito T (2018) Combined CT-based and image-free navigation systems in TKA reduces postoperative outliers of rotational alignment of the tibial component. Arch Orthop Trauma Surg 138(2):259–266
Amanatullah DF, Ollivier MP, Pallante GD, Abdel MP, Clarke HD, Mabry TM, Taunton MJ (2017) Reproducibility and precision of CT scans to evaluate tibial component rotation. J Arthroplast 32(8):2552–2555
Bedard M, Vince KG, Redfern J, Collen SR (2011) Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res 469:2346–2355
Incavo SJ, Wild JJ, Coughlin KM et al (2007) Early revision for component mal-rotation in total knee arthroplasty. Clin Orthop Relat Res 458:131–136
Lakstein D, Zarrabian M, Kosashhvili Y et al (2010) Revision total knee arthroplasty for component mal-rotation is highly beneficial. J Arthroplast 25:1047–1052
Lützner J, Krummenauer F, Wolf C et al (2008) Computer-assisted and conventional total knee replacement. A comparative, prospective, randomized study with radiological and CT evaluation. J Bone Joint Surg Br 90:1039–1044
Roper GE, Bloemke AD, Robert CC, Spangehl MJ, Clarke HD (2013) Analysis of tibial component rotation following total knee arthroplasty using 3D High definition computed tomography. J Arthroplast 28:106–111
Ma Y, Mizu-Uchi H, Okazaki K, Ushio T, Murakami K, Hamai S, Akasaki Y, Nakashima Y (2018) Effects of tibial baseplate shape on rotational alignment in total knee arthroplasty: three-dimensional surgical simulation using osteoarthritis knees. Arch Orthop Trauma Surg 138(1):105–114
Berhouet J, Beaufils P, Boisrenoult P, Frasca D, Pujol N (2011) Rotational positioning of the tibial tray in total knee arthroplasty: a CT evaluation. Orthop Traumatol Surg Res 97:699–704
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 92:1238–1244
Scott RD (2013) Femoral and tibial component rotation in total knee arthroplasty: methods and consequences. Bone Joint J 95-B(Suppl 1):140–143
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Incavo SJ, Coughlin KM, Pappas C, Beynnon BD (2003) Anatomic relationships of the proximal tibial, distal femur, and patella. J Arthroplast 18:643–648
Berger RA, Seel MJ, Schleiden M et al (1993) Computerized tomographic determination of the normal tibiofemoral rotational angles: a guide to tibial component rotational alignment in TKA. Orthop Trans 17:1174
Kim Joong Il, Jang Jak, Lee Ki Woong, Han Hyuk Soo, Lee Sahnghoon, Lee Myung Chul (2017) Anterior tibial curved cortex is a reliable landmark for tibial rotational alignment in total knee arthroplasty. BMC Musculoskelet Disord 18:252
Khan MS, Seon JK, Song EK (2012) Rotational profile of lower limb and axis for tibial component alignment in varus osteoarthritic knees. J Arthroplast 27(5):797–802
Ikeuchi M, Yamanaka N, Okanoue Y, Ueta E, Tani T (2007) Determining the rotational alignment of the tibial component at total knee replacement. J Bone Joint Surg Br 89:45–49
Acknowledgements
The authors would like to thank Prof. Yong Chan Ha and Jian Kang for their advice and expert technical assistance with the statistical analysis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Design of study: WHJ and JGS. Analysis of data: DHK, SB, UM, DK. Writing of manuscript: SB and UM. Supervision of study: WHJ and JGS. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Institutional Review Board approval was obtained. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jung, WH., Seo, JG., Kim, D.H. et al. Optimal rotational positioning of tibial component in total knee arthroplasty: determined by linker surgical technique using a high definition CT. Arch Orthop Trauma Surg 140, 401–408 (2020). https://doi.org/10.1007/s00402-020-03340-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03340-7