Abstract
Purpose
Contralateral medial meniscus posterior root tear (MMPRT) can sometimes occur after primary surgeries for MMPRT and lead to unsatisfactory outcomes. The incidence rate and risk factors for contralateral MMPRT have not been well investigated, despite their clinical importance. Therefore, the incidence and predictors of bilateral MMPRT were aimed to be evaluated.
Methods
Fourteen patients with bilateral MMPRT (group B) and 169 patients with unilateral MMPRT (group U) were enrolled in this study. Sex, age, body mass index, time between injury and surgery, and medial tibial slope angle (MTSA) were compared between the groups. MTSA was measured using lateral radiographs.
Results
The incidence rate of bilateral MMPRT was 6.2% among all patients with MMPRTs. Multivariate logistic regression analysis showed that a prolonged time between injury and surgery (odds ratio [OR], 1.0; 95% confidence interval [CI] 1.00–1.01; P < 0.05) and steeper MTSA (OR, 1.85; 95% CI 1.21–2.64; P < 0.01) were significantly associated with the development of bilateral MMPRT. Receiver operating characteristic curve analysis showed that MTSA > 10.0° was associated with bilateral MMPRT, with a sensitivity of 93% and specificity of 69%.
Conclusion
A longer time between injury and surgery and steeper MTSA were risk factors for the development of bilateral MMPRT. Surgeons need to pay close attention to the contralateral knee in addition to the primary injured knees when treating knees with steep MTSA. Besides, early meniscal repair of primary MMPRT would be important to prevent the events of contralateral MMPRT.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The posterior root of the medial meniscus (MM) can function as an anchor for regulating the meniscal shift during knee movement and load bearing. Pathologically, an MM posterior root tear (MMPRT) can accelerate degeneration of the articular cartilage in the knee joint by disrupting meniscal functions [3]. An increasing number of studies have been examining its biomechanical and clinical importance. Recent studies have demonstrated that MMPRT comprises 10–30% of meniscal injuries [4, 25]. MMPRT might occur mainly in middle-aged women with a painful popping during light activity, such as descending stairs or walking [1, 14, 16].
Despite the increased number of studies on MMPRT, there have been very few reports of the risks associated with MMPRT injuries [17, 24]. Variables including age, sex, body mass index (BMI), increased Kellgren–Lawrence (KL) grade, and knee alignment have all been reported to be associated with MMPRT [17]. Recently, increased angle of medial tibial slope (MTS) has been reported to be a risk factor for MMPRT and the average MTS angle (MTSA) in patients with MMPRT was reported as 7.2° measured using magnetic resonance imaging (MRI) [24]. Biomechanical studies have shown that a steep MTSA leads to increased anterior tibial translation and anteroposterior instability that result in secondary stabilizer insufficiency (anterior cruciate ligament [ACL] or MM posterior horn [MMPH]) [15, 21, 28].
Regardless of a good postoperative course following primary MMPRT repair, contralateral MMPRT was diagnosed. The study was performed to evaluate the incidence and predictors of bilateral MMPRT, as there were no such studies to date. It was hypothesized that patients with increased MTSA and longer time between injury and surgery would be at increased risk for developing bilateral MMPRT.
Material and methods
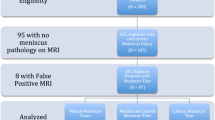
This study was approved by the University’s Institutional Review Board (approval no. 1857). All participants provided a written informed consent. The presence of MMPRT was defined in patients admitted to our institution from 2013 to 2019. The patients’ recorded data were retrospectively collected. This study included 227 patients who were diagnosed with MMPRT by two orthopedic surgeons according to the patients’ MRI findings after having painful popping events (Fig. 1) [6, 12]. Patients with MMPRT without a memory of painful popping (n = 32), those with previous meniscal injury and/or knee surgery (n = 5), and lack of radiographic data (n = 7) were excluded. Overall, 183 patients were enrolled in the study and retrospectively divided into two groups: patients with bilateral MMPRT (group B, n = 14) and unilateral MMPRT (group U, n = 169). The primary injured knee was evaluated using MRI analysis after a painful popping episode and at 20.8 days on average. Contralateral MRI was examined when the patients had painful popping event of the contralateral knee after primary surgery and no patients had undergone bilateral MRI during the same period. The diagnosis of MMPRT was confirmed during an arthroscopic evaluation or unicompartmental knee arthroplasty. The patients’ demographic information is shown in Table 1. The time of injury was set at the time of the painful popping episode.
The magnetic resonance images show characteristic signs of the MM posterior root tear in a 64-year-old woman (her left knee). a Coronal image. Giraffe neck sign of the MM posterior part (dotted area). The vertical linear defect called cleft sign (black arrowhead). b Sagittal image. A disappearance of the MM posterior root/horn called ghost sign (dotted area). MM medial meniscus
MTSA measurement
A goniometric measurement of the MTSA was performed on lateral radiographs by drawing two lines, as described by Brandon et al. [5], defined by the longitudinal axis of the tibia and the MTS, respectively. The MTSA was defined as 90° minus the angle made by the intersection of the line of the longitudinal axis of the tibia and the MTS. The MTSA value was rounded off to one decimal place. The longitudinal axis of the tibia was defined by the line created by connecting the midpoint of the anteroposterior diameter of the tibia just inferior to the tibial tubercle (line 1) and the midpoint of the anteroposterior diameter of the tibial shaft (line 2), measured no less than 5 cm distal to line 1 (Fig. 2).
MTSA measurement. The MTSA is defined as 90° minus the angle made by the intersection of the line along the longitudinal axis of the tibia and the medial tibial slope [5]. The black circle marks the MTSA. Lines 1 and 2 represent the anteroposterior diameters of the tibia just inferior to the tibial tubercle, and the tibial shaft no less than 5 cm distal to line 1, respectively. The line of the longitudinal axis of the tibia is made by connecting the midpoints of lines 1 and 2. MTS medial tibial slope, MTSA MTS angle
Statistical analysis
Statistical analysis was performed using EZR (Saitama Medical Center Jichi Medical University, Saitama, Japan). The Mann–Whitney U test or one-way analysis of variance with the post hoc Tukey HSD test was used to compare the MTSA between the two groups. The statistical significance level was set at P < 0.05. A multivariate logistic regression analysis was applied to the values as risk factors for contralateral MMPRT (Table 2). The MTSA cutoff associated with increased possibility to develop the contralateral MMPRT was determined by using receiver operating characteristic (ROC) analysis and calculating the Youden index (J) (Fig. 3). The inter-observer and intra-observer reliabilities were assessed with the intra-class correlation coefficient (ICC). An ICC > 0.83 was considered as a reliable measurement. To determine the inter-observer reproducibility, all radiographs were reviewed by two experienced orthopedic surgeons, and the values of the MTSA were investigated for calculating inter-observer reproducibility. One of the researchers reviewed the radiographs twice on two different occasions to calculate the intra-observer repeatability. The inter-observer reproducibility and intra-observer repeatability of the measurements and diagnosis of MMPRT using the MRI findings were satisfactory when the respective mean ICC values were 0.85, 0.87, 0.94, and 0.95, respectively. To determine the number of test samples, the outcome MTSA was used in the sample size calculation under a significance level of 0.05 and a power of 0.80. As a result, the required sample size was 13 patients in each group.
MTSA of the knees with unilateral and bilateral MMPRT. MTSA of the primary and contralateral knees with bilateral MMPRT were significantly steeper than that of knees with unilateral MMPRT. MTSA, medial tibial slope angle; MMPRT, medial meniscus posterior root tear. *Statistically significant (P < 0.01)
Results
Fourteen patients (6.2%) developed bilateral MMPRT (Table 1). There was no significant difference between the two groups in terms of age, BMI, and femorotibial angle. The time between injury and surgery (median, group B = 109 days; group U = 75 days; P < 0.001) and the MTSA (average, group B = 10.9°; group U = 8.3°; P < 0.001) were significantly different between the two groups. The median period from the primary MMPRT to secondary MMPRT was 330 days (196–826 days).
The multivariate logistic regression model indicated that the odds of bilateral MMPRT increased with the time between injury and surgery (odds ratio [OR], 1.0; 95% confidence interval [CI] 1.00–1.01; P = 0.030) and with MTSA (OR, 1.85; 95% CI 1.21–2.64; P ≤ 0.001). Sex, age, and BMI were not associated with increased risk of bilateral MMPRT development (Table 2).
The MTSA was compared between the primary and contralateral sides in groups B and U. The MTSA of the primary side (10.9°) and that of the contralateral side (10.4°) were significantly steeper in group B than in group U (8.3°) (P = 0.001, P < 0.001, respectively). There was no significant difference in MTSA between the primary and contralateral sides in group B (Fig. 3).
According to the ROC analysis, the MTSA cutoff value associated with contralateral MMPRT was 10.0°, with a sensitivity of 93% and specificity of 69% (Fig. 4).
Discussion
The most important finding of this study was that the incidence rate of bilateral MMPRT was 6.2% in patients with MMPRT. A relationship was demonstrated between two predictive factors (steeper MTSA and longer time between injury and surgery) and bilateral MMPRT development.
Several studies have shown that MTSA plays a role in knee laxity and biomechanics [19]. Many researchers have evaluated the association between a steep MTSA and ACL insufficiency [11, 29, 31]. Previous biomechanical studies have shown that anteroposterior instability or anterior translation increases resulting in a proportional increase in MTSA [7, 15]. However, few studies have investigated the association between MTSA and the development of MMPRT [18, 24]. Okazaki et al. concluded that patients with MMPRT had significantly steeper MTSA (7.2°) than those with normal MTSA (3.5°), or ACL-injured knees (4.0°) [24]. They concluded that posterior rollback of the femur due to a steeper MTSA caused impingement of the MMPH, resulting in MMPRT. In our study, MTSA over 10° was found to be a risk factor for bilateral MMPRT development. This value of MTSA was steeper than the corresponding value in knees without MMPRT [5, 20, 22]. Steeper MTSA causes an increased anterior tibial translation, and a larger load stress on the MMPH, which plays a secondary, yet important, role in the knee joint stabilization [32, 33]. In patients with bilateral MMPRT, MTSA of the contralateral side was also significantly steeper than in knees of patients with unilateral MMPRT (Fig. 3). Therefore, steep MTSA and primarily injured knee increase the risk of injury in the contralateral knee. In all cases in group B, each primarily injured knee had a steeper or equal MTSA than the contralateral knee. This suggests that the MMPH with a steeper MTSA has a tendency to be injured first, which also suggests that MTSA has an influence on MMPRT.
In addition to MTSA, the amount of time between injury and surgery had a significant association with contralateral MMPRT injuries. Biomechanical studies have shown altered loading and compensatory movement patterns after ACL reconstruction, which may result in increased loads on the contralateral limb during dynamic movement patterns [10, 23, 27]. In patients with MMPRT, the longer time between injury and surgery increased the load on the patients’ contralateral knees preoperatively [26]. The majority of patients with bilateral MMPRT were not properly diagnosed prior to hospital admission, which resulted in a delayed surgery. Missed diagnoses and delayed treatment cause a rapid deterioration of the articular cartilage and subchondral bone, and relate to contralateral MMPRT [13]. An accurate and timely diagnosis of the primary MMPRT may reduce the risk of contralateral knee injury.
In general, MMPRT is more commonly observed in women than in men, which was confirmed in this study. Moreover, the proportion of female patients with bilateral MMPRT was significantly steeper than the corresponding fraction of those with unilateral MMPRT, though the results were not significant (OR, 5.79; 95% CI 0.6–52.7; n.s). Women have a steeper MTSA than men, resulting in an increased risk of MMPRT. Moreover, women tend to have a lower muscle mass than men, and would, therefore, be more affected by an increased load on the contralateral knee joint [30]. The weak quadriceps muscles may lead to increased stress on the articular cartilage or meniscus [8, 9, 30]. Thus, early rehabilitation preoperatively might reduce the risk of contralateral MMPRT.
This study had several limitations. First, the retrospective nature of this very limited cohort study (only 14 patients with bilateral MMPRT) is an inherent limitation. Second, a sample size of 14 patients with bilateral MMPRT was extremely small for conducting a multivariate logistic regression analysis, and, therefore, the validity of these findings is limited. Additional study with larger sample size with bilateral MMPRTs will be required to confirm the risk factor for bilateral MMPRTs. Third, the evaluation of the time between injury and surgery was unclear in some cases, and a control group was not provided for this variable. Fourth, other factors that increase the risk for MMPRT, such as KL grade, knee alignment, or medial and lateral tibial plateau concavity, were not examined in this study [2, 17, 24]. Fifth, this study only included patients with a clear onset of injury; thus, patients with non-symptomatic MMPRT without painful popping episodes might have been missed. Finally, biomechanical examinations in patients with bilateral MMPRT were not performed. Such investigations may help to confirm our findings. Surgeons need to pay close attention to not only the primary injured knee, but also the contralateral knee when treating knees with steep MTSA, especially > 10.0°. Immediate radiographic examinations including MRI would be useful when suspecting contralateral MMPRT. Besides, early pullout repair of MMPRT would be important to prevent the event of contralateral MMPRT.
Conclusion
It was demonstrated that the incidence of bilateral MMPRT was 6.2% in patients with MMPRT. Surgeons need to pay attention to the contralateral knee in addition to the primary injured knees when treating knees with steep MTSA. Besides, early meniscal repair after primary MMPRT would be important to prevent the event of contralateral MMPRT.
Change history
02 January 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00167-020-06412-8
References
Bae JH, Paik NH, Park GW, Yoon JR, Chae DJ, Kwon JH et al (2013) Predictive value of painful popping for a posterior root tear of the medial meniscus in middle-aged to older Asian patients. Arthroscopy 29:545–549
Barber FA, Getelman MH, Berry KL (2017) Complex medial meniscus tears are associated with a biconcave medial Tibial Plateau. Arthroscopy 33:783–789
Bhatia S, LaPrade CM, Ellman MB, LaPrade RF (2014) Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med 42:3016–3030
Bin SI, Kim JM, Shin SJ (2004) Radial tears of the posterior horn of the medial meniscus. Arthroscopy 20:373–378
Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF (2006) The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 22:894–899
Choi SH, Bae S, Ji SK, Chang MJ (2012) The MRI findings of meniscal root tear of the medial meniscus: emphasis on coronal, sagittal and axial images. Knee Surg Sports Traumatol Arthrosc 20:2098–2103
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Jt Surg Br 76:745–749
Eitzen I, Grindem H, Nilstad A, Moksnes H, Risberg MA (2016) Quantifying quadriceps muscle strength in patients with ACL injury, focal cartilage lesions, and degenerative meniscus tears: differences and clinical implications. Orthop J Sports Med 4:2325967116667717
Ericsson YB, Roos EM, Owman H, Dahlberg LE (2019) Association between thigh muscle strength four years after partial meniscectomy and radiographic features of osteoarthritis 11 years later. BMC Musculoskelet Disord 20:512
Ernst GP, Saliba E, Diduch DR, Hurwitz SR, Ball DW (2000) Lower extremity compensations following anterior cruciate ligament reconstruction. Phys Ther 80:251–260
Fening SD, Kovacic J, Kambic H, McLean S, Scott J, Miniaci A (2008) The effects of modified posterior tibial slope on anterior cruciate ligament strain and knee kinematics: a human cadaveric study. J Knee Surg 21:205–211
Furumatsu T, Fujii M, Kodama Y, Ozaki T (2017) A giraffe neck sign of the medial meniscus: a characteristic finding of the medial meniscus posterior root tear on magnetic resonance imaging. J Orthop Sci 22:731–736
Furumatsu T, Kamatsuki Y, Fujii M, Kodama Y, Okazaki Y, Masuda S et al (2017) Medial meniscus extrusion correlates with disease duration of the sudden symptomatic medial meniscus posterior root tear. Orthop Traumatol Surg Res 103:1179–1182
Furumatsu T, Okazaki Y, Okazaki Y, Hino T, Kamatsuki Y, Masuda S et al (2018) Injury patterns of medial meniscus posterior root tears. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2018.10.001
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32:376–382
Hiranaka T, Furumatsu T, Masuda S, Okazaki Y, Okazaki Y, Kodama Y et al (2020) A repair technique using two simple stitches reduces the short-term postoperative medial meniscus extrusion after pullout repair for medial meniscus posterior root tear. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-020-02647-w
Hwang BY, Kim SJ, Lee SW, Lee HE, Lee CK, Hunter DJ et al (2012) Risk factors for medial meniscus posterior root tear. Am J Sports Med 40:1606–1610
Khan N, McMahon P, Obaid H (2014) Bony morphology of the knee and non-traumatic meniscal tears: is there a role for meniscal impingement? Skelet Radiol 43:955–962
Liu W, Maitland ME (2003) Influence of anthropometric and mechanical variations on functional instability in the ACL-deficient knee. Ann Biomed Eng 31:1153–1161
Mansori AE, Lording T, Schneider A, Dumas R, Servien E, Lustig S (2018) Incidence and patterns of meniscal tears accompanying the anterior cruciate ligament injury: possible local and generalized risk factors. Int Orthop 42:2113–2121
Marouane H, Shirazi-Adl A, Hashemi J (2015) Quantification of the role of tibial posterior slope in knee joint mechanics and ACL force in simulated gait. J Biomech 48:1899–1905
Napier RJ, Garcia E, Devitt BM, Feller JA, Webster KE (2019) Increased radiographic posterior tibial slope is associated with subsequent injury following revision anterior cruciate ligament reconstruction. Orthop J Sports Med 7:2325967119879373
Neitzel JA, Kernozek TW, Davies GJ (2002) Loading response following anterior cruciate ligament reconstruction during the parallel squat exercise. Clin Biomech (Bristol, Avon) 17:551–554
Okazaki Y, Furumatsu T, Kodama Y, Kamatsuki Y, Okazaki Y, Hiranaka T et al (2019) Steep posterior slope and shallow concave shape of the medial tibial plateau are risk factors for medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05590-4
Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN (2008) Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 16:849–854
Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE (2012) Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med 22:116–121
Salem GJ, Salinas R, Harding FV (2003) Bilateral kinematic and kinetic analysis of the squat exercise after anterior cruciate ligament reconstruction. Arch Phys Med Rehabil 84:1211–1216
Shelburne KB, Kim HJ, Sterett WI, Pandy MG (2011) Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res 29:223–231
Stijak L, Herzog RF, Schai P (2008) Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc 16:112–117
Thorlund JB, Felson DT, Segal NA, Nevitt MC, Niu J, Neogi T et al (2016) Effect of knee extensor strength on incident radiographic and symptomatic knee osteoarthritis in individuals with meniscal pathology: data from the multicenter osteoarthritis study. Arthritis Care Res (Hoboken) 68:1640–1646
Todd MS, Lalliss S, Garcia E, DeBerardino TM, Cameron KL (2010) The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med 38:63–67
Toman CV, Dunn WR, Spindler KP, Amendola A, Andrish JT, Bergfeld JA et al (2009) Success of meniscal repair at anterior cruciate ligament reconstruction. Am J Sports Med 37:1111–1115
Westermann RW, Wright RW, Spindler KP, Huston LJ, Group MK, Wolf BR (2014) Meniscal repair with concurrent anterior cruciate ligament reconstruction: operative success and patient outcomes at 6-year follow-up. Am J Sports Med 42:2184–2192
Acknowledgements
We would like to thank Editage (https://www.editage.jp) for English language editing.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Institutional Review Board in Okayama University (Ethical approval No. 1857). All procedures involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Written informed consent was obtained from all study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Affiliation of author Takaaki Hiranaka updated.
Rights and permissions
About this article
Cite this article
Hiranaka, T., Furumatsu, T., Okazaki, Y. et al. Steep medial tibial slope and prolonged delay to surgery are associated with bilateral medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc 29, 1052–1057 (2021). https://doi.org/10.1007/s00167-020-06079-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06079-1