Abstract
Objective
Meniscal tears are an important cause of morbidity. The aim of this study was to examine the relationship between non-traumatic meniscal tears and the intrinsic bony morphology of the knee.
Methods
A retrospective analysis of 160 knee MRI scans in 150 patients was carried out who met the following criteria: (a) age between 20 and 45 years, (b) no history of knee trauma, surgery, infection, metabolic bone disease, and (c) no collateral or cruciate ligamentous injury. The medial tibial slope (MTS), lateral tibial slope (LTS), medial tibial plateau depth (MTPD), and medial and lateral femoral condylar offset ratios were calculated. The anterior horn, body, and posterior horn of the menisci were graded as 0 (no tear), 1 and 2 (degenerative changes), or 3 (definitive tear). One-way ANOVA and linear regression was used for statistical analysis.
Results
In patients with grade 3 tears of the posterior horn of the medial meniscus, there was a significant association with shallower MTS (p < 0.05), smaller medial femoral offset ratio (p < 0.05) and smaller lateral femoral offset ratio (p < 0.05). Patients with grade 3 tears of anterior horn of the lateral meniscus had a significant association with shallower LTS (p < 0.05). No significant association was seen between MTPD and meniscal tears.
Conclusions
Our results suggest an association between bony morphology of the knee and non-traumatic meniscal tears. Shallower MTS and LTS may result in impingement of posterior horn of medial meniscus and anterior horn of lateral meniscus, respectively. Future kinematic studies will be needed to help confirm our findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscal tears are a common problem worldwide and can lead to significant morbidity for young patients in their productive age. Several studies have helped advance our understanding of the risk factors leading to meniscal tears. In patients with degenerative meniscal tears, risk factors include advanced age (especially over 60 years of age), male gender, and work-related repetitive activities such as kneeling or squatting [1–3]. Participation in sports activities has been implicated in acute, traumatic meniscal tears [4]. The ligamentous support network of the knee, when compromised, can also lead to meniscal tears. For example, waiting more than 12 months after an anterior cruciate ligament injury and reconstructive surgery has also been shown to be a risk factor for medial meniscus tears [5]. Interestingly, previous arthroscopic literature has suggested that mechanical impaction of the knee can result in cartilage damage [6]. However, no prospective or retrospective study to date has investigated the relationship between meniscal tears and the underlying bony morphology of the knee. The purpose of our retrospective study was to explore the relationship between non-traumatic meniscal tears and the bony morphology of the knee, with specific emphasis on the concept of meniscal impingement in a cohort of patients without established risk factors for meniscal tears.
Materials and methods
All patients who underwent an MRI examination of the knee at our hospital between May 2010 and Oct 2012 were included in the study if they met the following criteria: (a) age between 20 and 45 years of age, (b) no previous history of knee trauma, surgery, infection, or metabolic bone disease as indicated on the self-reported clinical information sheets, and (c) no findings of cruciate or collateral ligament injury on the MRI examination. These patients were then selected for further analysis that consisted of calculating their lateral tibial slope, medial tibial slope, medial tibia plateau depth, medial femoral condylar offset ratio, and the lateral femoral condylar offset ratio. In addition, meniscal tears in the anterior horn, body, and the posterior horn of the medial and the lateral menisci were also graded and recorded. The scans were performed on either a 1.5-T Siemens MAGNETOM Avanto (Siemens AG, Munich, Germany) and consisted of high-resolution coronal PD (TR/TE = 1,300/39, slice = 0.7 mm, field of view = 150 mm), coronal PD FS (TR/TE = 3,510/31, Slice = 3 mm, field of view = 160 mm), axial PD FS (TR/TE = 3,960/30, slice = 3 mm, field of view = 160 mm), sagittal PD FS (TR/TE = 3,440/30, slice = 3 mm, field of view = 160 mm) and sagittal T1 (TR/TE = 396/11, slice = 4 mm, field of view = 150 mm) or a 3-T Siemens MAGNETOM Skyra (Siemens) and consisted of high-resolution coronal PD (TR/TE = 1,200/27, slice = 0.75 mm, field of view = 160 mm), coronal PD FS (TR/TE = 2,500/33, slice = 3 mm, field of view = 150 mm), axial PD FS (TR/TE = 3,500/33, slice = 3 mm, field of view = 160 mm), sagittal PD FS (TR/TE = 4,310/33, slice = 3 mm, field of view = 160 mm) and sagittal T1 (TR/TE = 971/12, slice = 3 mm, field of view = 160 mm). This study was approved by our Institutional Ethics Board and is in compliance with the Health Information and Protection Act (HIPA) regulations.
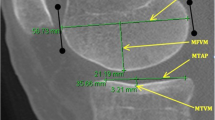
The medial and the lateral tibial slopes were calculated by one author (NK) in the same manner for each patient using the double-circle method [7]. A sagittal plane perpendicular to the coronal plane at the midpoint of the medial and lateral tibial plateau was selected for assessing the tibial slope (see Fig. 1a-b). The medial and the lateral femoral offsets were measured for each patient by one author (NK) and the offset ratio was calculated by dividing the posterior femoral offset by the femoral diaphysis width [8, 9] (see Fig. 1c-d). Both techniques have been previously validated in the literature with high reproducibility rates [8, 9]. The medial tibial plateau depth (MTPD) was measured by one author (NK) in the same manner for each patient (see Fig. 1e). The medial and lateral menisci were independently assessed by one fellowship-trained musculoskeletal radiologist (HO) with 11 years of clinical experience who was blinded to all other measurements. The medial and the lateral menisci were graded as follows: 0 = normal, 1 = amorphous signal, which does not abut the articular surface, 2 = linear signal, which does not abut the articular surface, 3 = linear signal, which contacts the articular surface (definitive tear). The image analysis and morphometric measurements were performed on a picture archiving and communications system (PACS).
Measurement of the tibial slope (a–b), femoral offset ratio (c–d), and medial tibia plateau depth (e). a Initial midline sagittal image is selected that outlines the tibial attachment of the PCL. A superior circle is drawn that connects the anterior, posterior, and superior cortex of the tibia. Second, an inferior circle is drawn that connects the anterior and posterior tibial cortex with its center positioned on the circumference of the superior circle. A longitudinal axis line is drawn that connects the centers of these two circles. Then, an orthogonal line, perpendicular to the longitudinal axis line, is drawn. b The orthogonal line is then copied onto a sagittal midline image of the middle of the medial (or lateral) tibia plateau. A straight line connecting the anterior and posterior cortical margins of the plateau is drawn and the angle between the straight line and the orthogonal line defines the tibial slope. c Using a sagittal midline image, the femoral diaphysis width is first measured 5 cm above the joint line (width in this case measured 28.4 mm). Then, a straight line along the posterior femoral cortex is drawn. d This straight line is then transposed onto a second sagittal image at the midpoint of each femoral condyle. Next, an orthogonal line is drawn from the straight line to the posterior most aspect of the femoral condyle (including the cartilage), which defined the posterior femoral offset (which measured 24 mm in this case). The offset ratio was calculated by dividing the femoral offset by the diaphysis width. e A sagittal image along the midpoint of the medial tibial plateau is selected and a line is drawn that connects the anterior and posterior superior cartilage. A second line parallel to this is drawn that intersects the subchondral bone at its maximum depth and the perpendicular distance between the two lines is defined as the medial tibial plateau depth
The influence of bony morphological factors (medial and lateral tibial slope, medial and lateral femoral offset ratio, and medial tibial plateau depth) on the grade of the meniscal tears (broken down across the different anatomic regions, e.g., anterior horn medial meniscus, body medial meniscus, etc.) was assessed by grouping patients into three categories, those without meniscal tears (control group - grade 0), those with degenerative meniscal changes (degenerative group - grade 1, 2) and those with meniscal tears (meniscal tear group - grade 3). For the purposes of statistical analysis, all tears within a specific anatomic region were combined together (e.g., analysis of the anterior horn of the medial meniscus would include all isolated tears of the anterior horn and tears, which extended to the body or body and posterior horn). One-way analysis of variance (ANOVA) with Tukey HSD test was used for statistical analysis using an online software package (GraphPad Software, 2013). Linear regression analysis was used to assess for intrinsic relationship between the tibial slopes and femoral offset ratios. The level of significance was set at p < 0.05. Data presented is mean (m), one standard deviation (sd), variance (v), F-ratio (f) and p value (p).
Results
Patient demographics
A total of 914 knees were initially analyzed for eligibility, and of these, 160 knees (150 patients) met the inclusion criteria and were included in the study. There were 74 females (74/150 = 49 %) and males (76/150 = 51 %). The average age of the patients was 33.4 ± 10.5 years. The overall distribution of meniscal tears across the different anatomical regions is summarized in Fig. 2 and the overall results are summarized in Fig. 3.
Distribution of the meniscal tears across the different anatomical regions. The above anatomical regions correspond to cooper’s meniscal zones as follows: posterior horn of medial meniscus = cooper’s zone A, body of medial meniscus = cooper zone B, anterior horn of medial meniscus = cooper’s zone C, anterior horn of lateral meniscus = cooper’s zone D, body of lateral meniscus = cooper’s zone E, posterior horn of lateral meniscus = cooper’s zone F [see Reference 10]
Medial meniscus—anterior horn
In the anterior horn of the medial meniscus, there was no statistically significant difference between the control group, degenerative group, and meniscal tear group with respect to the medial tibial slope (m3.3°, sd2.4°, v5.9° versus m3.7°, sd2.7°, v7.2° versus m1.5°, sd2.1°, v4.5°, f0.65, p0.52), lateral tibial slope (m4.2°, sd2.9°, v8.7° versus m3.7°, sd3.5°, v12.6° versus m5.0°, sd5.7°, v32.0°, f0.17, p0.84), medial femoral offset ratio (m0.89, sd0.15, v0.02 versus m0.85, sd0.13, v0.02 versus m0.94, sd0.13, v0.02, f0.30, p0.94), lateral femoral offset ratio (m0.86, sd0.14, v0.02 versus m0.81, sd0.14, v0.02 versus m0.97, sd0.19, v0.04, f1.16, p0.32) or the medial tibial plateau depth (m3.3, sd0.9, v0.8 versus m3.0, sd1.0, v1.1 versus m2.5, sd0.6, v0.4, f1.22, p0.30).
Medial meniscus—body
In the body of the medial meniscus, there was no statistically significant difference between the control group, degenerative group, and meniscal tear group with respect to the medial tibial slope (m3.6°, sd2.5°, v6.3° versus m3.3°, sd2.3°, v5.4° versus m2.1°, sd2.0°, v3.9°, f2.68, p0.07), lateral tibial slope (m4.4°, sd3.0°, v8.7° versus m4.2°, sd3.2°, v10.4° versus m3.3°, sd2.5°, v6.1°, f0.94, p0.39), medial femoral offset ratio (m0.90, sd0.15, v0.02 versus m0.90, sd0.16, v0.02 versus m0.81, sd0.14, v0.02, f2.59, p0.08), lateral femoral offset ratio (m0.87, sd0.14, v0.02 versus m0.86, sd0.14, v0.02 versus m0.79, sd0.15, v0.02, f2.24, p0.11) and the medial tibial plateau depth (m3.3, sd0.9, v0.8 versus m3.2, sd0.9, v0.8 versus m3.5, sd0.8, v0.6, f0.56, p0.57).
Medial meniscus—posterior horn
In the posterior horn of the medial meniscus, there was a statistically significant difference between the control group and the meniscal tear group with respect to the medial tibial slope (m3.8°, sd2.5°, v6.5° versus m2.4°, sd2.3°, v5.2°, f4.71, p0.01) (see Figs. 4 and 7) and the medial femoral offset ratio (m0.90, sd0.16, v0.02 versus m0.81, sd0.12, v0.01, f3.84, p0.02) (see Figs. 5 and 7) and the lateral femoral offset ratio (m0.88, sd0.15, v0.02 versus m0.78, sd0.10, v0.01, f5.77, p0.004) (see Figs. 6 and 7). There was no statistically significant difference between control group, degenerative group and the meniscal tear group with respect to the lateral tibial slope (m4.5°, sd3.0°, v8.9° versus m4.3°, sd3.0°, v9.3° versus m3.2°, sd2.7°, v7.4°, f1.91, p0.15) or medial tibial plateau depth (m3.3, sd0.9, v0.8 versus m3.3, sd0.8, v0.8 versus m3.3, sd0.9, v0.7, f0.07, p0.93).
The top left image shows the femoral diaphysis width in this patient to be 33.8 mm, measured 5.0 cm above the joint. The top middle image shows the medial femoral offset to be 25.5 mm. The top right image shows the lateral femoral offset to be 22.1 mm. The bottom left and middle images demonstrate the medial tibial slope in this patient, which was 1°. The bottom right image shows posterior horn meniscal tear abutting the inferior articular surface. The methods of calculating these bony morphometric measurements are described in Fig. 1a-e
Lateral meniscus—anterior horn
In the anterior horn of the lateral meniscus there was a statistically significant difference between the control group and the meniscal tear group with respect to lateral tibial slope (m4.4°, sd3.0°, v9.1° versus m1.7°, sd1.9°, v3.8°, f3.96, p0.02) (see Fig. 8). There was no significant difference between the control group, degenerative group, and meniscal tear group with respect to medial tibial slope (m3.4°, sd2.5°, v6.2° versus m3.2°, sd2.3°, v5.4° versus m2.9°, sd2.0°, v3.9, f0.18, p0.84), medial femoral offset ratio (m0.90, sd0.15, v0.02 versus m0.85, sd0.13, v0.02 versus m0.81, sd0.16, v0.03, f2.07, p0.13), lateral femoral offset ratio (m0.87, sd0.14, v0.02 versus m0.83, sd0.16, v0.02 versus m0.80, sd0.14, v0.02, f1.52, p0.22) or the medial tibial plateau depth (m3.3, sd0.9, v0.8 versus m3.3, sd0.8, v0.7 versus m2.9, sd0.8, v0.6, f0.78, p0.46).
Lateral meniscus—body
In the body of the lateral meniscus there was no statistically significant difference between the control group, degenerative group, and meniscal tear group with respect to the medial tibial slope (m3.3°, sd2.5°, v6.1° versus m3.4°, sd2.4°, v5.7° versus m3.6°, sd2.2°, v5.0°, f0.04, p0.96), lateral tibial slope (m4.3°, sd2.9°, v8.7° versus m3.1°, sd3.3°, v10.8° versus m3.7°, sd3.0°, v9.2°, f1.06, p0.35), medial femoral offset ratio (m0.90, sd0.15, v0.02 versus m0.82, sd0.12, v0.02 versus m0.85, sd0.12, v0.03, f1.60, p0.21), lateral femoral offset ratio (m0.87, sd0.14, v0.02 versus m0.78, sd0.12, v0.01 versus m0.84, sd0.19, v0.04, f2.62, p0.08) or the medial tibial plateau depth (m3.3, sd0.9, v0.8 versus m3.4, sd0.8, v0.7 versus m2.6, sd0.6, v0.4, f1.99, p0.14).
Lateral meniscus—posterior horn
In the posterior horn of the lateral meniscus there was no statistically significant difference between the control group, degenerative group, and meniscal tear group with respect to the medial tibial slope (m3.3°, sd2.5°, v6.1° versus m3.5°, sd2.2°, v4.7° versus m3.2°, sd2.2°, v4.7°, f0.02, p0.98), lateral tibial slope (m4.3°, sd3.0°, v8.9° versus m2.2°, sd2.3°, v5.4° versus m3.8°, sd3.1°, v9.7°, f1.54, p0.22), medial femoral offset ratio (m0.89, sd0.15, v0.02 versus m0.94, sd0.12, v0.01 versus m0.82, sd0.20, v0.04, f0.92, p0.40), lateral femoral offset ratio (m0.86, sd0.14, v0.02 versus m0.85, sd0.14, v0.02 versus m0.82, sd0.21, v0.04, f0.23, p0.79) or medial tibial plateau depth (m3.3, sd0.9, v0.8 versus m3.2, sd1.0, v1.1 versus m2.9, sd0.8, v0.7, f0.58, p0.56).
Correlation between tibial slope and femoral offset ratio
In our cohort of patients, there was a statistically significant association between a shallow medial tibial slope and smaller medial femoral offset ratio (p = 0.0003, see Fig. 9). In addition, patients with a smaller medial femoral offset ratio also demonstrated a smaller lateral femoral offset ratio (p < 0.0001, see Fig. 10).
Discussion
Meniscal tears are a common problem worldwide, and if left untreated, can lead to premature osteoarthrosis with significant pain and morbidity for the patient [11]. As a result, partial meniscectomies are a common procedure performed for its treatment. Meniscal tears can be broadly categorized into two groups, degenerative or traumatic in nature, and several etiologies or risk factors have been implicated in the past [12]. Despite this, many patients present with knee pain and are subsequently found to have meniscal tears but no established risk factors are discovered in these patients. Many of these patients are young patients, without any prior history of knee trauma or surgery, and there is no internal derangement in their knee apart from the meniscal tears, which raises the possibility that perhaps there are other factors yet to be identified. Interestingly, previous arthroscopic literature has suggested that mechanical impaction of the knee can result in cartilage damage. In a small series of six patients (seven knees) with anteromedial knee pain, McGuire et al. observed significant anteromedial femoral cartilage damage in patients with hyperextension during arthroscopy, raising the possibility of mechanical impaction and subsequent cartilage and/or meniscal damage [6]. Further to this, we hypothesize that the bony morphology of the knee may be responsible for meniscal tears secondary to impingement and abnormal contact forces. To test our hypothesis, we retrospectively studied a cohort of young patients without established risk factors for meniscal tears and correlated the findings with bony morphometric parameters in the knee, including medial and lateral tibial slopes, medial and lateral femoral condylar offset ratios, and the medial tibia plateau depth.
The incidence and distribution of meniscal tears across the different meniscal zones that we observed is similar to prior studies including an overall incidence of 3.1 % for isolated tears of the anterior horn of the lateral meniscus, which is comparable to other studies [13, 14]. Overall, we observed a significant association between shallower medial tibial slope and meniscal tears in the posterior horn of the medial meniscus with no such association seen between the control group and the degenerative group. It has been previously established that there is an inherent tightness in the medial compartment due to the tight medial collateral ligament and the fixed capsular attachment of the medial meniscus [15, 16]. Therefore, we hypothesize that meniscal entrapment of the posterior horn of medial meniscus within a tight medial compartment could occur as a result of the shallower medial tibial slope and this may be exacerbated during periods of knee flexion. We also observed a significant association between meniscal tears in the posterior horn of the medial meniscus and small medial and lateral femoral offset ratios but this is likely on the basis of the association between shallower medial tibial slope and smaller medial femoral offset ratio. This association has been previously established in the literature [9] and we were able to replicate that in our study. In addition, we observed a strong association between a small medial femoral offset ratio and a small lateral femoral offset ratio suggesting that this may be a natural compensatory matched pattern in individuals with shallower medial tibial slope.
In contrast to our findings in the medial meniscus, we observed a statistically significant association between a shallow lateral tibial slope and tears of the anterior horn of the lateral meniscus. Previous literature has shown that increasing lateral tibial slope causes an anterior shift in the resting position of the tibia with respect to the femur and vice versa [17]. We speculate that a shallower lateral tibial slope would then cause a posterior shift in the resting position of the tibia and bring the anterior horn of the lateral meniscus more in contact with the lateral femoral condyle, and in this regard, it would be subject to greater impingement and contact forces, and this is likely exaggerated during extension. In addition, the screw-home mechanism of the knee from flexion to full extension is a unique motion during which the tibia externally rotates about 5° during full extension (stance phase), therefore tightening the cruciates and locking the knee into place to relieve the quadriceps muscle during standing position; however, during flexion (swing phase) the tibia internally rotates as the knee is unlocked by the popliteus muscle [18]. As a result of this, a pivot-type of motion, helped by the medial tibial plateau depth, takes place in the medial compartment and a "posterior rollback" type of motion of the femur occurs in the lateral compartment. This posterior rollback of the contact surface of the femur is helped by the normal posterior down-sloping of the lateral tibial plateau [18]. Our findings suggest that a reduced posterior down-sloping is likely to have caused biomechanical alteration to the posterior rollback of the femur resulting in impingement of the anterior horn of the lateral meniscus and predisposing it to meniscal tears. Future kinematic studies will greatly help to further our understanding of this association. Finally, we did not observe a significant association between a shallow or deep medial tibia plateau depth and meniscal tears in our study population. This was an interesting observation as previous literature has shown an association between a shallow medial tibial plateau depth and risk of ACL injury [19].
There were several limitations to our study. The retrospective design of the study was an inherent limitation. The overall sample size was another limitation and this was reflected by our variance within certain sample groups, and future studies with larger patient cohorts would be helpful to confirm our findings. Information regarding previous trauma was gleaned from self-administered patient questionnaires, which is subject to recall bias on behalf of the patient. Our study also did not correlate the imaging findings of meniscal tears with surgical findings. Finally, our patients did not undergo kinematic testing or arthroscopic correlation, which may be an area of future research and will help shed further light on this subject.
Conclusions
Our results suggest an association between bony morphology of the knee and non-traumatic meniscal tears. Meniscal tears of the posterior horn of the medial meniscus were found to have an association with shallower medial tibial slope and smaller medial and lateral femoral offset ratio. Meniscal tears of the anterior horn of the lateral meniscus were associated with shallower lateral tibial slope. Future kinematic studies with arthroscopic correlation will be needed to help confirm our findings.
References
Rytter S, Jensen LK, Bonde JP, Jurik AG, Egund N. Occupational kneeling and meniscal tears: a magnetic resonance imaging study in floor layers. J Rheumatol. 2009;36:1512–9.
Englund M, Guermazi A, Gale D, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359:1108–15.
Bhattacharyya T, Gale D, Dewire P, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85-A:4–9.
Baker P, Reading I, Cooper C, Coggon D. Knee disorders in the general population and their relation to occupation. Occup Environ Med. 2003;60:794–7.
Church S, Keating JF. Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg (Br). 2005;87:1639–42.
McGuire DA, Barber FA, Hendricks SD. Meniscal impingement syndrome. Arthroscopy. 1996;12(6):675–9.
Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066–72.
Johal P, Hassaballa MA, Eldridge JD, Porteous AJ. The posterior condylar offset ratio. Knee. 2012;19(6):843–5.
Cinotti G, Sessa P, Ripani FR, et al. Correlation between posterior offset of femoral condyles and sagittal slope of the tibial plateau. J Anat. 2012;221(5):452–8.
Cooper DE, Arnoczky SP, Warren RF. Meniscal repair. Clin Sports Med. 1991;10(3):529–48.
Baker P, Coggon D, Reading I, et al. Sports injury, occupational physical activity, joint laxity, and meniscal damage. J Rheumatol. 2002;29:557–63.
Snoeker BA, Bakker EW, Kegel CA, Lucas C. Risk factors for meniscal tears: a systematic review including meta-analysis. J Orthop Sports Phys Ther. 2013;43(6):352–67.
Metcalf MH, Barrett GR. Prospective evaluation of 1485 meniscal tear patterns in patients with stable knees. Am J Sports Med. 2004;32(3):675–80.
Terzidis IP, Christodoulou A, Ploumis A, et al. Meniscal tear characteristics in young athletes with a stable knee: arthroscopic evaluation. Am J Sports Med. 2006;34(7):1170–5.
Messner K, Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat. 1998;193:161–78.
Masouros SD, McDermott ID, Amis AA, Bull AM. Biomechanics of the meniscus-meniscal ligament construct of the knee. Knee Surg Sports Traumatol Arthrosc. 2008;16(12):1121–32.
Giffin JR, Vogrin TM, Zantop T, et al. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376–82.
Freeman MA, Pinskerova V. The movement of the normal tibio-femoral joint. J Biomech. 2005;38(2):197–208.
Hashemi J, Chandrashekar N, Mansouri H, et al. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):54–62.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khan, N., McMahon, P. & Obaid, H. Bony morphology of the knee and non-traumatic meniscal tears: Is there a role for meniscal impingement?. Skeletal Radiol 43, 955–962 (2014). https://doi.org/10.1007/s00256-014-1867-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-014-1867-9