Abstract
Purpose
The aim of this study was to examine and evaluate the factors associated with changes in limb alignment 10 years after total knee arthroplasty (TKA). The hypothesis was that bone morphology and immediate postoperative alignment could be correlated with long-term post-operative alignment changes following TKA.
Methods
This study retrospectively analysed 136 consecutive primary TKA cases for varus deformity, performed from 2006 to 2008, that could be followed for at least 10 years postoperatively. Anteroposterior long-leg weight-bearing radiographs were obtained within 1 month and at least 10 years after surgery. The hip–knee–ankle (HKA) angle immediately after surgery was compared with that 10 years later; factors correlating with the change in HKA angle (δHKA) were evaluated.
Results
The mean HKA angles were significantly different between immediate and long-term postoperative assessments (0.1° ± 1.9° vs. 1.2° ± 2.9°, p < 0.001). Furthermore, a significant difference was observed in the outlier ratio (> 3° deviation from the 0° of HKA angle) (10% vs. 24%, p = 0.002). δHKA strongly correlated with a higher preoperative tibial plateau tip-to-proximal tibial shaft (TPTPS) angle, higher postoperative HKA angle, lateral distal femoral angle, and lower postoperative medial proximal tibial angle.
Conclusion
Varus deformity in the proximal part of the tibia, immediate postoperative varus alignment, and varus position of the femoral and tibial components may lead to varus progression in limb alignment in the long term, even 10 years after TKA; the surgeon should, therefore, weigh the risks of leaving a varus alignment during surgery. Moreover, if the preoperative TPTPS angle is high, the alignment may become varus after TKA, even in patients who have acquired neutral alignment.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Postoperative neutral limb alignment has generally been considered a prerequisite for successful total knee arthroplasty (TKA) [6]. Despite obtaining a neutral mechanical alignment, such as a hip-knee-ankle (HKA) angle of 0° after TKA, a low patient satisfaction score of 57.5% has been reported [13]. Bellemans et al. have stated that a physiologically normal human has a varus alignment of > 3°, termed as constitutional varus, the incidence being approximately 32% in men and 17% in women [3]. A study further suggested that the incidence of constitutional varus is higher in Asian than in Western nations (40% in men and 28% in women) [14]. Moreover, for patients with constitutional varus, the aforementioned study indicated that restoring neutral alignment after TKA might be unnatural and would result in excessive medial soft tissue release. A novel classification for the phenotype of the coronal lower limb alignment in young osteoarthritic knees has been introduced and 40% of the study group showed neutral alignment only [7]. Furthermore, only 5.6% men and 3.6% women were found with a knee phenotype representing neutral alignment for both femur and tibia, which is the target of mechanically aligned TKA [7, 8]. Vanlommel et al. showed that patients with preoperative varus limb alignment had better clinical and functional outcome scores when mild varus alignment was retained than when corrected to the neutral position [21]. Furthermore, Slevin et al. demonstrated no correlation between neutral postoperative TKA mechanical alignment and better clinical outcomes using three-dimensional computed tomography (3D-CT) in patients with a preoperative varus of 3° or more [19].
However, the abovementioned phenomenon remains controversial. There are several reasons why surgeons cannot concur on the best alignment method. As reported by Hirschmann et al., described above, the phenotype varies across individuals [7], and it is difficult to target a unified alignment for all patients. Another reason is that the immediate postoperative alignment obtained after TKA may not be preserved in the long term. For example, if the surgeon intends to achieve even a slight varus alignment, it may become severe varus in the long term, which may affect the durability of TKA. Regarding the time-dependent change in limb alignment, Matsumoto et al. showed that bone morphology, including an elevation in tibial plateau inclination, might contribute to the worsening of varus deformity in osteoarthritic knees [14]. Park et al. reported that the mean change in mechanical axis between examinations in the immediate postoperative period and 10 years later was greater in the outlier group (> 3° deviation from neutral alignment) than in the acceptable group (within ± 3° from neutral alignment) [16]. Thus, unknown factors may influence the change of lower limb alignment after TKA in the long term.
Therefore, this study aimed to examine the change in limb alignment 10 years after TKA and to evaluate factors correlated with this change. The hypothesis was that postoperative limb alignment may change with varus progression 10 years after TKA, and the change may correlate with bone morphology and immediate postoperative alignment. This is the first study to evaluate long-term alignment changes and related factors, and is expected to aid surgeons in determining the optimal alignment to aim for.
Materials and methods
A consecutive group of 185 primary mechanically aligned TKA was performed on 172 patients during the period from 2006 to 2008, were screened. To ensure fair radiographic assessment, patients with preoperative neutral or valgus alignment (6 patients), osteoarthritis from other aetiologies (e.g., post-traumatic, rheumatoid, or inflammatory arthritis) (4 patients), severe bony defects needing bone grafting/augmentation or revision surgeries owing to infection during follow-up (1 patient), or postoperative flexion contracture > 5° (3 patients) were excluded. The remaining 158 patients (168 TKAs) met the inclusion criteria. Among them, 130 patients (136 TKAs) could be followed for 10 years after surgery. Two patients died. Twenty-six patients were lost to follow-up. None of these patients experienced implant loosening.
Therefore, 136 TKAs in 130 patients with varus osteoarthritis (96 women and 34 men; mean age, 74.6 [49–90] years) were retrospectively included in this study. Patients underwent TKA using posterior-stabilised prostheses (Nexgen LPS Flex, Zimmer, USA [n = 64]; PFC Sigma, DePuy Synthes, USA [n = 35]; e-motion PS, B. Braun Aesculap, Germany [n = 11]) and cruciate-retaining implants (Nexgen CR Flex [n = 10]; e-motion CR [n = 16]). Patients had a mean preoperative coronal alignment of 12.6° (1.0–27.3; NEUHKA0° [n = 3], VARHKA3° [n = 10], VARHKA6° [n = 13], VARHKA > 9° [n = 111] [7]) in terms of the HKA angle, and the minimum follow-up period was 10 years. The surgeries were performed by a single surgeon with more than 10 years of experience with mechanically aligned TKA. This study was approved by the Institutional Review Board of the authors’ affiliated institutions (identification number: 1510), and informed consent was obtained from all patients.
Radiological assessment
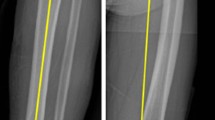
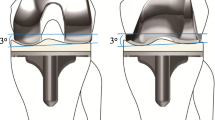
All preoperative and postoperative anteroposterior long-leg weight-bearing radiographs were obtained according to a previously reported standardised protocol [4]. To obtain long-leg weight-bearing radiographs, the patient’s patella was placed forward, and ankle was in the neutral position to unify the rotation. The patients were always instructed to stand upright with fully extended knees with the heels and greater toes in contact. The x-ray beam was directed perpendicular to the detector and centred on the knee from a distance of 2 m. Voltage and current were set at 200 mA and 85 kV, respectively. The preoperative radiographs were obtained within 1 month before surgery. The postoperative radiographs were taken within 1 month after surgery (immediate postoperative) and at least 10 years after surgery (long-term postoperative). The HKA angle, which is the angle between a line connecting the hip centre and the knee centre and another line connecting the knee centre and the ankle centre, was measured. The hip centre was defined as the centre of a circle that fits the contour of the femoral head. Preoperatively, the knee centre was set as the intersection of the midline between the femoral condyles and the tip of the tibia, and the midline between the tibial spines (Fig. 1a, b). Postoperatively, the knee centre was determined as the intersection of the midline between the condyles of the femoral component and the tip of the tibial component, and the midline of the polyethylene inlay (Fig. 1c, d). The ankle centre was defined as the middle of the talus roll at the level of the joint gap. Furthermore, the lateral distal femoral angle (LDFA) and medial proximal tibial angle (MPTA) were measured preoperatively and immediately after surgery (Fig. 1b, d). Preoperatively, the LDFA was defined as the angle between the femoral transcondylar tangent and the mechanical axis of the femur, and the MPTA was defined as the angle between the tibial articular marginal line and the mechanical axis of the tibia (Fig. 1b). Postoperatively, LDFA was calculated between the line parallel to the femoral component and the mechanical axis of the femur. MPTA was measured between the line parallel to the tibial baseplate and the mechanical axis of the tibia (Fig. 1d). To assess the preoperative bone morphology of the proximal tibia, based on a previous study, the tibial plateau tip-to-proximal tibial shaft (TPTPS) angle was defined as the angle between the line from the tip of the tibial plateau to the midpoint of the tibial shaft, 7.5 cm distal to the tibial plateau and the proximal tibial shaft line (Fig. 1e) [14].
Evaluation and statistical analysis
The HKA angle measured 10 years after TKA was compared with that measured immediately after TKA using the paired student t test. According to previous studies, neutral alignment is set at ± 3° of the mechanical axis [15], and traditionally, surgeons have performed surgery with the target of neutral alignment. Therefore, more than 3° deviation from an HKA angle of 0° (HKA angle, either < 3° or > 3°) was defined as an outlier and the outlier ratio was compared between the two groups using the chi-squared test.
The change in HKA angle (δHKA angle; long-term postoperative minus immediate postoperative) was noted. Pearson’s correlation coefficient and simple linear regression analyses were performed to determine the association of δHKA angle with multiple factors including age, body mass index (BMI), preoperative TPTPS angle, and preoperative and postoperative LDFA, MPTA, and HKA angle. Furthermore, multiple linear regression was performed with independent factors that were found to correlate significantly in the simple linear regression analysis.
To examine the reproducibility of this method, two observers measured the HKA angle, LDFA, MPTA, and TPTPS angle twice, with a 2-month interval, using a subset of 20 cases. Intra-observer and inter-observer reliabilities were evaluated with the intra-class correlation coefficient (ICC). Intra-observer reliability of the ICCs for intra- and inter-observer reliability were > 0.8 (range 0.82–0.94) for all measurements (Table 1). Based on the reliability observed above, measurements made by a single investigator were used in the analyses.
The data are shown as means ± standard deviations. Data analyses were performed using PASW Statistics 21 (SPSS, Chicago, IL). A value of p < 0.05 represented a statistically significant difference. A power analysis indicated that a minimum sample size of 115 subjects would be required using G*Power version 3.121, when alpha was set as 0.05, power (1 − β) at 0.95, and with a correlation ρH1 of 0.3 for simple linear regression [2].
Results
The mean HKA angles were significantly different between the immediate and long-term postoperative assessments (+ : varus alignment; −: valgus alignment, 0.1° ± 1.9° vs. 1.2° ± 2.9°, p < 0.001), and the HKA angle ranged between − 3.1° and 13.0° (1.1° ± 2.3°). The incidence of outliers was 14 of 136 (10%) immediately after surgery and 33 of 136 (24%) at ≥ 10 years postoperatively; a significant difference was observed between the two groups (p = 0.002) (Fig. 2).
The values of factors evaluated for correlation with δHKA are shown in Table 2. Pearson’s correlation analysis and simple linear regression analyses demonstrated that the δHKA was positively correlated with the preoperative TPTPS angle (R = 0.29, p < 0.001), postoperative LDFA (R = 0.21, p = 0.014), and postoperative HKA angle (R = 0.47, p < 0.001), and negatively correlated with postoperative MPTA (R = − 0.40, p < 0.001) (Fig. 3). Correlation with other factors was not found in the present study.
Furthermore, multivariate linear regression analyses showed that significant linear relationships between δHKA and preoperative TPTPS angle and postoperative LDFA and MPTA were maintained (Table 3). The postoperative HKA angle, which may affect the postoperative LDFA and MPTA, was excluded from the independent variables.
Discussion
The most important findings of the present study were that the HKA angle significantly changed with varus progression 10 years after TKA and that the change correlated with a higher preoperative TPTPS angle, higher postoperative LDFA and HKA angle, and lower postoperative MPTA, suggesting that varus deformity in the proximal part of the tibia, immediate postoperative varus alignment, and the varus position of the femoral and tibial components may lead to varus progression in limb alignment in the long term after TKA.
Recently, many studies have reported that mechanical alignment is inadequate for predicting knee prosthetic loading during gait, knee function, and long-term TKA implant survival [8, 18] and have suggested alternative anatomical surgical techniques [1]. TKA targeting under-corrected alignment has attracted attention as one of the techniques, since Bellemans et al. advocated the concept of “constitutional varus” [3]. Following the trend, favourable clinical outcomes in postoperative mild varus alignment after TKA were shown in patients with preoperative varus osteoarthritis after a mean follow-up period of 7.2 years and 3.6 years by Vanlommel et al. [21] and Nishida et al. [15] respectively. However, these assessments of postoperative radiographs were single time-point analyses and were not conducted over time. Therefore, it is unclear how postoperative alignment changes after surgery, making it difficult for the surgeon to set an acceptable range for allowing varus alignment with regard to predicting long-term clinical results and survivorship. In addition, a systematic review by Riviere et al. reported that few studies have assessed long-term survivorship after the preservation of slight or moderate constitutional deformity following TKA and concluded that a longer follow-up period was needed to define the best indication for an alternative surgical technique to conventional mechanically aligned TKA [17]. In the present study, significant varus progression was noted, and the outlier rate increased 10 years after surgery. δHKA was up to 13°, and in some individuals, the alignment may change to higher values over a long term period even with conventional mechanically aligned TKA, suggesting that the indications for targeting under-correction during TKA should be carefully considered.
In order to assess the risk factors for the aforementioned cases, simple and multivariate linear regression analyses were performed in this study and showed that the preoperative TPTPS angle, and postoperative LDFA, HKA angle, and MPTA were significantly associated with varus progression following TKA. Matsumoto et al. demonstrated that the TPTPS angle increased with the degree of varus deformity, whereas the tibial proximal–distal shaft angle did not change significantly in subjects with osteoarthritis, indicating that the tibial deformation in moderate-stage osteoarthritis originates from the proximal part of the tibia rather than from the shaft [14]. Even during the long-term period after TKA, the TPTPS angle indicative of proximal tibia deformation was significantly influenced by varus progression, while there was no significant association with the MPTA calculated from the tibial shaft. However, patients who undergo TKA have severe osteoarthritis, unlike the moderate osteoarthritis reported by Matsumoto et al. [14], and it is unlikely that the TPTPS angle will increase further after surgery. Thus, our findings suggest that the patients with varus deformity in the proximal tibia experienced mild migration due to higher medial compression in contrast to those without this deformity. In clinical practice, it is difficult to assess the tibial proximal axis, as surgeons generally perform osteotomy referring to the tibial shaft axis during TKA. Hence, the surgeon should measure the TPTPS angle for preoperative planning.
Surgical strategies for patients with high TPTPS angles are controversial. Since the alignment in these patients may progress to varus in the long-term period, and even if mild varus alignment is gained intra-operatively, the alignment may demonstrate even more varus progression, which may cause implant loosening. However, neutral alignment (an immediate postoperative HKA angle of 0.05° ± 1.92°) was the aim in this study, and even patients that acquired neutral alignment progressed to varus deformity if the TPTPS angle was high. Therefore, considering that immediate neutral alignment with a high TPTPS angle eventually progresses to varus in the long-term period, a high preoperative TPTPS angle may be a good indication for preserving mild varus alignment such as in kinematically aligned TKA [9].
Teeter et al. reported that increased varus in the tibial component resulted in growing implant migration and that overall postoperative varus limb alignment was correlated with isolated lateral compartment lift-off, which occurs more commonly than in neutral alignment 10 years after TKA [20]. However, Lee et al. advocated that varus mal-positioning of the femoral component was the main cause of the varus outliers in limb alignment and was a risk factor for aseptic revision compared with neutral femoral positioning after a mean follow-up of 8 years [12]. In addition, the aseptic loosening was reported to occur most commonly on the tibial side, and it was argued that varus mal-positioning of the femoral component may affect tibial loosening. Both simple and multiple linear regression analyses in our study showed that immediate postoperative varus limb alignment and varus positioning of both the femoral and tibial components were associated with varus progression of limb alignment 10 years after TKA. The above evidence and our findings suggest that these three factors may be mutually influential and are independent factors that lead to increased varus mal-alignment. Although several studies have reported that varus mal-positioning of the tibia increases failure rates [11], good long-term survivorship of kinematically aligned TKA, in which a tibial component was placed more varus than in a mechanically aligned TKA, has recently been reported [9]. The reason for this is that the valgus positioning of the femoral component may weaken the effects of the femoral side of the tibia. However, the varus alignment of the tibial component may progress independently; hence, the changes in the alignment of kinematically aligned TKA over time should be evaluated in the future.
Our study had several limitations. First, it included patients who underwent posterior-stabilised and cruciate-retaining TKAs. However, since a previous study demonstrated no statistically significant difference in radiographic alignment between the two prostheses postoperatively [10], it is believed that there was no difference in outcomes due to the design variation. Second, this study included several types of implants, and the influence of each implant on alignment needs to be evaluated in future. Third, the proportion of women is higher than that of men in this study. As reported by Hirschmann et al. [7], knee phenotypes are different between women and men, which may affect the alignment change after TKA. In future, research to analyse the sex ratio in this regard will be necessary. Fourth, clinical scores were not assessed in this study. The long-term changes in alignment and the risk factors shown in the present study may affect clinical outcomes. Hence, the evaluation of clinical scores is necessary in future studies. Fifth, all assessments were made using long-leg standing radiographs, which may be affected by rotation of the standing position. However, recently, Boonen et al. demonstrated the good reliability and validity of measurements using long-leg radiography compared with 3D-CT [4]. Therefore, we believe our results were not affected by the chosen imaging modality. Sixth, soft tissue balance which may affect postoperative alignment [5] was not evaluated in this study. In future, soft tissue laxity such as the varus-valgus stress test should be assessed. Finally, although there were no patients with implant loosening in this study, it is yet unknown whether the noted progress in varus alignment would be limited to mild migration or lead to loosening. Thus, a 15- or 20-year follow-up may be required to clarify this issue.
Conclusion
Based on the present study findings, the surgeon should ascertain the risks of leaving a varus alignment during surgery considering the possibility of potential varus progression in the long term. Furthermore, if the preoperative TPTPS angle is high, the alignment, even in patients who have acquired neutral alignment, may progress to varus after TKA. Our findings are expected to aid surgeons in determining the optimal alignment to aim for, when performing TKA.
References
Abdel MP, Oussedik S, Parratte S, Lustig S, Haddad FS (2014) Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Jt J 96-B:857–862
Bell ML, Teixeira-Pinto A, McKenzie JE, Olivier J (2014) A myriad of methods: calculated sample size for two proportions was dependent on the choice of sample size formula and software. J Clin Epidemiol 67:601–605
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Boonen B, Kerens B, Schotanus MG, Emans P, Jong B, Kort NP (2016) Inter-observer reliability of measurements performed on digital long-leg standing radiographs and assessment of validity compared to 3D CT-scan. Knee 23:20–24
Deep K (2014) Collateral ligament laxity in knees: what is normal? Clin Orthop Relat Res 472:3426–3431
Hirschmann MT, Becker R, Tandogan R, Vendittoli PA, Howell S (2019) Alignment in TKA: what has been clear is not anymore! Knee Surg Sports Traumatol Arthrosc 27:2037–2039
Hirschmann MT, Hess S, Behrend H, Amsler F, Leclercq V, Moser LB (2019) Phenotyping of hip-knee-ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg Sports Traumatol Arthrosc 27:1378–1384
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Howell SM, Shelton TJ, Hull ML (2018) Implant survival and function ten years after kinematically aligned total knee arthroplasty. J Arthroplasty 33:3678–3684
Kawakami Y, Matsumoto T, Takayama K, Ishida K, Nakano N, Matsushita T et al (2015) Intermediate-term comparison of posterior cruciate-retaining versus posterior-stabilized total knee arthroplasty using the new knee scoring system. Orthopedics 38:e1127–1132
Kim YH, Park JW, Kim JS, Park SD (2014) The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop 38:379–385
Lee BS, Cho HI, Bin SI, Kim JM, Jo BK (2018) Femoral component varus malposition is associated with tibial aseptic loosening after TKA. Clin Orthop Relat Res 476:400–407
Matsuda S, Kawahara S, Okazaki K, Tashiro Y, Iwamoto Y (2013) Postoperative alignment and ROM affect patient satisfaction after TKA. Clin Orthop Relat Res 471:127–133
Matsumoto T, Hashimura M, Takayama K, Ishida K, Kawakami Y, Matsuzaki T et al (2015) A radiographic analysis of alignment of the lower extremities–initiation and progression of varus-type knee osteoarthritis. Osteoarthritis Cartilage 23:217–223
Nishida K, Matsumoto T, Takayama K, Ishida K, Nakano N, Matsushita T et al (2017) Remaining mild varus limb alignment leads to better clinical outcome in total knee arthroplasty for varus osteoarthritis. Knee Surg Sports Traumatol Arthrosc 25:3488–3494
Park J-K, Seon J-K, Cho K-J, Lee N-H, Song E-K (2018) Is immediate postoperative mechanical axis associated with the revision rate of primary total knee arthroplasty? A 10-year follow-up study. Clinics in orthopedic surgery 10:167–173
Riviere C, Iranpour F, Auvinet E, Howell S, Vendittoli PA, Cobb J et al (2017) Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res 103:1047–1056
Riviere C, Ollivier M, Girerd D, Argenson JN, Parratte S (2017) Does standing limb alignment after total knee arthroplasty predict dynamic alignment and knee loading during gait? Knee 24:627–633
Slevin O, Hirschmann A, Schiapparelli FF, Amsler F, Huegli RW, Hirschmann MT (2018) Neutral alignment leads to higher knee society scores after total knee arthroplasty in preoperatively non-varus patients: a prospective clinical study using 3D-CT. Knee Surg Sports Traumatol Arthrosc 26:1602–1609
Teeter MG, Naudie DD, McCalden RW, Yuan X, Holdsworth DW, MacDonald SJ et al (2018) Varus tibial alignment is associated with greater tibial baseplate migration at 10 years following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:1610–1617
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330
Funding
No funding or external support was received by any of the authors in support of or in any relationship to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interests to declare.
Ethical approval
This study was approved by the Institutional Review Board of the authors’ affiliated institutions (identification number: 1510).
Informed consent
Informed consent was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuroda, Y., Takayama, K., Hayashi, S. et al. Varus deformity in the proximal tibia and immediate postoperative varus alignment result in varus progression in limb alignment in the long term after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 28, 3287–3293 (2020). https://doi.org/10.1007/s00167-019-05841-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05841-4