Abstract
Purpose
The purpose of the study was to determine the correlation between medial tibial slope (MTS) and anterior tibial translation (ATT) in female patients with an ACL-deficient knee. It was hypothesized that female patients with a greater medial tibial slope had an increased anterior tibial translation compared to males.
Methods
MTS and ATT were analysed in 276 patients (138 females and 138 males) with a complete ACL rupture from 2012 to 2016. The mean age was 32 ± 12 years. Previous surgery or additional ligament injury was excluded. CT scan was used for measuring MTS. Meniscal findings were reported. Anterior tibial translation and side to side difference (SSD) were measured by bilateral Telos™ stress radiography with knee flexion of 20°.
Results
There was no significant difference in ATT between females (5.4 ± 3.9) and males (5.8 ± 4.2), nor was there a difference in MTS between females (9.8 ± 2.8) and males (9.8 ± 2.7). A positive correlation was found between MTS and ATT absolute (r = 0.35, p < 0.001) and side to side difference (r = 0.12, p = 0.03). MTS greater or equal to 11° significantly increased the ATT (p < 0.05). For each degree of increase of the MTS, increases in ATT absolute of 0.6 mm and SSD of 0.18 mm were observed. Greater MTS was identified as a risk factor for an increase of ATT in females (r = 0.37, p < 0.001) but not in males (r = − 0.1, n.s). Increases of 1° of MTS increased ATT 0.57 mm in female patients (p < 0.001). MTS was influential in ATT despite the presence (r = 0.28 [0.11, 0.44], p = 0.001) or absence (r = 0.48 [0.35, 0.6], p < 0.001) of meniscal lesions.
Conclusions
Greater medial tibial slope is associated with increased anterior tibial translation in females with ACL-deficient knees compared to males, despite the presence or absence of meniscal lesions. This could be due to a quadriceps/hamstring imbalance in females and the ability of the hamstring muscles to moderate ATT.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) rupture is one of the most common knee injuries. Although it occurs frequently, controversies still remain regarding anatomical factors, neuromuscular control, and medial tibial slope and its relationship with anterior tibial translation.
There is an association between a high MTS and risk for ACL injury in adult [31] and current information about the specific influences of these risk factors on females [7, 10, 16] but correlations between gender and anatomic parameters as a risk factor for ACL injury have been reported in just one study [20]. A higher risk of non-contact ACL tear has been shown in women with an incidence two to five times that in men [30] and a previous study has shown a 33.7% greater risk of subsequent contralateral ACL reconstruction in female patients [21].
The influence of the tibial slope in anterior translation has been largely demonstrated. Dejour et al. [3] found a significant correlation between the tibial slope and the anterior translation of the tibia, both in healthy knees and with ACL rupture. They reported an increased ATT of 3.5 mm for every 10° of tibial slope (or 0.35 mm for each degree). The same author [4] describes that dynamic ATT appeared to increase significantly in knees with tibial slope greater than 12° (p = 0.041) but did not correlate with gender.
MTS seems to play an important role in the ATT in females according a recent study [29]. The ability to cope with ACL deficiency seemed to be affected by the tibial slope, especially in females, and this could be related to a quadriceps/hamstring imbalance in women. Liu and Maitland [14] demonstrated that in an ACL-deficient knee with 12° of tibial slope, anterior translation of the tibia could not be completely compensated by hamstring muscle force.
Knee laxity can be evaluated in different ways, including physical exam, using assessments with arthrometers (GnRB, KT 1000, KT 2000), or by radiological methods. Stress radiographs using an instrument such as Telos® system (Telos GmbH, Laubscher, Holstein, Switzerland) quantify objective and reproducible anterior laxity [1, 2, 11]. Panisset et al. [17] reported the correlation between radiological anteroposterior laxity using Telos system and the presence of a positive pivot shift test.
The aim of this study was to determine the effect of medial tibial slope on anterior tibial translation in the ACL-deficient knee in a cohort of patients with a first ACL rupture using CT scans and to determine the gender-specific correlations. The hypothesis was that female patients with a greater medial tibial slope had increased anterior tibial translation compared to males.
Materials and methods
A single-center retrospective study was conducted. Between 2012 and 2016, 786 patients surgically treated for ACL reconstruction were selected, 330 females (42%) and 456 male patients (58%). 138 CT scans were available from females and randomly matched with 138 CT scans from males. Mean age at surgery was 32 ± 12 years. Mean time from injury was 19 ± 37 months.
Eligibility criteria included skeletally mature with a complete ACL tear (acute and chronic). Patients were excluded if they had any additional bone, ligament or cartilage injuries, moderate or severe knee arthrosis (IKDC grade C or D) and history of previous surgery.
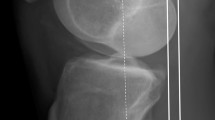
Preoperative laxity was quantified by bilateral, side-to-side stress, and comparative radiographs using the Stress Device® Telos (Metax, Hungen, Germany). The patient was placed in a supine position, knee at 20° flexion, a 150 Newton (15 kg) load was applied to the posterior border of the tibial plateau. The ATT was calculated with the lateral views, measuring the distance from the posterior border of the medial tibial condyle to the femoral condyles using the Dejour and Bonnin method [3], and the side-to-side difference (SSD) between the injured knee and healthy knee was calculated (Fig. 1a, b).
The patient stands on one leg with the knee flexed to 20°. A line was drawn on the radiograph perpendicular to the posterior border of the medial tibial plateau and a second one to the most posterior part of the femoral condyle. The distance between the femoral and tibial lines on the medial side was called the medial anterior tibial translation, MATT. The difference between the healthy and the injured knee is the side to side difference (SSD). a Left knee with ATT of 18.1 mm and b right knee with ATT of 1.5 mm. In this case, SSD was 16.6 mm
CT scans were performed postoperatively as a routine examination (initially for the evaluation of the positioning of femoral and tibial tunnels after ACL reconstruction) in the radiology department of the same institution and analyzed with Institutional Picture Archiving and Communications System (PACS, Centricity, GE Healthcare, Waukesha, Wisconsin) (Fig. 2a–c).
Sagittal geometry evaluation
All measurements used subchondral bone as a reference. The tibial slope evaluation was based on the radiological publication of Dejour et al. [3] and the CT scan evaluation of Kessler et al. [12], using the proximal tibial anatomic axis (PTAA), which has been shown to strongly correlate with the mechanical tibial axis [26, 27] and has been used by the American Knee Society.
Intraoperative data were collected for meniscal lesions and classified by type of tear (partial, complete), side (medial, lateral), location (posterior, mid body, anterior) and tear pattern (longitudinal-vertical, horizontal, radial, vertical flap, horizontal flap, complex).
CT scan measurement reliability
To assess reproducibility of the different measurements, intra-class correlation (ICC) was calculated. An ICC value greater than 0.9 was considered excellent and a value between 0.8 and 0.9 was considered good [8]. Intra-observer variability was assessed by the same surgeon re-measuring a random sample of 50 patients 2 weeks after the initial analysis of all 276 CT scans and TELOS. An independent radiologist measured CT scans and TELOS X-rays from another random sample of 50 patients to determine inter-observer variability.
Intra- and inter-observer reliability of measurements
The reproducibility of the measurements after reconstruction of the tibial bone segments in dedicated image processing software was excellent, with ICCs between 0.91 and 0.97. The reproducibility of the measurements of the SSD in ATT was good to excellent, with ICCs between 0.88 and 0.94. The average ICC for all measurements was 0.93.
The study was approved by the institutional review board of the Hospices Civils de Lyon and the protocol number for this approval was 2016-037.
Statistical analysis
Statistical analysis was performed by the Laboratory of Biostatistics at our institution using R software (version 3.1.1, Copyright © 2014 The R Foundation for Statistical Computing Platform). A value of p < 0.05 was considered statistically significant. The normality of the different variable variances was checked by Kolmogorov–Smirnov tests. Continuous variables were expressed as mean ± standard deviation. Student’s t tests for independent samples were used to compare parametric variables and Mann–Whitney–Wilcoxon tests were used for comparison of non-parametric variables. Pearson’s correlations test was used for linear correlations. To assess reproducibility of the different CT scan measurements, intra-class correlation (ICC) were calculated.
Results
The cohort comprised 276 patients with comparable demographic data shown in Table 1.
The ATT was 9.3 mm in ACL-deficient knees compared to 3.9 mm in ACL-intact knees. The ATT measured using the Telos device (SSD) was 5.6 ± 4.1 mm in the entire cohort. SSD in ATT was similar in females (5.4 ± 3.9) and males (5.8 ± 4.2) (ns). The MTS was 9.8° ± 2.8. MTS was similar in females (9.8 ± 2.8) and males (9.8 ± 2.7) (ns).
Medial meniscal tears were identified in 53 cases (38%) in females and in 68 cases (49%) in males. Lateral tears were found in 22 (16%) females and 34 (29%) males, and tears of both menisci were discovered in 11 (8%) females and 18 (13%) males. There was no significant difference in the incidence of these meniscal tears. Description of meniscal tears are shown in Table 2.
A positive correlation was found between MTS and absolute ATT (r = 0.35, p < 0.001) as well as SSD (r = 0.12, p = 0.03) (Fig. 3a, b). MTS greater than or equal to 11° significantly increases the ATT (p < 0.05). For each degree of increase of the MTS, absolute ATT increases 0.6 mm and SSD increases 0.2 mm in the entire cohort.
A greater MTS was identified as a risk factor for an increase of ATT in females (r = 0.37, p < 0.001) but not in males (n.s) (Fig. 4). In female patients, an increase in the MTS of 1° correlated with an increase in ATT of 0.6 mm (p < 0.001). An increased MTS represents a risk factor for increased ATT in female patients when compared to males.
MTS was influential in ATT regardless of the presence of meniscal lesion (r = 0.28 [0.11, 0.44], p = 0.001) or absence of one (r = 0.48 [0.35, 0.6], p < 0.001).
Discussion
The main findings of this study were that female patients with a greater medial tibial slope had increased anterior tibial translation in comparison to males.
The study describes the medial tibial slope as a reference as it was described by Dejour and Bonnin [3]. Those authors showed that the measurement of medial compartment translation was more informative and susceptible to less variability than the lateral compartment and demonstrated a strong correlation between the anterior tibial translation and the posterior tibial slope in a radiological analysis of 281 patients. Anterior tibial translation increased 6 mm for every 10° of slope (or 0.6 mm for each degree), whereas it increased by 3.5 mm for every 10° of slope which was found using the radiological Lachman test.
CT scan results showed that each degree of increase of the MTS increases the absolute ATT 0.6 mm and the SSD ATT 0.2 mm. This differs from the Dejour and Bonnin study and could be explained first because we excluded partial ruptures of the ACL, thus increasing the laxity [20], and second because of the average time from injury to surgery (19.4 months). Also, CT scan improved the accuracy of the measurements.
Despite studies that confirm the correlation between MTS and increases in ATT [4, 19], there is no consensus regarding a cutoff of the MTS that is related to higher ATT. This study showed that MTS greater than or equal to 11° increases the ATT (p < 0.05). Similar results were obtained by Dejour et al. [4] who described a significant increase of the static ATT in MTS greater than 7° (p = 0.002) and in dynamic ATT greater than 12° (p = 0.041). Galano et al. [5] and Ryan et al. [18] found no significant correlation between medial or lateral slope, and anterior tibial translation in a morphological study. However, that was a cadaveric study with few cases (22 knees).
The present study describes that a greater MTS correlates with increased ATT in females (r = 0.37, p < 0.001) but not in males (n.s).This is supported by Yue et al. [29] who, in the analysis of 150 knees, found an influence of the medial tibial slope on anterior tibial translation only in females. Two other recent studies also found a significant influence of the tibial slope on ACL rupture [9, 24], with no significant findings in males. A large series of 544 patients published by Hohmann [10] identified the medial tibial slope as a risk factor for ACL rupture only in women. Increased MTS is reported as a predisposition for ACL injury in females [30], and also identified as a risk factor for residual laxity and poorer outcome after reconstruction of ACL in a recent meta-analysis [23]. In contrast, Hashemi et al. [7] described greater medial tibial slope as a risk factor for ACL rupture only in males but the sample was 55 patients (33 women and 22 men).
Similar correlation between MTS and medial anterior tibial translation in a cadaveric study was described by Giffin et al. [6] who studied ATT in flexion and extension of the knee, and showed that the maximum anterior tibial translation of 3.6 mm was obtained during complete extension. This greater slope results in an increase in the anterior tibial translation during quadriceps contraction [9, 14], leading to an increased stress on the ACL and a high risk of rupture. The loading of the tibiofemoral joint and quadriceps contraction also produces an anterior shear force, leading to anterior tibial translation.
The results of this study could be due to a quadriceps/hamstring imbalance in females. The ability of the hamstring muscles to compensate for ATT due to ACL deficiency seemed to be affected by the tibial slope especially in females. Liu and Maitland [14] demonstrated in a mathematical model that the ability of the hamstrings to compensate for ATT due to ACL deficiency during walking was adversely affected by the tibial slope. In an ACL-deficient knee with a tibial slope of 4°, only 24% of the maximal hamstring muscle force was required to completely restore the tibia to its normal position. The required muscle force increased to 66% when the tibial slope was 8°. In an ACL-deficient knee with 12° of tibial slope, anterior displacement of the tibia could not be completely compensated by hamstring muscle force.
Females did not have greater posterior tibial slope than males but the difference in ATT could also be explained by a decreased congruency of the medial compartment in female patients [20] or lower ability of the soft tissues (joint capsule especially) to compensate for ACL deficiency.
Additionally, increased tibial slope affects the post-operative stabilization of ACL reconstructions like Li et al. [13] described. Webb et al. even found a risk of repeat rupture of the ACL when the medial tibial slope was greater than 12° [28]. This is because greater tibial slope would increase the stress on the graft and its fixation, resulting in elongation and a risk of early failure [22]. These results can make us think about the selection of the graft. Thus, knowing the influence of the inclination of the tibial plateau allows the development of specific rehabilitation programs preoperatively and postoperatively, dedicated and individualized especially according to the different parameters of the articular geometry.
The study demonstrated no gender-specific difference in the rates of meniscus tears, and that MTS is influential in ATT regardless of the presence or absence of meniscal lesions. This could be explained because of the different force vector during the laximetry similar to what was described by Dejour et al. [4] or by questioning the role of the menisci in limiting ATT, contrary to Trojani et al. [25] demonstrated in their study.
This is the largest series analysing anterior tibial translation on ACL-deficient patients supported by a CT scan analysis. A homogeneous and equal proportion of individuals of both genders makes the statistical analysis stronger. Most previous studies used images acquired via MRI to describe knee joint geometry, but could only subjectively determine for each compartment a sagittal cut passing through the centre of the compartment because 3D reconstruction is generally not available for MRI.
There are several limitations to the current study. First, blinding according to gender was not ensured because first names were visible during measurements. Including chronic ACL injuries can also create a bias due to secondary causes of instability. The decision to explore articular geometry by CT-based method did not allow us to account for the influence of the soft tissues on joint congruence and slope. Both articular cartilage and the menisci may alter joint congruity and slope and differences in these structures may exist between men and women. Lustig et al. [15] reported a reduction of the tibial slope of 1.8° in the medial compartment and 5.5° in the lateral compartment when considering the meniscus. However, this finding was not influenced significantly by the gender.
Measurement of the tibial slope in daily clinical practice is usually performed on strictly contoured knee radiographs. MRI and CT are more interesting alternatives than simple radiographs, and although they are more expensive, they offer the possibility of a combined measurement of the medial tibial slope and other radiologically identifiable factors of articular geometry due to bone superposition.
Finally, a consistent limitation was the evaluation of preoperative laxity. Stress radiographs investigate postero-anterior laxity and are highly dependent on patient cooperation and muscle relaxation, to the same extent as clinical examination manoeuvers. Panisset et al. [17] showed that an evaluation of preoperative laxity combining clinical manoeuvers (Lachman–Trillat test, pivot shift test) and instrumental laximetry was more informative than an isolated clinical or laximetric evaluation. Beldame et al. [1] demonstrated the superiority of the passive Telos system (at 250 Newtons of thrust) compared to Franklin's active radiological system.
Conclusions
Greater medial tibial slope is associated with increased anterior tibial translation in females with ACL-deficient knee when compared to males. Greater medial tibial slope plays a significant role in the anterior translation only in females, whether or not meniscal lesions are present. This could be due to a quadriceps/hamstring imbalance in females and the ability of the hamstring muscles to dampen ATT. An increased MTS in females should be a factor in the preoperative planning and graft selection as it can affect postoperative residual laxity and the risk of re-rupture after ACL reconstruction.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- MTS:
-
Medial tibial slope
- ATT:
-
Anterior tibial translation
- SSD:
-
Side-to-side difference
- IKDC:
-
International Knee Documentation Committee
- PTAA:
-
Proximal tibial anatomic axis
- ICC:
-
Intra-class correlation
References
Beldame J, Bertiaux S, Roussignol X, Lefebvre B, Adam JM, Mouilhade F, Dujardin F (2011) Laxity measurements using stress radiography to assess anterior cruciate ligament tears. Orthop Traumatol Surg Res 97(1):34–43
Boyer P, Djian P, Christel P, Paoletti X, Degeorges R (2005) Reliability of the KT-1000 arthrometer (Medmetric) for measuring anterior knee laxity: comparison with Telos in 147 knees. Rev Chir Orthop Reparatrice Appar Mot 90(8):757–764
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Jt Surg Br 76(5):745–749
Dejour D, Pungitore M, Valluy J, Nover L, Saffarini M, Demey G (2018) Preoperative laxity in ACL-deficient knees increases with posterior tibial slope and medial meniscal tears. Knee Surg Sports Traumatol Arthrosc 27(2):564–572
Galano GJ, Suero EM, Citak M, Wickiewicz T, Pearle AD (2012) Relationship of native tibial plateau anatomy with stability testing in the anterior cruciate ligament-deficient knee. Knee Surg Sports Traumatol Arthrosc 20(11):2220–2224
Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD (2007) Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med 35(9):1443–1449
Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck JR, Schutt RC Jr, Dabezies E, Beynnon BD (2010) Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med 38(1):54–62
Helito CP, Helito PV, Costa HP et al (2014) MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.5-T scans. Skeletal Radiol 43(10):1421–1427
Hohmann E, Bryant A, Reaburn P, Tetsworth K (2010) Does posterior tibial slope influence knee functionality in the anterior cruciate ligament-deficient and anterior cruciate ligament-reconstructed knee? Arthroscopy 26(11):1496–1502
Hohmann E, Bryant A, Reaburn P, Tetsworth K (2011) Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surg Sports Traumatol Arthrosc 19(Suppl 1):S109–114
Jardin C, Chantelot C, Migaud H, Gougeon F, Debroucker M, Duquennoy A (1999) Reliability of the KT-1000 arthrometer in measuring anterior laxity of the knee: comparative analysis with Telos of 48 reconstructions of the anterior cruciate ligament and intra-and interobserver reproducibility. Rev Chir Orthop Reparatrice Appar Mot 85(7):698–707
Kessler M, Burkart A, Martinek V, Beer A, Imhoff A (2003) Development of a 3-dimensional method to determine the tibial slope with multislice-CT. Z Orthop Ihre Grenzgeb 141(2):143–147
Li Y, Hong L, Feng H, Wang Q, Zhang J, Song G, Chen X, Zhuo H (2014) Posterior tibial slope influences static anterior tibial translation in anterior cruciate ligament reconstruction: a minimum 2-year follow-up study. Am J Sports Med 42(4):927–933
Liu W, Maitland ME (2003) Influence of anthropometric and mechanical variations on functional instability in the ACL-deficient knee. Ann Biomed Eng 31(10):1153–1161
Lustig S, Scholes CJ, Leo SP, Coolican M, Parker DA (2013) Influence of soft tissues on the proximal bony tibial slope measured with two-dimensional MRI. Knee Surg Sports Traumatol Arthrosc 21(2):372–379
McNair PJ, Wood GA, Marshall RN (1992) Stiffness of the hamstring muscles and its relationship to function in anterior cruciate ligament deficient individuals. Clin Biomech (Bristol, Avon) 7(3):131–137
Panisset JC, Ntagiopoulos PG, Saggin PR, Dejour D (2012) A comparison of Telos stress radiography versus Rolimeter in the diagnosis of different patterns of anterior cruciate ligament tears. Orthop Traumatol Surg Res 98(7):751–758
Ryan J, Magnussen RA, Cox CL, Hurbanek JG, Flanigan DC, Kaeding CC (2014) ACL reconstruction: do outcomes differ by sex? A systematic review. J Bone Jt Surg Am 96(6):507–512
Sauer S, Clatworthy M (2018) The effect of medial tibial slope on anterior tibial translation and short-term ACL reconstruction outcome. Surg J (N Y) 4(3):e160–e163
Schneider A, Si-Mohamed S, Magnussen RA, Lustig S, Neyret P, Servien E (2018) Tibiofemoral joint congruence is lower in females with ACL injuries than males with ACL injuries. Knee Surg Sports Traumatol Arthrosc 26(5):1375–1383
Snaebjornsson T, Hamrin Senorski E, Sundemo D, Svantesson E, Westin O, Musahl V, Alentorn-Geli E, Samuelsson K (2017) Adolescents and female patients are at increased risk for contralateral anterior cruciate ligament reconstruction: a cohort study from the Swedish National Knee Ligament Register based on 17,682 patients. Knee Surg Sports Traumatol Arthrosc 25(12):3938–3944
Southam BR, Colosimo AJ, Grawe B (2018) Underappreciated factors to consider in revision anterior cruciate ligament reconstruction: a current concepts review. Orthop J Sports Med. 6(1):2325967117751689. https://doi.org/10.1177/2325967117751689
Tan SH, Lau BP, Khin LW, Lingaraj K (2016) The Importance of patient sex in the outcomes of anterior cruciate ligament reconstructions: a systematic review and meta-analysis. Am J Sports Med 44(1):242–254
Todd MS, Lalliss S, Garcia E, DeBerardino TM, Cameron KL (2010) The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med 38(1):63–67
Trojani C, Sbihi A, Djian P et al (2011) Causes for failure of ACL reconstruction and influence of meniscectomies after revision. Knee Surg Sports Traumatol Arthrosc 19(2):196–201
Utzschneider S, Goettinger M, Weber P, Horng A, Glaser C, Jansson V, Muller PE (2011) Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc 19(10):1643–1648
Vacek PM, Slauterbeck JR, Tourville TW et al (2016) Multivariate analysis of the risk factors for first-time noncontact ACL injury in high school and college athletes: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med 44(6):1492–1501
Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP (2013) Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament–reconstructed patient. Am J Sports Med 41(12):2800–2804
Yue DB, Wang BL, Wang WG, Guo WS, Zhang QD (2013) Effects of posterior tibial slope on non-contact anterior cruciate ligament rupture and stability of anterior cruciate ligament rupture knee. Zhonghua yi xue za zhi 93(17):1309–1312
Zelisko JA, Noble HB, Porter M (1982) A comparison of men's and women's professional basketball injuries. Am J Sports Med 10(5):297–299
Zeng C, Yang T, Wu S et al (2016) Is posterior tibial slope associated with noncontact anterior cruciate ligament injury? Knee Surg Sports Traumatol Arthrosc 24(3):830–837
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Contributions
AS participated in the design of the study, acquisition and interpretation of the data. CAC helped to evaluate the inter-observer reliability and helped to translate the manuscript in English. CB helped to translate the manuscript in English. RG has made substantial contribution to the conception of the study. SL has given final approval of the version to be published. ES has given final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
This study was approved by our institutional review board.
Informed consent
Patients gave informed consent that data would be published.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schneider, A., Arias, C., Bankhead, C. et al. Greater medial tibial slope is associated with increased anterior tibial translation in females with an ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc 28, 1901–1908 (2020). https://doi.org/10.1007/s00167-019-05643-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05643-8