Abstract
Purpose
The purpose of this study was to report the long-term outcomes of a continuous series of patients who underwent simultaneous anterior cruciate ligament (ACL) reconstruction and opening wedge high tibial osteotomy (HTO) for varus-related early medial tibio-femoral osteoarthritis. It was hypothesized that this combined surgery sustainably allowed return to sport with efficient clinical and radiological results.
Methods
From 1995 to 2015, all combined ACL reconstruction (bone-patellar tendon-bone graft) and opening wedge HTO for anterior laxity and early medial arthritis were included. Clinical evaluation at final follow-up used Tegner activity score, Lysholm score, subjective and objective IKDC scores. Radiologic evaluation consisted in full-length, standing, hip-to-ankle X-rays, monopodal weight-bearing X-rays and skyline views. AP laxity assessment used Telos™ at 150 N load. Student’s t test was performed for matched parametric data, Wilcoxon for nonparametric variables and Friedman test was used to compare small cohorts, with p < 0.05.
Results
35 Patients (36 knees) were reviewed with a mean follow-up of 10 ± 5.2 years. The mean age at surgery was 39 ± 9. At final follow-up 28 patients (80%) returned to sport (IKDC ≥ B): 11 patients (31%) returned to sport at the same level and 6 (17%) to competitive sports. Mean subjective IKDC and Lysholm scores were 71.8 ± 14.9 and 82 ± 14.1, respectively. The mean decrease of the Tegner activity level from preinjury state to follow-up was 0.8 (p < 0.01). Mean side-to-side difference in anterior tibial translation was 5.1 ± 3.8 mm. Three patients were considered as failures. The mean preoperative mechanical axis was 4.2° ± 2.6° varus and 0.8° ± 2.7° valgus at follow-up. Osteoarthritis progression for medial, lateral, and femoro-patellar compartments was recorded for 12 (33%, p < 0.05), 6 (17%, p < 0.001), and 8 (22%, p < 0.05) knees, respectively. No femoro-tibial osteoarthritis progression was observed in 22 knees (61%).
Conclusions
Combined ACL reconstruction and opening wedge HTO allowed sustainable stabilization of the knee at 10-year follow-up. However, return to sport at the same level was possible just for one-third of patients, with femoro-tibial osteoarthritis progression in 39% of cases.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Valgus producing high tibial osteotomy (HTO) remains an accepted intervention in selected patients with medial femorotibial osteoarthritis and coexisting varus alignment, especially in the young with mild or moderate disease [18]. It has shown to be a durable intervention, capable of more than 80% good results at 5 years and more than 70% good results at 10 years [21] with high propensity for patients to return to work and sport [14]. HTO can be considered a clinically successful procedure that allows the active patient with symptomatic mild osteoarthritis of the knee to return to regular and sustained sporting activities [6, 16, 19, 36].
Reflecting the contribution of instability to rapid degeneration of the knee, early indications for HTO called for intact cruciate ligaments [8]. Surgery combining anterior cruciate ligament (ACL) reconstruction and HTO was first described in 1992 by O’Neill and James [35]. The aim of this intervention was to eliminate symptoms of pain and instability and to delay osteoarthritis in the young patient if possible [25]. Several authors have reported the clinical results of this procedure, although follow-up is typically limited [5, 7, 11, 24, 32, 33, 38, 42]. Few studies report medium or long-term results of combined ACL reconstruction and medial opening wedge (MOW) HTO [38, 42]. In particular, very few studies have described return to sport, which may be of relevance when considering the intended patient demographic [5, 7, 25, 38, 42].
The aim of this study was to evaluate the long-term activity outcome for a series of patients undergoing combined MOW HTO and ACL reconstruction. The hypothesis was that this procedure would allow sustained return to sporting activity. The secondary aims were to describe the subjective, objective, and radiological results as well as the morbidity of combined surgery.
Materials and methods
This retrospective, single centre study, involved a consecutive series of patients undergoing surgery between 1995 and 2015. Proximal tibial valgus producing osteotomy was performed by means of a MOW. Preoperative planning was performed to determine the desired correction with a postoperative target axis between 0° and 3° of valgus. During the same procedure, ACL reconstruction was performed using a bone-patellar tendon-bone (BTB) autograft. A lateral tenodesis was performed in cases of high-grade preoperative knee laxity (grade 3 pivot shift test, side-to-side difference > 10 mm with the radiologic Telos® test).
All patients who had undergone combined ACL reconstruction and MOW HTO during the review period were considered for inclusion. Those with radiological evidence of degenerative changes involving the medial femorotibial compartment, coexisting varus mechanical alignment on long leg weightbearing radiographs, associated chronic anterior laxity, and a minimum of 2-year follow-up were included.
Exclusion criteria included excessive constitutional varus alignment more than 6° [39] without signs of osteoarthritis, severe knee pathology defined by International Knee Documentation Committee (IKDC) radiological stage D, the presence of lateral or posterolateral laxity, or prior ACL reconstruction using an isolated synthetic ligament. Conversely, failure of a prior ACL reconstruction using autograft was not an exclusion criteria.
Patients were evaluated at 1 year postoperatively and last follow-up using the subjective and objective IKDC 2000 score [20].
Sporting activity and return to sport were evaluated by the Lysholm-Tegner score [26, 37] and IKDC subjective score at the time of last follow-up.
Radiological review was performed preoperatively, at 1 year, and at last follow-up. This consisted of anteroposterior and lateral X-rays in monopodal stance, standing Schuss views at 45° of flexion, full-length standing anteroposterior alignment films (Fig. 1), and patellar skyline views [12]. Bilateral, comparative anterior stress views at neutral and 30° flexion were obtained using the Telos® device applying 150 N of force [10].
Tibiofemoral lesions were staged radiologically according to the IKDC classification [20]. Patellofemoral osteoarthritis was described according to the Iwano classification [22]. Posterior tibial slope, using the proximal anatomical tibial axis method [10], strongly correlated to the mechanical tibial axis [41], as well as patellar height, according to Caton and Deschamps [9] and Blackburne-Peel ratios [4], were measured on the weightbearing lateral X-ray. The mechanical tibiofemoral angle was calculated in full-length, standing, hip-to-ankle X-rays. Anterior tibial translation was measured in millimeters on the monopodal stance and comparative stress (Radiologic Lachman) lateral views, as the displacement of the posterior edge of the medial tibial plateau from the posterior edge of the medial femoral condyle, measured perpendicular to a line projected along the posterior tibial diaphysis [12].
Complications were recorded. Patients requiring revision osteotomy or arthroplasty were considered failures, as were patients with ACL graft rupture or revision ACL reconstruction.
Surgical procedure
In all cases, a MOW HTO and BTB autograft ACL reconstruction was performed.
The tibial bone block of the BTB autograft was harvested in a trapezoidal shape so as to obtain a press fit in the femoral tunnel. A standard rectangular patellar bone block was harvested.
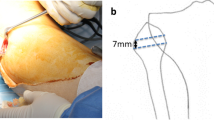
Prior to passage of the graft, the HTO was performed. A cortico-cancellous iliac crest bone graft was used and stable fixation of the osteotomy was then achieved using two or three metal staples (Fig. 2).
Patency of the tibial tunnel was checked. The trapezoidal bone block of the ACL graft harvested from the tibial side was impacted into the femoral condyle to achieve a press fit. Tibial fixation was achieved by a combination of metal wire or non-absorbable suture and cortical screw, then augmented with an interference screw. An extra-articular lateral tenodesis was performed in four cases, using a modified Lemaire type procedure, fixed in the femoral tunnel thanks to the press fit of the ACL graft impacted in the femoral tunnel.
Rehabilitative protocol
Patients were placed in a knee immobilizer immediately postoperatively, and an X-ray was obtained. Low molecular weight heparin was routinely administered for 30 days at prophylactic dose. The patient was advised to start static quadriceps exercises immediately when motor function returned. They were instructed to non-weightbear, with the knee immobilizer in place, for 6 weeks.
Closed chain range of motion exercises were started at the end of 2 weeks, not to exceed 120° of flexion during the first 6 weeks. Full weight bearing was allowed at the end of 6 weeks if repeat X-ray at this time showed callus. Following this appointment, routine clinical review with plain X-ray occurred at 6 weeks and 12 months postoperatively. At 12 months review, Telos stress radiographs were also performed.
Statistical analysis
Statistical analysis was performed using software R. The value adopted for the threshold of significance was set for a p of less than 0.05. Comparison of continuous quantitative variables, after verifying their normal distribution using a Pearson’s test, was performed using a Student’s t test for matched parametric data, and one Wilcoxon test was used for the comparison of nonparametric variables. A Friedman test, adapted to small numbers, was used to compare the functional evolution according to IKDC scores and osteoarthritis.
A study power of 0.9, associated with a median size effect d = 0.6 (acceptable for a comparison of pre and postoperative data for same patients) need a minimal study population of 31 patients.
Results
Fifty-four combined MOW HTO and ACL reconstruction were performed. Fourty-five patients met inclusion criteria, and 35 patients (36 knees) were evaluated at an average follow-up of 9.8 ± 5.2 years. Table 1 describes demographic data. 16 patients (44%) had prior ACL reconstruction, then new injury with iterative ACL rupture.
Table 2 shows the sports level at review. Eleven patients (35%) returned to their previous activity level. Six patients were able to return to competition. Patients with a preinjury Tegner score between 3 and 6 (N = 20) had a reduction to follow-up of 0.4 points (NS). Patients with a preinjury Tegner score above 6 (N = 12) had a significant reduction to follow-up of 2.1 points (p < 0.001), with 4 patients returned at the same level.
The mean subjective IKDC score at follow-up was 71.8 ± 14.9. The mean improvement in the subjective IKDC score between preoperative and follow-up was 30.2 points (p < 0.001). Thirty-one patients (88%) in this series would recommend this intervention to others and were satisfied or very satisfied. The mean Lysholm score at follow-up was 82.1 ± 14.1.
All patients had symptomatic chronic anterior instability preoperatively and abnormal physical examination. On preoperative clinical examination, Lachman test was lax with a soft end point for 33 patients (94%), and Pivot shift was abnormal for 31 patients (89%).
At follow-up Lachman test was normal in 22 cases (63%), lax with a firm end point 11 cases (31%), and a soft end point in 2 cases (6%). The pivot shift was normal in 26 cases (74%), a glide was found in 7 cases (20%), and a clunk in 2 (6%). At follow-up there was a significant average between sides loss of flexion 10° (p < 0.001).
The distribution of the population according to the objective IKDC classification is shown in Table 3. One patient needed a total knee replacement and was rated as D. At follow-up, 61% were rated IKDC grade A or B.
Radiographic results are shown in Tables 3 and 4. Three knees (8%) remained in varus alignment postoperatively. Twelve knees (33%) had progressed from a grade to the internal femoro-tibial interline with significant aggravation (p = 0.02). Lateral compartment osteoarthritis was found in 17% of patients at follow-up (Fig. 3). Two patients had narrowing of greater than 50%, at 13.5 and 16 years post-surgery. No radiographic progression of tibiofemoral arthritis was observed in 61% of the series. Patellofemoral joint narrowing was observed at follow-up in 33% of patients, compared with 11% preoperatively (p < 0.001).
There was no correlation between subjective scores and the radiographic presence of femorotibial or patellofemoral osteoarthritis. Residual laxity, on both Telos stress X-ray and monopodal stance X-ray, was correlated with worsening radiologic changes in the medial compartment (both p < 0.001). This was not found in the lateral or patellofemoral compartments (NS).
Early postoperative complications included one haematoma, two cases of deep vein thrombosis, one case of donor site patellar tendinitis which resolved spontaneously, one case of complex regional pain syndrome. Late complications included two cases of arthrofibrosis requiring arthroscopic arthrolysis in both instances and resection of a cyclops lesion in one. Thirteen patients (37%) underwent removal of prominent fixation hardware.
Three cases (8%) were considered as failures. There was one revision osteotomy, performed for non-union in a smoker patient, which was managed with bone grafting and the use of a locking plate. There was one confirmed ACL graft rupture, which occurred at 8 months following surgery. There was one 60 years old patient requiring revision to a total knee arthroplasty.
Discussion
The most important finding of this study was the good clinical results at 10 years of combined anterior cruciate ligament reconstruction and medial opening wedge high tibial osteotomy, with low morbidity, good control of anterior laxity, and no rapid progression of osteoarthritis. This procedure can produce durable return to sporting activity (about 80%), although typically not to a high level with return at the same level possible just for one-third of patients.
The improvement in activity following surgery found in this study is consistent with other literature on this topic. Dejour et al. [11] reported a return to leisure activities for the majority of patients (about 60%), but return to competitive sport was considered unrealistic. Similarly, Neuschwander et al. [29] found a significant improvement in clinical and functional scores, whilst generally being unable to return to high level activity. Akamatsu et al. [1], however, had greater success in patients with particularly high athletic expectations, albeit in a very small number of cases. At long-term follow-up, Boss et al. [7] reported that 52% of patients had a higher sport activity than preoperatively, but not back to their pre- injury performance level.
In this study, most of the patients had significantly declined by follow-up at an average of almost 10 years. This was particularly relevant as the preinjury level of activity was high. At final follow-up, 11 (31%) had returned to sport at their preinjury level, and 6 (17%) had returned to competitive sport. Ten patients (29%) were able to undertake IKDC very strenuous or strenuous sports activity.
Concerning the activity level after isolated HTO, recent systematic reviews and meta-analysis [14, 19] showed that 87–94% of patients could return to sport, and 85% returned to their pre-symptomatic sports level after knee osteotomies. Bonnin et al. [6] in a multicenter retrospective study showed that young motivated patients were able to resume strenuous activities following HTO but had to be informed that they would typically not recover their pre-pathology level and that residual pain during strenuous sports was not exceptional.
According to Oiestad et al. [34], participants who returned to very strenuous activities (pivoting sport) after ACL reconstruction were younger and had better self-reported knee function in the early phase post- ACL reconstruction. At 15-year follow-up, only 52% of 210 patients with a mean age of 39.1 ± 8.7 years had returned to pivoting sport.
This present study considered 36% of ACL reconstruction revisions among which 8% rate of iterative revisions. After ACL reconstruction revisions, Webster et al. [40] noted a 68% rate of patients who returned to their preinjury level of sport, compared with 83% after primary reconstruction in the same patients.
There is limited literature examining long-term outcome for combined ACL reconstruction and HTO. Bonin et al. [5] reported a return to strenuous or very strenuous physical activity in 47% of patients at an average follow-up of 12 years, compared with 29% of patients in this study. However, the group assessed by Bonin et al. had an average age approximately 10 years younger than this group, which could account for much of this difference. Trojani et al. [38] reported good results at an average of 6-year follow-up, with an overall return to sport in nearly 80% of cases, and strenuous or very strenuous activity in nearly 50%. They found, however, a return to the same level of competition for nearly half of their patients, which is superior to this study. Their study population also had an average age of about 10 years less, and a shorter follow-up period.
Zaffagnini et al. [42] showed 62% of patients with recurrence with a Tegner activity level greater than or equal to 5 and 18% of patients returning to their pre-traumatic sports level at an average of 6.5-year follow-up. In the present study was describe a return to preinjury sporting level in one-third of cases. The surgical technique in Zaffagnini’s study was different, with lateral closing wedge osteotomy combined with an “over the top” ACL reconstruction technique and routine lateral tenodesis, with a shorter follow-up, making direct comparison difficult.
Radiologically, the evaluation of the anterior–posterior laxity showed a significant reduction in anterior tibial translation at follow-up, in side-to-side comparison stress X-ray. However, the 5.1 mm differential found in this series was slightly higher than that found in the literature [33, 38, 42]. This is possibly explained by a larger number of medial meniscectomies [30, 31], and numerous previous surgical procedures. In this study, there was a significant correlation between residual laxity and progression of osteoarthritic lesions. Residual instability due to cartilage damage caused by shear forces and decreased meniscal capital are major factors responsible for osteoarthritis in this setting [11].
Posterior tibial slope was not significantly increased post-operatively. This result is in agreement with a recent French multicentre comparative study [13], which found an average increase of 0.6° for MOW osteotomy (average of 0.6° in our study), compared with a decrease it by 0.7° for a lateral closing wedge osteotomy. The absence of an increase in the tibial slope contributes to better control of the laxity and a reduced risk of rupture of the ACL graft [2, 27, 28]. However, a recent study by Arun et al. [3] showed that the increase in tibial slope after this combined surgery was a favourable factor in terms of subjective outcomes at 6 years of mean follow-up. No such correlation was demonstrated in this series.
Indices of patellar height were on average significantly reduced post-surgery, consistent with other literature findings [15]. Flexion was significantly reduced compared to the other side, by about ten degrees. This was also commented on by the majority of patients, with difficulty kneeling or bringing the heel to the buttocks.
One of the secondary objectives was to evaluate long-term osteoarthritic progression following this technique. Radiographic worsening of medial compartment osteoarthritis was found in less than one-third of patients (33%). This result remains more important than other series reported [5, 11, 38, 42]. Bonin et al. [5] found 17% of patients worsened by one grade according to the IKDC classification, however, their population was younger and they used a lateral closing wedge technique in 25 out of 30 cases. Additionally, the angular correction in this study was less than that compared to the other series [5, 33, 38, 42], and the latter worsened at the setback. Joint space narrowing of greater than 50% was found in 22% of patients, but only two cases of complete loss.
There were significant radiographic modifications of lateral compartment. However, there was only one case of narrowing of greater than 50%, which occurred in the largest angular correction in this series, with a mechanical femoro-tibial angle of 188° at review and a partial lateral meniscectomy had been imposed during the procedure. Hernigou et al. [17] reported significant deterioration of the lateral compartment with over correction with more than 6° valgus. Amis et al. [2] showed that in case of overcorrection with excessive residual valgus, there is an excessive contact pressure at the lateral part of the knee due to the articular geometry with a less congruent lateral compartment.
Osteoarthritic progression of the patellofemoral joint was also significant, notably with loss of joint space laterally, probably related to the patellar lowering. However, no correlation can be established between lowering of the patella and patellofemoral wear, possibly as the study was not sufficiently powered to detect it.
A recent meta-analysis published by Li et al. [25] referred to the possibility that this combined surgery would be comparable to an isolated reconstruction of the anterior cruciate ligament. Although there has been concern that combined HTO and ACL reconstruction could result in increased morbidity, no serious complications were reported likely due to the combined procedure [1, 23, 32,33,34]. Noyes et al. [32, 33] suggested that in athletic patients with chronic instability, early medial arthritis and varus deformity, ACL reconstruction plus tibial osteotomy at the same time should be favoured over osteotomy alone. In the present study, arthroscopic arthrolysis was rarely necessary, being required in two cases. This contrasts with the experience of Akamatsu et al. [1], who reported stiffness with either graft impingement or the presence of a cyclops lesion in all four cases in their series.
In this series, three patients as failures were recorded. At the time of final follow-up, one patient required revision to a total knee replacement, 13.5 years following surgery at the age of 60. The results of this study are in keeping with other literature describing low rates of revision osteotomy, ACL reconstruction, or to arthroplasty, albeit in cohorts with younger patients and shorter follow-up [5, 25, 33, 38, 42]. Almost 9 out of 10 patients would repeat this procedure or recommend it to a relative, reflecting the high level of satisfaction achieved [25, 33, 38].
This study had several limitations. It was a retrospective study without a control group. The heterogeneity of the study population in terms of initial arthritic degeneration, meniscal status and surgical history make generalization of results difficult. The size of the sample did not permit identification of many long-term prognostic factors. Reflecting the duration of time post-surgery, there was a significant loss to follow-up. There was probably a referral centre effect, with more than one in three patients being referred following multiple failed reconstructions, thus likely skewing functional and radiological scores.
Conclusion
Combined anterior cruciate ligament reconstruction and medial opening wedge high tibial osteotomy can produce durable return to sporting activity, although typically not to a high level. This procedure allows patients with early onset medial compartment knee osteoarthritis and chronic anterior cruciate instability to regain a stable knee at almost 10-year follow-up, with a return to sporting activities in about 80%. A significant decrease in sporting level is to be expected, and patient counselling is important as the preinjury activity level in the target patient demographic is high. Additionally, this study has found associated low morbidity, good control of anterior laxity, and no rapid progression of osteoarthritis.
Abbreviations
- HTO:
-
High tibial osteotomy
- ACL:
-
Anterior cruciate ligament
- MOW:
-
Medial opening wedge
- BTB:
-
Bone-patellar tendon-bone
- IKDC:
-
International Knee Documentation Committee
References
Akamatsu Y, Mitsugi N, Taki N, Takeuchi R, Saito T (2010) Simultaneous anterior cruciate ligament reconstruction and opening wedge high tibial osteotomy: report of four cases. Knee 17:114–118
Amis AA (2013) Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21:197–205
Arun GR, Kumaraswamy V, Rajan D, Vinodh K, Singh AK, Kumar P, Chandrasekaran K, Santosh S, Kishore C (2016) Long-term follow up of single-stage anterior cruciate ligament reconstruction and high tibial osteotomy and its relation with posterior tibial slope. Arch Orthop Trauma Surg 136:505–511
Berg EE, Mason SL, Lucas MJ (1996) Patellar height ratios. A comparison of four measurement methods. Am J Sports Med 24:218–221
Bonin N, Ait Si Selmi T, Donell ST, Dejour H, Neyret P (2004) Anterior cruciate reconstruction combined with valgus upper tibial osteotomy: 12 years follow-up. Knee 11:431–437
Bonnin MP, Laurent J-R, Zadegan F, Badet R, Pooler Archbold HA, Servien E (2013) Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc 21:64–73
Boss A, Stutz G, Oursin C, Gächter A (1995) Anterior cruciate ligament reconstruction combined with valgus tibial osteotomy (combined procedure). Knee Surg Sports Traumatol Arthrosc 3:187–191
Cantin O, Magnussen RA, Corbi F, Servien E, Neyret P, Lustig S (2015) The role of high tibial osteotomy in the treatment of knee laxity: a comprehensive review. Knee Surg Sports Traumatol Arthrosc 23:3026–3037
Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H (1982) Patella infera. Apropos of 128 cases. Rev Chir Orthopédique Réparatrice Appar Mot 68:317–325
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br 76:745–749
Dejour H, Neyret P, Boileau P, Donell ST (1994) Anterior cruciate reconstruction combined with valgus tibial osteotomy. Clin Orthop 299:220–228
Dejour H, Walch G, Chambat P, Ranger P (1988) Active subluxation in extension: a new concept of study of the ACL deficient knee. Am J Knee Surg 1:204–211
Ducat A, Sariali E, Lebel B, Mertl P, Hernigou P, Flecher X, Zayni R, Bonnin M, Jalil R, Amzallag J, Rosset P, Servien E, Gaudot F, Judet T, Catonné Y (2012) Posterior tibial slope changes after opening- and closing-wedge high tibial osteotomy: a comparative prospective multicenter study. Orthop Traumatol Surg Res 98:68–74
Ekhtiari S, Haldane CE, de Sa D, Simunovic N, Musahl V, Ayeni OR (2016) Return to work and sport following high tibial osteotomy: a systematic review. J Bone Joint Surg Am 98:1568–1577
El-Azab H, Glabgly P, Paul J, Imhoff AB, Hinterwimmer S (2010) Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med 38:323–329
Goutallier D, Hernigou P, Medevielle D, Debeyre J (1986) Outcome at more than 10 years of 93 tibial osteotomies for internal arthritis in genu varum (or the predominant influence of the frontal angular correction). Rev Chir Orthop Repar Appar Mot 72:101–113
Hernigou P (1996) A 20-year follow-up study of internal gonarthrosis after tibial valgus osteotomy. Single versus repeated osteotomy. Rev Chir Orthop Repar Appar Mot 82:241–250
Holden DL, James SL, Larson RL, Slocum DB (1988) Proximal tibial osteotomy in patients who are fifty years old or less. A long-term follow-up study. J Bone Joint Surg Am 70:977–982
Hoorntje A, Witjes S, Kuijer PPFM, Koenraadt KLM, van Geenen RCI, Daams JG, Getgood A, Kerkhoffs GMMJ (2017) High rates of return to sports activities and work after osteotomies around the knee: a systematic review and meta-analysis. Sports Med 47:2219–2244
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC, Shelbourne KD, International Knee Documentation Committee (2006) Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med 34:1567–1573
Ivarsson I, Myrnerts R, Gillquist J (1990) High tibial osteotomy for medial osteoarthritis of the knee. A 5 to 7 and 11 year follow-up. J Bone Joint Surg Br 72:238–244
Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y (1990) Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop 252:190–197
Lattermann C, Jakob RP (1996) High tibial osteotomy alone or combined with ligament reconstruction in anterior cruciate ligament-deficient knees. Knee Surg Sports Traumatol Arthrosc 4:32–38
Lerat JL, Moyen B, Garin C, Mandrino A, Besse JL, Brunet-Guedj E (1993) Anterior laxity and internal arthritis of the knee. Results of the reconstruction of the anterior cruciate ligament associated with tibial osteotomy. Rev Chir Orthop Reparat Appar Mot 79:365–374
Li Y, Zhang H, Zhang J, Li X, Song G, Feng H (2015) Clinical outcome of simultaneous high tibial osteotomy and anterior cruciate ligament reconstruction for medial compartment osteoarthritis in young patients with anterior cruciate ligament-deficient knees: a systematic review. Arthroscopy 31:507–519
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154
Martineau PA, Fening SD, Miniaci A (2010) Anterior opening wedge high tibial osteotomy: the effect of increasing posterior tibial slope on ligament strain. Can J Surg 53:261–267
McLean SG, Oh YK, Palmer ML, Lucey SM, Lucarelli DG, Ashton-Miller JA, Wojtys EM (2011) The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am 93:1310–1317
Neuschwander DC, Drez D, Paine RM (1993) Simultaneous high tibial osteotomy and ACL reconstruction for combined genu varum and symptomatic ACL tear. Orthopedics 16:679–684
Neyret P, Donell ST, Dejour H (1993) Results of partial meniscectomy related to the state of the anterior cruciate ligament. Review at 20 to 35 years. J Bone Joint Surg Br 75:36–40
Neyret P, Walch G, Dejour H (1988) Intramural internal meniscectomy using the Trillat technic. Long-term results of 258 operations. Rev Chir Orthop Repar Appar Mot 74:637–646
Noyes FR, Barber SD, Simon R (1993) High tibial osteotomy and ligament reconstruction in varus angulated, anterior cruciate ligament-deficient knees. A two- to seven-year follow-up study. Am J Sports Med 21:2–12
Noyes FR, Barber-Westin SD, Hewett TE (2000) High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 28:282–296
Øiestad BE, Holm I, Risberg MA (2018) Return to pivoting sport after ACL reconstruction: association with osteoarthritis and knee function at the 15-year follow-up. Br J Sports Med 52:1199–1204
O’Neill DF, James SL (1992) Valgus osteotomy with anterior cruciate ligament laxity. Clin Orthop 278:153–159
Salzmann GM, Ahrens P, Naal FD, El-Azab H, Spang JT, Imhoff AB, Lorenz S (2009) Sporting activity after high tibial osteotomy for the treatment of medial compartment knee osteoarthritis. Am J Sports Med 37:312–318
Tegner Y, Lysholm J, Lysholm M, Gillquist J (1986) A performance test to monitor rehabilitation and evaluate anterior cruciate ligament injuries. Am J Sports Med 14:156–159
Trojani C, Elhor H, Carles M, Boileau P (2014) Anterior cruciate ligament reconstruction combined with valgus high tibial osteotomy allows return to sports. Orthop Traumatol Surg Res 100:209–212
Vandekerckhove P-JTK, Matlovich N, Teeter MG, MacDonald SJ, Howard JL, Lanting BA (2017) The relationship between constitutional alignment and varus osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 25:2873–2879
Webster KE, Feller JA, Kimp AJ, Whitehead TS (2018) Revision anterior cruciate ligament reconstruction outcomes in younger patients: medial meniscal pathology and high rates of return to sport are associated with third ACL injuries. Am J Sports Med 46:1137–1142
Yoo JH, Chang CB, Shin KS, Seong SC, Kim TK (2008) Anatomical references to assess the posterior tibial slope in total knee arthroplasty: a comparison of 5 anatomical axes. J Arthroplasty 23:586–592
Zaffagnini S, Bonanzinga T, Grassi A, Marcheggiani Muccioli GM, Musiani C, Raggi F, Iacono F, Vaccari V, Marcacci M (2013) Combined ACL reconstruction and closing-wedge HTO for varus angulated ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc 21:934–941
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
AS participated in the design of the study, acquisition and interpretation of the data. RG, SG and CB helped to translate the manuscript in English and revising it critically for important intellectual content. PN have given final approval of the version to be published. SL have given final approval of the version to be published. ES have made substantial revisions to the study and have given final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schneider, A., Gaillard, R., Gunst, S. et al. Combined ACL reconstruction and opening wedge high tibial osteotomy at 10-year follow-up: excellent laxity control but uncertain return to high level sport. Knee Surg Sports Traumatol Arthrosc 28, 960–968 (2020). https://doi.org/10.1007/s00167-019-05592-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05592-2