Abstract
Purpose
The role of neutral alignment in total knee arthroplasty (TKA) on short- and long-term outcomes has become controversial. Based on the concept of constitutional varus, it has been suggested that under-correction in TKA in a varus osteoarthritis (OA) population might lead to better clinical outcomes. However, it is still unknown what the relationship between constitutional varus and the development of end-stage OA is. The goal of this study was to analyse the contribution of constitutional varus in a medial OA population and to define a correlation between the constitutional alignment and end-stage varus OA.
Methods
Based on full-length radiographs, corrected for the intra-articular deformity of the knee, of 315 patients with unilateral end-stage medial OA of the knee (Charnley type A), a correlation in the coronal plane was made between medial end-stage OA and the contralateral non-arthritic side.
Results
With increasing varus alignment in the arthritic limb, the physiologic limb alignment also became more varus. The proportion of constitutional varus rose with increasing overall alignment and was found to be continuous for males. Constitutional varus was three times higher in men when the overall arthritic alignment was greater more than 6° varus.
Conclusion
Constitutional varus significantly contributes to varus osteoarthritis and was found to be higher than in the general population.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restoration of the mechanical axis to neutral in the frontal plane has been considered the standard of care in total knee arthroplasty (TKA), with evidence showing it to be a prerequisite for successful long-term outcomes [3, 20, 35]. Biomechanical, retrieval, cadaver, and finite element studies have all supported neutral alignment after TKA, demonstrating lower stress, loading, and polyethylene wear compared to varus alignment [1, 12, 13, 15, 17, 21, 24, 29, 33].
However, the role of neutral alignment on short- and long-term outcomes has become controversial, as the literature shows no difference in revision rates between a neutrally aligned (within ±3°) TKA and “outlier” varus- and valgus-aligned TKAs [4, 16, 23, 25, 30]. This has been further supported by data of Miller et al. who compared static and dynamic loading of the knee in TKA patients. They reported that dynamic equal mediolateral joint loading is not correlated with a neutrally mechanically aligned knee, indicating that frontal plane alignment is only one of the contributing factors to joint loading [26]. Furthermore, a recent study by Vanlommel et al. [36] showed superior clinical outcome scores in under-corrected TKAs (3°–6° varus) in a varus osteoarthritic (OA) population. It has been questioned whether these results might be related to the fact that part of this medial OA population has so-called constitutional varus.
Constitutional varus, a physiologic mechanical axis of 3° varus or more, was recently described by Bellemans et al. [2]. While previous alignment reports provided data that the overall mechanical axis in the general population is 1°–1.3° varus [6, 10, 27], Bellemans found that in a general healthy population, 32 % of males and 17 % of females had constitutional varus. It has been suggested that varus alignment is one of the main determinants in developing medial OA [19, 34]. If this population presented with end-stage medial OA, correcting the alignment to neutral when performing a TKA would result in a significant anatomy alteration and potentially decreased patient satisfaction due to these changes in biomechanics in different planes [22]. Unfortunately, some of the data suggesting varus alignment is a risk factor for OA examine incidence in end-stage cases without considering constitutional alignment [19].
It is unknown whether there is a higher incidence of constitutional varus in medial OA patients, and it remains unknown what the relationship between physiologic alignment and end-stage varus OA is [38]. This information might be of importance regarding the placement of physiologic TKAs. The goal of this study is to analyse the contribution of constitutional varus in a medial OA population and to define a correlation between the constitutional alignment and end-stage varus OA. This study hypothesised that there would be a greater incidence of constitutional varus in patients with greater varus alignment in their arthritic limb.
Materials and methods
Ethics approval was obtained from the institutional research ethics board (The University of Western Ontario Research Ethics Board for Health Sciences Research Involving Human Subjects, File No. 104928). A clinical database of all arthroplasty patients operated on at our institution was queried for unilateral end-stage OA patients, (Charnley type-A patients), who had a TKA preformed between 2005 and 2014. A total of 1558 patients were identified, and two observers checked for inclusion and exclusion criteria.
The inclusion criteria for the study were patients with unilateral medial end-stage OA (Kellgren–Lawrence grade 4) and a contralateral knee with less than 50 % cartilage loss (Kellgren–Lawrence grade 0–2). The side with end-stage OA was termed the “arthritic limb”, and the contralateral limb was termed the “physiologic limb”. Also required was the presence of full-leg standing radiographs, with antero-posterior, lateral, skyline, and tunnel views of both knees prior to TKA. Exclusion criteria were inflammatory or posttraumatic OA, unicompartmental lateral or patellofemoral end-stage OA, extra-articular deformities of the lower leg, prior surgery of the hip, femur, tibia or ankle changing the mechanical axis, or poor-quality full-leg standing radiographs. After inclusion and exclusion criteria were met, a total of 315 patients were available for further analysis.
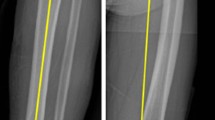
Full-leg standing digital radiographs were available for all included patients and obtained prior to primary TKA as described by Paley et al. [28]. Both limbs (arthritic and physiologic sides) were measured by two independent examiners for coronal plane mechanical alignment as previously described by Cooke et al. [11], as represented in Fig. 1. Measurements up to 0.01° were taken.
The overall mechanical axis was defined as the hip–knee–ankle (HKA) angle, which was the angle between the femoral and tibial mechanical axes. This was expressed as a deviation from 180°, with a negative value correlating with varus and a positive value with valgus. The femoral mechanical axis was defined as a line from the centre of the femoral head (measured with the use of digital concentric templates) to the centre of the femoral notch. The tibial mechanical axis was defined as a line from the midline between the tibial spines and the mid-point of the talus. The plateau-ankle (PA) angle was defined as the angle between the tibial margin and the tibial mechanical axis. The condylar-hip (CH) angle was defined as the angle of the femoral condylar tangent with respect to the femoral mechanical axis. For both the CH and PA angles, a negative value correlated with varus alignment and a positive value correlated with valgus alignment. The condylar-plateau (CP) angle represents the intra-articular deformity and was defined as the angle between the femoral and tibial joint surfaces. This CP angle represents the soft tissue laxity and has been shown to influence the alignment in a weight-bearing position [31]. Narrowing medially has a negative value (thus contributing to varus alignment), while lateral narrowing correlated with a positive value (thus contributing to valgus alignment). To differentiate between the physiologic and the arthritic limbs, all values addressing the arthritic side were given a subscript “oa” (e.g. HKAoa) and values addressing the physiologic side a subscript “phys” (e.g. HKAphys).
Since the physiologic side included Kellgren–Lawrence grades 0, 1, and 2 OA, the mean CPphys angle of grades 1 and 2 was corrected for the difference to CPphys of grade 0 for each individual. This was performed to better represent the true constitutional alignment of the patient, by eliminating any difference due to OA-induced intra-articular deformity. The correction in CPphys was therefore also applied to adjust the HKAphys, which was alternatively defined as the constitutional mechanical alignment. Similarly on the arthritic side, CP varies greatly due to articular deformity. Several possibilities for correction were examined, including using the measured CPoa, substituting CPphys, and correcting CP to 0°, with HKAoa adjusted accordingly in all cases. The strongest correlation between HKAphys and HKAoa was found with CP corrected to zero (r 2 = 0.33, p < 0.0001); therefore, this method was used for the HKAoa measurements.
Statistical analysis
The distribution of physiologic alignment (HKAphys) for every 3° of HKAoa was determined and analysed for the general OA population and separately for males and females. The contribution of constitutional varus in medial OA patients was also determined and specified for gender. A Bland–Altman analysis was performed to determine the limits of agreements (95 % confidence interval) between examiners. The D’Agostino and Pearson omnibus normality test was used to evaluate whether data were normally distributed. Unpaired t-tests were used to compare CH and PA between groups. Linear regression was used to examine trends in distribution.
Results
Of the 315 patients, 49 % of the population were female and 51 % were male. The physiologic knee was graded as a grade 0 OA in 19 patients, grade 1 OA in 105 patients, and grade 2 OA in 189 patients. The mean age (±SD) was 61.6 ± 9.9 years in the grade 0 group, 66.5 ± 9.0 years in the grade 1 group, and 67.7 ± 9.0 years in the grade 2 group. The mean CPphys before correction was −0.43° ± 1.10° for grade 0, −0.96° ± 1.10° for grade 1, and −1.96° ± 1.20° for grade 2. There was no difference in PA angle (n.s.) or CH angle (n.s.) between grades 0 and 1 and the grade 2 OA group (Table 1).
The limits of agreement (95 % CI) between the two examiners for the overall mechanical alignment—HKA—measurements were −0.19° to 0.24°. Almost all patients with an HKAoa—of 0 ± 3° had an HKAphys also within 0 ± 3° (Fig. 2), including 91 % of patients up to 3° valgus and 88 % of patients up to 3° varus. With increasing varus alignment in the arthritic limb, the physiologic limb alignment also became more varus. The HKAphys was within 3° ± 3° varus for 81 % of patients with HKAoa alignment of 3°–6° varus, for 77 % of patients with HKAoa alignment of 6°–9° varus, and for 80 % of patients with HKAoa alignment of 9°–12° varus. The HKAphys was within 6° ± 3° varus for all patients with HKAoa alignment of 12°–15° varus. None of the patients had a constitutional varus of more than 9°, with 8.47° being the highest value.
Overall, 46 % of male patients and 23 % of female patients with HKAoa > 0° varus had constitutional varus (HKAphys ≥ 3° varus). The proportion with constitutional varus rose with increasing HKAoa (Fig. 3). The rise was continuous for males, eventually reaching 100 % for patients with HKAoa alignment of 12°–15° varus (r 2 = 0.99, p = 0.0005). For females, the proportion with constitutional varus rose and then fell (n.s.). In every group, more men than women had constitutional varus. However, there were three times greater males (n = 64) than females (n = 23) with an HKAoa alignment of >6° varus. This pattern of the proportion of patients with constitutional varus was again found within specific ranges of HKAoa (Fig. 4), with a continuous rise for males (r 2 = 0.97, p = 0.002) and a rise then fall for females (n.s.).
Discussion
The present study is the first to describe a correlation between primary varus OA and physiologic alignment. The most important finding of our study is that the contribution of constitutional varus in a medial OA population is higher than in the general population and that it increases with progressively more varus arthritic knees. This trend was stronger for male patients than for females, potentially due to relatively lower numbers of females with more varus-aligned arthritic knees in the study. Considering the overall population, patients with constitutional varus may be more at risk to develop end-stage OA and may therefore be a “high target” for future realignment procedures or arthroplasty.
The results of this study further open the debate on frontal plane alignment in TKA. While numerous studies [3, 14, 32] on survivorship describe excellent outcomes when the frontal plane axis was corrected to neutral alignment (0° ± 3°), recent reports have challenged this long-standing “gold standard” [4, 16, 23, 25, 30]. Motivation for these challenges stems from the finding that patient satisfaction after TKA is lower than after total hip arthroplasty [5]. Recently, Vanlommel et al. demonstrated that superior clinical outcomes were achieved if the TKA was left “under-corrected” (i.e. in 3°–6° of varus) in a varus OA population. In the present study, a large portion of patients with an alignment of >0° varus in their arthritic limb had constitutional varus. However, only a minority of these patients had a physiologic alignment >6° varus.
This distribution could provide an opportunity for defining a more physiologic target for TKA placement in patients with end-stage OA and varus frontal plane alignment. Most patients with an arthritic limb alignment of 0° ± 3° also had neutral (0° ± 3°) physiologic limb alignment. For patients with >3°–12° varus arthritic limb alignment, the constitutional alignment was 3° ± 3° varus in approximately 80 % of the population, and those with an arthritic limb alignment of >12° varus all had constitutional varus of 6° ± 3°. Taking into account the possible error in placement of TKA, a target of 0° for an HKAoa of 0° ± 3° and a target of 3° varus for an HKAoa of >3° varus might reconstruct the physiologic alignment as close as possible. In some cases, computer-assisted surgery might be necessary to achieve these goals [7, 8]. These targets of correction will require further analysis in future descriptive clinical outcome studies in varus OA patients undergoing TKA, especially regarding whether this “under-correction” undermines survivorship. Given the high incidence of constitutional varus patients found in this study, and the difference between males and females, studies describing outcomes after TKA would be prudent to specify varus, neutral, or valgus OA and subdivide outcomes for women and men.
This study has its limitations. The use of full-leg radiographs has been showed to possibly have rotational errors and therefore might reduce the accuracy of measurements [9, 11, 37]. The error of measurements was reduced in our study by using two independent observers, and the inter-observer variability was shown to be low. Secondly, the contralateral non-arthritic side was used as the control population, without evidence that the contralateral side has the same physiologic alignment as the OA side. Ideally, patients would be followed longitudinally with full-leg radiographs in order to understand the natural course of physiologic alignment. However, this is obviously difficult to accomplish. Similarly, most of the patients presenting with primary OA have bilateral arthritic changes, and with low numbers of patients with grade 0 OA in the physiologic limb, patients with grade 1 OA (possible narrowing of the joint space) and grade 2 OA (with less than 50 % cartilage loss) of their physiologic limbs were also included. There was no difference in CH and PA angle between grades 0 and 1 versus grade 2, which suggests the difference in alignment between grades 0 and 2 is minor. A correction for CP was performed in the physiologic limb for grades 1 and 2 to equal the mean CP in the grade 0 group and corrected CP in the arthritic limb to 0°, with corresponding adjustments to HKA in both the physiologic and arthritic groups. This served to minimise the effects of intra-articular deformity and medial bony wear at the tibial and femoral side on HKA, which have a wide variability. Finally, compared to the general population having constitutional varus as described by Bellemans et al., the present study population was significantly older with a mean age of 66.9 years. However, knee joint orientation has previously been described in elderly up to 60 years [6, 18].
Correlation of unilateral arthritic knees to the unaffected, physiologically aligned knee using full-leg radiographs indicates that it may be possible to understand the patient’s physiologic, pre-arthritic coronal plane alignment. This research may provide important information regarding the placement of physiologic TKAs and direct future research questions.
Conclusion
Constitutional varus significantly contributes to varus osteoarthritis.
References
Bargren JH, Blaha JD, Freeman MA (1983) Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Clin Orthop Relat Res 173:178–183
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat Award: Is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) The Chetranjan Ranawat Award: tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Bonner TJ, Eardley WGP, Patterson P, Gregg PJ (2011) The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg Br 93:1217–1222
Bourne RB, Chesworth B, Davis A, Mahomed N (2010) Comparing patient outcomes after THA and TKA is there a difference? Clin Orthop Relat Res 468:542–546
Chao EY, Neluheni EV, Hsu RW, Paley D (1994) Biomechanics of malalignment. Orthop Clin North Am 25:379–386
Cheng T, Zhao S, Peng X, Zhang X (2012) Does computer-assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized controlled trials? Knee Surg Sports Traumatol Arthrosc 20:1307–1322
Cip J, Widemschek M, Luegmair M, Sheinkop MB, Benesch T, Martin A (2014) Conventional versus computer-assisted technique for total knee arthroplasty: a minimum of 5-year follow-up of 200 patients in a prospective randomized comparative trial. J Arthroplasty 29:1795–1802
Colebatch AN, Hart DJ, Zhai G, Williams FM, Spector TD, Arden NK (2009) Effective measurement of knee alignment using AP knee radiographs. Knee 16:42–45
Cooke TD, Li J, Scudamore RA (1994) Radiographic assessment of bony contributions to knee deformity. Orthop Clin North Am 25:387–393
Cooke TDV, Sled EA, Scudamore RA (2007) Frontal plane knee alignment: a call for standardized measurement. J Rheumatol 34:1796–1801
D’Lima DD, Chen PC, Colwell CW (2001) Polyethylene contact stresses, articular congruity, and knee alignment. Clin Orthop Relat Res 392:232–238
D’Lima DD, Hermida JC, Chen PC, Colwell CW (2001) Polyethylene wear and variations in knee kinematics. Clin Orthop Relat Res 392:124–130
Fang DM, Ritter MA, Davis KE (2009) Coronal alignment in total knee arthroplasty: Just how important is it? J Arthroplasty 24:39–43
Green GV, Berend KR, Berend ME, Glisson RR, Vail TP (2002) The effects of varus tibial alignment on proximal tibial surface strain in total knee arthroplasty: the posteromedial hot spot. J Arthroplasty 17:1033–1039
Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML (2015) Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop 39:2117–2124
Hsu HP, Garg A, Walker PS, Spector M, Ewald FC (1989) Effect of knee component alignment on tibial load distribution with clinical correlation. Clin Orthop Relat Res 248:135–144
Hsu RW, Himeno S, Coventry MB, Chao EY (1990) Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res 255:215–227
Hunter DJ, Zhang Y, Niu J, Tu X, Amin S, Goggins J, Lavalley M, Guermazi A, Gale D, Felson DT (2005) Structural factors associated with malalignment in knee osteoarthritis: the Boston osteoarthritis knee study. J Rheumatol 32:2192–2199
Lewallen DG, Bryan RS, Peterson LF (1984) Polycentric total knee arthroplasty. A ten-year follow-up study. J Bone Joint Surg Am 66:1211–1218
Liau JJ, Cheng CK, Huang CH, Lo WH (2002) The effect of malalignment on stresses in polyethylene component of total knee prostheses—a finite element analysis. Clin Biomech 17:140–146
Luyckx T, Zambianchi F, Catani F, Bellemans J, Victor J (2013) Coronal alignment is a predictor of the rotational geometry of the distal femur in the osteo-arthritic knee. Knee Surg Sports Traumatol Arthrosc 21:2331–2337
Magnussen RA, Weppe F, Demey G, Servien E, Lustig S (2011) Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res 469:3443–3450
Matsuda S, Whiteside LA, White SE (1999) The effect of varus tilt on contact stresses in total knee arthroplasty: a biomechanical study. Orthopedics 22:303–307
Matziolis G, Adam J, Perka C (2010) Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg 130:1487–1491
Miller EJ, Pagnano MW, Kaufman KR (2014) Tibiofemoral alignment in posterior stabilized total knee arthroplasty: static alignment does not predict dynamic tibial plateau loading. J Orthop Res 32:1068–1074
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 69:745–749
Paley D (2002) Principles of deformity correction. Springer, Berlin, Heidelberg, pp 1–60
Pang H-N, Jamieson P, Teeter MG, McCalden RW, Naudie DDR, Macdonald SJ (2014) Retrieval analysis of posterior stabilized polyethylene tibial inserts and its clinical relevance. J Arthroplasty 29:365–368
Parratte S, Pagano MW, Trousdale RT, Berry DJ (2014) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92:2143–2149
Paternostre F, Schwab PE, Thienpont E (2014) The difference between weight-bearing and non-weight bearing alignment in patient-specific instrumentation planning. Knee Surg Sports Traumatol Arthrosc 22:674–679
Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 93:1588–1596
Srivastava A, Lee GY, Steklov N, Colwell CW, Ezzet KA, D’Lima DD (2012) Effect of tibial component varus on wear in total knee arthroplasty. Knee 19:560–563
Swärd P, Fridén T, Boegård T, Kostogiannis I, Neuman P, Roos H (2013) Association between varus alignment and post-traumatic osteoarthritis after anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 21:2040–2047
Tew M, Waugh W (1985) Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg Br 67:551–556
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330
Vanwanseele B, Parker D, Coolican M (2009) Frontal knee alignment: three-dimensional marker positions and clinical assessment. Clin Orthop Relat Res 467:504–509
Victor JM, Bassens D, Bellemans J, Gürsu S, Dhollander AA, Verdonk PC (2014) Constitutional varus does not affect joint line orientation in the coronal plane. Clin Orthop Relat Res 472:98–104
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vandekerckhove, PJ.T.K., Matlovich, N., Teeter, M.G. et al. The relationship between constitutional alignment and varus osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 25, 2873–2879 (2017). https://doi.org/10.1007/s00167-016-3994-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-3994-4