Abstract
Purpose
Meniscal graft extrusion is a concern following meniscal allograft transplantation (MAT). MAT surgical techniques continue to evolve in an effort to reduce extrusion; however, improvements remain difficult to measure in vivo. A novel MRI-compatible in vitro loading device capable of applying physiologically relevant loads has been developed, allowing for the measurement of extrusion under a variety of controllable conditions. The objective of this study was to compare maximal medial MAT extrusion (1) with and (2) without an additional peripheral third point of fixation on the tibial plateau.
Methods
Twelve human cadaveric knees underwent medial MAT, utilizing soft tissue anterior and posterior root fixation via transosseous suture, with a third transosseous suture tied over a button providing peripheral fixation on the tibial plateau. The joint was positioned at 5 degrees of flexion and loaded to 1 × body weight (647.7 ± 159.0 N) during MR image acquisition, with and without peripheral fixation. The joint was then positioned at 30 degrees of flexion and the process was repeated. Maximal coronal extrusion was measured.
Results
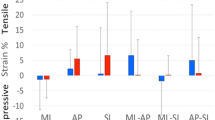
An increase in maximal coronal meniscal extrusion was noted between the unloaded and loaded states. At 30 degrees of flexion, with the addition of a peripheral fixation point, a statistically significant difference in absolute extrusion (p = 0.02) and relative percent extrusion (p = 0.04) between the unloaded and loaded state was found. The addition of a peripheral fixation suture resulted in an overall mean percent difference of − 2.49% (SD 14.1; 95% CI − 11.95, 6.97; n.s.) in extrusion at 5 degrees of flexion and a mean percent difference of − 0.95% (SD 7.3; 95% CI − 5.62, 3.71; n.s.) in extrusion at 30 degrees of flexion. These differences were not statistically significant.
Conclusion
These results suggest that the addition of a peripheral anchor in medial MAT does not reduce the amount of maximal coronal extrusion and, therefore, may not confer any clinical benefit. Surgical techniques utilized to reduce MAT extrusion need further investigation to understand if the added technical difficulty and potential expense is warranted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The meniscus is one of the most commonly injured structures in the knee, resulting in pain, swelling and mechanical symptoms [1]. Although meniscus repair techniques have resulted in improved patient outcomes, partial meniscectomy remains one of the most common arthroscopic procedures performed in the knee. The loss of meniscus tissue results in a reduction of joint congruity and load sharing, and is associated with the degeneration of articular cartilage and premature development of osteoarthritis (OA) [2].
Meniscus allograft transplantation (MAT) has been advocated in the treatment of the partial or total meniscectomized knee in young, active patients to provide pain relief and functional improvements [3]. However, MAT has not been shown to reduce the incidence of OA [4]. A major concern regarding MAT is post-operative extrusion of the meniscus graft, often visualized using magnetic resonance imaging (MRI) [5]. Graft extrusion, defined as the distance the meniscus graft displaces out of the joint [6], results in non-anatomic positioning of the allograft and can lead to biomechanical disadvantages such as loss of meniscal load sharing [5].
As a result, the surgical technique of MAT continues to evolve. Early techniques involved the use of soft tissue anchors to attach the cadaveric meniscus graft into the affected compartment [7]. Later techniques employed the use of bone bridges or bone plugs, which retain the important anterior and posterior meniscotibial ligaments, to provide strong attachment at these sites [8]. Recent studies have shown improved graft stability with bone plug fixation when compared to soft tissue anchor fixation [9, 10]. However, meniscus extrusion still remains a significant problem common to the aforementioned techniques [11]. Most recent techniques have attempted to employ different root fixation techniques again with the attempt of reducing extrusion [12,13,14,15,16].
Surgical techniques have been described in the literature, which may improve the incidence of extrusion. In 2003, Stone and Walgenbach published a technical note describing a three-tunnel technique, which involves a third fixation point of the meniscus graft to the tibia to increase the stability of the graft [17]. In 2018, Masferrer-Pino et al. described an all arthroscopic technique that included a capsulodesis to try and reduce extrusion, reporting similar results to a bone bridge fixation, although they recognized a steep learning curve that may have had a negative impact on the results [13]. However, there is a paucity of data with regard to meniscus extrusion studied in a controlled, laboratory setting. One major concern is that surgical techniques to reduce extrusion could result in over-constraining the meniscus graft, thereby altering the physiological loads placed on the graft, resulting in graft injury and, ultimately, failure of the MAT.
The hypothesis of this study was that an additional point of peripheral fixation of the meniscus graft to the tibial plateau would result in a reduction in meniscus extrusion during simulated joint loading following meniscal allograft transplantation.
Materials and methods
Twelve fresh-frozen human cadaveric knees (six males, mean age 67 years) underwent medial MAT using a standardized surgical procedure described below. Specimens were evaluated using a novel MRI-compatible loading device which is capable of positioning and loading a cadaveric knee joint using simulated quadriceps and hamstring forces applied via hydraulic actuators [18]. The device has been shown to have good repeatability and reproducibility, making it an effective tool for in vitro testing of soft tissue repairs of the knee [18]. Magnetic resonance images were acquired with the joint positioned at 5 degrees and 30 degrees of flexion, in both the unloaded and loaded states (Fig. 1).
Surgical technique
Knee joint specimens were prepared for the loading device as per a published protocol [18]. The specimens were size-matched to within 4 mm of fresh-frozen meniscus allografts via fluoroscopy using the technique described by Pollard et al. [19]. The native meniscus was removed arthroscopically by a fellowship trained knee surgeon who has clinical experience with MAT (blinded), preserving the peripheral rim. Arthroscopic medial MAT was then performed by the same surgeon, with fixation of the anterior and posterior horns being achieved via two transosseous sutures tied over the anteromedial tibial cortex. The meniscus graft was fixated and sutured in place using a standardized inside-out suture technique. A third transosseous tunnel was placed from the anterolateral tibial cortex to the periphery of the tibial plateau, at the 50% position on the circumference of the meniscus body as described by Stone and Walgenbach (Fig. 2) [17]. A suture was anchored to the meniscus and pulled through the tunnel; however, it was not fixed over a button on the anteromedial cortex until after the baseline MRI images were acquired (Fig. 3).
Imaging protocol
Knee specimens were manually cycled through ten repetitions of flexion and extension prior to testing. The joint was loaded into the device and positioned at 5 degrees of flexion using a handheld goniometer. The device was loaded into a 3-Tesla MRI (MAGNETOM Prisma, Siemens Healthcare) and T1-weighted VIBE images of the unloaded joint were acquired. Image acquisition time was approximately 6 min. Anatomical load was then applied in the MRI scanner via the quadriceps and hamstring muscle cables via hydraulic actuators until a joint load of approximately body weight (647.7 ± 159.0 N) was achieved. Another image was acquired in this loaded state. The knee joint was then positioned at 30 degrees of flexion and images were acquired in the unloaded and then loaded states. The peripheral, transosseous suture was then tied over a button and the entire series was repeated following manual conditioning of the knee joint.
This laboratory study was performed under the standard Western University institutional approval for the use of anonymous human cadaveric tissue.
Data analysis
Meniscal extrusion was measured in the coronal plane using the technique described by Lee et al. [5] using OsiriX Imaging Software (Pixmeo) with a measurement accuracy of 0.1 mm [20]. Since maximal graft extrusion in the coronal plane usually occurs at the mid-body region, extrusion was measured on the most central coronal slice. Absolute meniscal extrusion, defined as the distance between the outer edge of the tibial plateau and the outer edge of the meniscus, was measured. Relative percentage of extrusion (RPE), defined as the width of the extruded menisci relative to the total width of the meniscus, was then calculated (Fig. 4) [5, 21].
Two fellowship trained orthopaedic surgeons independently evaluated all of the scans (inter-rater reliability 0.75; 95% CI 0.61–0.84) and the average value of their measurements were used during the analysis.
Statistical analysis
Meniscal graft extrusion measurements with two fixation points only were compared to those with the third fixation point using paired sample t tests at both 5 degrees and 30 degrees of flexion. All statistical analyses were performed using SPSS Statistics version 22 (IBM Corp., Armonk, NY). A p value < 0.05 was considered to be statistically significant. A three-way ANOVA was then performed to determine if there is an interaction between surgical technique, knee flexion angle and load. The inter-rater reliability of graft extrusion measurements was assessed by calculating the interclass correlation coefficient (ICC).
Results
Absolute extrusion and relative percentage of extrusion (RPE) of the meniscus graft increased when the joint was loaded compared to the unloaded state for both fixation techniques (Table 1; Fig. 5). At 30 degrees of flexion, the increase in extrusion for the three-tunnel fixation was statistically significant.
There were no statistically significant differences found between the two surgical techniques in mean difference measurements comparing loaded versus unloaded states (Table 2). The addition of a peripheral fixation suture resulted in an overall mean percent difference of − 2.49% (SD 14.1; 95% CI − 12.0, 7.0; n.s.) in extrusion at 5 degrees of flexion and a mean percent difference of − 0.95% (SD 7.3; 95% CI − 5.6, 3.7; n.s.) in extrusion at 30 degrees of flexion. These differences were not statistically significant.
The three-way interaction between surgical technique, flexion angle and load was not statistically significant (n.s.).
Reliability
In the present study, the inter-rater reliability for all measurements was 0.75 (95% confidence interval 0.6–0.8), indicating good reliability [22].
Discussion
The most important finding of this study was that the addition of a peripheral fixation point did not affect the degree of graft extrusion following medial MAT. In 2003, Stone and Walgenbach [17] originally suggested that the addition of a third peripheral fixation point of the meniscus graft to the tibial plateau would increase the stability of the graft. Using fresh cadaveric knees fixed in a MRI-compatible joint loading device, our study is the first to use a simulated physiological loading approach to provide clear empirical evidence to suggest that the addition of a peripheral fixation point does not significantly change graft extrusion compared with traditional methods in both the loaded and unloaded states. To our knowledge no other studies examining the addition of a third point of fixation have been published.
In comparison to clinical studies we found lower absolute values of graft extrusion. Ha et al. [21] found an average of 4.18 ± 1.44 mm of extrusion in medial MATs and 3.65 ± 2.06 mm in lateral MATs. Lee et al. [5] found average values of 4.29 ± 1.39 mm and 2.74 ± 1.05 mm of absolute extrusion in medial and lateral MATs, respectively. The largest value of extrusion in the current study was only 3.02 ± 1.1 mm and it occurred in the loaded condition. This suggests that meniscus extrusion may gradually increase over time and may indicate a combined mechanical and biological cause requiring further clinical investigation.
Numerous other studies examining meniscus extrusion following MAT have been published [5, 9, 21, 23,24,25,26]. Noyes and Barber-Westin [26] performed a systematic review to determine the incidence and clinical significance of meniscus extrusion following MAT. Seven studies found no significant association between extrusion and patient-reported outcomes. However, most studies report short-term results following MAT.
It is hypothesized that meniscus extrusion results in the loss of articular surface cover and loss of contact with the joint surfaces resulting in reduced joint congruency, which in turn leads to increased contact pressures over the joint surface. This can potentially lead to the loss of chondroprotection and result in increased wear. Extrusion of the native meniscus has a high association with meniscal tears, and it has been associated with the development of osteoarthritis [27]. Therefore, extrusion following MAT may result in graft failure and the early development of osteoarthritis.
This is the first study to quantitatively study meniscal graft extrusion under simulated physiological loading in a controlled, laboratory setting. The ability to show an increase in extrusion under load and the high inter-rater reliability (ICC 0.75) suggest this is an acceptable method for examining meniscus extrusion out of the knee joint. The ability to compare surgical techniques in a simulated, laboratory setting is of huge benefit to the surgical community.
This study is limited by its small sample size, resulting in high variability and inadequate power to draw definitive conclusions. However, in vitro testing is both costly and time consuming, and this exploratory study of 12 cadaveric knee joints offers an initial baseline of the magnitude of graft extrusion following MAT. Furthermore, due to limited resources not all allografts were perfectly size-matched to the knee specimens. In the clinical setting, MAT would only proceed when a perfect size-match was found. Knee flexion angles were set using a handheld goniometer which has been shown to have an error of anywhere between five and ten degrees [28]. Lastly, some of the knees had prior meniscal damage with the peripheral rim not fully intact. This may have a significant effect on post-op extrusion and requires further study.
The clinical relevance of this study pertains to the extra point of fixation of a medial MAT. Following on from Stone’s original paper [17], there have now been a number of technical studies describing the use of peripheral fixation in MAT. To date, none of these techniques have actually been investigated as to whether they actually reduce extrusion, and whether this has an effect on clinical outcome following MAT. Until that time, this current shows that the addition of peripheral fixation may not be worth the added technical complexity, expense of fixation, and potential further surgical morbidity. Translation into common clinical practice should, therefore, be guarded until clinical studies have investigated its utilization and efficacy more rigorously.
Conclusions
The present study provides evidence to suggest that the addition of a peripheral anchor does not significantly change the amount of maximal coronal extrusion of a medial meniscal allograft, and is thus not recommended when performing MAT. Furthermore, using an MRI-compatible joint loading device, our study provides the first example of specimen-matched, radiographic surgical assessment of human joints during unloaded and physiologically loaded condition states.
References
Horneff J (2014) Meniscectomy: the basics. In: Kelly JD IV (ed) Meniscal injuries. Springer, Berlin, pp 39–44
McDermott ID, Amis AA (2006) The consequences of meniscectomy. J Bone Joint Surg Br 88:1549–1556
Hergan D, Thut D, Sherman O, Day MS (2011) Meniscal allograft transplantation. Arthroscopy 27:101–112
ElAttar M, Dhollander A, Verdonk R, Almqvist KF, Verdonk P (2011) Twenty-six years of meniscal allograft transplantation: is it still experimental? A meta-analysis of 44 trials. Knee Surg Sports Traumato Arthrosc 19:147–157
Lee D-H, Lee C-R, Jeon J-H, Kim K-A, Bin S-I (2015) Graft extrusion in both the coronal and sagittal planes is greater after medial compared with lateral meniscus allograft transplantation but is unrelated to early clinical outcomes. Am J Sports Med 43:213–219
De Coninck T, Huysse W, Verdonk R, Verstraete K, Verdonk P (2013) Open versus arthroscopic meniscus allograft transplantation: magnetic resonance imaging study of meniscal radial displacement. Arthroscopy 29:514–521
Van Arkel ER, De Boer HH (1992) Human meniscus transplantation. Agents Actions Suppl 39:243–246
Noyes FR, Heckmann TP, Barber-Westin SD (2012) Meniscus repair and transplantation: a comprehensive update. J Orthop Sports Phys Ther 42:274–290
Abat F, Gelber PE, Erquicia JI, Pelfort X, Gonzalez-Lucena G, Monllau JC (2012) Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med 40:1591–1596
Abat F, Gelber PE, Erquicia JI, Tey M, Gonzalez-Lucena G, Monllau JC (2013) Prospective comparative study between two different fixation techniques in meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc 21:1516–1522
Verdonk PCM, Verstraete KL, Almqvist KF, De Cuyper K, Veys EM, Verbruggen G et al (2006) Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc 14:694–706
Lee DW, Park JH, Chung KS, Ha JK, Kim JG (2017) Arthroscopic lateral meniscal allograft transplantation with the key-hole technique. Arthrosc Tech 6:e1815–e1820
Masferrer-Pino A, Monllau JC, Ibanez M, Erquicia JI, Pelfort X, Gelber PE (2018) Capsulodesis versus bone trough technique in lateral meniscal allograft transplantation: graft extrusion and functional results. Arthroscopy 34:1879–1888
Woodmass JM, Johnson NR, Levy BA, Stuart MJ, Krych AJ (2017) Lateral meniscus allograft transplantation: the bone plug technique. Arthrosc Tech 6:e1215–e1220
Zacchilli MA, Dai AZ, Strauss EJ, Jazrawi LM, Meislin RJ (2017) Bone trough lateral meniscal allograft transplantation: the tapered teardrop technique. Arthrosc Tech 6:e2301–e2312
Zhang YD, Hou SX, Zhong HB, Zhang YC, Luo DZ (2018) Meniscal allograft transplantation using a novel all-arthroscopic technique with specifically designed instrumentation. Exp Ther Med 15:3020–3027
Stone KR, Walgenbach AW (2003) Meniscal allografting: the three-tunnel technique. Arthroscopy 19:426–430
Chen L, Gordon K, Hurtig M (2014) Design and validation of a cadaveric knee joint loading device compatible with magnetic resonance imaging and computed tomography. Med Eng Phys 36:1346–1351
Pollard ME, Kang Q, Berg EE (1995) Radiographic sizing for meniscal transplantation. Arthroscopy 11:684–687
Kim G, Jung HJ, Lee HJ, Lee JS, Koo S, Chang SH (2012) Accuracy and reliability of length measurements on three-dimensional computed tomography using open-source OsiriX software. J Digit Imaging 25:486–491
Ha JK, Shim JC, Kim DW, Lee YS, Ra HJ, Kim JG (2010) Relationship between meniscal extrusion and various clinical findings after meniscus allograft transplantation. Am J Sports Med 38:2448–2455
Fleiss JL (1981) The measurement of interrater agreement. Stat Methods Rates Proportions 2:212–236
Jang SH, Kim JG, Ha JG, Shim JC (2011) Reducing the size of the meniscal allograft decreases the percentage of extrusion after meniscal allograft transplantation. Arthroscopy 27:914–922
Koh YG, Moon HK, Kim YC, Park YS, Jo SB, Kwon SK (2012) Comparison of medial and lateral meniscal transplantation with regard to extrusion of the allograft, and its correlation with clinical outcome. J Bone Joint Surg Br 94:190–193
Lee D-H, Kim S-B, Kim T-H, Cha E-J, Bin S-I (2010) Midterm outcomes after meniscal allograft transplantation comparison of cases with extrusion versus without extrusion. Am J Sports Med 38:247–254
Noyes FR, Barber-Westin SD (2015) A systematic review of the incidence and clinical significance of postoperative meniscus transplant extrusion. Knee Surg Sports Traumatol Arthrosc 23:290–302
Harper KW, Helms CA, Lambert Iii HS, Higgins LD (2005) Radial meniscal tears: significance, incidence, and MR appearance. AJR 185:1429–1434
Milanese S, Gordon S, Buettner P, Flavell C, Ruston S, Coe D et al (2014) Reliability and concurrent validity of knee angle measurement: smart phone app versus universal goniometer used by experienced and novice clinicians. Man Ther 19:569–574
Funding
This study was supported by a research grant from the Musculoskeletal Transplant Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Ethical approval
This laboratory study was performed under the standard Western University institutional approval for the use of anonymous human cadaveric tissue.
Informed consent
For this type of study informed consent was not required.
Rights and permissions
About this article
Cite this article
Hewison, C., Kolaczek, S., Caterine, S. et al. Peripheral fixation of meniscal allograft does not reduce coronal extrusion under physiological load. Knee Surg Sports Traumatol Arthrosc 27, 1924–1930 (2019). https://doi.org/10.1007/s00167-018-5305-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5305-8