Abstract
Purpose
To determine the incidence and clinical significance of postoperative meniscus transplant extrusion.
Methods
A systematic search was performed using PubMed and Cochrane online databases. Inclusionary criteria were English language, clinical trials of meniscus transplantation published from 1984 to 2014, and meniscus extrusion measured on magnetic resonance imaging (MRI).
Results
Twenty-three studies were included, in which 814 menisci were implanted into 803 patients. MRIs were obtained from 2 days to 10 years postoperatively. Eighteen studies used fresh-frozen meniscus transplants implanted with bone (n = 612) or suture fixation (n = 116); four studies, cryopreserved transplants; and one, irradiated transplants. Three measurements assessed extrusion: absolute millimeters of extrusion (0–8.8 mm), relative percentage of extrusion (0–100 %), and the percent of transplants that were extruded (0–100 %). Relationships between transplant extrusion and clinical rating scales, joint space narrowing on standing radiographs, and arthrosis progression were inconclusive. Non-anatomic placement of lateral meniscus transplants and suture fixation of medial and lateral transplants were associated with greater extrusion in two studies.
Conclusions
Inconsistencies among studies prevent conclusions regarding the incidence and clinical significance of meniscus transplant extrusion. Even so, the short- to mid-term results were encouraging for knee function with daily activities and low rates of failure requiring transplant removal. A postoperative MRI showing more than 3-mm extrusion occurring in some studies suggested technique and/or implant sizing problems that required correction. Future studies should report absolute transplant extrusion, relative percent of extrusion, percent of transplant within the tibiofemoral compartment, and the percent of transplants that are extruded.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Meniscus transplantation is an accepted operation for younger, active patients who have undergone a meniscectomy, have pain that limits activities, and demonstrate early articular cartilage deterioration in the involved tibiofemoral compartment. The goals are to restore partial load-bearing meniscus function, decrease symptoms, and provide some chondroprotective effects [16, 20, 35, 49]. The method and goal of transplant fixation are to reproduce the normal attachment sites, allowing transplants to remain in their anatomic location (without extrusion) and move normally throughout knee motion [12, 39]. Most investigators have implanted grafts with bony fixation accomplished with a central bone bridge or a two-tunnel double bone-plug technique, although a few [17, 46, 50] have implanted grafts secured with suture fixation. The problem exists that many investigations report, from either magnetic resonance imaging (MRI) or follow-up arthroscopy findings, that most transplants gradually deteriorate, tear, extrude from their normal position, or shrink in size, thereby loosing the ability to provide the function required to achieve chondroprotective effects [14, 18, 24, 38].
The meniscus is considered extruded, subluxed, or displaced when it extends beyond the tibial margin. Meniscal extrusion is a well-recognized phenomenon in the natural course of aging and degenerative knee joint disease [3, 13, 44] and may also exist in normal, asymptomatic knees [4, 8, 52]. Both medial and lateral meniscus extrusion are associated with lower extremity malalignment (varus or valgus) and chondral damage [13].
The hypothesized causes of meniscus transplant extrusion include preoperative sizing issues resulting in an oversized graft, overtensioning of meniscus sutures during surgery, loss of fixation of the anterior and posterior horns, non-anatomic position of the insertion site of the graft, and unrestored meniscotibial ligament and popliteomeniscal fascicles [29, 41, 48, 51]. More than 3 mm of extrusion is considered by some investigators to be clinically significant because it has been hypothesized that this amount will result in altered biomechanical function and progression of osteoarthritis [11, 13, 31]. However, the effect of different amounts of meniscal extrusion on joint contact area and pressures under loading conditions is unknown. The clinical implications of extrusion of meniscus transplants are unclear with regard to symptoms, functional limitations, and future joint deterioration. Therefore, the purpose of this study is to determine the incidence of meniscus transplant extrusion, the effect of graft fixation techniques on extrusion rates, and the clinical significance of this potential problem.
Materials and methods
Search strategy
PRISMA guidelines were followed in conducting this study [30]. An online search was performed using PubMed (January 1, 1984, to February 28, 2014) and the Cochrane Database of Systematic Reviews (2005 to February 28, 2014) using the key phrases “meniscus allograft transplantation” and “meniscus extrusion.” Major orthopedic journals were searched individually using these terms, including Arthroscopy, American Journal of Sports Medicine, Journal of Bone and Joint Surgery (American and British), Knee Surgery Sports Traumatology Arthroscopy, Journal of Knee Surgery, Knee, and Sports Health. The full text was retrieved and reviewed if the abstract suggested that this might be a clinical study in our topic of interest. Article reference lists from general review articles, systematic reviews, and meta-analyses obtained from the search were examined in order to find any other original research investigations not otherwise obtained. In addition, the reference lists of the articles that met the inclusionary criteria were searched.
Study selection
Inclusionary criteria were as follows: (1) English language, (2) meniscus extrusion measured postoperatively with MRI, (3) any patient age, (4) clinical trials of all kinds, and (5) all levels of evidence. Exclusionary criteria were as follows: (1) articles that were off topic, (2) laboratory-based investigations, (3) investigations that focused on transplant sizing and tissue banking issues, (4) failure to achieve the inclusionary criteria listed above, and (5) other types of articles such as case reports, abstracts, and technical notes. In addition, any study that was later updated with longer follow-up and a larger cohort was excluded.
Data extraction
Each study that met the inclusion criteria was abstracted for information regarding the following: (1) total number of patients entered into study, (2) number of patients that underwent postoperative MRI, (3) number of meniscus transplants that underwent postoperative MRI, (4) number of medial and lateral meniscus transplants that underwent postoperative MRI, (5) number of males and females, (6) patient age at index operation, (7) duration of symptoms before the index operation, (8) time postoperatively the MRIs were obtained, (9) associated major operative procedures, (10) condition of the articular cartilage in the affected tibiofemoral compartments at surgery, (11) transplant processing, (12) transplant fixation methods, (13) preoperative sizing methods, (14) area where extrusion was measured, (15) absolute extrusion (millimeters) for all transplants, (16) absolute extrusion for medial meniscus transplants (MMT), (17) absolute extrusion for lateral meniscus transplants (LMT), (18) relative percentage of extrusion (RPE) for all transplants, (19) RPE for MMT, (20) RPE for LMT, (21) percent of all transplants that were extruded, (22) percent of MMT that were extruded, (23) percent of LMT that were extruded, (24) results of clinical outcome assessments, (25) correlation analyses between extrusion and any factor, and (26) study conclusions and recommendations. The findings were reviewed by both authors and agreement reached regarding data extracted. The level of evidence for each study was documented as determined by the journal of publication [36, 54].
Data synthesis
A quantitative analysis of the data abstracted was not performed because the included studies were heterogeneous with regard to the following: meniscus transplant processing, methods of transplant fixation, the amount of time postoperatively MRIs were obtained, the location where transplant extrusion was measured, method of reporting of transplant extrusion, the type of postoperative radiographs, articular cartilage grading systems, and clinical rating scales. Therefore, the results were qualitatively compared and summarized in the current systematic review [30].
Results
Literature search
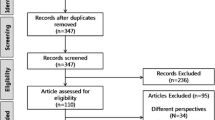
The online search initially identified 193 original research articles. In addition, 57 general review articles, systematic reviews, and meta-analyses were reviewed for additional studies, but not included in the final study. A total of 170 original articles were excluded for the reasons shown in Table 1. Of note was the finding that 31 clinical outcome studies did not include MRI, and 8 other studies obtained postoperative MRI, but did not measure or report on transplant extrusion. This left 23 articles that were included in this systematic review [1, 12, 14, 17–19, 22–25, 27–29, 35, 38, 39, 43, 47, 48, 50, 55, 58, 59].
Patient and meniscus transplant characteristics
A total of 1,006 patients were enrolled in the 23 studies, of whom 803 (80 %) underwent MRI. Seventeen studies identified the gender of the patients, which were 475 men and 196 women. The mean patient age was 34 years (range 14–57 years).
There were 814 menisci transplanted: 508 LMT and 306 MMT. Most studies used the radiographic method described by Pollard et al. [37] to obtain transplant size measurements (Table 2). Some investigators emphasized the effort to obtain true anteroposterior (AP) and lateral radiographs, with magnification factors accounted for, and attempted to not exceed a 10 % mismatch with regard to transplant width and length [18, 23, 24, 27, 43]. One study used the exact dimensions obtained with the Pollard method in one group of knees, and then reduced these dimensions by 5 % in a second group in a deliberate effort to reduce the incidence of transplant extrusion [22]. Another study used both the Pollard method and morphometric dimensions (patient weight and size) [17], while another used the Pollard method and a calibrated computed tomography (CT) scan to obtain maximum diameter of the medial or lateral tibial plateau [59]. MRI was used in two studies in which the axial cut of the tibial plateau was used to determine transplant width and length [14, 58].
Associated operative procedures
Two hundred and forty-five major concomitant operative procedures were performed in the 803 patients (Table 3). The most common were anterior cruciate ligament (ACL) reconstructions (138 patients, 17 %) and articular cartilage restorative procedures (82 patients, 10 %).
Condition of the articular cartilage in the involved tibiofemoral compartment at transplantation
Six studies described the condition of the articular cartilage in the involved tibiofemoral joint [18, 35, 38, 39, 50, 55]. Using the Outerbridge classification system, four studies [18, 38, 50, 55] documented abnormal cartilage (grades 3–4) in 9 % [55], 14 % [18], 35 % [50], and 92 % [38] of the knees. Two studies [35, 39] used the Cincinnati articular cartilage classification system; one [39] reported that 62 % had abnormal findings (grades 2B and 3A) and the second [35] reported that 85 % had abnormal findings. Three studies [1, 12, 28] did not provide specific data, but reported that patients with either more than a grade 2 [1, 28] or grade 3 [12] cartilage lesion were not considered for the operation.
Meniscus transplant extrusion: indices measured
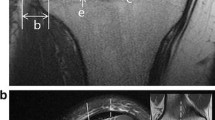
The timing of the postoperative MRI varied (Table 4). Transplant extrusion was typically measured on coronal MRI slices on a horizontal line parallel to the proximal tibial articular surface, defined as the distance between the outer edge of the transplant and the outer edge of the tibial articular surface (Fig. 1). Variability existed in the areas in which transplant extrusion was measured. While some studies indicated the exact site (midbody or anterior and posterior horns), others indicated that extrusion was measured from the coronal MRI image that showed maximal extrusion. The areas that were then selected and used for analysis were not indicated.
Example of how the amount of extrusion of the meniscus transplant was measured in one study. Extrusion at the medial (a) or lateral (b) sides was measured from the outer margin of the medial or lateral tibial plateau at the proximal articular cartilage surfaces to the meniscal outer edge (reprinted with permission from Lee et al. [28])
Measurements used were the absolute amount of transplant extrusion (given in millimeters), the RPE ([width of extruded meniscus]/[width of entire meniscus] × 100), and/or the percent of transplants that were extruded. Different indicators described the amount of transplants that were extruded such as “partial” or “some degree,” or a measurement (i.e., >3 mm) was used to define extrusion. Twenty-one studies obtained MRIs in the supine, non-weight-bearing position and two conducted the scans under partially loaded (176 N) [35] or fully loaded (standing, 100 % weight bearing) [39] conditions.
Effect of preservation and fixation on meniscus transplant extrusion
Fifteen studies analyzed 612 fresh-frozen meniscus transplants implanted with bone fixation (Table 4). Yoon et al. [58] compared MMT with LMT and reported a significant difference in the RPE (32 and 19 %, respectively, P = 0.01). In contrast, Koh et al. [25] reported that LMT had significantly greater extrusion and RPE than MMT (P < 0.001). Two studies [23, 55] found that all of the transplants extruded to “some degree,” while others [12, 27] reported that 47–48 % extruded more than 3 mm. Five studies [18, 24, 28, 29, 38] combined MMT and LMT and reported mean extrusion values from 2.96 to 3.87 mm and RPE from 29 to 42.6 %.
Three studies [35, 39, 43] analyzed 48 cryopreserved meniscus transplants implanted with bone fixation. Rankin et al. [39] reported that 14 % of anterior horns and 28 % of posterior horns were extruded greater than 3 mm. Noyes et al. [35] found only 1 of 29 transplants had major extrusion (9 mm). Five studies [1, 14, 17, 48, 50] analyzed fresh-frozen meniscus transplants implanted without bone fixation and reported that 70–100 % had some degree of extrusion.
Correlation meniscus transplant extrusion and other factors
Correlation analyses between transplant extrusion and clinical, surgical technique, or radiographic factors were done in ten studies (Table 5). Seven found no significant associations between extrusion and clinical-scale scores. All four investigations that studied radiographic factors failed to find any significant associations with transplant extrusion [18, 19, 22, 28].
Discussion
The most important findings of the present study were the inconsistencies among the 23 studies regarding the incidence and clinical significance of meniscus transplant extrusion that led to our recommendations for future work in this area, as will be discussed later. There were differences in the time MRIs were obtained, how extrusion was measured and reported, descriptions of the condition of the articular cartilage at surgery, and clinical rating scales used to assess outcome. Even so, conclusions may be drawn and recommendations made for future studies with regard to MRI and clinical factors to rate and the timing of postoperative assessments. The mostly short-term results of the studies in this review were encouraging with regard to knee function during daily activities and low rates of failure.
MRIs were obtained in one study [58] between 6 months and 10 years postoperatively and between 3 months and 3.4 years postoperatively in another [38]. It would be useful for future studies to acquire a postoperative MRI early after meniscus transplantation in all patients when full weight-bearing has been resumed to determine the initial healing, height, width, and extent of extrusion. Then, a second MRI could be obtained later at a defined time to determine whether changes in meniscus characteristics occurred. In addition, studies should obtain MRIs at the same time period in all patients in a prospective manner to eliminate the high variability found in this review.
There are several advantages of obtaining an MRI after meniscus transplantation. The surgeon can determine whether the operative technique was successful in terms of transplant placement and fixation and prevention of extrusion. Two studies that reported high rates of extrusion were able to identify problems with operative techniques that were addressed. Choi et al. [12] obtained MRIs 6 months postoperatively and noted that non-anatomic placement of the bone bridge was a cause of LMT midbody extrusion. These investigators recommended placing the center of the bone bridge as close to the middle of the tibial plateau as possible. Lee et al. [27] collected MRIs immediately after surgery and reported that the risk of LMT extrusion increased as the axial bony trough angle increased. The recommendation was made to reduce the angle by ensuring the starting point of the trough was not created in too lateral a position. Other authors recommended using a template of the implant at surgery to more accurately establish the bone bridge placement of LMT [35] and to use a transpatellar approach and ream the tunnel with the knee fully extended [58] (Table 6).
Another advantage of obtaining a postoperative MRI is that, if extrusion or a reduced meniscus size is found, the surgeon may counsel the patient regarding future high-loading activities. This is especially warranted in individuals who wish to resume athletics or in whom articular cartilage deterioration is already present.
In our review, 40 of the 63 (63 %) clinical outcome studies that comprised 1,432 transplants were excluded because they either did not obtain MRIs or did not provide meniscus extrusion data. This represents nearly 60 % of all meniscus transplants that have been reported in the English literature as of the time of writing. Acknowledging that some of these studies were done before the widespread use of MRI, the recommendation is made for future studies to include meniscus morphology data using the most sophisticated MRI scanners and software available. One problem exists that, at present, clinicians cannot predict when meniscus transplants begin the degenerative process that involves shrinking, extrusion, and/or tearing frequently reported [9, 14, 17, 35, 38, 43, 47]. Noyes et al. [35] reported this deleterious remodeling process occurred in approximately 50 % of transplants a mean of 3 years postoperatively and believed that most, if not all, transplants will undergo alterations in collagen fiber architecture that affect load-sharing capabilities and long-term survival. If future studies include MRI in the assessment of postoperative transplant characteristics, these issues may become clearer.
This systematic review was unable to answer the question of the definition of clinically relevant meniscus transplant extrusion in terms of symptoms and/or future joint degeneration. Problems encountered were the wide variability in how meniscus extrusion was measured and reported and the relative short-term follow-up in the majority of studies. Although some authors provided the anatomic description of the area measured (midbody, anterior horn, posterior horn), others simply indicated that the region where the largest extrusion was found was used for analysis. Several investigators choose a value of greater than 3 mm to represent (or define) extrusion; however, there are no biomechanical studies we are aware of that support this value in regard to deleterious changes in contact area or pressure.
Clinical studies have provided extrusion reference values of normal, asymptomatic knees with no radiographic evidence of osteoarthritic degeneration that are useful in determining abnormal transplant extrusion values. For instance, Boxheimer et al. [6] reported that no knee (N = 22) had more than 3 mm of extrusion in either the sagittal (anterior and posterior horns) or coronal (midbody) plane. Bloecker et al. [4] obtained MRIs in 102 knees and reported mean extrusion rates in the midbody of medial menisci of 1.24 ± 1.18 mm in men and 0.83 ± 1.06 mm in women. Bruns et al. [8] found, in 118 subjects, mean extrusion values in the midbody of medial and lateral menisci of 1.64 ± 0.92 and 0.63 ± 0.73 mm, respectively.
In addition, the mean widths of the native medial and lateral meniscus have been reported to range (under non-weight-bearing conditions) from 8.86 to 11.8 and 8.6 to 10.4 mm, respectively [4, 8, 52]. One study [26] measured the width of 31 LMT 12 months postoperatively and reported a mean of 8.31 ± 1.79 mm in the midbody and 12.17 ± 2.75 mm in the posterior horn. Therefore, the extrusion value of more than 3 mm indicates ~35 % or more of the relative percentage of the entire meniscus width is displaced out of the tibiofemoral compartment. Huang et al. [21] previously reported the importance of matching the width and height of meniscus transplants to the native meniscus in determining contact pressure distribution. These authors noted that failure to match these cross-sectional parameters caused substantial differences in maximum pressure and contact area between allografts and autografts in cadaver knees.
Bruns et al. [8] proposed using the RPE instead of a millimeter value to describe meniscus extrusion to account for the normal variability in size of menisci and tibial width between genders. These authors suggested using tibial width as the denominator instead of meniscus width because the meniscus body may be affected by degeneration or tearing. Their meniscal body extrusion index is calculated by ([meniscus body extrusion/tibial width] × 100). This suggestion may be applicable to meniscus transplants in light of data from several studies that reported transplant shrinkage or degeneration on MRI [9, 14, 17, 35, 38, 43, 47].
Another method to consider in reporting meniscus transplantation MRI characteristics is percent of coverage. This value indicates the percent of the meniscus that is located within the tibiofemoral joint. Bruns et al. [8] suggested that this factor be calculated as: ([meniscus body width] − [meniscus body extrusion])/[ipsilateral tibia plateau width]. These authors found, in 118 asymptomatic subjects (aged 45–78 years), a mean percent coverage of 34.4 ± 12 % in the medial compartment and 31.1 ± 8 % in the lateral compartment. The authors attributed the wide range in this factor to the variety of anatomic shapes and dimensions of the tibial plateaus and meniscus bodies.
The measurement of meniscus extrusion or percent of coverage using standard MRI protocols provides, at best, an approximation of the position of the meniscus. A sophisticated analysis, full segmentation of meniscal body volume and its relation to the coverage of the tibial plateau, is possible with three-dimensional MRI modeling using commercially available software [4, 5, 52, 53]. Using this method, Bloecker et al. [4] reported (in 122 asymptomatic subjects) that the mean area of cartilage surface covered with the meniscus body was 50 ± 5.7 % in the medial compartment and 58 ± 6.8 % in the lateral compartment. In a similar manner, Wenger et al. [52] found (in 39 normal subjects) mean areas of coverage of 50 % in the medial compartment and 54 % in the lateral compartment. Both of these investigations were done under non-weight-bearing conditions, and only the position of the meniscus body from coronal images was determined. Future studies should also include sagittal images to determine anterior and posterior horn position, percent coverage, and extrusion. We recognize that three-dimensional reconstruction of the menisci is costly and time-consuming and, at present, not feasible in clinical practice. Future clinical investigations with available funding should conduct this advanced analysis of meniscus transplants so that a comparison may be made with previously reported data from native menisci in normal subjects.
In knees with preexisting noteworthy articular cartilage deterioration in the involved tibiofemoral compartment, it is not possible to determine, in patients in whom symptoms return after meniscus transplantation and extrusion is detected on MRI, whether the pain is due to the joint damage (subchondral bone exposed) or from a non-functioning transplant. In fact, there were investigations in this review in which high levels of extrusion were reported, but no correlations were found with clinical rating scales [1, 18, 19, 22, 25, 28]. Future studies should report the condition of the articular cartilage at surgery to allow an analysis to be performed of the effect of this variable on extrusion and subsequent clinical symptoms.
Seven studies [1, 18, 19, 22, 25, 28, 50] found no relationship between meniscus transplant extrusion and function in terms of daily activities and symptoms. Ha et al. [18] noted three possible explanations for the lack of such as association: Extrusion does not have a marked effect on the chondroprotective effect of the transplant, the duration of follow-up was too short (2–3 years), and other factors exist that effect functional results such as rehabilitation, chondral status, and transplant healing. Overall, the data showed that the transplants were still functional in terms of pain relief with daily activities, even though some extrusion was noted in many patients. It would be helpful for future studies to use both daily and sports activity rating scales and to separately rate pain in the involved tibiofemoral compartment so that additional analyses may be conducted.
Four investigators found no association between transplant extrusion and joint space narrowing on radiographs or arthrosis grade progression measured on MRI or follow-up arthroscopy [18, 19, 22, 28]. The problem of the short-term follow-up was acknowledged by these authors. Future studies should conduct these analyses when all patients are in the mid- to long-term postoperative time period (5–10 years).
The hypothesized causes of meniscus transplant extrusion include preoperative sizing issues resulting in an oversized graft, overtensioning of the meniscus sutures during surgery, loss of fixation of both anterior and posterior horns, non-anatomic position of the insertion site of the graft, and unrestored meniscotibial ligament and popliteomeniscal fascicles [10, 15, 29, 41, 48, 51]. In addition, implanting a meniscus transplant into a joint that has lost its normal joint geometry, with flattening of the femoral condyle, concavity of the tibial plateau, and osteophytes that prevent anatomic seating of the transplant, has been hypothesized to lead to failure [34, 38, 43]. Absence of a remaining native meniscal rim or soft tissues required to suture and fixate the transplant would also be expected to play a role in subsequent extrusion.
In regard to meniscus transplant sizing issues, there exists a lack of consensus regarding the most reliable technique that will match the transplant to the patient’s bony dimensions. The majority of investigations used AP and lateral radiographs to obtain approximate width and length measurements for the transplant (based on tibial plateau measurements) [37]. Other sizing methods that have been investigated include MRI; three-dimensional CT; photographs of the transplant; and calculations based on patient height, weight, and gender [2, 32, 56, 57]. The problem is that radiographic techniques tend to overestimate meniscus size and MRI tends to underestimate size [32]. Jang et al. [22] assessed extrusion between transplants that were sized according to the Pollard method and transplants sized by this method and then reduced (in total size) by 5 %. These investigators reported a significant difference between these methods in the RPE (47 ± 17 and 35 ± 17 %, respectively; P = 0.03). However, there was no difference in absolute extrusion or between MMT and LMT in extrusion rates. Yoon et al. [56] reported improved accuracy in sizing of LMT from an anatomic study of 25 knees with their “modified Pollard method” equation. These authors recommended sizing LMT anatomic length as follows: 0.52 × plateau length (according to Pollard’s method) + 5.2 mm. This method increased the accuracy of radiographic measurements to actual anatomic tibial length value from 40 to 92 %. Surgeons should be aware that there are differences in radiographic sizing protocols among studies. This is especially true for the lateral meniscus, in which some studies take the entire lateral anteroposterior dimension of the tibial plateau [37], whereas others attempt to measure the most anterior lateral meniscus attachment [40].
The surgeon must be able to make adjustments at surgery for a graft that is larger than required. This is possible with MMT double-tunnel techniques by advancing the meniscus bone plug into the tunnel in the appropriate amount to prevent extrusion. A LMT that is oversized, even with a correct bone trough placement, is more difficult to correct. The anterior horn bone attachment may be advanced separately into an anterior bone tunnel. A second technique is to convert to a soft tissue attachment of the anterior horn of the LMT to the native lateral meniscus.
Most investigators use bone fixation in LMT and MMT in the belief that it provides superior fixation and will aid in preventing major extrusion. De Coninck et al. [14] and Abat et al. [1] performed the only studies (evidence level 3 and level 2, respectively) that directly compared extrusion in transplants inserted with bone tunnel fixation to those implanted with a soft tissue fixation technique. The transplants implanted with bone fixation were less extruded in both compartments. For instance, in De Coninck et al.’s [14] series, the extrusion of MMT implanted with soft tissue fixation was significantly larger than that of the bone fixation (4.71 and 2.36 mm, respectively, P = 0.003). In addition, there was a significantly greater percentage of knees that had >3 mm of radial displacement following soft tissue fixation compared with bone fixation of MMTs (100 and 14.4 %, respectively, P = 0.01).
A limitation of this review is that all studies except one were low evidence (levels 3–4) and several were retrospective [14, 18, 22–25, 28, 58, 59]. The lack of a clear, consistent definition of transplant extrusion precludes definitive conclusions, and it is hoped that future studies will address this issue. The short-term follow-up of most of the studies prevents any conclusion regarding the longer-term clinical relevance of transplant extrusion. The mixed cohorts in regard to concomitant operative procedures is another limitation. There is a potential limitation in that all of the MRI studies except two [35, 39] were conducted under non-weight-bearing conditions. The issue of whether a clinically significant difference exists in the amount of meniscus extrusion measured on a non-weight-bearing MRI versus a weight-bearing (loaded) MRI has not been resolved. It is difficult to perform MRI under loaded conditions, which requires special equipment or a vertically oriented scanner. Boxheimer et al. [6] reported that the differences in meniscus position, extrusion, and height were minimal between partially loaded and fully loaded conditions in 22 normal knees. Other investigators have reported changes in meniscus movement and extrusion [6, 7, 45], as well as cartilage matrix in the tibiofemoral joint [33], under loaded conditions. Stehling et al. [42] conducted 3T MRI evaluations on 10 healthy and 20 osteoarthritis knees under unloaded and partially loaded (50 % body weight) conditions. There was significantly greater meniscus extrusion measured under partially loaded conditions. The amount of meniscus extrusion measured in the studies in this systematic review may be smaller than that incurred under full weight-bearing conditions; however, the clinical relevance of the difference remains unclear at present.
Recommendations for future studies
The results of this review have led to the following recommendations for future studies. It would be useful for future studies to acquire a postoperative MRI early after meniscus transplantation in all patients when full weight-bearing has been resumed to determine the initial healing, height, width, and extent of extrusion. Then, a second MRI could be obtained at a defined time later to determine whether changes in meniscus characteristics occurred. In addition, studies should obtain MRIs at the same time period in all patients in a prospective manner to eliminate the high variability in timing found in this review.
From MRI data, investigators should report (1) absolute meniscus transplant extrusion, (2) relative percent of extrusion (using the width of the involved tibiofemoral compartment as the denominator), (3) percent coverage (percent of transplant located within the tibiofemoral compartment), and (4) percent of transplants in the cohort that were extruded. More sophisticated three-dimensional MRI modeling should be used when feasible to obtain these values. Extrusion assessments should include both the meniscus body and anterior and posterior horns. The condition of the articular cartilage in the involved tibiofemoral compartment at the time of transplantation should be reported using International Cartilage Repair Society grade, size, and location. Clinical rating scales should include those that assess both daily and sports activities and tibiofemoral joint pain. Investigators who desire to determine whether associations exist between transplant extrusion, and arthrosis grade progression should conduct these assessments when all patients are in the mid- to long-term postoperative time period (5–10 years).
Conclusions
Inconsistencies among the studies in this review prevent definitive conclusions regarding the incidence and clinical significance of meniscus transplant extrusion. Wide variability was found in the reported rates for the absolute millimeters of extrusion (0–8.8 mm), the relative percentage of extrusion (0–100 %), and the percent of transplants that were extruded (0–100 %). Correlations between transplant extrusion and clinical rating scales (for daily activities), joint space narrowing on posteroanterior radiographs, and arthrosis progression were inconclusive. Still, the short- to mid-term results were encouraging in regard to knee function with activities of daily living and low failure rates. A few authors reported that non-anatomic placement of lateral meniscus transplants and suture fixation of medial and lateral transplants were associated with greater extrusion. Even so, the issue of whether transplant fixation (and preservation) affects extrusion remains unresolved.
References
Abat F, Gelber PE, Erquicia JI et al (2012) Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med 40(7):1591–1596
Berhouet J, Marty F, Rosset P et al (2013) Meniscus matching: evaluation of direct anatomical, indirect radiographic, and photographic methods in 10 cadaver knees. Orthop Traumatol Surg Res 99(3):291–297
Berthiaume MJ, Raynauld JP, Martel-Pelletier J et al (2005) Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis 64(4):556–563
Bloecker K, Englund M, Wirth W et al (2011) Revision 1 size and position of the healthy meniscus, and its correlation with sex, height, weight, and bone area- a cross-sectional study. BMC Musculoskelet Disord 12:248
Bowers ME, Tung GA, Fleming BC et al (2007) Quantification of meniscal volume by segmentation of 3T magnetic resonance images. J Biomech 40(12):2811–2815
Boxheimer L, Lutz AM, Treiber K et al (2004) MR imaging of the knee: position related changes of the menisci in asymptomatic volunteers. Invest Radiol 39(5):254–263
Boxheimer L, Lutz AM, Zanetti M et al (2006) Characteristics of displaceable and nondisplaceable meniscal tears at kinematic MR imaging of the knee. Radiology 238(1):221–231
Bruns K, Svensson F, Turkiewicz A et al (2014) Meniscus body position and its change over four years in asymptomatic adults: a cohort study using data from the Osteoarthritis Initiative (OAI). BMC Musculoskelet Disord 15:32
Carter T, Economopoulos KJ (2013) Meniscal allograft shrinkage-MRI evaluation. J Knee Surg 26(3):167–171
Chen MI, Branch TP, Hutton WC (1996) Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy 12(2):174–181
Choi CJ, Choi YJ, Lee JJ et al (2010) Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy 26(12):1602–1606
Choi NH, Yoo SY, Victoroff BN (2011) Position of the bony bridge of lateral meniscal transplants can affect meniscal extrusion. Am J Sports Med 39(9):1955–1959
Crema MD, Roemer FW, Felson DT et al (2012) Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the multicenter osteoarthritis study. Radiology 264(2):494–503
De Coninck T, Huysse W, Verdonk R et al (2013) Open versus arthroscopic meniscus allograft transplantation: magnetic resonance imaging study of meniscal radial displacement. Arthroscopy 29(3):514–521
Donahue TL, Hull ML, Howell SM (2006) New algorithm for selecting meniscal allografts that best match the size and shape of the damaged meniscus. J Orthop Res 24(7):1535–1543
Elattar M, Dhollander A, Verdonk R et al (2011) Twenty-six years of meniscal allograft transplantation: is it still experimental? A meta-analysis of 44 trials. Knee Surg Sports Traumatol Arthrosc 19(2):147–157
Gonzalez-Lucena G, Gelber PE, Pelfort X et al (2010) Meniscal allograft transplantation without bone blocks: a 5- to 8-year follow-up of 33 patients. Arthroscopy 26(12):1633–1640
Ha JK, Shim JC, Kim DW et al (2010) Relationship between meniscal extrusion and various clinical findings after meniscus allograft transplantation. Am J Sports Med 38(12):2448–2455
Ha JK, Sung JH, Shim JC et al (2011) Medial meniscus allograft transplantation using a modified bone plug technique: clinical, radiologic, and arthroscopic results. Arthroscopy 27(7):944–950
Hergan D, Thut D, Sherman O et al (2011) Meniscal allograft transplantation. Arthroscopy 27(1):101–112
Huang A, Hull ML, Howell SM et al (2002) Identification of cross-sectional parameters of lateral meniscal allografts that predict tibial contact pressure in human cadaveric knees. J Biomech Eng 124(5):481–489
Jang SH, Kim JG, Ha JG et al (2011) Reducing the size of the meniscal allograft decreases the percentage of extrusion after meniscal allograft transplantation. Arthroscopy 27(7):914–922
Kim CW, Kim JM, Lee SH et al (2011) Results of isolated lateral meniscus allograft transplantation: focus on objective evaluations with magnetic resonance imaging. Am J Sports Med 39(9):1960–1967
Kim JM, Lee BS, Kim KH et al (2012) Results of meniscus allograft transplantation using bone fixation: 110 cases with objective evaluation. Am J Sports Med 40(5):1027–1034
Koh YG, Moon HK, Kim YC et al (2012) Comparison of medial and lateral meniscal transplantation with regard to extrusion of the allograft, and its correlation with clinical outcome. J Bone Joint Surg Br 94(2):190–193
Lee BS, Chung JW, Kim JM et al (2012) Morphologic changes in fresh-frozen meniscus allografts over 1 year: a prospective magnetic resonance imaging study on the width and thickness of transplants. Am J Sports Med 40(6):1384–1391
Lee DH, Kim JM, Lee BS et al (2012) Greater axial trough obliquity increases the risk of graft extrusion in lateral meniscus allograft transplantation. Am J Sports Med 40(7):1597–1605
Lee DH, Kim SB, Kim TH et al (2010) Midterm outcomes after meniscal allograft transplantation: comparison of cases with extrusion versus without extrusion. Am J Sports Med 38(2):247–254
Lee DH, Kim TH, Lee SH et al (2008) Evaluation of meniscus allograft transplantation with serial magnetic resonance imaging during the first postoperative year: focus on graft extrusion. Arthroscopy 24(10):1115–1121
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Magee T (2008) MR findings of meniscal extrusion correlated with arthroscopy. J Magn Reson Imaging 28(2):466–470
McConkey M, Lyon C, Bennett DL et al (2012) Radiographic sizing for meniscal transplantation using 3-D CT reconstruction. J Knee Surg 25(3):221–225
Nishii T, Kuroda K, Matsuoka Y et al (2008) Change in knee cartilage T2 in response to mechanical loading. J Magn Reson Imaging 28(1):175–180
Noyes FR, Barber-Westin SD (2005) Meniscus transplantation: indications, techniques, clinical outcomes. Instr Course Lect 54:341–353
Noyes FR, Barber-Westin SD, Rankin M (2004) Meniscal transplantation in symptomatic patients less than fifty years old. J Bone Joint Surg Am 86-A(7):1392–1404
Obremskey WT, Pappas N, Attallah-Wasif E et al (2005) Level of evidence in orthopaedic journals. J Bone Joint Surg Am 87(12):2632–2638
Pollard ME, Kang Q, Berg EE (1995) Radiographic sizing for meniscal transplantation. Arthroscopy 11(6):684–687
Potter HG, Rodeo SA, Wickiewicz TL et al (1996) MR imaging of meniscal allografts: correlation with clinical and arthroscopic outcomes. Radiology 198(2):509–514
Rankin M, Noyes FR, Barber-Westin SD et al (2006) Human meniscus allografts’ in vivo size and motion characteristics: magnetic resonance imaging assessment under weightbearing conditions. Am J Sports Med 34(1):98–107
Shaffer B, Kennedy S, Klimkiewicz J et al (2000) Preoperative sizing of meniscal allografts in meniscus transplantation. Am J Sports Med 28(4):524–533
Starke C, Kopf S, Grobel KH et al (2010) The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: a biomechanical study. Arthroscopy 26(3):358–365
Stehling C, Souza RB, Hellio Le Graverand MP et al (2012) Loading of the knee during 3.0T MRI is associated with significantly increased medial meniscus extrusion in mild and moderate osteoarthritis. Eur J Radiol 81(8):1839–1845
Stollsteimer GT, Shelton WR, Dukes A et al (2000) Meniscal allograft transplantation: a 1- to 5-year follow-up of 22 patients. Arthroscopy 16(4):343–347
Sugita T, Kawamata T, Ohnuma M et al (2001) Radial displacement of the medial meniscus in varus osteoarthritis of the knee. Clin Orthop Relat Res 387:171–177
Tibesku CO, Mastrokalos DS, Jagodzinski M et al (2004) MRI evaluation of meniscal movement and deformation in vivo under load bearing condition. Sportverletz Sportschaden 18(2):68–75
van Arkel ER, de Boer HH (2002) Survival analysis of human meniscal transplantations. J Bone Joint Surg Br 84(2):227–231
van Arkel ER, Goei R, de Ploeg I et al (2000) Meniscal allografts: evaluation with magnetic resonance imaging and correlation with arthroscopy. Arthroscopy 16(5):517–521
Verdonk P, Depaepe Y, Desmyter S et al (2004) Normal and transplanted lateral knee menisci: evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc 12(5):411–419
Verdonk PC, Demurie A, Almqvist KF et al. (2005) Transplantation of viable meniscal allograft. Survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am 87-A(4):715–724
Verdonk PC, Verstraete KL, Almqvist KF et al (2006) Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc 14(8):694–706
von Lewinski G, Kohn D, Wirth CJ et al (2008) The influence of nonanatomical insertion and incongruence of meniscal transplants on the articular cartilage in an ovine model. Am J Sports Med 36(5):841–850
Wenger A, Wirth W, Hudelmaier M et al (2013) Meniscus body position, size, and shape in persons with and persons without radiographic knee osteoarthritis: quantitative analyses of knee magnetic resonance images from the osteoarthritis initiative. Arthritis Rheum 65(7):1804–1811
Wirth W, Frobell RB, Souza RB et al (2010) A three-dimensional quantitative method to measure meniscus shape, position, and signal intensity using MR images: a pilot study and preliminary results in knee osteoarthritis. Magn Reson Med 63(5):1162–1171
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85-A (1):1–3
Yoon JR, Kim TS, Lee YM et al (2011) Transpatellar approach in lateral meniscal allograft transplantation using the keyhole method: can we prevent graft extrusion? Knee Surg Sports Traumatol Arthrosc 19(2):214–217
Yoon JR, Kim TS, Lim HC et al (2011) Is radiographic measurement of bony landmarks reliable for lateral meniscal sizing? Am J Sports Med 39(3):582–589
Yoon JR, Kim TS, Wang JH et al (2011) Importance of independent measurement of width and length of lateral meniscus during preoperative sizing for meniscal allograft transplantation. Am J Sports Med 39(7):1541–1547
Yoon KH, Lee SH, Park SY et al (2014) Meniscus allograft transplantation: a comparison of medial and lateral procedures. Am J Sports Med 42(1):200–207
Zhang H, Liu X, Wei Y et al (2012) Meniscal allograft transplantation in isolated and combined surgery. Knee Surg Sports Traumatol Arthrosc 20(2):281–289
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Noyes, F.R., Barber-Westin, S.D. A systematic review of the incidence and clinical significance of postoperative meniscus transplant extrusion. Knee Surg Sports Traumatol Arthrosc 23, 290–302 (2015). https://doi.org/10.1007/s00167-014-3329-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3329-2