Abstract
Purpose
(1) To investigate whether an increased lateral meniscal slope measured on magnetic resonance image (MRI) would be associated with greater risk of bone contusions in noncontact anterior cruciate ligament injury, and (2) to measure the relationship between the occurrence of bone contusions and associated findings observed in ACL deficient knees such as cartilage damage, anterolateral complex injury and concomitant meniscal tears.
Method
Patients who underwent ACL reconstruction surgery between 2013 and 2018 were retrospectively reviewed. Sixty-three patients were included in the study group (ACL + bone contusions group), 56 participants were in the control group (isolated ACL group). The presence and severity of bone contusions were determined from preoperative MRIs. The lateral meniscal slope and lateral posterior tibial slope were measured on the MRIs in a blinded fashion. The predictors of lateral bone contusions including age, sex, body mass index, lateral meniscal slope and lateral posterior tibial slope were examined by multivariable logistic regression. Associated findings including concomitant meniscal lesions, intra-articular cartilage damage and anterolateral complex injury, which were also calculated by multivariable logistic regression.
Results
The mean lateral meniscal slope in the study group was 6.5° ± 3.5°, which was significantly larger than that in the control group (3.8° ± 2.7°; P < 0.01). In addition, increased lateral meniscal slope was significantly associated with lateral bone contusions in noncontact ACL injury (Lateral femoral condyle (LFC): AOR 16.5; 95% CI 5.40–50.20; P < 0.01; Lateral tibial plateau (LTP): AOR 31.8; 95% CI 8.68–116.7; P < 0.01). However, lateral posterior tibial slope was not significantly associated with bone contusions. Moreover, the presence of lateral bone contusions was associated with concomitant lateral meniscal tears (OR 12.4; 95% CI 3.30–46.30) and cartilage damage (OR 2.9; 95% CI 1.04–8.18).
Conclusion
An increased lateral meniscal slope was associated with increased risk of lateral bone contusions in noncontact ACL injury. In addition, the presence of lateral bone contusions was associated with intra-articular cartilage damage, anterolateral complex injury and concomitant meniscal tears. Hence, additional information was provided for counseling patients who have increased LMS on the greater risk of knee rotational instability and identify patients undergoing ACL reconstruction who may benefit from extra-articular tenodesis.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Noncontact anterior cruciate ligament (ACL) injuries account for almost three quarters of all ACL injuries observed clinically and previous studies have proposed different theories and risk factors [2]. Several associated injuries such as anterolateral ligament (part of anterolateral complex) injury and bone contusions may help us better understand the mechanism of injury and thus optimize prevention strategies [28, 30, 31, 41].
Bone contusions are present in up to 80% of ACL ruptures [9], which are observed by MRI as trabecular bone marrow edema [3, 5, 12, 18, 37]. The most common bone bruise site is on the lateral femoral condyle (LFC) at the sulcus terminalis and posterior lateral tibial plateau (LTP) [26]. The injury results from a pivot-shift like mechanism, which is characterized by anterior subluxation of the lateral tibial plateau on the femoral condyle [19, 25]. In addition, severe bone contusions are suggested to be an indicator of early degenerative changes in the knee [23, 36]. However, the exact mechanism and risk factors for bone contusions still remain unknown.
The posterior tibial slope (PTS) of the bony tibial plateaus frequently is mentioned for its association to noncontact ACL injury. It is defined by a tangent line to the respective tibial plateau and a line perpendicular to the longitudinal axis of the tibial bone. Prior studies have suggested that in ACL ruptured knees, every 10 degree increase of PTS results in 6 mm of anterior tibial translation [7]. Song et al. [31] have shown that increased PTS was connected to high-grade pivot-shift, which is the injury mechanism for lateral bone contusions in ACL rupture. However, the relation of tibial slope and ACL rupture, together with its associated injuries remains controversial [10, 39]. This lack of consensus may be attributed to the use of bony tissue to define the tibial slope [16]. Some investigators have claimed that the assessment of meniscal slope was more accurate since it might represent the true surface of the tibia [21, 34]. Therefore, the lateral meniscal slope (LMS) will potentially be a more accurate assessment of the relationship between the tibia and the femur in the lateral compartment of the knee [8].
Thus, an increased LMS as measured on MRI is hypothesized to be correlated with the occurrence of bone contusions in noncontact ACL injury. The aim of the current study was to investigate the relationship between LMS and bone contusions in noncontact ACL ruptured knee. The secondary objective was to measure the relationship between the occurrence of bone contusions and different signs observed in ACL deficient knees such as cartilage damage, ALL injury and concomitant meniscal tears.
Materials and methods
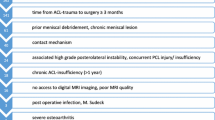
A retrospective case–control study was performed on 563 patients who underwent ACL reconstruction between 2013 and 2018. Patients were selected through our computer-based patient record system. Both medical records and operation records were reviewed to determine if inclusion criteria were present: primary ACL reconstruction relative to a lesion resulting from a noncontact mechanism. If the mechanism of injury was not described in detail in the medical records, the patient would be interviewed by telephone to obtain the required information. Patients were excluded if they (1) did not have lateral bone contusions; (2) had partial ACL injury; (3) had a history of knee surgery on the affected side; (4) had combined ligament injuries including PCL injury, MCL injury or PLC injury; (5) had severe degeneration of cartilage > grade 2 according to Kellgren-Lawrence grading system; (6) had severe malalignment of the lower limb or (7) had general joint laxity. Demographic data including gender, age, side, BMI and follow-up time were recorded. The flow chart of patient selection is presented in Fig. 1.
Preoperative evaluation
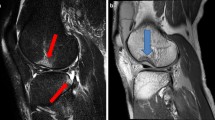
The medical history, physical examinations, demographic data including age and sex were retrospectively reviewed. A sports medicine-trained orthopedic surgeon and a radiologist specialized in musculoskeletal imaging independently reviewed the preoperative MRI and were blinded to the results found by other observers. The sagittal, coronal and axial sequences with T1 and T2 phases of MRI were included in the protocol. Fat suppressed sequence was utilized to evaluate the presence and severity of bone contusions on the lateral femoral condyle (LFC) and lateral tibial plateau (LTP). The severity of bone contusions was defined as none, minimal, moderate and severe, using the International Cartilage Repair Society (ICRS) grading system [4] (Fig. 2).
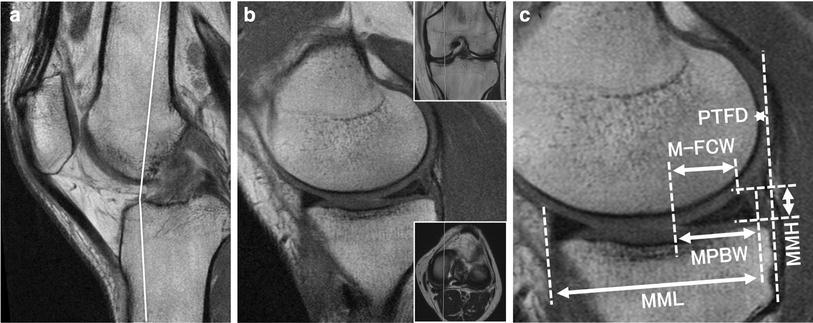
The previously utilized method [16, 17] was conducted to measure the lateral meniscal slope (LMS) and lateral posterior tibial slope (LPTS) preoperatively in MRI scans: The first step was to define the central sagittal slice, which consisted of attachment of the posterior cruciate ligament (PCL) and the intercondylar eminence. The second step was to draw two circles, the first circle was tangent to the anterior, posterior and proximal borders of the tibia and the second circle was centered on the perimeter of the first circle. Thus, the longitudinal axis is defined as the line connecting the two centers of the circles (Fig. 3a). The last step was to measure the angle between the line perpendicular to the tibial longitudinal axis and the tangent to the lateral bony tibial plateau and lateral meniscal borders (Fig. 3b, c). The tangent to the lateral meniscal borders was defined as the line connecting the superior anterior and posterior meniscal borders on the middle slice between the most medial slice and the central sagittal slice.
a The central sagittal slice consisted of attachment of the posterior cruciate ligament (PCL) and the intercondylar eminence, the longitudinal axis is defined as the line connecting the two centers of the circles. b Measurement of the angle between the line perpendicular to the tibial longitudinal axis and the tangent to the lateral meniscal borders. c Measurement of the angle between the line perpendicular to the tibial longitudinal axis and the tangent to the lateral bony tibial plateau
An examination of ALL status was conducted on T2 weighted coronal plane, normally, the ALL could be seen starting from the lateral epicondyle of the distal femur, going obliquely to the proximal tibia between Gerdy’s tubercle and fibula head [30].
Intraoperative assessment
All the meniscal tears, intra-articular cartilage damage and other abnormalities were documented using the images and videos recorded during surgery. Meniscal tears were evaluated according to ISAKOS classification [38]. Cartilage degradation was evaluated according to Outerbridge classification [24].
This study was approved by the institutional review board of the First Affiliated Hospital of Chongqing Medical University (IRB approval number: 2017-108).
Statistical analysis
Outliers were checked, then corrected or excluded before statistical analysis. A sample size calculation was performed using the formula for difference in means in case–control study. Standard deviation (σ) of LMS in samples was set as 4, difference between case and control group was 2.5, 80% power, 0.05 significance level and equal number of case and control group, the sample size should be 41 in each group. So, the sample size in our study with 63 cases and 56 controls was ample to discover the difference between two groups.
In this study, descriptive data were calculated for LMS, LPTS, bone contusions and demographic data. The population was divided into two groups according to the presence of bone contusions. An intraclass correlation coefficient (ICC) was used to evaluate the reliability of measurement performance. ICC value > 0.9 were considered excellent, values of 0.8–0.9 indicated good reliability. The inter-observer ICCs were 0.92 for the severity of bone contusions at LFC and LTP and 0.82 for ALL status. The inter-observer ICCs were 0.9 and 0.87 for LPTS and LMS, suggesting a good reliability.
Pearson Chi square test or Fisher exact test were used to compare categorical variables and Student t test was utilized to compare continuous variables. The predictors of lateral bone contusions (LFC, LTP or both) including age, gender, BMI LMS, LPTS and associated findings including meniscal lesion and cartilage damage were examined by multivariable logistic regression.
Currently there is not an established criterion for the abnormal value of LMS and LPTS, thus, the mean and SD of the control group were calculated and ≥ 1 SD from the mean was considered abnormal (≥ 6.52 for LMS; ≥ 10.36 for LPTS). Odds ratio (OR) or adjusted OR (AOR) and 95% confidence interval (CI) were computed. P < 0.05 was considered statistically significant. Analyses were conducted using SAS 9.4 (Cary, NC, USA).
Results
Descriptive statistics
The mean LMS in the study group was 6.5 ± 3.5 and mean LMS in the control group was 3.8 ± 2.7 (P < 0.01). The incidence of cartilage damage, ALL abnormality and concomitant meniscal tears were also significantly higher in the study group than in the control group (Table 1). In addition, there were more males in the study group. Whereas, age, LPTS, and BMI were similar between groups.
Relationship between LMS/LPTS and bone contusions
The multivariable logistic regression analysis for predictors of the presence of bone contusions was presented in Table 2. The LMS was found to be significantly correlated with bone contusions (AOR 7.0; 95% CI 2.42–20.0). In addition, further analysis showed that the LMS (LFC: AOR 16.5; 95% CI 5.40–50.20; P < 0.01; LTP: AOR 31.8; 95% CI 8.68–116.7; P < 0.01) was an independent risk factor of lateral bone contusions (LFC and LTP). However, LPTS was not found to be associated with bone contusions.
The severity of bone contusions was further analyzed by multivariable logistic regression. Only LMS was found to be significantly associated with the moderate/severe lateral bone contusions (LFC: AOR 12.2; 95% CI 2.59–57.5; P < 0.01; LTP: AOR 23.4; 95% CI 5.88–93.4; P < 0.01), whereas LPTS, BMI, age and gender were not.
Associate findings with the presence of bone contusions
Multivariable logistic regression was used for the presence of bone contusions of the knee. The multivariable logistic regression analysis (Table 3) reveals that lateral bone contusions was significantly associated with concomitant lateral meniscal lesions (OR 2.0; 95% CI 3.30–46.3) and anterolateral complex injury (OR 53.5; 95% CI 12.47–229.50). Both lateral and medial bone contusions (OR 2.9; 95% CI 1.04–8.18; OR 3.1; 95% CI 1.11–8.80) were found to be significantly associated with cartilage injury.
Discussion
The main findings in the current work were: First, patients in the study group (ACL injuries + bone contusions) showed significantly increased LMS, more cartilage damage and concomitant meniscal tears especially lateral meniscal tears than in the control group (Isolated ACL injuries). Second, increased LMS was further demonstrated by multivariable logistic regression to be an independent risk factor for both the presence and severity of lateral bone contusions, whereas, LPTS, BMI and age were not. Third, bone contusions were significantly correlated with cartilage damage.
Bone contusions detected by MRI have gained increasing interest since their first description [40]. ACL rupture has long been suggested to be correlated with early occurrence of degenerative osteoarthritis, which was originally explained by abnormal knee kinematics and ligament insufficiency. However, recent studies have indicated that even after ACL reconstruction, many of these patients will develop degenerative changes in less than 10 years [6, 11, 22]. These results showed that the occurrence of early degenerative arthritis have some other predisposing factors such as intra-articular cartilage damage and bone contusions. In addition, the location of bone contusions was always specific to the injured ligament, thus investigating bone bruise location could be essential to help orthopaedic surgeons better understand the mechanism of ligament injury [14, 20, 33]. On the basis of these findings, Speer et al. [32] suggested a pivot-shift like injury of the femoral condyle and posterolateral tibial rim. However, to our knowledge, the exact mechanism and risk factors for lateral bone contusions still remain unknown. When a pivot-shift like movement occurs, the tibia translates anteriorly and internally rotates, the lateral femoral condyle moves posteriorly and subluxation occurs. In addition to bone contusions, this movement could result in damages on several structures like ALL and lateral meniscus, which are rotational stabilizers of the knee. Thus, bone contusions may serve as a bridge between LMS/LPTS and rotational instability. Previously, studies have shown that the ALL could be observed on MRI and ultrasound, making ALL evaluation possible [15, 27]. Song et al. [30] has indicated several associated findings of bone contusions in patients with ACL injury including high grade pivot-shift, concomitant lateral meniscal tear and ALL abnormality. These findings are yet to be verified but they could help us better understand that pivot-shift like mechanism of ACL injury could imply a series of injuries occurred not only on ACL but also the lateral meniscus, ALL, cartilage damage and bone contusions.
Previously, an increased LPTS as measured on MRI has been regarded as a risk factor for ACL injury in the native knee [1]. It has been suggested that with increased LPTS, the ACL will suffer from greater loading and thus, injury could more easily happen [13]. However, recent studies have suggested that tibial slope measurement should not be conducted using the bony tissue [8, 21, 34]. The soft tissue such as meniscus and cartilage on the tibial plateau may more accurately reflect the true surface of tibia and thus play a crucial role in controlling the anterior translation of the tibia in the ACL ruptured knee [35]. Currently, it is still too early to indicate that the decision to perform HTO in patients with ACL injury should be made based on LPTS or LMS, but due to the discrepancy of different results, considering both as a reference may be a better choice. When lateral bone contusions occur, the lateral femoral condyle often moves posteriorly to impact on the posterolateral part of the tibia including the posterior horn of the lateral meniscus. A previous study has suggested the association between increased medial meniscal slope and medial meniscal ramp lesions in noncontact ACL injury patients [29]. When the menisci are unable to serve as a secondary stabilizer, the pivot-shift like movement easily happens and thus lateral bone contusions occur [30]. However, whether the LPTS or LMS is an independent risk factor of lateral bone contusions still remains unclear. This study showed that LMS, rather than LPTS was significantly increased in the study group (ACL injuries + bone contusions) than in the control group (isolated ACL injuries), moreover, only increased LMS was demonstrated by multivariable logistic regression to be strongly correlated with both the presence and severity of lateral bone contusions, which indicated that only LMS, rather than LPTS, was an independent risk factor.
Understanding of the anatomic predictors and associated injuries of bone contusions might help us better evaluate the ACL injury. Patients who have increased LMS might be of greater risk of concomitant bone contusions, especially lateral bone contusions, and early occurrence of degenerative arthritis. Increased LMS was indicated in this study to correlate with higher prevalence of lateral bone contusions, which could be associated with concomitant meniscal tear and intra-articular cartilage damage.
MRI was used to visualize the true surface geometry of the tibio-femoral articulation in this study. In addition, high inter-observer ICCs in MRI measurement of LMS and LPTS indicated good reliability. However, limitations still exist. First, this is a retrospective case–control study. Second, a larger sample size would strengthen this study and provide insights into other associated findings although a sample size calculation was performed and it showed that our study with 63 cases and 56 controls was ample to discover the difference between two groups. Third, patients in the study group were not matched by age and sex to control group participants and there were more males in the study group. This could be explained by the fact that males are more involved in physically demanding sports and thus, severe injury could more easily happen in males.
To our knowledge, this is the first study focusing on correlation between increased LMS and lateral bone contusions in patients with noncontact ACL injuries. The lateral bone contusions associated with ACL injury were multifactorial and several factors should be taken into account. This could help orthopaedic surgeons in identifying susceptible individuals who may experience greater benefit from targeted ACL injury-prevention counseling and intervention. In addition, since higher LMS, ALL injury, bone contusions are risk factors for rotational instability after ACL injury, this study would help to identify patients undergoing ACL reconstruction who may benefit from additional surgical procedures such as extra-articular tenodesis.
Conclusion
An increased LMS was associated with and could be an independent risk factor for lateral bone contusions in noncontact ACL injury. In addition, the presence of lateral bone contusions is associated with intra-articular cartilage damage, ALL injury and concomitant meniscal tears. These factors above should be considered by orthopedic surgeons as part of the preoperative evaluation of patients with ACL injury.
References
Bisson LJ, Gurske-DePerio J (2010) Axial and sagittal knee geometry as a risk factor for noncontact anterior cruciate ligament tear: a case-control study. Arthroscopy 26(7):901–906
Boden BP, Dean GS, Feagin JA Jr, Garrett WE Jr (2000) Mechanisms of anterior cruciate ligament injury. Orthopedics 23(6):573–578
Bretlau T, Tuxoe J, Larsen L, Jorgensen U, Thomsen HS, Lausten GS (2002) Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc 10(2):96–101
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85A(Suppl 2):58–69
Costa-Paz M, Muscolo DL, Ayerza M, Makino A, Aponte-Tinao L (2001) Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy 17(5):445–449
Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR (1994) Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med 22(5):632–644
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br 76(5):745–749
Elmansori A, Lording T, Dumas R, Elmajri K, Neyret P, Lustig S (2017) Proximal tibial bony and meniscal slopes are higher in ACL injured subjects than controls: a comparative MRI study. Knee Surg Sports Traumatol Arthrosc 25(5):1598–1605
Faber KJ, Dill JR, Amendola A, Thain L, Spouge A, Fowler PJ (1999) Occult osteochondral lesions after anterior cruciate ligament rupture. Six-year magnetic resonance imaging follow-up study. Am J Sports Med 27(4):489–494
Feucht MJ, Mauro CS, Brucker PU, Imhoff AB, Hinterwimmer S (2013) The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 21(1):134–145
Fithian DC, Paxton EW, Stone ML, Luetzow WF, Csintalan RP, Phelan D, Daniel DM (2005) Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am J Sports Med 33(3):335–346
Frobell RB (2011) Change in cartilage thickness, posttraumatic bone marrow lesions, and joint fluid volumes after acute ACL disruption: a two-year prospective MRI study of sixty-one subjects. J Bone Joint Surg Am 93(12):1096–1103
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32(2):376–382
Graf BK, Cook DA, De Smet AA, Keene JS (1993) “Bone bruises” on magnetic resonance imaging evaluation of anterior cruciate ligament injuries. Am J Sports Med 21(2):220–223
Helito CP, Helito PVP, Leao RV, Demange MK, Bordalo-Rodrigues M (2017) Anterolateral ligament abnormalities are associated with peripheral ligament and osseous injuries in acute ruptures of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 25(4):1140–1148
Hudek R, Fuchs B, Regenfelder F, Koch PP (2011) Is noncontact ACL injury associated with the posterior tibial and meniscal slope? Clin Orthop Relat Res 469(8):2377–2384
Illingworth KD, Hensler D, Casagranda B, Borrero C, van Eck CF, Fu FH (2014) Relationship between bone bruise volume and the presence of meniscal tears in acute anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc 22(9):2181–2186
Johnson DL, Urban WP Jr, Caborn DN, Vanarthos WJ, Carlson CS (1998) Articular cartilage changes seen with magnetic resonance imaging-detected bone bruises associated with acute anterior cruciate ligament rupture. Am J Sports Med 26(3):409–414
Kim SY, Spritzer CE, Utturkar GM, Toth AP, Garrett WE, DeFrate LE (2015) Knee kinematics during noncontact anterior cruciate ligament injury as determined from bone bruise location. Am J Sports Med 43(10):2515–2521
Krosshaug T, Andersen TE, Olsen OE, Myklebust G, Bahr R (2005) Research approaches to describe the mechanisms of injuries in sport: limitations and possibilities. Br J Sports Med 39(6):330–339
Lustig S, Scholes CJ, Leo SP, Coolican M, Parker DA (2013) Influence of soft tissues on the proximal bony tibial slope measured with two-dimensional MRI. Knee Surg Sports Traumatol Arthrosc 21(2):372–379
Myklebust G, Holm I, Maehlum S, Engebretsen L, Bahr R (2003) Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury: a follow-up study. Am J Sports Med 31(6):981–989
Nakamae A, Engebretsen L, Bahr R, Krosshaug T, Ochi M (2006) Natural history of bone bruises after acute knee injury: clinical outcome and histopathological findings. Knee Surg Sports Traumatol Arthrosc 14(12):1252–1258
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43:752–757
Papalia R, Torre G, Vasta S, Zampogna B, Pedersen DR, Denaro V, Amendola A (2015) Bone bruises in anterior cruciate ligament injured knee and long-term outcomes. A review of the evidence. Open Access J Sports Med 6:37–48
Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE (2014) Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports Med 44(2):281–293
Puzzitiello RN, Agarwalla A, Zuke WA, Garcia GH, Forsythe B (2018) Imaging diagnosis of injury to the anterolateral ligament in patients with anterior cruciate ligaments: association of anterolateral ligament injury with other types of knee pathology and grade of pivot-shift examination: a systematic review. Arthroscopy 34(9):2728–2738
Shaikh H, Herbst E, Rahnemai-Azar AA, Bottene Villa Albers M, Naendrup JH, Musahl V, Irrgang JJ, Fu FH (2017) The segond fracture is an avulsion of the anterolateral complex. Am J Sports Med 45(10):2247–2252
Song GY, Liu X, Zhang H, Wang QQ, Zhang J, Li Y, Feng H (2016) Increased medial meniscal slope is associated with greater risk of ramp lesion in noncontact anterior cruciate ligament injury. Am J Sports Med 44(8):2039–2046
Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H (2016) Bone contusions after acute noncontact anterior cruciate ligament injury are associated with knee joint laxity, concomitant meniscal lesions, and anterolateral ligament abnormality. Arthroscopy 32(11):2331–2341
Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H (2016) Risk factors associated with grade 3 pivot shift after acute anterior cruciate ligament injuries. Am J Sports Med 44(2):362–369
Speer KP, Spritzer CE, Bassett FH 3rd, Feagin JA Jr, Garrett WE Jr (1992) Osseous injury associated with acute tears of the anterior cruciate ligament. Am J Sports Med 20(4):382–389
Speer KP, Warren RF, Wickiewicz TL, Horowitz L, Henderson L (1995) Observations on the injury mechanism of anterior cruciate ligament tears in skiers. Am J Sports Med 23(1):77–81
Sturnick DR, Vacek PM, DeSarno MJ, Gardner-Morse MG, Tourville TW, Slauterbeck JR, Johnson RJ, Shultz SJ, Beynnon BD (2015) Combined anatomic factors predicting risk of anterior cruciate ligament injury for males and females. Am J Sports Med 43(4):839–847
Sturnick DR, Van Gorder R, Vacek PM, DeSarno MJ, Gardner-Morse MG, Tourville TW, Slauterbeck JR, Johnson RJ, Shultz SJ, Beynnon BD (2014) Tibial articular cartilage and meniscus geometries combine to influence female risk of anterior cruciate ligament injury. J Orthop Res 32(11):1487–1494
Szkopek K, Warming T, Neergaard K, Jorgensen HL, Christensen HE, Krogsgaard M (2012) Pain and knee function in relation to degree of bone bruise after acute anterior cruciate ligament rupture. Scand J Med Sci Sports 22(5):635–642
Theologis AA, Kuo D, Cheng J, Bolbos RI, Carballido-Gamio J, Ma CB, Li X (2011) Evaluation of bone bruises and associated cartilage in anterior cruciate ligament-injured and -reconstructed knees using quantitative t(1rho) magnetic resonance imaging: 1-year cohort study. Arthroscopy 27(1):65–76
Wadhwa V, Omar H, Coyner K, Khazzam M, Robertson W, Chhabra A (2016) ISAKOS classification of meniscal tears-illustration on 2D and 3D isotropic spin echo MR imaging. Eur J Radiol 85(1):15–24
Wordeman SC, Quatman CE, Kaeding CC, Hewett TE (2012) In vivo evidence for tibial plateau slope as a risk factor for anterior cruciate ligament injury: a systematic review and meta-analysis. Am J Sports Med 40(7):1673–1681
Yao L, Lee JK (1988) Occult intraosseous fracture: detection with MR imaging. Radiology 167(3):749–751
Yu B, Garrett WE (2007) Mechanisms of non-contact ACL injuries. Br J Sports Med 41(Suppl 1):i47–i51
Funding
This work is funded by the National Natural Science Foundation of China (NO.81902293) (K.L).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no competing interests exist.
Ethical approval
This study was approved by the institutional review board of the First Ailiated Hospital of Chongqing Medical University (IRB approval number: 2017-108).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, K., Li, J., Zheng, X. et al. Increased lateral meniscal slope is associated with greater incidence of lateral bone contusions in noncontact ACL injury. Knee Surg Sports Traumatol Arthrosc 28, 2000–2008 (2020). https://doi.org/10.1007/s00167-019-05724-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05724-8