Abstract
Purpose
This study evaluated the repair integrity and patient clinical outcomes following arthroscopic rotator cuff repair of medium to large rotator cuff tears using a single-row technique consisting of medially based, triple-loaded anchors augmented with bone marrow vents in the rotator cuff footprint lateral to the repair.
Methods
This is a retrospective study of 52 patients (53 shoulders) comprising 36 males and 16 females with a median age of 62 (range 44–82) with more than 24-month follow-up, tears between 2 and 4 cm in the anterior–posterior dimension and utilizing triple-loaded anchors. Mann–Whitney test compared Western Ontario Rotator Cuff (WORC) outcome scores between patients with healed and re-torn cuff repairs. Multivariate logistic regression analysed association of variables with healing status and WORC score. Cuff integrity was assessed on MRI, read by a musculoskeletal fellowship-trained radiologist.
Results
Magnetic resonance imaging (MRI) demonstrated an intact repair in 48 of 53 shoulders (91%). The overall median WORC score was 95.7 (range 27.6–100.0). A significant difference in WORC scores were seen between patients with healed repairs 96.7 (range 56.7–100.0) compared with a re-tear 64.6 (27.6–73.8), p < 0.00056.
Conclusions
Arthroscopic repair of medium to large rotator cuff tears using a triple-loaded single-row repair augmented with bone marrow vents resulted in a 91% healing rate by MRI and excellent patient reported clinical outcomes comparable to similar reported results in the literature.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Symptomatic rotator cuff tears are common in the active ageing population, and recent clinical results of arthroscopic rotator cuff repair have been promising [25, 29, 42]. However, achieving consistent radiologic healing of full-thickness rotator cuff tears remains a challenge, with re-tear rates ranging from 20 to 94% [5, 15, 24, 60]. Both patient- and surgeon-related factors variably affect healing after rotator cuff repair [3, 15, 19, 24, 44, 56, 62]. Patient-related factors include advancing age, chronicity of symptoms, amount of fatty infiltration and tear size, amongst others [3, 19, 24, 44, 62]. Two factors controlled by the surgeon are the surgical construct and the tension of the repaired muscle–tendon unit [19, 35]. The detrimental effects of excess tension on cuff repairs have long been recognized, although few studies have directly evaluated these effects [19, 21, 22].
Recent biomechanical research has focused on repair designs to improve rotator cuff tendon repair strength and healing rates. These efforts have led to the development of various single-row (SR) and double-row (DR) techniques, including the transosseous equivalent (TOE) technique which reestablishes tendon contact to the entire footprint by advancing the torn rotator cuff tendon towards the lateral margin of the greater tuberosity. Several biomechanical studies have demonstrated the TOE technique provides the strongest biomechanical fixation [46, 51, 52, 54]. Despite these developments, the literature continues to report suboptimal healing rates regardless of technique, especially for larger tears with recent studies reporting healing rates from 68 to 88% for SR, DR and TOE repairs (Table 1) [5, 24].
The senior surgeons at our institution developed a novel technique eschewing use of more anchors to overcome the biomechanical and biological challenges of rotator cuff repair by minimizing repair tension and maximizing repair strength. This technique consists of a medialized SR repair with triple-loaded suture anchors with bone marrow vents in the lateral cuff footprint. These vents enhance the healing biological milieu with bone marrow growth factors, platelets and mesenchymal stem cells. This technique has been utilized at our institution for over a decade with excellent clinical results.
The study’s purpose was to evaluate the repair integrity and clinical outcomes of a consecutive series of patients with medium to large RCTs treated arthroscopically with this novel single-row technique. The clinical and MRI results were hypothesized to be superior to recent results in the literature for similar-sized rotator cuff tears treated with other constructs.
Materials and methods
A retrospective review of our institutional database identified all patients who underwent arthroscopic rotator cuff repair over a 24-month period, from 2008 to 2010. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The inclusion criteria were as follows:
-
1.
Symptomatic rotator cuff tear failing non-operative therapy including 6-week physical therapy, non-steroidal anti-inflammatories and activity modification
-
2.
Rotator cuff tear between 2 and 4 cm in anterior to posterior (AP) dimension measured at time of arthroscopy
-
3.
Novel SR arthroscopic repair with medialized placement of two or three polyethylether ketone (PEEK) anchors triple-loaded with high strength suture (Healix, Depuy Mitek, Raynham, MA) and adjacent bone marrow vents
-
4.
Minimum 24-month follow-up
-
5.
Surgery performed by one of two senior authors
The exclusion criteria were as follows:
-
1.
Revision rotator cuff repair
-
2.
Tears requiring interval slides and/or margin convergence sutures
-
3.
Tears requiring anchor fixation of the subscapularis tendon
-
4.
Irreparable tears
-
5.
Inability to tolerate repeat MRI imaging despite PO sedation
Figure 1 displays the results of our retrospective database review. Fifty-eight patients were identified; 6 declined to participate or could not be reached, leaving a final study group of 52 patients (90% follow-up). The median age was 62 (range 44–82), with 36 male and 16 female patients. The median tear size was 3.0 cm (range 2.0–4.0) as determined intraoperatively from anterior to posterior at the medial cuff footprint as visualized from the lateral portal. The cuff tears were repaired with use of a median of 2 anchors (range 2–3). Chronic degenerative and acute on chronic rotator cuff tears are more common within this study’s age group; however, younger patients with acute tears were included as well. While most tolerated a repeat MRI, some patients were excluded due to claustrophobia despite PO medication.
All procedures were performed under general anaesthesia in the lateral decubitus position with the arm in balanced skeletal suspension. Standard diagnostic arthroscopy of the glenohumeral and subacromial spaces was performed. Concomitant pathology was identified and treated (Table 2). Subacromial decompression was performed if signs of coracoacromial ligament undersurface mechanical abrasion were present. The rotator cuff tendon was debrided to a stable edge, and anatomic footprint soft tissues were debrided to bare bone. The tear pattern and size was arthroscopically assessed from the lateral portal as previously described [9].
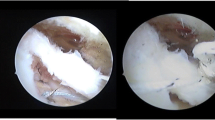
During repair, the arm was placed in 45 degrees of abduction and neutral rotation. Two to three anchors triple-loaded with high strength suture (Healix PEEK Anchors with Orthocord Suture, Depuy Mitek, Raynham, MA) were used at surgeon discretion based upon tear size and pattern. Anchors were inserted into the prepared bone at the previously described deadman angle, roughly 3 mm lateral to the articular cartilage for a medialized single-row construct [7]. Prior to tendon repair, 7–9 bone marrow vents 5–7 mm deep were created in the lateral tuberosity footprint with a 1.9 mm bone punch (MiniRevo punch, Linvatec, Key Largo FL) (Fig. 2). The vents are of sufficient size and depth to permit clinically observable release of marrow fat droplets and blood with reduced pump pressure. After surgery, these vents allow egress of blood containing bone marrow elements to improve local biological healing milieu (Fig. 2). Rotator cuff repair was performed utilizing a standard shuttle technique with the three sutures passed as simple stitches in a “fan-like” array [9]. All sutures were tied with locking sliding knots placed over the cuff and followed by three reverse half-hitches on alternating posts.
Arthroscopic view of completed medialized repair with bone marrow vents in the lateral rotator cuff footprint and Crimson Duvet. Arthroscopic view of a completed medialized repair viewed from lateral portal. a Black line arrows point to fan-like array of sutures from a triple-loaded anchor placed on medial boarder of rotator cuff footprint. Black block arrow identifies a bone marrow vent created by a MiniRevo punch (Linvatec, Key Largo FL) in the lateral cuff footprint, white block arrow. b Reducing pump pressure demonstrates blood flowing from the bone marrow vents. c Final view showing the “Crimson Duvet” with blood covering the rotator cuff repair and footprint on greater tuberosity
Postoperatively, all patients were immobilized in a neutral rotation sling (Ultra Sling III, DonJoy Orthopaedics, Inc, Carlsbad, CA) for 4–5 weeks. All patients followed a standardized, supervised physiotherapy programme beginning on postoperative day one with active elbow, wrist, and hand exercises as well as shoulder shrugs followed by passive supine external rotation and pendulum exercises after the first week. Strengthening was initiated at 8 weeks, and patients were allowed to resume full, unrestricted activities at 16–20 weeks.
Magnetic resonance imaging was performed on a single 1.5 Tesla MRI scanner at our institution (Fig. 3). An independent and blinded fellowship-trained musculoskeletal radiologist interpreted all scans. Repairs were graded according to the criteria published by Sugaya et al. as either “healed” (types I–III) or “re-torn” (types IV–V) (Table 3). In addition, re-torn cuffs were categorized by the criteria published by Cho et al. with type 1 having no repaired cuff tissue attached to the tuberosity and type 2 with a remnant of repaired cuff tissue remaining on the tuberosity [12, 58].
Comparison of preoperative and postoperative MRI scans. a Preoperative coronal MRI of a left shoulder showing a full-thickness rotator cuff tear. b Postoperative coronal MRI of the same left shoulder 2 years after arthroscopic rotator cuff repair. Note the regenerated tissue coverage over the lateral tuberosity rotator cuff footprint. Snyder and Buford have reported upon this, with biopsy-proven “neo-tendon” covering the tuberosity lateral to the repair site [6, 57]. c Preoperative coronal MRI of a right shoulder showing a full-thickness rotator cuff tear. d Postoperative coronal MRI of the same right shoulder at 2 years demonstrates a Sugaya V, Cho type I re-torn rotator cuff
Subjective clinical outcomes were evaluated with three surveys. First, a custom short survey to assess the patient’s overall satisfaction with the surgery and questions regarding medical issues shown to influence rotator cuff healing in previous studies, including history of diabetes mellitus, smoking or alcohol usage [3, 11, 56, 62]. Secondly, a Western Ontario Rotator Cuff Index (WORC), a validated outcome measure shown to correlate well with other outcome tools, and also more responsive (sensitive to change) than other outcome tools (UCLA, DASH, ASES, Constant, Rowe) for rotator cuff disease [40]. Finally, a short-form 36 version 2 mental and physical scores were completed. Institutional approval for this study was obtained from the Southern California Orthopedic Research and Education Center for a non-therapeutic retrospective study.
Statistical analysis
Mann–Whitney tests compared patient’s outcome scores between healed and re-torn cuff repairs. Multivariate logistic regression was performed to determine the association of selected variables with healing status and WORC score, including age, tear size, number of anchors, surgeon, tobacco and/or alcohol use and history of diabetes. A p value (alpha) less than 0.05 was considered significant. All analyses were performed with SAS software (version 9.1; SAS Institute, Cary NC). Post hoc analysis indicated this study did not achieve sufficient power with an estimated necessary sample size of 140.
Results
At a mean follow-up of 34 ± 9 months, MRI demonstrated an intact repair in 48 of 53 shoulders (91%) with breakdown by Sugaya classification (Table 3). All five failures were Cho Type I [12]. Forty-six of 53 shoulders (87%) reported complete satisfaction with their results. The median WORC score was 95.7 (range 27.6–100.0). The median SF-36 Physical and Mental score was 51 (range 29–62) and 58 (41–66), respectively.
During uni- and multivariate analyses, no correlations were observed between repair integrity or WORC score with: age, sex, tear size, anchor number, surgeon, previous surgery (three patients had previous surgery), diabetes, alcohol use and smoking (all three smokers healed). Significant difference in WORC scores was observed between healed repairs 96.7 (range 56.7–100.0) and re-torn cuffs versus 64.6 (range 27.6–73.8), p < 0.00056.
Complications and adverse events
Two patients required revision repair within 12 months of index surgery.
One patient developed postoperative subacromial fibrosis and arthrofibrosis requiring manipulation under anaesthesia, lysis of adhesions and subacromial debridement seven months postoperatively.
Discussion
The 91% intact repair rate on postoperative MRI and excellent overall patient reported clinical outcomes for medium to large rotator cuff tears supports the concepts of minimizing repair tension, optimizing biomechanics and maximizing biology of healing that are fundamental to our novel SR technique. While there is no study control group, our observed healing rate meets or exceeds other recently published studies of similar-sized tears repaired utilizing various different techniques (Table 1).
Three core features in combination distinguish this novel SR technique from others:
-
1.
A single row of screw-in suture anchors triple-loaded with high strength #2 sutures passed as simple stitches in a “fan-like” array.
-
2.
A medially based repair with anchors placed near the articular margin of the greater tuberosity minimizes repaired tendon tension.
-
3.
Bone marrow vents placed in the greater tuberosity lateral to the repair allows bone marrow element egress and vascular channel formation.
With the improved bony interface of modern suture anchors, the point of failure shifts to the tendon-suture interface as the tendon often slides through a suture’s grasp before the implant “fails” [18, 20]. Recent biomechanical studies have shown the number of tendon fixation points is the most important factor affecting repair strength, not number of anchors [33, 43].
DR constructs are favoured over SR constructs by most biomechanical studies, but few have compared to SR constructs using triple-loaded anchors. Coons et al. [17] found the additional third suture reduced cyclical gapping by a factor of 2.6 versus a double-loaded anchor. Barber et al. [2] reported significantly less cyclical load gap formation and no difference in load to failure between two triple-loaded anchors and TOE construct. More recently, Jost et al. published biomechanical results showing no difference in cyclic gap formation and mean load to failure between a 4-suture SR repair and a 4-suture DR repair (362 and 386 N, p = 0.58) [33].
While no in vivo studies have evaluated correlation between repair tension and healing rates, Davidson et al. did show significantly lower outcome scores in repairs requiring higher repair tension [19]. Several factors dictate repair tension, including the surgical technique and intrinsic tissue tension. The tendon typically tears in the hypovascular region leaving a shortened tendon. Repairing a shortened tendon to the lateral versus medial footprint increases repair tension from 2.2- to 5.4-fold in vivo as reported by Dierckman et al. [21, 22, 31, 47]. This is also compounded by the decreased modulus of elasticity with increasing tendon tear chronicity noted in animal models [16, 27, 28]. In combination, this is the primary biomechanical advantage of a medially based repair—attaching a shortened tendon to the medial footprint minimizes repaired muscle–tendon unit tension.
The peribursal tissues are the primary vascular source of healing with secondary cuff footprint contribution [1]. To augment the vascularity and local biological environment, several authors have advocated supplementing healing with bone marrow cells and growth factors to form a “super clot”, akin to the early clot during fracture healing, from bone vents in the tuberosity (Fig. 2) [32, 48, 58, 61].
Kida et al. [34] utilized a rat model to show the presence of significantly more chimeric green fluorescent marrow-derived cells within the tendon of the cuff repair/drilling group compared to the control shoulder along with higher tendon load to failure. Showing improved healing potential of vents, Jo et al. [32] reported decreased CT arthrogram dye leakage, to 16% from 35.5%, in patients undergoing DR cuff repair overlying footprint “channels” versus controls. Milano et al. [48] found improved MRI healing rates from 12.5% in controls to 60% with footprint “microfracture” for large cuff tears in a prospective randomized study of 80 patients using double-loaded SR repair. Validating the effects of marrow-derived stem cells, Hernigou et al. [30] demonstrated improved healing rates with iliac crest mesenchymal stem cells augmented SR repair at both six month and minimum ten year time points. They also noted increased long-term tendon integrity was related to injected stem cell number.
In the current study, patients with intact repairs demonstrated significantly better outcome scores than patients with a re-tear. Kim et al. also reported similar findings but most studies show no difference in outcomes [5, 14, 15, 36, 39, 50, 55, 59]. Kim et al. [36] also found that younger patients showed distinctly inferior outcomes compared with older patients when a re-tear occured. Although a re-tear does not preclude reasonable clinical outcomes especially in the older population, we believe anatomic healing should be the surgeon’s goal whenever possible.
Recent meta-analyses on SR versus DR repairs have shown a slight clinical and/or radiologic advantage towards DR repairs but none of the studies used a SR technique employing all three key features of out novel SR technique [45, 49, 64]. Amongst the Level I studies comparing SR to DR, six of seven studies placed the single row of anchors at the lateral margin of the greater tuberosity; all seven implanted double-loaded, not triple-loaded, anchors, and no studies utilized bone marrow vents [8, 10, 13, 23, 25, 29, 42]. These three key features of our technique in combination should represent a unique rotator cuff repair technique worthy of distinction from other SR repairs, just as the TOE technique receives distinction from other DR repairs. Future studies are needed directly comparing this novel SR technique to other SR and DR techniques for validation.
This study’s technique results in high repair healing rates and excellent patient reported outcomes. This can help guide surgeon technique choice to minimize recurrent rotator cuff tear rates for medium to large rotator cuff tears along with associated patient morbidity and socioeconomic costs. In addition to these benefits, there are direct cost savings from choosing the lower cost SR construct and by utilizing cost-free bone marrow vents [4, 26].
The study was limited by the lack of preoperative WORC scores, and the retrospective study design can introduce treatment and selection bias despite strict inclusion and exclusion criteria and prevents ability to compare to a simultaneous control group necessitating comparing results with recently published studies. The study was not sufficiently powered despite a relatively large sample size. Application of this data would not be applicable to larger or more complex tears requiring interval slides or margin convergence sutures.
Conclusion
Arthroscopic repair of medium to large rotator cuff tears using a triple-loaded single-row repair augmented with bone marrow vents resulted in a 91% healing rate by MRI and excellent clinical outcomes comparable to recently published rotator cuff repairs using other techniques.
Abbreviations
- SR:
-
Single-row
- DR:
-
Double-row
- MRI:
-
Magnetic resonance imaging
- PEEK:
-
Polyethylether ketone
- RCT:
-
Rotator cuff tear
- TOE:
-
Transosseous equivalent
- WORC:
-
Western Ontario Rotator Cuff
References
Adler RS, Johnson KM, Fealy S, Maderazo A, Gallo RA, Gamradt SC, Warren RF (2011) Contrast-enhanced sonographic characterization of the vascularity of the repaired rotator cuff: utility of maximum intensity projection imaging. J Ultrasound Med 30:1103–1109
Barber FA, Herbert MA, Schroeder FA, Aziz-Jacobo J, Mays MM, Rapley JH (2010) Biomechanical advantages of triple-loaded suture anchors compared with double-row rotator cuff repairs. Arthroscopy 26:316–323
Bedi A, Fox A, Harris P, Deng XH, Ying L, Warren R, Rodeo S (2010) Diabetes mellitus impairs tendon-bone healing after rotator cuff repair. J Shoulder Elb Surg 19:978–988
Bisson L, Zivaljevic N, Sanders S, Pula D (2015) A cost analysis of single-row versus double-row and suture bridge rotator cuff repair methods. Knee Surg Sports Traumatol Arthrosc 23(2):487–493
Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG (2005) Arthroscopic repair of full-thickness tears of the supraspinatus: Does the tendon really heal? J Bone Joint Surg Am 87A:1229–1239
Buford DA (2010) Restoration of the rotator cuff footprint after arthroscopic single row repair. Arthroscopy 26:SS-01
Burkhart SS (1995) The deadman theory of suture anchors: observations along a south Texas fence line. Arthroscopy 11:119–123
Burks RT, Crim J, Brown N, Fink B, Greis PE (2009) A prospective randomized clinical trial comparing arthroscopic single- and double-row rotator cuff repair: magnetic resonance imaging and early clinical evaluation. Am J Sports Med 37:674–682
Burns JP, Snyder SJ, Albritton M (2007) Arthroscopic rotator cuff repair using triple-loaded anchors, suture shuttles, and suture savers. J Am Acad Orthop Surg 15:432–444
Carbonel I, Martinez AA, Calvo A, Ripalda J, Herrera A (2012) Single-row versus double-row arthroscopic repair in the treatment of rotator cuff tears: a prospective randomized clinical study. Int Orthop 36:1877–1883
Cho NS, Moon SC, Jeon JW, Rhee YG (2015) The influence of diabetes mellitus on clinical and structural outcomes after arthroscopic rotator cuff repair. Am J Sports Med 43:991–997
Cho NS, Yi JW, Lee BG, Rhee YG (2010) Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med 38:664–671
Choi CH, Kim SK, Cho MR, Baek SH, Lee JK, Kim SS, Park CM (2012) Functional outcomes and structural integrity after double-pulley suture bridge rotator cuff repair using serial ultrasonographic examination. J Shoulder Elb Surg 21:1753–1763
Choi S, Kim MK, Kim GM, Roh YH, Hwang IK, Kang H (2014) Factors associated with clinical and structural outcomes after arthroscopic rotator cuff repair with a suture bridge technique in medium, large, and massive tears. J Shoulder Elb Surg 23:1675–1681
Cole B, McCarty P, Kang R, Alford W, Lewis PB, Hayden JK (2007) Arthroscopic rotator cuff repair: prospective functional outcome and repair integrity at minimum 2-year follow-up. J Shoulder Elb Surg 16:579–585
Coleman SH, Fealy S, Ehteshami JR, MacGillivray JD, Altchek DW, Warren RF, Turner AS (2003) Chronic rotator cuff injury and repair model in sheep. J Bone Joint Surg Am 85-A:2391–2402
Coons DA, Barber FA, Herbert MA (2006) Triple-loaded single-anchor stitch configurations: an analysis of cyclically loaded suture-tendon interface security. Arthroscopy 22:1154–1158
Cummins CA, Murrell GA (2003) Mode of failure for rotator cuff repair with suture anchors identified at revision surgery. J Shoulder Elb Surg 12:128–133
Davidson PA, Rivenburgh DW (2000) Rotator cuff repair tension as a determinant of functional outcome. J Shoulder Elb Surg 9:502–506
Denard PJ, Burkhart SS (2011) Arthroscopic revision rotator cuff repair. J Am Acad Orthop Surg 19:657–666
Dierckman BD, Wang D, Burns J, Getelman M (2016) In vivo measurement of rotator cuff tear tension: medial versus lateral footprint position. Am J Orthop 45:E83–E90
Domb B, Glousman R, Brooks A, Hansen M, Lee T, ElAttrache N (2008) High-tension double-row footprint repair compared with reduced-tension single-row repair for massive rotator cuff tears. J Bone Joint Surg Am 90(Suppl 4):35–39
Franceschi F, Ruzzini L, Longo U, Martina FM, Zobel BB, Maffulli N, Denaro V (2007) Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med 35:1254–1260
Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K (2004) The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 86-A:219–224
Gartsman GM, Drake G, Edwards TB, Elkousy HA, Hammerman SM, O’Connor DP, Press CM (2013) Ultrasound evaluation of arthroscopic full-thickness supraspinatus rotator cuff repair: single-row versus double-row suture bridge (transosseous equivalent) fixation. Results of a prospective, randomized study. J Shoulder Elb Surg 22:1480–1487
Genuario JW, Donegan RP, Hamman D, Bell JE, Boublik M, Schlegel T, Tosteson AN (2012) The cost-effectiveness of single-row compared with double-row arthroscopic rotator cuff repair. J Bone Joint Surg Am 94:1369–1377
Gerber C, Meyer DC, Schneeberger AG, Hoppeler H, von Rechenberg B (2004) Effect of tendon release and delayed repair on the structure of the muscles of the rotator cuff: an experimental study in sheep. J Bone Joint Surg Am 86-A:1973–1982
Gimbel JA, Van Kleunen JP, Lake SP, Williams GR, Soslowsky LJ (2007) The role of repair tension on tendon to bone healing in an animal model of chronic rotator cuff tears. J Biomech 40:561–568
Grasso A, Milano G, Salvatore M, Falcone G, Deriu L, Fabbriciani C (2009) Single-row versus double-row arthroscopic rotator cuff repair: a prospective randomized clinical study. Arthroscopy 25:4–12
Hernigou P, Flouzat Lachaniette CH, Delambre J, Zilber S, Duffiet P, Chevallier N, Rouard H (2014) Biologic augmentation of rotator cuff repair with mesenchymal stem cells during arthroscopy improves healing and prevents further tears: a case–controlled study. Int Orthop 38(9):1811–1818
Hersche O, Gerber C (1998) Passive tension in the supraspinatus musculotendinous unit after long-standing rupture of its tendon: a preliminary report. J Shoulder Elb Surg 7:393–396
Jo CH, Shin JS, Park IW, Kim H, Lee SY (2013) Multiple channeling improves the structural integrity of rotator cuff repair. Am J Sports Med 41:2650–2657
Jost PW, Khair MM, Chen DX, Wright TM, Kelly AM, Rodeo SA (2012) Suture number determines strength of rotator cuff repair. J Bone Joint Surg Am 94:e100
Kida Y, Morihara T, Matsuda K, Kajikawa Y, Tachiiri H, Iwata Y, Sawamura K, Yoshida A, Oshima Y, Ikeda T, Fujiwara H, Kawata M, Kubo T (2013) Bone marrow-derived cells from the footprint infiltrate into the repaired rotator cuff. J Shoulder Elb Surg 22:197–205
Kim D, ElAttrache N, Tibone J, Jun BJ, DeLaMora S, Kvitne R, Lee T (2006) Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med 34:407–414
Kim HM, Caldwell JM, Buza JA, Fink LA, Ahmad CS, Bigliani LU, Levine WN (2014) Factors affecting satisfaction and shoulder function in patients with a recurrent rotator cuff tear. J Bone Joint Surg Am 96:106–112
Kim KC, Shin HD, Cha SM, Lee WY (2013) Comparison of repair integrity and functional outcomes for 3 arthroscopic suture bridge rotator cuff repair techniques. Am J Sports Med 41:271–277
Kim KC, Shin HD, Lee WY, Han SC (2012) Repair integrity and functional outcome after arthroscopic rotator cuff repair: double-row versus suture-bridge technique. Am J Sports Med 40:294–299
Kim SJ, Kim SH, Lee SK, Seo JW, Chun YM (2013) Arthroscopic repair of massive contracted rotator cuff tears: aggressive release with anterior and posterior interval slides do not improve cuff healing and integrity. J Bone Joint Surg Am 95:1482–1488
Kirkley A, Alvarez C, Griffin S (2003) The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: the Western Ontario Rotator Cuff Index. Clin J Sport Med 13:84–92
Koh K, Kang K, Lim T, Shon M, Yoo J (2011) Prospective randomized clinical trial of single versus double-row suture anchor repair in 2- to 4-cm rotator cuff tears: clinical and magnetic resonance imaging results. Arthroscopy 27:453–462
Lapner PLC, Sabri E, Rakhra K, McRae S, Leiter J, Bell K, Macdonald P (2012) A multicenter randomized controlled trial comparing single-row with double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am 94:1249–1257
Lorbach O, Kieb M, Raber F, Busch LC, Kohn D, Pape D (2012) Comparable biomechanical results for a modified single-row rotator cuff reconstruction using triple-loaded suture anchors versus a suture-bridging double-row repair. Arthroscopy 28:178–187
Mall NA, Tanaka MJ, Choi LS, Paletta GA Jr (2014) Factors affecting rotator cuff healing. J Bone Joint Surg Am 96:778–788
Mascarenhas R, Chalmers PN, Sayegh ET, Bhandari M, Verma NN, Cole BJ, Romeo AA (2014) Is double-row rotator cuff repair clinically superior to single-row rotator cuff repair: a systematic review of overlapping meta-analyses. Arthroscopy 30:1156–1165
Mazzocca AD, Bollier MJ, Ciminiello AM, Obopilwe E, DeAngelis JP, Burkhart SS, Warren RF, Arciero RA (2010) Biomechanical evaluation of arthroscopic rotator cuff repairs over time. Arthroscopy 26:592–599
Meyer DC, Farshad M, Amacker NA, Gerber C, Wieser K (2012) Quantitative analysis of muscle and tendon retraction in chronic rotator cuff tears. Am J Sports Med 40:606–610
Milano G, Saccomanno MF, Careri S, Taccardo G, De Vitis R, Fabbriciani C (2013) Efficacy of marrow-stimulating technique in arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy 29:802–810
Millett PJ, Warth RJ, Dornan GJ, Lee JT, Spiegl UJ (2014) Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elb Surg 23:586–597
Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS (2009) Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy 25:30–39
Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun BJ, Lee TQ (2007) Part I: footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elb Surg 16:461–468
Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun BJ, Lee TQ (2007) Part II: biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elb Surg 16:469–476
Pennington WT, Gibbons DJ, Bartz BA (2010) Comparative analysis of single-row versus double-row repair of rotator cuff tears. Arthroscopy 26:1419–1426
Quigley RJ, Gupta A, Oh JH, Chung KC, McGarry MH, Gupta R, Tibone JE, Lee TQ (2013) Biomechanical comparison of single-row, double-row, and transosseous-equivalent repair techniques after healing in an animal rotator cuff tear model. J Orthop Res 31:1254–1260
Russell RD, Knight JR, Mulligan E, Khazzam MS (2014) Structural integrity after rotator cuff repair does not correlate with patient function and pain: a meta-analysis. J Bone Joint Surg Am 96:265–271
Santiago-Torres J, Flanigan DC, Butler RB, Bishop JY (2015) The effect of smoking on rotator cuff and glenoid labrum surgery: a systematic review. Am J Sports Med 43:745–751
Snyder SJ, Arnoczky SP, Bond JL, Dopirak R (2009) Histologic evaluation of a biopsy specimen obtained 3 months after rotator cuff augmentation with GraftJacket Matrix. Arthroscopy 25:329–333
Snyder S, Burns J (2009) Rotator cuff healing and the bone marrow “Crimson Duvet”. From clinical observations to science. Tech Shoulder Elb Surg 10:130–137
Sugaya H, Maeda K, Matsuki K, Moriishi J (2007) Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am 89:953–960
Sugaya H, Mueda K, Matsuki K, Moriishi J (2005) Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single versus dual-row fixation. Arthroscopy 21:1307–1316
Taniguchi N, Suenaga N, Oizumi N, Yamaguchi H, Inoue K, Chosa E (2015) Bone marrow stimulation at the footprint of arthroscopic surface-holding repair advances cuff repair integrity. J Shoulder Elb Surg 24:860–866
Tashjian R, Hollins A, Kim HM, Teefey SA, Middleton WD, Steger-May K, Galatz LM, Yamaguchi K (2010) Factors affecting healing rates after arthroscopic double-row rotator cuff repair. Am J Sports Med 38:2435–2442
Wu XL, Briggs L, Murrell GA (2012) Intraoperative determinants of rotator cuff repair integrity: an analysis of 500 consecutive repairs. Am J Sports Med 40:2771–2776
Xu C, Zhao J, Li D (2014) Meta-analysis comparing single-row and double-row repair techniques in the arthroscopic treatment of rotator cuff tears. J Shoulder Elb Surg 23:182–188
Acknowledgements
The authors would like to thank Dr. Greg Applegate for his assistance reviewing MRI scans for this study.
Author's contributions
BDD has made substantial contributions to the conception, design and acquisition of data, the statistical analysis and interpretation of the data, has been involved in drafting the manuscript for important intellectual content. He has given final approval of the version to be published and agrees to be accountable for all aspects of the work. JJN has made contributions to the statistical analysis and interpretation of the data, has been involved in drafting and revision of the manuscript for important intellectual content. He has given final approval of the version to be published and agrees to be accountable for all aspects of the work. RPK has made substantial contributions to the conception, design and acquisition of data, has been involved in drafting the manuscript for important intellectual content. He has given final approval of the version to be published and agrees to be accountable for all aspects of the work. MHG has made substantial contributions to the conception, design and acquisition of data, has been involved in drafting the manuscript for important intellectual content. He has given final approval of the version to be published and agrees to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The senior author RPK is a consultant for MicroAire Surgical Instruments and Smith and Nephew, and has a financial interest in Surgical Solutions and royalties from Lippincott Williams and Wilkins. MHG is a consultant for Mitek, and has research grants from Rotation Medical and Histogenics and royalties from Lippincott Williams and Wilkins.
Funding
There was a grant from Depuy Synthes.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Southern California Orthopedic Research and Education Center provided institutional approval for this non-therapeutic retrospective study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Dierckman, B.D., Ni, J.J., Karzel, R.P. et al. Excellent healing rates and patient satisfaction after arthroscopic repair of medium to large rotator cuff tears with a single-row technique augmented with bone marrow vents. Knee Surg Sports Traumatol Arthrosc 26, 136–145 (2018). https://doi.org/10.1007/s00167-017-4595-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4595-6