Abstarct
Purpose
Multiligamentous injury to the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) is an uncommon but debilitating event. Patients with combined ligament injuries typically complain of painful, debilitating knee instability that restricts their sports and daily activities. The purpose of this retrospective study was to evaluate functional and clinical outcomes of patients with chronic ACL and PCL deficiency who underwent simultaneous single-stage arthroscopic reconstruction of the central pivot.
Methods
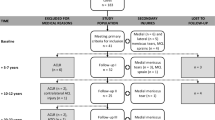
Medical records of 20 consecutive patients with chronic ACL and PCL deficiency who underwent simultaneous single-stage arthroscopic reconstruction of the central pivot were retrospectively reviewed. All patients had received either an allograft (group A) or a semitendinosus–gracilis graft for ACL repair and a bone–patellar tibial–bone graft for PCL repair (group B). Functional outcomes, after the initial follow-up period at 24-month FU, were assessed with concentric isokinetic knee extensor–flexor testing at 60 and 180°/s. The secondary aim was to compare long-term clinical recovery by the administration of the IKDC (International Knee Document Committee) Knee Ligament Evaluation Form, the Lysholm Knee Scoring Scale and the Cincinnati Knee Rating Scale.
Results
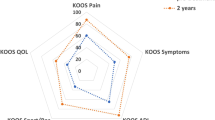
The mean per cent quadriceps strength deficit in the operated as compared to the healthy knee was 13.5 % in group A and 15 % in group B (angular velocity 60°/s) and 13.5 % in group A and 9.4 % in group B (angular velocity 180°/s). The mean per cent flexor strength deficit in the operated as compared to the healthy knee was 10.4 % in group A and 12.3 % in group B (angular velocity 60°/s) and 12.2 % in group A and 9 % in group B (angular velocity of 180°/s). The flexor–quadriceps ratio was 49.4 % in group A and 48.8 % in group B in the healthy knee and 53.2 % in group A and 53.8 % in group B in the operated knee (angular velocity 60°/s) and 63.9 % in group A and 60.7 % in group B in the healthy knee and 65 % in group A and 64.9 % in group B in the operated knee (angular velocity 180°/s). Lysholm outcome was 93.9 ± 3.9 in group A and 89.1 ± 7.6 in group B (n.s). Cincinnati score was 89.6 ± 7.3 in group A and 91.0 ± 6.9 in group B (p = 0.791). IKDC results were group A in six patients (60 %), group B in three patients (30 %) and group C in one patient (10 %) in the allograft group and group A in seven patients (70 %) and group B in three patients (30 %) for autologous group.
Conclusions
The results of this study suggest that one-stage arthroscopic bicruciate ligament reconstruction can restore good knee joint function. Surgical treatment should be followed by a comprehensive rehabilitation programme with specific goals, objectives and strategies, including pain management and assessment of progress in recovery of joint function and perception of knee stability.
Level of evidence
Retrospective case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiligamentous injury to the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) is an uncommon but debilitating event [5, 6]. The mechanism of injury is often caused by deceleration with external rotation and valgus stress, frequently in association with sports accidents or vehicular trauma resulting in subluxation or frank dislocation of the knee joint. Two types are distinguished: high-energy and low-energy mechanisms of injury. High-energy mechanisms are caused by a sudden, direct blow as occurs, for example, in road traffic accidents and are often associated with peripheral ligament damage and disruption of blood vessels and nerves [7, 8, 17]. Low-energy mechanisms occur more commonly during contact sports accidents, but seldom involve the peripheral knee joint capsule and ligaments and, more rarely, blood vessels and nerves [7, 8, 17].
Patients with combined ligament injuries typically complain of painful, debilitating knee instability that restricts their sports and daily activities [7, 16]. The patients we encounter have a chronic condition, with knee instability usually following a low-energy injury. The primary aim of this retrospective study was to evaluate knee joint stability by functional outcomes, in particulary by isokinetic assessment over a 2-year follow-up period after central pivot reconstruction. The secondary aim was to compare long-term clinical recovery in patients who had received either an allograft (Achilles and/or posterior tibial tendon) or a semitendinosus–gracilis graft for ACL repair and a bone–patellar tibial–bone graft for PCL repair.
Materials and methods
Between 2000 and 2006, we carried out 42 combined ACL–PCL arthroscopic reconstructions and 29 associated with posteromedial or lateral repairs of chronic knee ligament injuries.
Peripheral repairs were performed only when major damage to the medial or posterolateral compartment was present. For the complete and isolated reconstruction of the central pivot, we reconstructed the two ligaments during a single-stage arthroscopy. In order to obtain homogeneous data for the long-term results and condition, we retrospectively reviewed the medical records of 20 consecutive patients with chronic ACL and PCL deficiency with no meniscal injuries associated who underwent simultaneous single-stage arthroscopic reconstruction of the central pivot by the same surgeon (MD). The patient sample was divided into two groups. Group A (n = 10) received an allograft tendon (Achilles and/or posterior tibial tendon) for both repairs; group B (n = 10) received STG graft for PCL repair and a BPTB graft for ACL repair (n = 5) if the size of the STG graft was 9 mm in diameter or more, otherwise the patients received a semitendinosus–gracilis (STG) graft for ACL repair and a bone–patellar tendon–bone (BPTB) graft for PCL repair (n = 5). The type of transplant has been decided by the senior surgeon based on the needs and demands of the patient.
Surgical technique
Three comparably trained orthopaedic surgeons (MD, PV, HS) performed the surgeries using the same arthroscopic technique at the time of the operation. The first stage of the surgical procedure involved balancing the joint and treating any cartilage or meniscal damage if present. Standard arthroscopic portals were established. An accessory posteromedial portal was placed to facilitate PCL repair. Full tibial tunnels were created; the out–in technique was used to create the femoral tunnel for PCL repair and the endoscopic transtibial technique for ACL repair. Autografts or allografts were used for all reconstructions. The reconstructed PCL was fixed with two absorbable interference screws, and the reconstructed ACL was fixed with two biopins placed in the femur and an absorbable screw in the tibia.
Rehabilitation programme
All patients underwent the same rehabilitation programme which included:
-
Use of a rehabilitation brace with rear leg support for 6 weeks: locked in extension for the first week, released 0°–60° in the second week, released 0°–90° from the third week until removal and then progressive full ROM starting the fourth week
-
Brace locked in extension during gait for the first 4 weeks
-
Weight-bearing during the first week, minimal (toe-touch) weight-bearing during the second week and gradual progression to partial weight-bearing during the third week
-
Prevention of posterior translation for the first month during both supine decubitus and mobilization exercises
Functional outcomes
The primary outcomes after the initial follow-up period at 24-month FU were assessed with concentric isokinetic knee extensor–flexor testing at 60 and 180°/s.
Isokinetic testing was performed on a REV 9000 isokinetic dynamometer (Technogym, Gambettola, Bologna, Italy). Subjects sat in a comfortable, upright seated position and were secured using torso, pelvic and thigh straps to minimize extraneous body movements. The lateral femoral epicondyle was used as the bony landmark for aligning the axis of rotation of the knee with the lever arm axis. A 6-min warm-up on the exercise bicycle (70 pedal turns per min) was followed by three 30-s knee extensor and flexor stretching exercises. The uninvolved side was assessed first and then the operated side. Three submaximal and two maximal knee extension–flexion contractions were performed at both test speeds to enable the patients to become accustomed with the system.
The test consisted of five knee extension–flexion cycles along a range of motion (ROM) of 0°–90°, first at 60°/s and then at 180°/s after 1-min rest. Only the peak value was considered.
During the test, the patients held their arms folded across the chest and were given verbal encouragement and visual feedback from the REV 9000 computer monitor to reach maximal effort level. Gravity correction was performed. Bilateral comparison of peak torques was conducted to assess muscular insufficiency.
Clinical outcomes
The secondary objective (clinical outcomes) after long-term follow-up was assessed using the IKDC (International Knee Document Committee) Knee Ligament Evaluation Form [4], the Lysholm Knee Scoring Scale [14] and the Cincinnati Knee Rating Scale [10].
Statistical analysis
Data were expressed as number and percentage, if categorical, or mean and standard deviation, if continuous. Differences between groups were explored with the Chi-square test with Fisher’s correction if categorical or with the Wilcoxon test if continuous. Continuous data were represented with box-and-whisker plots where the internal line represents the median, the box itself is delimited by the first quartile (Q1) and the third quartile (Q3), and the whiskers are delimited by the formula Q1 − 1.5 × IQR for the lower whisker and by Q3 + 1.5 × IQR for the upper whisker, where IQR is the interquartile range. All analyses were performed using Stata Statistical Software Release 13 (StataCorp LP, College Station, TX). A p value lower than 0.05 was considered significant. This study received IRB notification as request by national guidelines because it includes human subjects and health informations.
Results
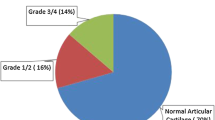
The mean age was 36 ± 14 years in group A and 33 ± 8 years in group B (n.s). The right knee was operated on in five (50 %) patients in group A and eight (80 %) patients in group B (n.s). Isokinetic testing was performed at 24 months in both groups. Long-term clinical assessment was performed at 109.3 months (range 95.8–117.4) in group A and at 135.9 months (range 96.4–168.6) in group B (p = 0.018). Table 1 reports the peak torque of the quadriceps and flexor muscles of the healthy and the operated knee. The mean per cent quadriceps strength deficit in the operated as compared to the healthy knee was 13.5 % in group A and 15 % in group B (angular velocity 60°/s) and 13.5 % in group A and 9.4 % in group B (angular velocity 180°/s). The mean per cent flexor strength deficit in the operated as compared to the healthy knee was 10.4 % in group A and 12.3 % in group B (angular velocity 60°/s) and 12.2 % in group A and 9 % in group B (angular velocity of 180°/s). The flexor–quadriceps ratio was 49.4 % in group A and 48.8 % in group B in the healthy knee and 53.2 % in group A and 53.8 % in group B in the operated knee (angular velocity 60°/s) and 63.9 % in group A and 60.7 % in group B in the healthy knee and 65 % in group A and 64.9 % in group B in the operated knee (angular velocity 180°/s) (Table 2). Table 3 reports the scores from the Lysholm Knee Scoring Scale, Cincinnati Knee Rating Scale and International Knee Documentation Committee (IKDC) subjective evaluation (Fig. 1).
There were no statistically significant differences for any of the parameters measured (p < 0.05). Return to sports occurred at 14.8 months on average. Three of the five competitive (60 %) athletes and 8 (73 %) of the 11 amateur athletes returned to their previous sports levels (p = 1)
Discussion
The most important finding of this study was that one-stage ACL/PCL reconstruction is a reliable technique for restoring knee function. In the literature, evidence-based treatment guidelines are lacking and treatment options are controversial [1, 2] (Fig. 2).
Although isokinetic test results do not predict dynamic stability of the knee, they can provide objective data on activator muscle strength. No statistically significant differences in any of the parameters measured during isometric testing between the two groups were found, but partially unexpected results that diverged from previous studies were noted. Takaes et al. [13] performed isokinetic evaluation at 27 months of follow-up after two-stage bicruciate reconstruction with autografts in 14 patients. They reported a mean extensor peak torque of 167 and 122 Nm at an angular velocity of 60 and 180°/s, respectively, in the operated side and a mean flexor peak torque of 98 and 79 Nm at an angular velocity of 60 and 180°/s, respectively, in the operated side. As compared to the unoperated side, the strength deficit of the extensors at both velocities was significantly different, but that of the flexors was not. The flexor–extensor ratio was similar for both knees. In an earlier study, Tornese et al. [15] compared the outcomes after arthroscopic reconstruction of the PCL using the double-bundle technique with the ipsilateral STG graft and the single-bundle technique with an ipsilateral patellar tendon graft. At the 12-month follow-up examination, no significant differences in the IKDC, Lysholm or Cincinnati Rating Scale scores were found, but the isokinetic tests disclosed a loss of strength in the corresponding muscles at the harvest site (Fig. 3).
On the basis of these observations, one would expect a minor muscle strength deficit after reconstruction with cadaveric tendons. One explanation for this could be that the mean length of follow-up was a contributing factor to the statistically significant difference between the two groups. It may have allowed the group B patients to recover a per cent of muscle strength deficit at the harvest site. In any case, this empirical observation needs to be further investigated (Fig. 4).
Analysis of the Lysholm, Cincinnati and IKDC Rating Scale scores, at longer follow-up, showed good recovery of biomechanical function of the operated knee. These clinical results are similar to those shown by other authors as Zaho [18] who reported excellent subjective outcomes with mean IKDC = 92.4 at 2-year follow-up in 12 patients. Strobel reported mean IKDC of 71.1 on 17 patients with combined ACL, PCL and PLC reconstructions at 2-year follow-up [12].
Hart et al. [3] reported mean IKDC subjective score of 61.2 ± 23.1 at 2-year follow-up after multiple ligament knee reconstruction surgeries.
Despite the severity of knee instability and the surgical challenge of restoring knee joint function, the scores were substantially within the normal range and indicated a satisfactory outcome. Biomechanical function was similar or in some cases very similar to normal performance on manual and instrumental testing and during routine activities (walking, climbing and descending stairs, squatting and running) which the patients were able to carry out with reasonable ease, considering the high incidence of joint stiffness associated with surgical repair of the central pivot [16].
Overall, results expressed in this study are consistent with previous studies [9, 11, 19] reporting that ACL/PCL reconstruction is an optimal approach to treating chronic central pivot injuries. Furthermore, safe return to sports depends not only on surgical outcome and adherence to a rehabilitation programme but oftentimes on personal motivation and self-management. Surgical treatment should be followed by a comprehensive rehabilitation programme with specific goals, objectives and strategies for achieving good biomechanical knee joint function. The limitation of this retrospective study was a small number of patients for each functional group and with a short functional follow-up. This fact is due to the fact that knee joint dislocation is rare and accounts for only approximately 0.02 % of all musculoskeletal injuries and most published studies include only a small number of cases [2].
Conclusions
This study results suggest that one-stage arthroscopic bicruciate ligament reconstruction can restore good biomechanical knee joint function.
References
Arøen A, Sivertsen ES, Owesen C, Engebretsen L, Granan LP (2013) An isolated rupture of the posterior cruciate ligament results in reduced preoperative knee function in comparison with an anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 21(5):1017–1221
Frosch KH, Preiss A, Heider S, Stengel D, Wohlmuth P, Hoffmann MF, Lill H (2013) Primary ligament sutures as a treatment option of knee dislocations: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 21(7):1502–1509
Hart JM, Blancharrd BF, Hart JA, Montgomery SC, Schonderbek R, Miller MD (2009) Multiple ligament knee reconstruction clinical follow-up and gait analysis. Knee Surg Traumatol Arthrosc 17:277–285
Hefti F, Muller W, Jakob RP, Stäubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1(3–4):226–234
Jenkins PJ, Clifton R, Gillespie GN, Will EM, Keating JF (2011) Strength and function recovery after multiple-ligament reconstruction of the Knee. Injury. Int J Care Injured 43:1426–1429
Kannus P (1994) Isokinetic evaluation of muscular performance. Implications for muscle testing and rehabilitation. Int J Sports Med 15:11–18
Kannus P, Bergefeld J, Jarvinen M, Johnson RJ, Pope M, Renstrom P et al (1991) Injuries to the posterior cruciate ligament of the knee. Sports Med 12:10–131
Mariani PP, Becker R, Rhin J, Margheritini F (2003) Surgical treatment of posterior cruciate ligament and posterolateral corner injury. An anatomical, biomechanical and clinical review. Knee 10:311–324
Noyes FR, Barber-Westin SD (1997) Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Use of early protected postoperative motion to decrease arthrofibrosis. Am J Sports Med 25:769–778
Noyes FR, McGinnis GH, Grood ES (1985) The variable functional disability of the anterior cruciate ligament deficient knee. Orthop Clin of North Am 16:47–67
Pierce CM, O’Brien L, Wohlt Griffin L, LaPrade R (2013) Posterior cruciate ligament tears: functional and postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc 21(5):1071–1084
Strobel MJ, Schulz MS, Petersen WJ, Eichhorn HJ (2006) Combined anterior cruciate ligament, posterior cruciate ligament and posterolateral corner reconstruction with autogenous hamstring grafts in chronic instabilities. Arthroscopy 22:182–192
Takaes IG, Inada MM, de Miranda JB, Cunha SA, Piedade SR (2014) Isokinetic evaluation after two-stage bicruciate reconstruction. Acta Orthop Bras 22:21–24
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of the knee ligament injuries. Clin Orthop Rel Res 198:43–49
Tornese D, Bandi M, Volpi P, Schonhuber H, Denti M, Ricci G, Melegati G (2008) Patellar tendon graft vs Semitendinosus and Gracilis graft for posterior cruciate ligament reconstruction: an isokinetic and functional study one year after the operation. Isokinet Exerc Sci 16:133–137
Tzurbakis M, Diamantopoulos A, Xenakis T, Georgoulis A (2006) Surgical treatment of multiple knee ligament injuries in 44 patients: 2–8 years follow up results. Knee Surg Sports Traumatol Arthrosc 14:739–749
Young A, Hughes I, Round JM, Edwards RH (1982) The effect of knee injury on the number of muscle fibres in the human quadriceps femoris. Clin Sci 62:227–234
Zhao J, He Y, Wang J (2006) Simultaneous arthroscopic reconstruction of the anterior and posterior cruciate ligament with autogenous hamstring tendons. Arthroscopy 22:497–504
Zorzi C, Alam M, Iacono V, Madonna V, Rosa D, Maffulli N (2013) Combined PCL and PLC reconstruction in chronic posterolateral instability. Knee Surg Sports Traumatol Arthrosc 21(5):1036–1042
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Denti, M., Tornese, D., Melegati, G. et al. Combined chronic anterior cruciate ligament and posterior cruciate ligament reconstruction: functional and clinical results. Knee Surg Sports Traumatol Arthrosc 23, 2853–2858 (2015). https://doi.org/10.1007/s00167-015-3764-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3764-8