Abstract
Purpose
Component malrotation has a major impact on patellar kinematics in total knee arthroplasty. The influence of natural rotational limb alignment on patellar kinematics is unclear so far. Based on recent clinical investigations, we hypothesized that rotational limb alignment significantly influences patellar kinematics.
Methods
Patellar kinematics of ten cadaveric knees was measured using computer navigation during passive motion. Data were correlated with different rotational limb alignment parameters of preoperative CT scans.
Results
Femoral antetorsion showed a significant influence on patellar rotation, while tibial tubercle–posterior cruciate ligament distance additionally displayed a significant influence on patellar mediolateral shift (p < 0.05). Femoral posterior condylar angle was sensitive to patellar epicondylar distance, rotation and tilt (p < 0.05). Patellar rotation was influenced by five out of eight rotational limb alignment parameters (p < 0.05).
Conclusions
Rotational limb alignment should be paid more attention in terms of clinical evaluation of patellar tracking and future biomechanical and clinical investigations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the main functions of the patella is to centralize the forces of the different quadriceps muscle bellies to allow a smooth gliding mechanism and to improve the efficiency of the extension forces [1, 13]. These biomechanical functions are achieved successfully only if the patellar tracking in the femoral trochlea groove occurs correctly [17]. Data on patellar biomechanics have been collected through the description of patellar tracking, muscle forces and retropatellar contact pressure and shear forces in many recent biomechanical studies under static and dynamic conditions before and after TKA [3, 7, 11, 14, 17, 20, 22, 26, 27, 34]. Three-dimensional patellar kinematics has also been analysed using patellar tracking navigation system [2, 22]. All of these studies were designed to describe patellar kinematics in the natural knee and to compare different designs of total knee arthroplasties (TKA). Component malrotation has a major impact on the patellofemoral joint [5, 21], but little is known about the influence of natural rotational limb alignment on patellar kinematics. Recent clinical studies suggest that transverse plane rotation of the femur and the tibia may also contribute to patellar maltracking; in addition, these studies have shown an association between femoral antetorsion and anterior knee pain [10, 28]. Less is known about the influence of tibial torsion and further rotational limb alignment parameters on patellar kinematics [12]. Based on the above-mentioned investigations, we hypothesized that rotational limb alignment has a significant influence on patellar kinematics. The aim of this study was to analyse and quantify a possible influence of different rotational limb alignment parameters on natural patellar kinematics.
Materials and methods
Ten intact lower limbs still attached to the torso of whole Thiel-embalmed cadavers were used for this investigation. CT scans of the complete lower limbs were performed preoperatively in supine position. The limbs were mounted in a footrest and rotated approximately 15° externally, to stabilize them during examination. Sections of 1.25 mm thickness of the whole limbs were taken. One CT-experienced observer measured the different rotational limb alignment parameters using AGFA Healthcare IMPAX Software (53227 Bonn, Germany). All knees were free from significant arthritic deterioration, and with intact joint capsules, patellar and quadriceps tendons and cruciate and collateral ligaments. No patellar or trochlear dysplasia, patellar luxation or subluxation could be detected in the specimens. Patellar kinematics was analysed using a commercial optical computer navigation system (Knee Patella Tracking Software, BrainLAB; Feldkirchen, Germany). The optical computer navigation system used has been verified to be a reliable measurement procedure to evaluate three-dimensional tibiofemoral and patellofemoral kinematics with an accuracy of 0.1 mm and 0.1° [15, 23].
Anatomical preparation and patellar tracking assessment
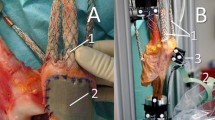
After a standard midline incision, a medial parapatellar approach was performed. The capsule was marked at standardized locations to ensure later anatomical closure. The reference arrays for the navigation system were attached to the distal femur, proximal tibia and the patella. For the femoral attachment, an additional, more proximal incision was performed to avoid soft tissue tension while flexion. The landmarks for tibiofemoral and patellofemoral kinematics needed for the navigation software were registered. The most proximal, distal and medial point on the patellar articular surface and a point in the middle of the posterior articular ridge were chosen to track the patella on the registered trochlear groove. After registration, the arthrotomy was closed carefully with respect to the markings to achieve anatomical aligned closure. The limbs were placed onto a continuous passive motion machine to perform a motion cycle between 30° and 90° of flexion. Due to missing muscle tone and floppy patellae, values until 30° of flexion were irregular and excepted from the experimental protocol. The motion cycle was repeated three times to verify patellar tracking behaviour.
Data analysis
The data were analysed using patellar tracking software (BrainLAB; Feldkirchen, Germany). The motion of the tracked patella relative to the femur was calculated. Patellar kinematics could be analysed through mediolateral translation/shift in millimetres (medial: +, lateral: −), mediolateral tilt in degrees (lateral: +, medial: −), internal and external rotation in degrees (internal: +, external: −). Additionally, the epicondylar distance (mm) describing the line from the prior chosen most prominent point at the middle of the posterior articular ridge of the patella perpendicular to the transepicondylar line, which is built by the registered femoral epicondyles, was measured during the whole motion cycle (Fig. 1).
CT scan analysis
The transverse CT images were evaluated according to different measurement procedures. The following eight objective radiological parameters were measured:
-
1.
Femoral antetorsion according to Murphy [25]: Three transverse sections were used to calculate femoral antetorsion. The first section defined the centre of the femoral head. The second section defined the centre of the base of the femoral neck at the level of the lesser trochanter, and the third section defined the femoral posterior condylar line. The first two sections were superimposed, and a line was drawn connecting the two centres representing the femoral neck axis. The angle between the femoral neck axis (FNA) and the condylar axis (CA) represents the femoral antetorsion.
-
2.
Tibial torsion was measured according to the method of Jend et al. [19]: A section of the proximal tibia directly distal to the femorotibial joint and proximal to the fibula head was used. The tangent to the dorsal margin of the tibia was taken as the reference in this section. A section directly proximal to the talocrural joint was chosen in the distal tibia. A line connecting the centre of the pilon tibiale and the midpoint of the fibular incision of the distal tibia was taken as the reference in this section (upper ankle joint axis).
-
3.
Tibial tubercle–trochlear groove distance (TT-TG) was measured according to Dejour et al. [6]: to measure the TT-TG distance, an axial section at the deepest point of the trochlear was superimposed upon the centre of the tibial tuberosity, ensuring that the measurement was performed parallel to the posterior condylar line.
-
4.
Tibial tubercle–posterior cruciate ligament distance (TT-PCL) was measured according to Seitlinger et al. [32]: the mediolateral distance between the midpoint of the insertion of the patellar tendon and the medial border of the posterior cruciate ligament parallel to the dorsal tibia condylar line (tangent to the proximal tibia below the joint and above the head of the fibula) was defined as TT-PCL distance.
-
5.
Femoral posterior condylar angle was defined as the angle between the line drawn from the lateral epicondylar spike to the deepest point of the medial epicondylar sulcus (surgical transepicondylar axis, TEA) and the posterior condylar line as described by Hauschild et al. [16].
-
6.
The rotation of the tibial tubercle to the proximal tibia [31] described by Berger et al. [4] in order to measure tibial component rotation was measured as well. To determine rotation of the tibial tubercle, the geometric centre of the proximal tibia directly distal to the femorotibial joint and above the fibular head was located and superimposed to the level of the tibial tubercle. Then, the geometric centre of the proximal tibia and the tip of the tubercle were connected, giving the orientation of the tubercle. The angle between this line and a line perpendicular to the tangent of the posterior tibial margin of the posterior tibia in the section of the geometric tibial centre was measured and defined as the tibial tubercle–tibia angle (TTT).
-
7.
Tibiofemoral rotation angle (TFRA) was expressed using modified methods of Schneider and Tomczak [31, 33] as described by Salsich and Perman [30]. The angle formed by a line drawn tangent to the posterior femoral condyles and the horizontal section line was set as angle one. Angle two was determined as the angle between a line drawn tangent to the posterior tibia and the horizontal section line. The sections were chosen as described in points 1 and 2. Angle one minus angle two equals the TFRA, which represents external rotation of the tibia relative to the femur.
-
8.
Furthermore, neck–malleolar angle suggested by Liodakis et al. [24] was used for a second determination of overall rotational leg alignment. The difference between the upper ankle joint axis (as described in point 2)/horizontal section line angle and the FNA/horizontal section line angle was measured.
Statistical analysis
Continuous variables are presented as means and standard deviations. To analyse the impact of knee flexion and rotational limb alignment parameters on patellar mediolateral shift, epicondylar distance, rotation and tilt, linear mixed models were used. Flexion was used as a repeated effect, and the correlation structure between the degrees of flexion was specified as unstructured. All reported p values are two-sided, and a p value of 0.05 is considered the threshold of statistical significance. Due to the explorative nature of this study, no adjustment for multiple testing was done. Data entry and calculations were made with the software package SPSS 22.0 (IBM, Chicago, IL, USA), and the linear mixed model analyses were undertaken using the SAS 9.3 procedure PROC MIXED (SAS Institute, Cary, NC, USA).
Results
Rotational limb alignment parameters are presented by means and standard deviations (Table 1). The patellae displayed an increase in medial shift with increased tibiofemoral flexion in most knees. In contrast, knee #5 and #9 showed an increase in lateral shift throughout flexion, while in knee #1 and #7, the mediolateral shift of the patella remained steady (Fig. 2a; Table 2). While an almost linear decrease in epicondylar distance over flexion excursion was found (Fig. 2b; Table 2), a nearly linear increase in patellar external rotation could be observed in every knee (Fig. 2c; Table 2). Except in knee #10, the patellae tilted more laterally with increased flexion in a nearly linear behaviour as well. In knee #10, the patella tilted more medially from 50° to 80° of flexion (Fig. 2d; Table 2). Femoral posterior condylar angle showed a significant impact on epicondylar distance, rotation and tilt, but not on mediolateral shift. A decrease in femoral posterior condylar angle resulted in a decrease in epicondylar distance, an increased internal rotation as well as in an increased lateral tilt of the patella (Fig. 3a; Table 3). Femoral antetorsion showed a significant influence on patellar epicondylar distance and rotation. Increased femoral antetorsion resulted in an increased patellar internal rotation and a reduction in epicondylar distance (Fig. 3b; Table 3). With regard to patellar tilt and shift, no dependency on femoral antetorsion could be found. TT-TG influenced patellar epicondylar distance, rotation and tilt significantly, whereas no influence on mediolateral shift was seen. A decrease in TT-TG was followed by an increase in patellar internal rotation, a decrease in patellar epicondylar distance and lateral tilt (Fig. 3c; Table 3). Furthermore, a significant influence of TT-PCL on patellar mediolateral shift as well as on patellar rotation could be found. A decrease in TT-PCL led to increased internal patellar rotation and medial patellar shift (Fig. 3d; Table 3). With an increase in TFRA, the patella shifted more medially. No significant influence on remaining patellar kinematic parameters could be found for this rotational limb alignment parameter. The neck–malleolar angle showed a significant influence on patellar mediolateral shift and rotation. With increased neck–malleolar angle, the patella shifted more medially and rotated more externally. No influence on epicondylar distance and tilt was seen. Moreover, no influence of tibial torsion and tibia/tibial tubercle rotation on patellar kinematics was found. All significant values are presented in Table 3.
Discussion
The most important finding of the present investigation was that rotational limb alignment parameters have a significant influence on natural patellar kinematics. Using one measurement method, different rotational limb alignment parameters could be screened and their influence on patellar kinematics quantified. In the natural knee, the mediolateral shift of the patella from 30° to 90° of flexion ranged within 2 mm. The mean tilt was within 4°, while the mean patellar rotation was within 7°. In their investigation, Nha et al. [26] found a mean patella shift within 3 mm, a mean tilt within 6° and a mean total excursion of patellar rotation of 8° during full range of weight-bearing flexion. These relatively small patellar motion results can be confirmed, even though the mean total excursions in this study were smaller. This finding could be a result of the passive motion cycles instead of active ones. Patellar rotation and epicondylar distance showed a nearly steady and similar behaviour in every knee, whereas patellar tilt and mediolateral shift displayed a diverse motion excursion in some knees. Lateral tilt and external rotation of the patella increased continuously with increased tibiofemoral flexion in all knees, while lateral shift and epicondylar distance decreased in our investigation. Also, Heinert et al. [18] described a more lateral tilt and external rotation of the natural patella in higher flexion angles, but we could not confirm their findings of an increased patellar lateral shift with increased flexion. However, similar to our results, Kessler et al. [21] demonstrated a medial shift with increased tibiofemoral flexion and a nearly steady tilt behaviour in the natural knee in their biomechanical study. Furthermore, significant influence of TT-PCL distance on patellar mediolateral shift was found, while TT-TG distance showed no influence on patellar shift during whole flexion. Also, Seitlinger et al. [32] postulated in their radiological investigation that the TT-TG distance does not necessarily implicate a too laterally placed tibial tubercle and therefore a certain pathology. Furthermore, Dietrich et al. [9] demonstrated that the TT-TG distance increases significantly at the end-stage extension of the knee; therefore, the informative value of the TT-TG distance in different flexion angles is limited. Hence, our findings of missing significant influence of TT-TG on patellar mediolateral shift during different knee flexion angles support these investigations. Both TT-TG distance and TT-PCL distance influenced patellar rotation significantly. Additionally, patellar epicondylar distance and tilt showed a dependency on TT-PCL distance. A significant influence of femoral antetorsion on patellar rotation as well as on epicondylar distance could be displayed. An increased femoral antetorsion led to an increase in patellar internal rotation and a decrease in epicondylar distance, but did not show a significant influence on patellar shift or tilt. Airanow and Zippel [29] reported a significantly increased femoral antetorsion and increased TFRAs in patients suffering from patellar instability compared to healthy individuals in a CT study. In an MRI investigation, Diederichs et al. [8] also found that patients with a history of patellar dislocation have a greater femoral antetorsion compared to healthy controls. Thus, even though no correlation between femoral antetorsion and patellar shift or tilt was found, our results highlight the importance of femoral antetorsion affecting patellar kinematics and suggest that patellar rotation and epicondylar distance are reliable parameters to assess patellar kinematics. Femoral posterior condylar angle showed a significant influence on patellar epicondylar distance as well as on patellar rotation and tilt. A decrease in femoral posterior condylar angle resulted in an increase in patellar internal rotation and lateral tilt, while epicondylar distance was decreased. Many recent studies dealt with femoral posterior condylar angle in relation to femoral component alignment in TKA, but no study describing the influence of this rotational alignment parameter on natural patellar kinematics was found. Increased TFRA led to an increased medial patellar shift. Eckhoff et al. [10] reported a significantly increased tibiofemoral angle in patients suffering from anterior knee pain in their CT investigation. Furthermore, Salsich and Perman [30] reported a significant influence of TFRA on patellofemoral joint contact area in individuals with patellofemoral pain. No significant influence of tibial torsion and tibia–tibial tubercle rotation on patellar kinematics could be displayed in this investigation. Also, Diederichs et al. [8] reported no difference in tibial torsion between patients with experienced patella dislocation and healthy controls. As a very sensitive parameter on rotational limb alignment, patellar rotation should be considered in further biomechanical studies. In addition, patellar epicondylar distance seems to be a relevant kinematic parameter to quantify the anterior-posterior position of the patella during different flexion angles. Already in 1994, Dejour et al. [6] stressed the importance of the trochlea dysplasia and depth in knees with symptomatic patellar instability. This study has several limitations. First, we used Thiel-embalmed cadavers performing passive knee flexion. The cadaveric knees might not reproduce the kinematics of the knee from a living person performing an active flexion cycle with the influence of quadriceps muscle activity. To avoid differences in performed flexion cycles, a passive motion machine was used and three motion cycles were conducted. We did not investigate flexion angles between 0° and 30° of flexion. Therefore, we could not analyse a possible effect of the tibiofemoral “screw home mechanism” at early flexion angles and its influence on patellar kinematics. Furthermore, we used computer navigation system including a patella reference array for collecting kinematic data. Although optical computer navigation has been verified to be a reliable measurement tool to evaluate three-dimensional knee kinematics [15, 23], the patella reference array might have altered patellar kinematics caused by its own dynamics and centre of gravity. In order to register the landmarks needed by the navigation software for tibiofemoral and patellofemoral kinematics, arthrotomy of the knee capsule was necessary. Although the closure and reopening of the arthrotomy were conducted with great care and standardized locations for suturing the capsule were used, deviations to intact knees might have occurred. For generating rotational limb alignment parameters, only ten CT scan measurements for each parameter were used. However, for the linear regression models, patellar kinematic values in seven flexion angles from 30° to 90° were registered. Therefore, to correlate with rotational limb alignment measurements, seventy values for each patellar kinematic parameter were applied. Nevertheless, the results of the present investigation suggest to ascribe more importance to these rotational limb alignment parameters in terms of evaluating patellar maltracking of the natural knee as well as after TKA. Both component rotation and rotational limb alignment should be considered in diagnostic CT scans prior indicating a revision of TKA.
Conclusion
Rotational limb alignment has a major impact on patellar kinematics. Therefore, more importance should be ascribed to rotational limb alignment parameters in terms of clinical evaluation of patellar tracking and future biomechanical and clinical investigations regarding post-operative anterior knee pain in TKA.
References
Ahmed AM, Duncan NA (2000) Correlation of patellar tracking pattern with trochlear and retropatellar surface topographies. J Biomech Eng 122:652–660
Belvedere C, Catani F, Ensini A, de la Barrera JLM, Leardini A (2007) Patellar tracking during total knee arthroplasty: an in vitro feasibility study. Knee Surg Sports Traumatol Arthrosc 15:985–993
Bengs BC, Scott RD (2006) The effect of patellar thickness on intraoperative knee flexion and patellar tracking in total knee arthroplasty. J Arthroplasty 21:650–655
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Colwell CW Jr, Chen PC, D’Lima D (2011) Extensor malalignment arising from femoral component malrotation in knee arthroplasty: effect of rotating–bearing. Clin Biomech 26:52–57
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Dhollander A, Bassens D, Victor J, Verdonk P (2013) Patellar tilt and thickness do not influence postoperative flexion in a high-flex design total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2817–2822
Diederichs G, Köhlitz T, Kornaropoulos E, Heller MO, Vollnberg B, Scheffler S (2013) Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med 41:51–57
Dietrich TJ, Betz M, Pfirrmann CWA, Koch PP, Fucentese SF (2014) End-stage extension of the knee and its influence on tibial tuberosity-trochlear groove distance (TTTG) in asymptomatic volunteers. Knee Surg Sports Traumatol Arthrosc 22:214–218
Eckhoff DG, Brown AW, Kilcoyne RF, Stamm ER (1997) Knee version associated with anterior knee pain. Clin Orthop Relat Res 339:152–155
Elias J, Carrino J, Saranathan A, Guseila L, Tanaka M, Cosgarea A (2014) Variations in kinematics and function following patellar stabilization including tibial tuberosity realignment. Knee Surg Sports Traumatol Arthrosc 22:2350–2356
Feller JA, Amis AA, Andrish JT, Arendt EA, Erasmus PJ, Powers CM (2007) Surgical biomechanics of the patellofemoral joint. Arthrosc J Arthrosc Relat Surg 23:542–553
Ficat P (1970) Pathologie femoro-patellaire. Masson et Cie, Paris
Fujikawa K, Seedhom BB, Wright V (1983) Biomechanics of the patello-femoral joint. Part II: a study of the effect of simulated femoro-tibial varus deformity on the congruity of the patello-femoral compartment and movement of the patella. Eng Med 12:13–21
Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15:970–973
Hauschild O, Muenzberg M, Knothe D, Konstantinidis L, Helwig P, Sudkamp NP, Thielemann FW (2013) Rotational limb alignment changes following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2346–2354
Heegaard J, Leyvraz PF, Curnier A, Rakotomanana L, Huiskes R (1995) The biomechanics of the human patella during passive knee flexion. J Biomech 28:1265–1279
Heinert G, Kendoff D, Preiss S, Gehrke T, Sussmann P (2011) Patellofemoral kinematics in mobile-bearing and fixed-bearing posterior stabilised total knee replacements: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 19:967–972
Jend HH, Heller M, Dallek M, Schoettle H (1981) Measurement of tibial torsion by computer tomography. Acta Radiol Diagn 22:271–276
Van Kampen A, Huiskes R (1990) The three-dimensional tracking pattern of the human patella. J Orthop Res 8:372–382
Kessler O, Patil S, Colwell CW Jr, D’Lima DD (2008) The effect of femoral component malrotation on patellar biomechanics. J Biomech 41:3332–3339
Koh TJ, Grabiner MD, De Swart RJ (1992) In vivo tracking of the human patella. J Biomech 25:637–643
Lee D-H, Park J-H, Song D-I, Padhy D, Jeong W-K, Han S-B (2010) Accuracy of soft tissue balancing in TKA: comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc 18:381–387
Liodakis E, Aljuneidi W, Krettek C, Ettinger M, Kenawey M (2011) The neck–malleolar angle: an alternative method for measuring total lower limb torsion that considers the knee joint rotation angle. Skeletal Radiol 40:617–621
Murphy S, Simon S, Kijewski P, Wilkinson R, Griscom N (1987) Femoral anteversion. J Bone Joint Surg 69:1169–1176
Nha KW, Papannagari R, Gill TJ, Van de Velde SK, Freiberg AA, Rubash HE, Li G (2008) In vivo patellar tracking: clinical motions and patellofemoral indices. J Orthop Res 26:1067–1074
Ostermeier S, Buhrmester O, Hurschler C, Stukenborg-Colsman C (2005) Dynamic in vitro measurement of patellar movement after total knee arthroplasty: an in vitro study. BMC Musculoskelet Disord 6:30
Reikerås O (1992) Patellofemoral characteristics in patients with increased femoral anteversion. Skeletal Radiol 21:311–313
Airanow S, Zippel H (1990) Femoro-tibial torsion in patellar instability. A contribution to the pathogenesis of recurrent and habitual patellar dislocations. Orthop Traumatol 37:311–316
Salsich GB, Perman WH (2007) Patellofemoral joint contact area is influenced by tibiofemoral rotation alignment in individuals who have patellofemoral pain. J Orthop Sports Phys Ther 37:521–528
Schneider B, Laubenberger J, Jemlich S, Groene K, Weber HM, Langer M (1997) Measurement of femoral antetorsion and tibial torsion by magnetic resonance imaging. Br J Radiol 70:575–579
Seitlinger G, Scheurecker G, Högler R, Labey L, Innocenti B, Hofmann S (2012) Tibial tubercle-posterior cruciate ligament distance a new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med 40:1119–1125
Tomczak RJ, Guenther KP, Rieber A, Mergo P, Ros PR, Brambs HJ (1997) MR imaging measurement of the femoral antetorsional angle as a new technique: comparison with CT in children and adults. Am J Roentgenol 168:791–794
Veress SA, Lippert FG, Hou MCY, Takamoto T (1979) Patellar tracking patterns measurement by analytical X-ray photogrammetry. J Biomech 12:639–650
Acknowledgments
We would like to thank Depuy, Germany, and Brainlab, Germany, for their technical and logistical support for this study. Furthermore, we would like to thank the Institute of Anatomy at the Medical University of Graz, Austria, to provide the specimen for this investigation.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keshmiri, A., Maderbacher, G., Baier, C. et al. Significant influence of rotational limb alignment parameters on patellar kinematics: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24, 2407–2414 (2016). https://doi.org/10.1007/s00167-014-3434-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3434-2