Abstract
Ischemic stroke is the major contributor to morbidity and mortality in people with diabetes mellitus. In ischemic stroke patients, neuroinflammation is now understood to be one of the main underlying mechanisms for cerebral damage and recovery delay. It has been well-established that toll-like receptor 4 (TLR4) signaling pathway plays a key role in neuroinflammation. Emerging research over the last decade has revealed that, compared to ischemic stroke without diabetes mellitus, ischemic stroke with diabetes mellitus significantly upregulates TLR4-mediated neuroinflammation, increasing the risk of cerebral and neuronal damage as well as neurofunctional recovery delay. This review aims to discuss how ischemic stroke with diabetes mellitus amplifies TLR4-mediated neuroinflammation and its consequences. Additionally covered in this review is the potential application of TLR4 antagonists in the management of diabetic ischemic stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is a serious condition that impairs social, familial, and individual well-being on a global level. As of 2019, stroke is the second leading cause of death worldwide [1]. Stroke can be classified into two types: ischemic stroke and hemorrhagic stroke, accounting for ~ 85% and ~ 15% of all cases, respectively [2]. Diabetes, obesity, hypertension, sedentary lifestyle, smoking, dyslipidemia, and cardiac conditions such as atrial fibrillation are the major modifiable risk factors for ischemic stroke [3].
Diabetes and diabetes-related risk factors are well known to develop pathological deteriorations in the blood vessels of the human body, leading to various subtypes of ischemic stroke if the brain blood vessels are pathologically impacted by the condition, with the middle cerebral arteries being the most commonly affected [4]. People with diabetes have a nearly 2-fold greater chance of experiencing an ischemic stroke compared to those without the disease [5]. Ischemic stroke can also result in glucose metabolism disorders, which can, in turn, exacerbate the brain damage and delay brain functional recovery [6]. In comparison to ischemic stroke patients without diabetes, those with uncontrolled high blood sugar levels had worse acute stroke outcomes, as well as a higher risk of mortality and stroke recurrence [7].
To date, tissue plasminogen activator is the only medication approved for the treatment of ischemic stroke, and it must be administered within 4.5 h of the stroke onset [8, 9]. However, the administration of tissue plasminogen activator after the ischemic stroke may raise the chance of intracerebral hemorrhage [10]. As an alternative to tissue plasminogen activator, mechanical thrombectomy, which removes the thrombus occluded in large arteries, has been used to treat ischemic stroke [11]. Mechanical thrombectomy, on the other hand, is not an option for ischemic stroke patients who have small artery or multiple arteries occlusions, as well as inadequate collateral circulation. Although tissue plasminogen activator and mechanical thrombectomy are both effective first-line treatments for ischemic stroke, it is crucial to remember that neither treatment specifically targets the cellular injury mechanisms due to ischemic stroke; rather, both only aim to improve cerebral blood flow in stroke patients. Thus, an understanding of the molecular mechanisms involved in the pathophysiology of the ischemic stroke concomitant with diabetes (hereafter referred to as “diabetic stroke”) could make a significant contribution to the development of potential therapeutics to lessen neuronal death and damage after the diabetic stroke patients.
Growing evidence shows that the innate immune system initiates the protracted inflammatory cascade that is the primary etiology of cerebral damage and brain functional recovery delay in diabetic stroke [12,13,14]. As a part of the innate neuroimmune system, pattern recognition receptors (PRRs) such as toll-like receptors (TLRs) have been shown to play a significant role in the development of neuroinflammation [15]. Over the past ten years, a number of studies have demonstrated that the TLR4 signaling pathway is crucial for the pathogenesis of neuroinflammation and subsequent brain pathologies [16, 17]. Although the evidence linking TLR4-mediated neuroinflammation to cerebral damage and brain functional recovery delay in diabetic stroke patients is still limited, pre-clinical studies have shown that TLR4-mediated neuroinflammation significantly contributes to the escalation of cerebral damage and brain functional recovery delay following a diabetic stroke [18, 19]. This review intends not only to provide an overview of recent findings on TLR4-mediated neuroinflammatory process but also to discuss how TLR4-mediated neuroinflammatory process exacerbates the cerebral damage and delays brain functional recovery in the diabetic stroke.
General aspect of TLR4 signaling pathway in neuroinflammation
TLR4, the first mammalian toll-like receptor identified, is traditionally an innate immune receptor that is primarily found on neuroimmune cells like microglia and astrocytes, in addition to neurons, oligodendrocytes, and blood-brain barrier (BBB) endothelial cells [20]. Being an immune receptor, TLR4 functions as a PRR with its vital co-receptor, myeloid differentiation factor 2, recognizing the pathogen-associated molecular pattern like lipopolysaccharide, and then releasing the inflammatory cytokines to kill the invading pathogens [21]. Additionally, the damage-associated molecular pattern (DAMP), such as heat shock protein and high mobility group box 1 (HMGB1), can also prompt the TLR4 signaling pathway to be activated [22]. Once the ligands bind to the TLR4, the intracellular adaptor molecules are recruited: toll-interleukin-1 receptor domain-containing adaptor protein-inducing interferon (TRIF), TRIF-related adaptor molecule (TRAM), myeloid differentiation primary response protein 88 (MyD88), and MyD88-adaptor-like (MAL) protein, resulting in MyD88 dependent and independent intracellular pathways activation and inflammatory cytokines release, leading to neuroinflammation [17, 21].
Neuroinflammation typically emerges as a beneficial protective immune response, but if this immune response is unregulated and prolonged over a certain period, it can become harmful. Pre-clinical and clinical studies have both shown that persistent TLR4-mediated neuroinflammation is a major contributor to a variety of brain pathologies and cerebral damage [16,17,18, 20, 23].
Diabetes as a risk factor for stroke
Diabetes mellitus is caused by a loss of functional pancreatic islet beta-cell mass. According to the American Diabetes Association, type 1 diabetes is a chronic autoimmune disease characterized by the absolute insulin deficiency as a consequence of loss of pancreatic islet beta-cells, while type 2 diabetes is characterized by the progressively impaired pancreatic islet beta-cells usually in the presence of pre-existing insulin resistance [24]. An estimated 136 million adults, or 19.5% of the adult population aged 65 to 99, were diagnosed with diabetes in 2019. This figure is expected to rise to 195 million by 2030, and 276.2 million by 2045 [25]. Type 1 diabetes affects 5–10% of those diagnosed [26], while type 2 diabetes accounts for 90% of all cases [27].
Type 1 diabetes is the most prevalent form of diabetes in children under the age of 15, with a peak incidence rate at the age of 12–14 [28]. There are two types of type 1 diabetes: pre-symptomatic type 1 diabetes characterized by lower β-cell mass without symptoms, and symptomatic type 1 diabetes characterized by hyperglycemia symptoms including hunger, thirst, polyuria, and weight loss). Furthermore, type 1 diabetes can be divided into three stages: stage 1 is characterized by the presence of autoantibodies but not hyperglycemia; stage 2 is characterized by the presence of both autoantibodies and hyperglycemia; and stage 3 is characterized by hyperglycemic symptoms, which is a form of symptomatic type 1 diabetes [29].
Type 2 diabetes, which is far more common than type 1 diabetes (accounting for 90% of all cases), is characterized by dysregulation of protein, lipid, and carbohydrate metabolism, and triggered by insulin resistance, impaired insulin secretion, or a combination of the two [30]. The pathophysiology of type 2 diabetes mellitus is significantly influenced by adipose tissue, as the majority of affected individuals have central visceral adiposity and obesity. Type 2 diabetes has a wide range of underlying pathophysiology, clinical presentation, and disease progression, and atypical symptoms can complicate type 2 diabetes classification [30].
A common outcome of type 1 and type 2 diabetes mellitus is hyperglycemia. Long-term hyperglycemia in chronic type 1 and type 2 diabetes can lead to severe cerebrovascular complications, including strokes [31]. Diabetes was linked to hazard ratios of 1.84 for unclassified stroke, 1.56 for hemorrhagic stroke, and 2.27 for ischemic stroke, per the Emerging Risk Factors Collaboration [32]. A 34% increase in ischemic stroke was observed in diabetic subjects (CI 1.11-162) among the over 41,000 patients registered in the Lausanne Stroke Registry [33]. A prospective Japanese study found that the incidence of all types of ischemic stroke was two to four times higher in male and female diabetic subjects, with no correlation to subarachnoid or intraparenchymal hemorrhage [34]. Diabetes increases the risk of ischemic stroke-related morbidity, mortality, and brain damage, but it is unclear what underlying factors exacerbate the ischemic stroke.
Diabetic stroke, TLR4-mediated neuroinflammation, and cerebral reperfusion
Diabetes is a type of metabolic disease characterized by high blood sugar levels. A growing body of evidence suggests that high blood sugar levels in diabetes activate TLR4 signaling pathway, triggering systemic and brain inflammation [35, 36]. Furthermore, impaired insulin function in diabetes enhances lipolysis and free fatty acid release, which activates TLR4 signaling, resulting in systemic inflammation [37]. Also, hyperglycemic-induced oxidative stress in diabetes activates TLR4 signaling pathway and initiates the oxidative-inflammatory vicious cycle [38]. The risk for suffering from a diabetic stroke rises as a result of the systemic metabolic and inflammatory cascades as well as oxidative stress, all of which contribute to diabetes-induced vascular complications [39].
An ischemic stroke happens when cerebral vascularization is decreased or interrupted, causing a disruption in the supply of oxygen and glucose to the brain that propagates cerebral homeostasis impairments, ultimately leading to neuronal injury and death [40, 41]. It has been reported that uncontrolled blood sugar level with a history of diabetes exacerbates cerebral ischemic injury and leads to poorer functional outcomes [7]. In the last decade, a growing body of research indicates that the cerebral damage in diabetic stroke is reported to be significantly greater than ischemic stroke without diabetes due to exacerbated brain inflammation via TLR4 signaling pathway. Although the underlying pathological mechanisms of diabetic stroke are still poorly understood, pre-clinical research has shown a strong link between diabetic stroke and TLR4-mediated neuroinflammation, which delays brain functional recovery after diabetic stroke [12, 18, 19, 42,43,44,45].
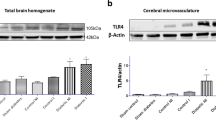
Ning et al. [42] reported that TLR4 expressions in the ischemic brain area of diabetic rats were significantly increased after 48 h of ischemic stroke compared to those in ischemic stroke with non-diabetic rats. Kurita and colleagues discovered that after 7 days of ischemic stroke, TLR4-mediated neuroinflammation in ischemic brain area of db/db mice was significantly higher than those in ischemic stroke with db/+ mice [43]. Similarly, Ye and colleagues demonstrated that TLR4 expressions were significantly higher in ischemic brain area of diabetic rats following 14 days of ischemic stroke compared to those of ischemic stroke with non-diabetic rats [12]. Pre-clinical studies have shown that diabetic stroke is associated with a markedly higher level of TLR4-mediated neuroinflammation, which can persist for up to 14 days after an ischemic stroke [12, 42, 43]. Short-term neuroinflammatory response can be beneficial for removing the damaged tissue in ischemic brain, but long-term neuroinflammatory response may harm the surrounding tissue of ischemic brain [46]. To date, pre-clinical studies have been extensively conducted to develop novel therapeutic approaches to reduce the TLR4 signaling pathway activity after diabetic stroke [13, 44, 45].
Restoring cerebral blood flow to the ischemic brain is a crucial first step in the treatment of ischemic stroke [47, 48]. However, reperfusion itself can harm the ischemic brain due to an increase in neuroinflammation and brain oxidative stress [44, 49]. Furthermore, high blood glucose level in diabetes aggravates cerebral reperfusion injury [50]. This review also compiles preclinical research demonstrating that cerebral reperfusion after a diabetic stroke significantly amplifies TLR4-mediated neuroinflammation compared to it does following a normoglycemic stroke.
Zhang et al. [44] reported that TLR4-mediated neuroinflammation is significantly higher after cerebral reperfusion for 24 h in diabetic stroke compared to those in ischemic stroke without diabetes. Interestingly, after 48 h of cerebral reperfusion, TLR4 expressions in ischemic brain area of diabetic stroke were significantly increased compared to those of ischemic stroke with normoglycemia [45, 51]. A growing body of evidence demonstrated that cerebral reperfusion for 72 h in diabetic stroke significantly increased TLR4-mediated neuroinflammation in comparison to ischemic stroke without diabetes [18, 19, 52]. The standard therapeutic strategy for treating ischemic stroke is prompt blood vessel recanalization; however, pre-clinical studies show that reperfusion in diabetic stroke amplifies TLR4-mediated neuroinflammation. Table 1 shows the evidence of TLR4-mediated neuroinflammation in experimental diabetic stroke models.
Inflammatory mediators of TLR4-mediated neuroinflammation and secondary complications in diabetic stroke
In the early stages of diabetic stroke, the death neurons passively secrete DAMPs like HMGB1 into the extracellular space of the nervous system [19, 52], where they are then released into the peripheral circulation. Following an ischemic stroke, the level of HMGB1 in the peripheral blood is markedly increased within 24 h and can rise by as much as 13 times, reflecting the degree of HMGB1 expression in the nervous system [53]. Similarly, Kim et al. [51] demonstrated that serum HMGB1 level was significantly increased in the diabetic stroke rodent model. Ischemic stroke-induced extracellular HMGB1 functions as a pro-inflammatory factor, activating not only cerebral immune cells such as microglia and astrocytes, but also recruiting systemic immune cells in the brain via the TLR4 signaling pathway, resulting in brain inflammation [54]. In addition, active secretions of HMGB1 occur when brain immune cells are activated in response to an ischemic stroke, aggravating TLR4-mediated brain inflammation [9, 55]. Once HMGB1 binds to TLR4 receptor, it activates nuclear factor kappa B (NF-KB) which leads to enhance the levels of pro-inflammatory cytokines such as tumor necrosis factor alpha (TNF-α) and interleukin 6 (IL-6), as well as matrix metalloproteinase 9 (MMP-9) [52]. Moreover, TLR4 upregulates NLR family pyrin domain containing 3 (NLRP3) inflammasome formation which contributes to amplifies brain inflammation and provoke neuronal cell death in the ischemic brain [44].
In the brain, inflammatory cytokines were already elevated at baseline in diabetic conditions before the ischemic event [56]. The inflammatory cytokines produced as a result of the ischemic condition and those already present due to diabetes intensify brain immune cells activation and TLR4-mediated neuroinflammation in diabetic stroke [12, 42, 51, 52]. Experimental and clinical studies have shown that the infiltration of systemic immune cells, such as neutrophils, lymphocytes, and monocytes, also aggravates neuroinflammation and neuronal cell death in ischemic stroke [57,58,59,60,61,62]. During the early phase of cerebral ischemia, reactive oxygen species (ROS) and pro-inflammatory agents like cytokines, chemokines, and DAMPs are released by damaged brain tissue, and these substances encourage the adherence and trans-endothelial transfer of systemic immune cells by upregulating the adhesion molecules on cerebral endothelial cells as well as systemic immune cells [63].
Following the early stages of ischemic stroke, the infiltrated systemic immune cells release additional cytokines and chemokines, creating the oxidative inflammatory vicious cycle that stimulates MMP-9 production [64]. The increased MMP-9 level in diabetic stroke intensifies the neuroinflammatory process and significantly contributes to BBB disruption [12, 42]. Once the BBB has been disrupted, the ruptured BBB provides a significant entry point for the invasion of peripheral inflammatory cells into the cerebral ischemic area [65]. Furthermore, blood serum leaks into the brain through the compromised BBB, causing brain oedema, an increase in brain water content, a larger infarct size, and hemorrhagic transformation of cerebral infarct in diabetic stroke, all of which contribute to impaired brain functions and neurological deficits [12, 42, 51, 52]. The pathophysiology of TLR4-mediated neuroinflammation in diabetic stroke and its consequences are illustrated in Fig. 1.
Pathophysiology of TLR4-mediated neuroinflammation in diabetic stroke and its consequences. In diabetes, hyperglycemia amplifies systemic inflammation and oxidative stress, both of which induce TLR4-mediated neuroinflammation. In addition, diabetes-related metabolic changes cause vascular damage that can result in an ischemic stroke. Increased level of HMGB1 due to neuronal death in ischemic stroke induces TLR4-mediated neuroinflammation which can consequently induce several brain pathologies. Moreover, reperfusion injury in ischemic stroke amplifies TLR4-mediated neuroinflammation and its consequences. In diabetic stroke, diabetes-related systemic pathologies amplify TLR4-mediated neuroinflammation, which can lead to numerous brain pathologies and functional recovery delay. HMGB1, high mobility group box 1; TLR4, toll-like receptor 4
TLR4-mediated neuroinflammation, along with its secondary complications, thus significantly influences on neurofunctional impairments and lowers the chance of survival in diabetic stroke [18, 19, 42,43,44, 52]. Furthermore, diabetes-related vascular impairments such as arterial stiffness are one of the factors that trigger neuronal death and functional recovery delay following an ischemic stroke [66]. To date, the results of experimental studies highlight the impact of TLR4-mediated neuroinflammation on cerebral damage and secondary complications in diabetic stroke [18, 19, 42,43,44, 52]. The harmful consequences arise in diabetic stroke when proper resolution does not apply. Thus, targeting TLR4 piques researchers’ interest as a potential therapeutic approach for diabetic stroke.
Potential roles of TLR4 antagonist in diabetic stroke
Numerous studies have shown that the TLR4 signaling pathway plays an important role in the pathophysiology of stroke [67,68,69]. Kilic and colleagues demonstrated that TLR4 knockout mice had the significant reduction in brain infarct size during focal cerebral ischemia [70]. In the study conducted by Hua and co-workers, systemic administration of TAK-242, TLR4 antagonist, after experimental stroke significantly reduced cerebral infarct, TLR4-mediated neuroinflammation, and improved neurological function [71]. Parada et al. [72] found that systemic administration of eritoran, TLR4 inhibitor, after cerebral ischemia significantly attenuated cerebral infarct size, BBB disruption, neuroinflammation, and neurological deficits.
To date, evidences regarding the pharmacological intervention of TLR4 antagonists in diabetic stroke are still limited. Abdul et al. [18] reported that systemic administration of TAK242 after diabetic stroke improves BBB integrity and neurofunctional outcome. Interestingly, Li and colleagues showed that systemic administration of TAK-242 after diabetic stroke significantly reduced cerebral infarct, cerebral oedema, brain oxidative stress, neuronal apoptosis, neuroinflammation, and neurological deficits [73]. The experimental studies demonstrated that pharmacological interventions targeting TLR4 might have a significant positive impact in diabetic stroke [18, 73]; however, in order to be effective in humans, these interventions should be able to promote resolution and an anti-inflammatory phenotype rather than completely suppress inflammation.
Clinical translation of diabetic stroke treatment: challenges
Although experimental studies have improved our comprehension of brain physiology and the pathophysiology of diabetic stroke, clinical application of this knowledge is challenging and frequently falls short. The primary causes are the structural and functional distinctions between the human brain and that of experimental animals, as well as the metabolic functions. Furthermore, human disease cannot be easily compared to experimental animal stroke models due to the complexity of human disease pathophysiology and co-morbidities. Clinical trials are therefore eventually depended upon to offer significant insights into human diabetes and its treatments. When analyzing data from animal studies, researchers need to be aware of these limitations and take them into consideration. Moreover, it is crucial to reproduce the pathophysiology of the disease in lab animals when developing models that resemble diabetes. Since damage to pancreatic β-cells can result in both types of diabetes, injecting streptozotocin into a particular model can kill pancreatic beta cells and mimic type 1 and later stages of type 2 diabetes. In addition, the neurobehavioral assessment techniques used in experimental animal models provide limited relevance for human neurobehavioral outcomes, making it impossible to compare human and animal neurobehavioral outcomes. In order for the findings of experimental neuroscience to be applied clinically, it is necessary to develop neurobehavioral assessment techniques for experimental animals that can be equally relevant to human neurobehavioral functions. However, animal models have made a substantial contribution to our understanding of the pathophysiology of diabetes, even in spite of these limitations.
Conclusion
Diabetes is a well-known high-risk factor for ischemic stroke. The experimental studies conducted in the previous decade highlight that in diabetic stroke, TLR4-mediated brain inflammation due to various inflammatory cell responses contributes to significant cerebral damage and neurofunctional recovery delay. Although there are currently few experimental studies that demonstrate the beneficial effects of TLR4 antagonists on diabetic stroke, the promising findings will encourage more research focusing on the potential benefits of novel TLR4 antagonists or the anti-inflammatory phenotypes for the treatment of diabetic stroke. In addition, developing the experimental models as well as optimizing the neurofunctional assessments in animals are also necessary for the translation of experimental neuroscience to clinical application in diabetic stroke. There are still a lot of significant unanswered questions, but the useful information gleaned from animal experiments and upcoming clinical trials will eventually lead to the development of therapies that lessen the impact of diabetic stroke.
Availability of data and material
Not applicable.
References
Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG, Abbasifard M, Abbasi-Kangevari M, Abd-Allah F, Abedi V et al (2021) Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 20(10):795–820. https://doi.org/10.1016/s1474-4422(21)00252-0
Musuka TD, Wilton SB, Traboulsi M, Hill MD (2015) Diagnosis and management of acute ischemic stroke: speed is critical. CMAJ 187(12):887–893. https://doi.org/10.1503/cmaj.140355
Simons LA, McCallum J, Friedlander Y, Simons J (1998) Risk factors for ischemic stroke. Stroke 29(7):1341–1346. https://doi.org/10.1161/01.STR.29.7.1341
Banerjee C, Chimowitz MI (2017) Stroke caused by atherosclerosis of the major intracranial arteries. Circ Res 120(3):502–513. https://doi.org/10.1161/circresaha.116.308441
Mosenzon O, Cheng AYY, Rabinstein AA, Sacco S (2023) Diabetes and stroke: what are the connections? J Stroke 25(1):26–38. https://doi.org/10.5853/jos.2022.02306
Kruyt ND, Nys GM, van der Worp HB, van Zandvoort MJ, Kappelle LJ, Biessels GJ (2008) Hyperglycemia and cognitive outcome after ischemic stroke. J Neurol Sci 270(1–2):141–147. https://doi.org/10.1016/j.jns.2008.02.020
Luitse MJ, Biessels GJ, Rutten GE, Kappelle LJ (2012) Diabetes, hyperglycaemia, and acute ischaemic stroke. Lancet Neurol 11(3):261–271. https://doi.org/10.1016/s1474-4422(12)70005-4
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359(13):1317–1329. https://doi.org/10.1056/NEJMoa0804656
Huang H, Oo TT, Apaijai N, Chattipakorn N, Chattipakorn SC (2023) An updated review of mitochondrial transplantation as a potential therapeutic strategy against cerebral ischemia and cerebral ischemia/reperfusion injury. Mol Neurobiol 60(4):1865–1883. https://doi.org/10.1007/s12035-022-03200-y
Donnan GA, Fisher M, Macleod M, Davis SM (2008) Stroke. The lancet 371(9624):1612–1623. https://doi.org/10.1016/S0140-6736(08)60694-7
Berlis A, Lutsep H, Barnwell S, Norbash A, Wechsler L, Jungreis CA, Woolfenden A, Redekop G, Hartmann M, Schumacher M (2004) Mechanical thrombolysis in acute ischemic stroke with endovascular photoacoustic recanalization. Stroke 35(5):1112–1116. https://doi.org/10.1161/01.STR.0000124126.17508.d3
Ye X, Chopp M, Liu X, Zacharek A, Cui X, Yan T, Roberts C, Chen J (2011) Niaspan reduces high-mobility group box 1/receptor for advanced glycation endproducts after stroke in type-1 diabetic rats. Neuroscience 190:339–345. https://doi.org/10.1016/j.neuroscience.2011.06.004
Ning R, Chopp M, Zacharek A, Yan T, Zhang C, Roberts C, Lu M, Chen J (2014) Neamine induces neuroprotection after acute ischemic stroke in type one diabetic rats. Neuroscience 257:76–85. https://doi.org/10.1016/j.neuroscience.2013.10.071
Venkat P, Yan T, Chopp M, Zacharek A, Ning R, Van Slyke P, Dumont D, Landschoot-Ward J, Liang L, Chen J (2018) Angiopoietin-1 mimetic peptide promotes neuroprotection after stroke in type 1 diabetic rats. Cell Transplant 27(12):1744–1752. https://doi.org/10.1177/0963689718791568
Kigerl KA, de Rivero Vaccari JP, Dietrich WD, Popovich PG, Keane RW (2014) Pattern recognition receptors and central nervous system repair. Exp Neurol 258:5–16. https://doi.org/10.1016/j.expneurol.2014.01.001
Oo TT, Sumneang N, Ongnok B, Arunsak B, Chunchai T, Kerdphoo S, Apaijai N, Pratchayasakul W, Liang G, Chattipakorn N et al (2022) L6H21 protects against cognitive impairment and brain pathologies via toll-like receptor 4-myeloid differentiation factor 2 signalling in prediabetic rats. Br J Pharmacol 179(6):1220–1236. https://doi.org/10.1111/bph.15741
Huang NQ, Jin H, Zhou SY, Shi JS, Jin F (2017) TLR4 is a link between diabetes and Alzheimer’s disease. Behav Brain Res 316:234–244. https://doi.org/10.1016/j.bbr.2016.08.047
Abdul Y, Abdelsaid M, Li W, Webb RC, Sullivan JC, Dong G, Ergul A (2019) Inhibition of Toll-Like Receptor-4 (TLR-4) Improves neurobehavioral outcomes after acute ischemic stroke in diabetic rats: possible role of vascular endothelial TLR-4. Mol Neurobiol 56(3):1607–1617. https://doi.org/10.1007/s12035-018-1184-8
Li Y, Yao N, Zhang T, Guo F, Niu X, Wu Z, Hou S (2020) Ability of post-treatment glycyrrhizic acid to mitigate cerebral ischemia/reperfusion injury in diabetic mice. Med Sci Monit 26:e926551. https://doi.org/10.12659/MSM.926551
Oo TT, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2022) Emerging roles of toll-like receptor 4 in chemotherapy-induced neurotoxicity. Neurotoxicology 93:112–127. https://doi.org/10.1016/j.neuro.2022.09.006
Oo TT, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2020) Potential roles of myeloid differentiation factor 2 on neuroinflammation and its possible interventions. Mol Neurobiol 57(11):4825–4844. https://doi.org/10.1007/s12035-020-02066-2
Lee K-M, Seong S-Y (2009) Partial role of TLR4 as a receptor responding to damage-associated molecular pattern. Immunol Lett 125(1):31–39. https://doi.org/10.1016/j.imlet.2009.05.006
Pandey GN, Rizavi HS, Bhaumik R, Ren X (2019) Innate immunity in the postmortem brain of depressed and suicide subjects: role of toll-like receptors. Brain Behav Immun 75:101–111. https://doi.org/10.1016/j.bbi.2018.09.024
Committee ADAPP (2021) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2022. Diabetes Care 45(Supplement_1):S17–S38. https://doi.org/10.2337/dc22-S002
Sinclair A, Saeedi P, Kaundal A, Karuranga S, Malanda B, Williams R (2020) Diabetes and global ageing among 65–99-year-old adults: findings from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract 162:108078. https://doi.org/10.1016/j.diabres.2020.108078
American Diabetes Association (2009) Diagnosis and classification of diabetes mellitus. Diabetes Care 32(Suppl 1):S62–67. https://doi.org/10.2337/dc09-S062
Chen L, Magliano DJ, Zimmet PZ (2011) The worldwide epidemiology of type 2 diabetes mellitus–present and future perspectives. Nat Rev Endocrinol 8(4):228–236. https://doi.org/10.1038/nrendo.2011.183
Patterson CC, Dahlquist GG, Gyürüs E, Green A, Soltész G (2009) Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20: a multicentre prospective registration study. Lancet 373(9680):2027–2033. https://doi.org/10.1016/s0140-6736(09)60568-7
Katsarou A, Gudbjörnsdottir S, Rawshani A, Dabelea D, Bonifacio E, Anderson BJ, Jacobsen LM, Schatz DA, Lernmark Å (2017) Type 1 diabetes mellitus. Nat Rev Dis Primers 3(1):17016. https://doi.org/10.1038/nrdp.2017.16
DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, Hu FB, Kahn CR, Raz I, Shulman GI et al (2015) Type 2 diabetes mellitus. Nat Rev Dis Primers 1(1):15019. https://doi.org/10.1038/nrdp.2015.19
Maida CD, Daidone M, Pacinella G, Norrito RL, Pinto A, Tuttolomondo A (2022) Diabetes and Ischemic Stroke: An Old and New Relationship an Overview of the Close Interaction between These Diseases. Int J Mol Sci 23(4):2397. https://doi.org/10.3390/ijms23042397
Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M et al (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375(9733):2215–2222. https://doi.org/10.1016/s0140-6736(10)60484-9
Karapanayiotides T, Piechowski-Jozwiak B, van Melle G, Bogousslavsky J, Devuyst G (2004) Stroke patterns, etiology, and prognosis in patients with diabetes mellitus. Neurology 62(9):1558–1562. https://doi.org/10.1212/01.wnl.0000123252.55688.05
Cui R, Iso H, Yamagishi K, Saito I, Kokubo Y, Inoue M, Tsugane S (2011) Diabetes mellitus and risk of stroke and its subtypes among Japanese: the Japan public health center study. Stroke 42(9):2611–2614. https://doi.org/10.1161/strokeaha.111.614313
Wang L, Wang J, Fang J, Zhou H, Liu X, Su SB (2015) High glucose induces and activates Toll-like receptor 4 in endothelial cells of diabetic retinopathy. Diabetol Metab Syndr 7(1):89. https://doi.org/10.1186/s13098-015-0086-4
Kawamoto EM, Cutler RG, Rothman SM, Mattson MP, Camandola S (2014) TLR4-dependent metabolic changes are associated with cognitive impairment in an animal model of type 1 diabetes. Biochem Biophys Res Commun 443(2):731–737. https://doi.org/10.1016/j.bbrc.2013.12.039
Rohm TV, Meier DT, Olefsky JM, Donath MY (2022) Inflammation in obesity, diabetes, and related disorders. Immunity 55(1):31–55. https://doi.org/10.1016/j.immuni.2021.12.013
Carrillo-Sepulveda MA, Spitler K, Pandey D, Berkowitz DE, Matsumoto T (2015) Inhibition of TLR4 attenuates vascular dysfunction and oxidative stress in diabetic rats. J Mol Med 93(12):1341–1354. https://doi.org/10.1007/s00109-015-1318-7
Forbes JM, Cooper ME (2013) Mechanisms of diabetic complications. Physiol Rev 93(1):137–188. https://doi.org/10.1152/physrev.00045.2011
Feske SK (2021) Ischemic stroke. Am J Med 134(12):1457–1464. https://doi.org/10.1016/j.amjmed.2021.07.027
Lakhan SE, Kirchgessner A, Hofer M (2009) Inflammatory mechanisms in ischemic stroke: therapeutic approaches. J Transl Med 7(1):97. https://doi.org/10.1186/1479-5876-7-97
Ning R, Chopp M, Yan T, Zacharek A, Zhang C, Roberts C, Cui X, Lu M, Chen J (2012) Tissue plasminogen activator treatment of stroke in type-1 diabetes rats. Neuroscience 222:326–332. https://doi.org/10.1016/j.neuroscience.2012.07.018
Kurita N, Yamashiro K, Kuroki T, Tanaka R, Urabe T, Ueno Y, Miyamoto N, Takanashi M, Shimura H, Inaba T et al (2020) Metabolic endotoxemia promotes neuroinflammation after focal cerebral ischemia. J Cereb Blood Flow Metab 40(12):2505–2520. https://doi.org/10.1177/0271678X19899577
Zhang YJ, Guo WJ, Tang ZY, Lin HB, Hong P, Wang JW, Huang XX, Li FX, Xu SY, Zhang HF (2022) Isoflurane attenuates cerebral ischaemia-reperfusion injury via the TLR4-NLRP3 Signalling Pathway in Diabetic Mice. Oxid Med Cell Longev 2022:2650693. https://doi.org/10.1155/2022/2650693
Yang WC, Li TT, Wan Q, Zhang X, Sun LY, Zhang YR, Lai PC, Li WZ (2022) Molecular hydrogen mediates neurorestorative effects after stroke in diabetic rats: the TLR4/NF-kappaB inflammatory pathway. J Neuroimmune Pharmacol. https://doi.org/10.1007/s11481-022-10051-w
Jayaraj RL, Azimullah S, Beiram R, Jalal FY, Rosenberg GA (2019) Neuroinflammation: friend and foe for ischemic stroke. J Neuroinflammation 16(1):142. https://doi.org/10.1186/s12974-019-1516-2
Krishnan A, Lopes RD, Alexander JH, Becker RC, Goldstein LB (2010) Antithrombotic therapy for ischemic stroke: guidelines translated for the clinician. J Thromb Thrombolysis 29(3):368–377. https://doi.org/10.1007/s11239-010-0439-7
Hurford R, Sekhar A, Hughes TAT, Muir KW (2020) Diagnosis and management of acute ischaemic stroke. Pract Neurol 20(4):304–316. https://doi.org/10.1136/practneurol-2020-002557
Eltzschig HK, Eckle T (2011) Ischemia and reperfusion–from mechanism to translation. Nat Med 17(11):1391–1401. https://doi.org/10.1038/nm.2507
Shukla V, Shakya AK, Perez-Pinzon MA, Dave KR (2017) Cerebral ischemic damage in diabetes: an inflammatory perspective. J Neuroinflammation 14(1):21. https://doi.org/10.1186/s12974-016-0774-5
Kim D, Choi I-Y, Jang H, Lee S-H (2013) HMGB1 suppression confers neuroprotection against stroke in diabetic rats. Transl Neurosci 4(4):477–483. https://doi.org/10.2478/s13380-013-0145-y
Kim JM, Lee JE, Cheon SY, Lee JH, Kim SY, Kam EH, Koo BN (2016) The anti-inflammatory effects of agmatine on transient focal cerebral ischemia in diabetic rats. J Neurosurg Anesthesiol 28(3):203–213. https://doi.org/10.1097/ana.0000000000000195
Goldstein RS, Gallowitsch-Puerta M, Yang L, Rosas-Ballina M, Huston JM, Czura CJ, Lee DC, Ward MF, Bruchfeld AN, Wang H et al (2006) Elevated high-mobility group box 1 levels in patients with cerebral and myocardial ischemia. Shock 25(6):571–574. https://doi.org/10.1097/01.shk.0000209540.99176.72
Kim SW, Lee H, Lee HK, Kim ID, Lee JK (2019) Neutrophil extracellular trap induced by HMGB1 exacerbates damages in the ischemic brain. Acta Neuropathol Commun 7(1):94. https://doi.org/10.1186/s40478-019-0747-x
Zhu S, Tang S, Su F (2018) Dioscin inhibits ischemic stroke-induced inflammation through inhibition of the TLR4/MyD88/NF-κB signaling pathway in a rat model. Mol Med Rep 17(1):660–666. https://doi.org/10.3892/mmr.2017.7900
Muriach M, Flores-Bellver M, Romero FJ, Barcia JM (2014) Diabetes and the brain: oxidative stress, inflammation, and autophagy. Oxid Med Cell Longev 2014:102158. https://doi.org/10.1155/2014/102158
Amantea D, Nappi G, Bernardi G, Bagetta G, Corasaniti MT (2009) Post-ischemic brain damage: pathophysiology and role of inflammatory mediators. Febs j 276(1):13–26. https://doi.org/10.1111/j.1742-4658.2008.06766.x
Kriz J (2006) Inflammation in ischemic brain injury: timing is important. Crit Rev Neurobiol 18(1–2):145–157. https://doi.org/10.1615/critrevneurobiol.v18.i1-2.150
Schilling M, Besselmann M, Leonhard C, Mueller M, Ringelstein EB, Kiefer R (2003) Microglial activation precedes and predominates over macrophage infiltration in transient focal cerebral ischemia: a study in green fluorescent protein transgenic bone marrow chimeric mice. Exp Neurol 183(1):25–33. https://doi.org/10.1016/s0014-4886(03)00082-7
Tanaka R, Komine-Kobayashi M, Mochizuki H, Yamada M, Furuya T, Migita M, Shimada T, Mizuno Y, Urabe T (2003) Migration of enhanced green fluorescent protein expressing bone marrow-derived microglia/macrophage into the mouse brain following permanent focal ischemia. Neuroscience 117(3):531–539. https://doi.org/10.1016/s0306-4522(02)00954-5
Price CJ, Menon DK, Peters AM, Ballinger JR, Barber RW, Balan KK, Lynch A, Xuereb JH, Fryer T, Guadagno JV et al (2004) Cerebral neutrophil recruitment, histology, and outcome in acute ischemic stroke: an imaging-based study. Stroke 35(7):1659–1664. https://doi.org/10.1161/01.Str.0000130592.71028.92
Buck BH, Liebeskind DS, Saver JL, Bang OY, Yun SW, Starkman S, Ali LK, Kim D, Villablanca JP, Salamon N et al (2008) Early neutrophilia is associated with volume of ischemic tissue in acute stroke. Stroke 39(2):355–360. https://doi.org/10.1161/strokeaha.107.490128
Yilmaz G, Granger DN (2008) Cell adhesion molecules and ischemic stroke. Neurol Res 30(8):783–793. https://doi.org/10.1179/174313208x341085
Yang Y, Rosenberg GA (2015) Matrix metalloproteinases as therapeutic targets for stroke. Brain Res 1623:30–38. https://doi.org/10.1016/j.brainres.2015.04.024
Li Y, Zhu Z-Y, Huang T-T, Zhou Y-X, Wang X, Yang L-Q, Chen Z-A, Yu W-F, Li P-Y (2018) The peripheral immune response after stroke—a double edge sword for blood-brain barrier integrity. CNS Neurosci Ther 24(12):1115–1128. https://doi.org/10.1111/cns.13081
Lee YB, Park JH, Kim E, Kang CK, Park HM (2014) Arterial stiffness and functional outcome in acute ischemic stroke. J Cerebrovasc Endovasc Neurosurg 16(1):11–19. https://doi.org/10.7461/jcen.2014.16.1.11
Arumugam TV, Okun E, Tang SC, Thundyil J, Taylor SM, Woodruff TM (2009) Toll-like receptors in ischemia-reperfusion injury. Shock 32(1):4–16. https://doi.org/10.1097/SHK.0b013e318193e333
Li M, Liu J, Bi Y, Chen J, Zhao L (2018) Potential medications or compounds acting on toll-like receptors in cerebral ischemia. Curr Neuropharmacol 16(2):160–175. https://doi.org/10.2174/1570159x15666170601125139
Brea D, Blanco M, Ramos-Cabrer P, Moldes O, Arias S, Pérez-Mato M, Leira R, Sobrino T, Castillo J (2011) Toll-like receptors 2 and 4 in ischemic stroke: outcome and therapeutic values. J Cereb Blood Flow Metab 31(6):1424–1431. https://doi.org/10.1038/jcbfm.2010.231
Kilic U, Kilic E, Matter CM, Bassetti CL, Hermann DM (2008) TLR-4 deficiency protects against focal cerebral ischemia and axotomy-induced neurodegeneration. Neurobiol Dis 31(1):33–40. https://doi.org/10.1016/j.nbd.2008.03.002
Hua F, Tang H, Wang J, Prunty MC, Hua X, Sayeed I, Stein DG (2015) TAK-242, an antagonist for Toll-like receptor 4, protects against acute cerebral ischemia/reperfusion injury in mice. J Cereb Blood Flow Metab 35(4):536–542. https://doi.org/10.1038/jcbfm.2014.240
Parada E, Casas AI, Palomino-Antolin A, Gómez-Rangel V, Rubio-Navarro A, Farré-Alins V, Narros-Fernandez P, Guerrero-Hue M, Moreno JA, Rosa JM et al (2019) Early toll-like receptor 4 blockade reduces ROS and inflammation triggered by microglial pro-inflammatory phenotype in rodent and human brain ischaemia models. Br J Pharmacol 176(15):2764–2779. https://doi.org/10.1111/bph.14703
Li C, Che LH, Ji TF, Shi L, Yu JL (2017) Effects of the TLR4 signaling pathway on apoptosis of neuronal cells in diabetes mellitus complicated with cerebral infarction in a rat model. Sci Rep 7:43834. https://doi.org/10.1038/srep43834
Author information
Authors and Affiliations
Contributions
Thura Tun Oo conceptualizes, writes, edits, and finalizes the whole manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oo, T.T. Ischemic stroke and diabetes: a TLR4-mediated neuroinflammatory perspective. J Mol Med 102, 709–717 (2024). https://doi.org/10.1007/s00109-024-02441-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-024-02441-9