Abstract
AVE0991, a nonpeptide angiotensin-(1–7) mimic, has similar protective effects for cardiovascular system to Ang-(1–7). In this article, we aimed to explore the effects of AVE0991 and Ang-(1–7) on abdominal aortic aneurysm (AAA) induced by Ang II in apolipoprotein E knockout mice. The mice AAA model was established by Ang II infusion, and then mice received different treatment with saline, Ang II (1.44 mg/kg/day), different dose AVE0991 (0.58 or 1.16 μmol/kg/day), or Ang-(1–7) (400 ng/kg/min). The incidence of AAA was 76%, 48%, 28%, and 24% in the vehicle, the low-dose AVE0991, high-dose AVE0991, and the Ang-(1–7) group, respectively. In comparison with control group, AVE0991 and Ang-(1–7) treatment significantly increased smooth muscle cells and decreased macrophage accumulation, the expression levels of monocyte chemoattractant protein-1 (MCP-1) and tumor necrosis factor α (TNF-α), and the expression and activity of metalloproteinases 2 and 9 in mice AAA model or in human smooth muscle cells (hVSMCs). The therapeutic effects may be contributed to reduction of oxidative stress and downregulation of P38 and ERK1/2 signal pathways via Mas receptor activation, whereas the positive impacts were reversed by co-administration with the Mas antagonist A779 (400 ng/kg/min) and AVE0991 in Ang II–infused mice or in hVSMCs. Therefore, AVE0991 and Ang-(1–7) might be novel and promising interventions in the prevention and treatment of AAA.
Key messages
• AVE0991 dose-dependently inhibited Ang II–induced AAA formation in Apoe−/− mice.
• Ang-(1–7) played the same protective role as high-dose AVE0991.
• Inhibition of Mas receptor with A779 could reverse the protective effect of AVE0991.
• The therapeutic effects may be contributed to reduction of oxidative stress and downregulation of P38 and ERK1/2 signal pathways via Mas receptor activation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abdominal aortic aneurysm (AAA) is a common vascular disease, which is often asymptomatic. AAA is characterized by permanent dilatation or ballooning of the abdominal aorta surpassing the normal diameter by more than 50%. In the men over 65, up to 6–9% suffer from AAA claiming more than 15,000 lives annually [1]. Currently, surgery repair has been proven to restrain AAA progression and rupture. However, surgery is limited for the treatment of patients with small AAAs or contraindications for surgery. Therefore, searching for a safe and effective therapeutic approach of preventing AAA formation and progression remains an important issue.
Pathologically, AAA is characterized by apoptosis of smooth muscle cells and loss of elastin [2]. In AAA formation, the inflammation and matrix degradation of arterial tissues contribute to the tissue destruction and arterial wall impairment [3,4,5]. Oxidative stress has been demonstrated to become a causative bridge between inflammation, degradation of matrix, and AAA pathogenesis [6]. For instance, angiotensin II (Ang II) increases oxidative stress [7], activates matrix metalloproteinase (MMPs) expression [8], and induces AAA formation in experimental studies via inflammation [9].
For the mice AAA model, Ang II infusion into apolipoprotein E knockout (Apoe−/−) mice is commonly used, which is similar to the pathology of human AAA [10]. As a major family member of the renin–angiotensin system (RAS), Ang II play a part in oxidative stress, matrix degradation, inflammation, and vascular remodeling of the abdominal aorta [11]. Previous studies have reported that angiotensin-(1–7) (Ang-(1–7)), which is cleaved from Ang II by angiotensin-converting enzyme 2 (ACE2) [12], neutralizes the adverse effects of Ang II in atherosclerosis [13]. Recently, ACE2 and Ang-(1–7) as a novel therapeutic target for cardiovascular diseases have been systemically evaluated. Previous studies show that Ang-(1–7), which is primarily mediated by a G protein-coupled receptor, the Mas receptor, exerts protective roles against vascular inflammation and remodeling in the pathophysiology of intracranial aneurysms [14]. The nonpeptide Ang-(1–7) mimic, AVE0991, is recognized an agonist at Mas receptor which has beneficial cardiovascular effects similar to anti-inflammation and reduction of oxidative stress induced by Ang-(1–7) [15,16,17]. However, it remains unknown whether AVE0991 and Ang-(1–7) are able to prevent Ang II–induced AAA formation and, if they are so, what mechanisms may be involved in these therapeutic approaches.
In this study, we explore the hypothesis that AVE0991 and Ang-(1–7) may prevent Ang II–induced AAA in Apoe−/− mice through inhibiting inflammation and MMP-2 and MMP-9. A series of in vivo and in vivo experiments were designed and performed to validate this hypothesis.
Materials and methods
Animal protocol
Two hundred male Apoe−/− mice (8–12 weeks) were obtained from Beijing WeiTongLiHua Animal Experimental Center and housed in the temperature and humidity-controlled cages. The animal protocol was reviewed and approved by Shandong University Institute Animal Care and Use Committee. And all the animal experiments followed the “3R” (Reduction, Replacement, Refinement) guidelines in this article.
Our animal studies were consisted of two parts. In the first part, in order to examine the dose-effect of AVE0991 on Ang II–induced abdominal aortic aneurysm (AAA), Apoe−/− mice were randomly divided into 5 groups after a 1-week regular diet feeding (n = 25 per group), and were treated with continuous subcutaneous infusion of different agents via an osmotic minipump (Model 2004, Durect Corporation, CA, USA) for 28 days as described previously [18]. The control group received infusion of saline, the vehicle group received infusion of Ang II (1.44 mg/kg/day, Sigma-Aldrich), the low-dose AVE0991 group received the same diet, mixed with AVE0991 (Sanofi-Aventis Deutschland GmbH, Frankfurt am Main, Germany) at a dose of 0.58 μmol/kg/day [19] and infusion of Ang II (1.44 mg/kg/day), the high-dose AVE0991 group received orally AVE0991 (1.16 μmol/kg/day) and infusion of Ang II (1.44 mg/kg/day), and the Ang-(1–7) group received infusion of Ang II (1.44 mg/kg/day) plus Ang-(1–7) (400 ng/kg/min, Bachem, Torrance, CA). All mice underwent euthanasia after 28-day infusion and the whole aortas including thoracic and abdominal aortas were collected for morphological and histological analysis of AAA.
In the second part of the study, in order to elaborate the role of Mas receptor in the effect of AVE0991 on Ang II–induced AAA, Apoe−/− mice were randomly divided into 3 groups (n = 25 per group): a vehicle group that received infusion of only Ang II (1.44 mg/kg/day), a high-dose AVE0991 group received orally AVE0991 (1.16 μmol/kg/day) and infusion of Ang II (1.44 mg/kg/day), and a high-dose AVE0991 + A779 group received orally AVE0991 (1.16 μmol/kg/day) and infusion of Ang II (1.44 mg/kg/day) plus A779 (Mas antagonist, 400 ng/kg/min, Bachem, Torrance, CA). These agents were continuously infused into mice subcutaneously via an osmotic minipump for 28 days and then the whole aortas were collected from all mice after euthanasia for morphological and histological analysis of AAA.
Cell cultures
Human vascular smooth muscle cells (hVSMCs) from ATCC were grown in SMC medium (SclenCell, USA) containing 2% fetal bovine serum (gibco, Australia), 1% SMC growth supplement, 100 U/ml penicillin, and 10 mg/ml streptomycin. All cells were incubated at 37 °C in a humidified atmosphere of 5% CO2 and 95% air and were used between passages 4–6. Cells were cultured to 80% confluency before being treated with different agents.
In the first part, the experiments were divided into 5 groups: a control group that received no drug stimulation, a Ang II group that received only stimulation of Ang II (10−6 mol/L), a low-dose AVE0991 group that received treatment of Ang II (10−6 mol/L) + AVE0991(10−8 mol/L), a high-dose AVE0991 group that received treatment of Ang II (10−6 mol/L) + AVE0991 (10−6 mol/L), and a Ang-(1–7) group that received treatment of Ang II (10−6 mol/L) + Ang-(1–7) (10−6 mol/L). Cultured hVSMCs were pretreated with AVE0991 or Ang-(1–7) for 1 h followed by co-incubation of Ang II for 24 h [20].
To further study the role of Mas receptor in the effect of AVE0991 against Ang II, cells were cultivated with Mas antagonist A779 (10−6 mol/L) for 1 h before adding Ang II (10−6 mol/L) and AVE0991(10−6 mol/L). Cells seeded in 6 wells were divided into 4 groups: a control group that received no drug stimulation, a Ang II group that received only stimulation of Ang II (10−6 mol/L), a high-dose AVE0991 group that received treatment of Ang II (10−6 mol/L) + AVE0991(10−6 mol/L), and a high-dose AVE0991 + A779 group that received treatment of Ang II (10−6 mol/L) + AVE0991 (10−6 mol/L) + A779 (10−6 mol/L).
Statistical analysis
Statistical analyses involved use of SPSS 20 (SPSS Inc., Chicago, IL). Data were displayed as scatter plots and bar graphs with indication of mean ± SEM. Comparisons of parameters among more than two groups were made by one-way ANOVA with least significant difference post hoc analysis. Chi-square test was applied to comparisons of AAA incidence, mortality. A value with P < 0.05 was considered statistically significant.
More methods are included in the Supplemental sections
Results
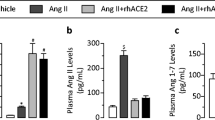
Serum lipid and blood pressure
As indicated in Supplementary Table S1 and S2, serum lipid levels did not differ among all mice groups. Systolic blood pressure (SBP) was significantly increased in Ang II–infused Apoe−/− mice compared with the control group. However, neither AVE0991 at different doses and Ang-(1–7) nor A779-AVE0991 had effect on SBP (Supplementary Table S1 and S2).
AVE0991 and Ang-(1–7) attenuated Ang II–induced AAA formation in Apoe−/− mice
We detected the effects of AVE0991 at different doses and Ang-(1–7) on AAA formation. As shown in Fig. 1B, the incidence of AAA was 76%, 48%, 28%, and 24% and the mortality of mice was 24%, 12%, 0%, and 4% in the vehicle, low-dose AVE0991, high-dose AVE0991, and Ang-(1–7) groups, respectively. There were no mice in the control group developing AAA and death (0%). Compared with the vehicle group, the AAA incidence and mortality of mice were significantly decreased in the low-dose AVE0991, high-dose AVE0991, and Ang-(1–7) groups (Fig. 1A, B). In addition, the AAA incidence and mortality were substantially decreased in the high-dose AVE0991 and Ang-(1–7) groups compared with the low-dose AVE0991 group, with no significant difference between the high-dose AVE0991 and Ang-(1–7) groups. As well, the maximal diameter of the abdominal aorta was gradually reduced by AVE0991 in concentration-dependent manner in comparison with the vehicle group (Fig. 1D). Compared with low-dose AVE0991 group, the maximal diameter was significantly decreased in the Ang-(1–7) group, but with no significant difference between the high-dose AVE0991 and Ang-(1–7) groups. Therefore, AVE0991 dose-dependently reduced the incidence and mortality of Ang II–induced AAA in Apoe−/− mice.
Effect of AVE0991 and Ang-(1–7) on the formation of Ang II–induced AAA in Apoe−/− mice. (A) Representative photographs showing macroscopic features of abdominal aortic specimens in 5 groups of mice. (B) The incidence and the mortality in 5 groups of mice. (C) Representative hematoxylin and eosin staining in abdominal aortic cross-section. (D) Maximal abdominal aortic diameters in 5 groups of mice. * P < 0.05 vs low-dose AVE0991, high-dose AVE0991, and Ang-(1–7) groups; #P < 0.05 vs low-dose AVE0991 group
Effect of AVE0991 and Ang-(1–7) treatment on Ang II–induced histological and morphological changes in Apoe−/− mouse aortas
Angiotensin II infusion induced the abdominal aorta remodeling, breakdown of the aortic media and adventitia, and breakage and discontinuity of elastin fibers in the aortic wall of mice. Hematoxylin and eosin and Verhoff–Van Gieson staining showed that AVE0991 in dose-dependent manner and Ang-(1–7) treatment largely reversed these pathological changes (Figs. 1C and 2A). However, the morphology of the abdominal aorta was similar in high-dose AVE0991 and Ang-(1–7) groups, which was characterized by the slight pathological changes.
Effect of AVE0991 and Ang-(1–7) on abdominal aortic wall compositions in Ang II–infused Apoe−/− mice. (A) Representative erhoff-Van Gieson staining, immunohistochemistry of α SM-actin and MOMA-2 in abdominal aortic cross-section. (B and C) Quantitative analysis of α SM-actin and MOMA-2 staining in 4 groups of mice. *P < 0.05 vs low-dose AVE0991, high-dose AVE0991, and Ang-(1–7) groups; #P < 0.05 vs low-dose AVE0991 group
Specifically, the relative content of SMCs in the aortic wall was gradually increased by AVE0991 in dose-dependent manner, whereas the content of macrophages was gradually decreased in comparison with the vehicle group (Fig. 2A–C). In addition, these parameters showed the same trend between the high-dose AVE0991 and Ang-(1–7) groups.
AVE0991 and Ang-(1–7) downregulated the expression of proinflammatory cytokines
Chronic inflammation of the aortic wall is crucial for AAA formation. Previous studies indicated that proinflammatory cytokines, such as monocyte chemoattractant protein-1 (MCP-1) and tumor necrosis factor α (TNF-α), were upregulated with chronic infusion of Ang II in Apoe−/− mice [21, 22]. In this study, both Western blot and immunohistochemical analysis showed that the protein expression levels of MCP-1 and TNF-α in the aortic tissues were significantly decreased in the low-dose AVE0991, high-dose AVE0991, and Ang-(1–7) groups compared with the vehicle group (Fig. 3A, D, E and Supplementary Fig. S1A, S1D, S1E); Nevertheless, these measurements were significantly attenuated by high-dose AVE0991 and Ang-(1–7) treatment relative to the low-dose AVE0991 group, but there was no significant difference between the high-dose AVE0991 and Ang-(1–7) groups.
Effect of AVE0991 and Ang-(1–7) on the expression of MMPs and proinflammatory cytokines in Ang II–infused Apoe−/− mice. (A) Western blot analysis of MMP-2, MMP-9, MCP-1, and TNF-α expression in abdominal aortic aneurysm from Ang II–infused Apoe−/− mice. (B to E) Quantitative analysis of MMP-2, MMP-9, MCP-1, and TNF-α expression in 4 groups of mice. (F) Gelatin zymography analysis of MMP-9 and MMP-2 activity and their quantitative analysis (G and H). *P < 0.05 vs low-dose AVE0991, high-dose AVE0991, and Ang-(1–7) groups; #P < 0.05 vs low-dose AVE0991 group
In vitro study, we found that the protein expression levels of MCP-1 and TNF-α were gradually reduced by AVE0991 in concentration-dependent manner in comparison with the vehicle group in human vascular smooth muscle cells (hVSMCs) as in vivo study (Supplementary Fig. S2A, S2F and S2G), whereas the high-dose AVE0991 (10−6 mol/L) and Ang-(1–7) had the similar effect of inflammatory cytokines expression. Thus, AVE0991 in concentration-dependent manner and Ang-(1–7) downregulated the expression of proinflammatory cytokines.
AVE0991 and Ang-(1–7) attenuated MMP-2 and MMP-9 expression
MMP-2 and MMP-9 are the predominant proteinases in the aortic wall for elastin degradation in the process of AAA [23, 24]. The protein expression levels and activities of MMP-2 and MMP-9 by Western blot or immunohistochemical analysis and gelatin zymography were significantly lower in the low-dose AVE0991, high-dose AVE0991, and Ang-(1–7) groups than in the vehicle group (Fig. 3A–C, F–H and Supplementary Fig. S1A-S1C). Furthermore, MMP-2 and MMP-9 expression levels in the high-dose AVE0991 and Ang-(1–7) groups had similar pattern, but were lower than in the low-dose AVE0991 group. In hVSMCs, AVE0991 in concentration-dependent manner and Ang-(1–7) blunted Ang II–induced upregulation of MMP-2 and MMP-9 (Supplementary Fig. S2A, S2D and S2E), and there was no significant difference between the high-dose AVE0991 and Ang-(1–7) groups.
AVE0991 and Ang-(1–7) reduced oxidative stress
Oxidative stress is established mediators of AAA development [25]. We detected the protein expression of p47 and NOX2 in the aortic tissues of Apoe−/− mice by Western blot and found that were significantly reduced in the low-dose AVE0991, high-dose AVE0991 and Ang-(1–7) groups compared with the vehicle group (Fig. 4A, B). Furthermore, these measurements were significantly lower in the high-dose AVE0991 and Ang-(1–7) groups than in the low-dose AVE0991 group, but with no significant difference between the high-dose AVE0991 and Ang-(1–7) groups. In hVSMCs, we obtained the same results as in Apoe−/− mice (Supplementary Fig. S2A-S2C).
Effect of AVE0991 and Ang-(1–7) on oxidative stress, Mas receptor and signaling proteins in Ang II–infused Apoe−/− mice. (A) Western blot analysis of p47 and NOX2 expression in 4 groups of mice and their quantitative analysis (B). (C) The level of Mas receptor mRNA expression was assayed by RT-PCR. (D) Mas receptor protein expression in abdominal aortic arteries was determined by Western blot and it quantitative analysis. (E and F) The levels of pP38, P38, pERK, and ERK in abdominal aortic arteries were measured by Western blot and quantitative analysis of pP38/P38, pERK/ERK. *P < 0.05 vs low-dose AVE0991, high-dose AVE0991 and Ang-(1–7) groups; #P < 0.05 vs low-dose AVE0991 group
AVE0991 and Ang-(1–7) suppressed the activation of P38 MAPK and ERK1/2 signal pathway
To verify the signaling proteins involved in the AVE0991 effect on Ang II–induced AAA, we examined the expression levels of P38 MAPK (P38) and extracellular signal-regulated kinase 1/2 (ERK1/2) both in vivo and in vitro. In AVE0991-treated mice and hVSMCs, phosphorylated P38 (pP38) and phosphorylated ERK1/2 (pERK1/2) were significantly decreased in comparison with vehicle mice and Ang II group of cells (Fig. 4E, F and Supplementary Fig. S2H, S2J, S2K). In addition, pP38 and pERK1/2 were significantly decreased in the high-dose AVE0991 and Ang-(1–7) groups compared with the low-dose AVE0991 group, but there was no significant difference between the high-dose AVE0991 and Ang-(1–7) groups.
AVE0991 and Ang-(1–7) increased the expression of Mas receptor
We then investigated the expression of Mas receptor involved in the protective effect of AVE0991 on Ang II–induced AAA in vivo. Compared with the vehicle group, low-dose and high-dose AVE0991 and Ang-(1–7) treatment significantly upregulated the mRNA and protein expression of Mas receptor (Fig. 4C, D), whereas Mas receptor expression was significantly increased in high-dose AVE0991 and Ang-(1–7) groups compared with the low-dose AVE0991 group, with no significant difference between the high-dose AVE0991 and Ang-(1–7) groups. The results in hVSMCs showed relative to the control and Ang II groups, the mRNA and protein expression of Mas receptor were gradually increased by AVE0991 in concentration-dependent manner (Supplementary Fig. S2H, S2I and S2L), but there was no significant difference between the control and Ang II groups or between the high-dose AVE0991 and Ang-(1–7) groups.
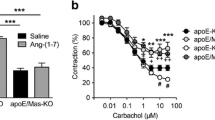
To further understand whether AVE0991 exerted its protective effect via Mas receptor, we co-treated mice with Mas antagonist A779 and high-dose AVE0991. We found that A779 not only reversed the AAA incidence and mortality of mice, and the maximal diameter of the abdominal aorta by AVE0991 (Fig. 5), but also reversed high-dose AVE0991-induced increase in SMCs content in AAA (Fig. 6A, B). As well, it markedly blunted the suppression of macrophage infiltration and inflammation by high-dose AVE0991 (Figs. 6A, C and 7A, D, E; Supplementary Fig. S3A, S2D, S3E). The protein expression and activity of MMP-2 and MMP-9 were restored with the co-treatment of AVE0991 and A779 (Fig. 7A–C, F–H; Supplementary Fig. S3A-S3C). The expression of p47 and NOX2 and the phosphorylation of P38 and ERK1/2 were increased in AVE0991 and A779 co-administrated group (Supplementary Fig. S4A, S4B and S4E, S4F). Compared with the high-dose AVE0991 group, A779 treatment downregulated mRNA and protein expression of Mas receptor (Supplementary Fig. S4C and S4D). In hVSMCs, consistent with vivo results, A779 treatment significantly increased the expression levels of proinflammatory cytokines, MMPs, p47, NOX2, and signal proteins, but decreased the expression of Mas receptor compared with the high-dose AVE0991 group (Supplementary Fig. S5). Therefore, Mas receptor may play an important role in the beneficial effect of AVE0991 on Ang II–induced AAA.
Effect of Mas antagonist A779 on Ang II–induced AAA formation. (A) Representative images showing macroscopic features of abdominal aortic specimens in 3 groups of mice. (B) The incidence and the mortality in 3 groups of mice. (C) Representative hematoxylin and eosin staining in abdominal aortic cross-section. (D) Maximal abdominal aortic diameters in 3 groups of mice. *P < 0.05 vs vehicle group; #P < 0.05 vs high-dose AVE0991 group
Effect of A779 on abdominal aortic wall compositions in Ang II–infused Apoe−/− mice. (A) Representative erhoff-Van Gieson staining, immunohistochemistry of α SM-actin and MOMA-2 in abdominal aortic cross-section. (B and C) Quantitative analysis of α SM-actin and MOMA-2 staining in 3 groups of mice. *P < 0.05 vs vehicle group; #P < 0.05 vs high-dose AVE0991 group
Effect of A779 on the expression of MMPs and proinflammatory cytokines in Ang II–infused Apoe−/− mice. (A) Western blot analysis of MMP-2, MMP-9, MCP-1, and TNF-α expression in abdominal aortic aneurysm from Ang II–infused Apoe−/− mice. (B to E) Quantitative analysis of MMP-2, MMP-9, MCP-1, and TNF-α expression in 3 groups of mice. (F) Gelatin zymography analysis of MMP-9 and MMP-2 activity and their quantitative analysis (G and H). *P < 0.05 vs vehicle group; #P < 0.05 vs high-dose AVE0991 group
Discussions
In the present study, we used 2 different doses of AVE0991 (0.58 μmol/kg/day and 1.16 μmol/kg/day) continued the treatment time to 28 days. We provide the first evidence that AVE0991 dose-dependently inhibited Ang II–induced AAA formation in Apoe−/− mice, and Ang-(1–7) played the same protective role as high-dose AVE0991. Moreover, inhibition of Mas receptor with A779 could reverse the protective effect of AVE0991. The mechanisms underlying these therapeutic effects involved increased SMCs content, inhibited inflammation, and decreased MMP-2 and MMP-9 expression induced by reduction of oxidative stress and downregulation of P38 and ERK1/2 signal pathways via Mas receptor activation.
An important finding of this study is that AVE0991 and Ang-(1–7) treatment did not differ in serum lipid levels in our animal model, indicating that the therapeutic effects of AVE0991 and Ang-(1–7) are independent of lipid levels. Although infusion of AngII could increase BP, AVE0991 and Ang-(1–7) treatment did not affected the elevated BP in the mouse model. Previous study illustrated that BP did not play an important role in AAA induced by Ang II infusion [26]. Thus, the protective effects of AVE0991 and Ang-(1–7) treatment on AAA formation are both lipid- and BP-independent.
One of the characterized signs in the pathogenesis of AAA is chronic inflammation of the aortic wall, which is characterized by the resultant infiltration of inflammatory cells, particularly macrophages, and increased the expression of proinflammatory cytokines [23]. In the present study, AVE0991 and Ang-(1–7) treatment significantly decreased macrophage infiltration and the expression levels of proinflammatory cytokines, such as MCP-1 and TNF-α, in aortic tissues and hVSMCs. These results suggested that the therapeutic effects of AVE0991 and Ang-(1–7) treatment are associated with the attenuated inflammatory cell accumulation and proinflammatory cytokine expression.
Degradation of extracellular matrix and vascular remodeling are main pathological features of human AAA and mediated mainly by MMPs [4]. MMPs expressions, particularly MMP-2 and MMP-9, are increased in human aneurysmal tissues, which are essential to the formation of AAA [24]. Experimental studies demonstrated that a concerted role of MMP-2 and MMP-9 is required for aneurysmal degeneration, whereas MMP-2 and MMP-9 deficiency could prevent AAA progression [24]. In the present study, we found that the expression and activity of MMP-2 and MMP-9 were inhibited by AVE0991 and Ang-(1–7) in mouse aortas and in HASMCs, which may contribute to attenuate aortic matrix degradation and tissue disintegration in our mouse model.
Previous studies demonstrate that oxidative stress plays an important role in AAA formation [25, 27]. NADPH oxidase (NOX) expression and levels of the p47phox subunit are markedly upregulated in human aortic aneurysmal tissues [28]. Furthermore, experimental studies have produced ROS, which is generated mainly by NOX, in the development and progression of AAA [29]. Oxidative stress was associated with inflammatory cytokines expression and MMPs production in the progression of AAA [6]. In our study, AVE0991 and Ang-(1–7) treatment significantly reduced the expression of p47 and NOX2 in aortic tissues in Apoe−/− mice and in hVAMCs, suggesting that blunted oxidative stress may be a key mechanism in inhibiting AAA formation.
Several studies demonstrated that mitogen-activated protein kinase (MAPK) was involved in the development and progression of AAA [30, 31]. P38 and ERK1/2, main members of MAPK family, are upregulated in human and mouse AAA tissues and was associated with activated inflammation and MMP production [32, 33]. In this study, the activation of P38 and ERK1/2 was markedly reduced in AVE0991- and Ang-(1–7)-treated mice and hVSMCs, indicating that the therapeutic effects of AVE0991 and Ang-(1–7) on AAA were via downregulating the activation of P38 and ERK1/2.
We know that the role of angiotensins is receptor-mediated. In this study, we found that AVE0991 and Ang-(1–7) treatment significantly increased Mas receptor protein and mRNA expression in Apoe−/− mice and in hVSMCs, suggesting that Mas receptor was activated by AVE0991 and Ang-(1–7). Previous studies demonstrate that AVE0991 or Ang-(1–7) has been shown to exert potential beneficial cardiovascular actions via upregulating the expression of Mas receptor [14, 17]. In the present study, we found that co-treatment of A779, an antagonist of Mas receptor, reversed the beneficial effects of AVE0991 in vivo and in vitro. These results suggested that the therapeutic effects of AVE0991 and Ang-(1–7) on AAA were via increasing the activation of Mas receptor.
Interestingly, we found that the Ang II–treated mice showed marked cardiac hypertrophy than the control group, which is consistent with previous studies [34, 35]. There are also reports showed that AVE0991 and Ang-(1–7) attenuate cardiac hypertrophy and improve cardiac function [36, 37]. According to our research, the AAA formation induced by Ang II is weakened by AVE0991 and Ang-(1–7). And the related signal pathway such as ERK and p38-MAPK might be participated in the myocardial remodeling induced by AVE0991 and Ang-(1–7).
In conclusion, AVE0991 dose-dependently inhibited Ang II–induced AAA formation in Apoe−/− mice, and Ang-(1–7) played the same protective role as high-dose AVE0991. Furthermore, inhibition of Mas receptor with A779 could reverse the protective effect of AVE0991. The mechanisms underlying these therapeutic effects involved increased SMCs content, inhibited inflammation, decreased MMP-2 and MMP-9 expression and activity induced by reduction of oxidative stress and downregulation of P38 and ERK1/2 signal pathways via Mas receptor activation. Therefore, AVE0991 and Ang-(1–7) may become novel and promising approaches in the prevention and treatment of AAA.
Change history
30 March 2020
The corrected Figure 7 image is presented in this paper.
References
Daugherty A, Cassis LA (2002) Mechanisms of abdominal aortic aneurysm formation. Curr Atheroscler Rep 4(3):222–227
Thompson RW, Geraghty PJ, Lee JK (2002) Abdominal aortic aneurysms: basic mechanisms and clinical implications. Curr Probl Surg 39(2):110–230
Davis FM, Rateri DL, Daugherty A (2014) Mechanisms of aortic aneurysm formation: translating preclinical studies into clinical therapies. Heart. 100(19):1498–1505
Hellenthal FA, Buurman WA, Wodzig WK, Schurink GW (2009) Biomarkers of AAA progression. Part 1: extracellular matrix degeneration. Nat Rev Cardiol 6(7):464–474
Yokoyama U, Ishiwata R, Jin MH, Kato Y, Suzuki O, Jin H, Ichikawa Y, Kumagaya S, Katayama Y, Fujita T, Okumura S, Sato M, Sugimoto Y, Aoki H, Suzuki S, Masuda M, Minamisawa S, Ishikawa Y (2012) Inhibition of EP4 signaling attenuates aortic aneurysm formation. PLoS One 7(5):e36724
Wang S, Zhang C, Zhang M, Liang B, Zhu H, Lee J, Viollet B, Xia L, Zhang Y, Zou MH (2012) Activation of AMP-activated protein kinase α2 by nicotine instigates formation of abdominal aortic aneurysms in mice in vivo. Nat Med 18(6):902–910
Rajagopalan S, Kurz S, Münzel T, Tarpey M, Freeman BA, Griendling KK, Harrison DG (1996) Angiotensin II-mediated hypertension in the rat increases vascular superoxide production via membrane NADH/NADPH oxidase activation. Contribution to alterations of vasomotor tone. J Clin Invest 97(8):1916–1923
Browatzki M, Larsen D, Pfeiffer CA, Gehrke SG, Schmidt J, Kranzhofer A, Katus HA, Kranzhofer R (2005) Angiotensin II stimulates matrix metalloproteinase secretion in human vascular smooth muscle cells via nuclear factor-kappaB and activator protein 1 in a redox-sensitive manner. J Vasc Res 42(5):415–423
Thomas M, Gavrila D, McCormick ML, Miller FJ Jr, Daugherty A, Cassis LA, Dellsperger KC, Weintraub NL (2006) Deletion of p47phox attenuates angiotensin II-induced abdominal aortic aneurysm formation in apolipoprotein E-deficient mice. Circulation. 114(5):404–413
Daugherty A, Rateri DL, Lu H, Inagami T, Cassis LA (2004) Hypercholesterolemia stimulates angiotensin peptide synthesis and contributes to atherosclerosis through the AT1A receptor. Circulation. 110(25):3849–3857
Lu WW, Jia LX, Ni XQ et al (2016) Intermedin1-53 attenuates abdominal aortic aneurysm by inhibiting oxidative stress. Arterioscler Thromb Vasc Biol 36(11):2176–2190
Vickers C, Hales P, Kaushik V, Dick L, Gavin J, Tang J, Godbout K, Parsons T, Baronas E, Hsieh F, Acton S, Patane M, Nichols A, Tummino P (2002) Hydrolysis of biological peptides by human angiotensin-converting enzyme-related carboxypeptidase. J Biol Chem 277(17):14838–14843
Yang JM, Dong M, Meng X et al (2013) Angiotensin-(1-7) dose-dependently inhibits atherosclerotic lesion formation and enhances plaque stability by targeting vascular cells. Arterioscler Thromb Vasc Biol 33(8):1978–1985
Shimada K, Furukawa H, Wada K, Wei Y, Tada Y, Kuwabara A, Shikata F, Kanematsu Y, Lawton MT, Kitazato KT, Nagahiro S, Hashimoto T (2015) Angiotensin-(1-7) protects against the development of aneurysmal subarachnoid hemorrhage in mice. J Cereb Blood Flow Metab 35(7):1163–1168
Ebermann L, Spillmann F, Sidiropoulos M, Escher F, Heringer-Walther S, Schultheiss HP, Tschöpe C, Walther T (2008) The angiotensin-(1-7) receptor agonist AVE0991 is cardioprotective in diabetic rats. Eur J Pharmacol 590(1–3):276–280
Rodrigues-Machado MG, Magalhães GS, Cardoso JA, Kangussu LM, Murari A, Caliari MV, Oliveira ML, Cara DC, Noviello ML, Marques FD, Pereira JM, Lautner RQ, Santos RA, Campagnole-Santos MJ (2013) AVE 0991, a non-peptide mimic of angiotensin-(1-7) effects, attenuates pulmonary remodelling in a model of chronic asthma. Br J Pharmacol 170(4):835–846
Wiemer G, Dobrucki LW, Louka FR, Malinski T, Heitsch H (2002) AVE 0991, a nonpeptide mimic of the effects of angiotensin-(1-7) on the endothelium. Hypertension. 40(6):847–852
Kong J, Zhang K, Meng X, Zhang Y, Zhang C (2015) Dose-dependent bidirectional effect of angiotensin IV on abdominal aortic aneurysm via variable angiotensin receptor stimulation. Hypertension. 66(3):617–626
Toton-Zuranska J, Gajda M, Pyka-Fosciak G, Kus K, Pawlowska M, Niepsuj A, Wolkow P, Olszanecki R, Jawien J, Korbut R (2010) AVE 0991-angiotensin-(1-7) receptor agonist, inhibits atherogenesis in apoE-knockout mice. J Physiol Pharmacol 61(2):181–183
Lee S, Evans MA, Chu HX, Kim HA, Widdop RE, Drummond GR, Sobey CG (2015) Effect of a selective mas receptor agonist in cerebral ischemia in vitro and in vivo. PLoS One 10(11):e0142087
Hashizume R, Yamawaki-Ogata A, Ueda Y, Wagner WR, Narita Y (2011) Mesenchymal stem cells attenuate angiotensin II-induced aortic aneurysm growth in apolipoprotein E-deficient mice. J Vasc Surg 54(6):1743–1752
Martin-McNulty B, Tham DM, da Cunha V et al (2003) 17 Beta-estradiol attenuates development of angiotensin II-induced aortic abdominal aneurysm in apolipoprotein E-deficient mice. Arterioscler Thromb Vasc Biol 23(9):1627–1632
Hellenthal FA, Buurman WA, Wodzig WK, Schurink GW (2009) Biomarkers of abdominal aortic aneurysm progression. Part 2: inflammation. Nat Rev Cardiol 6(8):543–552
Longo GM, Xiong W, Greiner TC, Zhao Y, Fiotti N, Baxter BT (2002) Matrix metalloproteinases 2 and 9 work in concert to produce aortic aneurysms. J Clin Invest 110(5):625–632
Satoh K, Nigro P, Matoba T, O'Dell MR, Cui Z, Shi X, Mohan A, Yan C, Abe J, Illig KA, Berk BC (2009) Cyclophilin A enhances vascular oxidative stress and the development of angiotensin II-induced aortic aneurysms. Nat Med 15(6):649–656
Cassis LA, Gupte M, Thayer S, Zhang X, Charnigo R, Howatt DA, Rateri DL, Daugherty A (2009) ANG II infusion promotes abdominal aortic aneurysms independent of increased blood pressure in hypercholesterolemic mice. Am J Physiol Heart Circ Physiol 296(5):H1660–H1665
Ejiri J, Inoue N, Tsukube T, Munezane T, Hino Y, Kobayashi S, Hirata K, Kawashima S, Imajoh-Ohmi S, Hayashi Y, Yokozaki H, Okita Y, Yokoyama M (2003) Oxidative stress in the pathogenesis of thoracic aortic aneurysm: protective role of statin and angiotensin II type 1 receptor blocker. Cardiovasc Res 59(4):988–996
Miller FJ Jr, Sharp WJ, Fang X, Oberley LW, Oberley TD, Weintraub NL (2002) Oxidative stress in human abdominal aortic aneurysms: a potential mediator of aneurysmal remodeling. Arterioscler Thromb Vasc Biol 22(4):560–565
Gavrila D, Li WG, McCormick ML et al (2005) Vitamin E inhibits abdominal aortic aneurysm formation in angiotensin II-infused apolipoprotein E-deficient mice. Arterioscler Thromb Vasc Biol 25(8):1671–1677
Chakraborti S, Mandal M, Das S, Mandal A, Chakraborti T (2003) Regulation of matrix metalloproteinases: an overview. Mol Cell Biochem 253(1–2):269–285
Cho A, Graves J, Reidy MA (2000) Mitogen-activated protein kinases mediate matrix metalloproteinase-9 expression in vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 20(12):2527–2532
Aoki H, Yoshimura K, Matsuzaki M (2007) Turning back the clock: regression of abdominal aortic aneurysms via pharmacotherapy. J Mol Med (Berl) 85(10):1077–1088
Xiong W, Mactaggart J, Knispel R, Worth J, Zhu Z, Li Y, Sun Y, Baxter BT, Johanning J (2009) Inhibition of reactive oxygen species attenuates aneurysm formation in a murine model. Atherosclerosis. 202(1):128–134
Paradis P, Dali-Youcef N, Paradis F et al (2000) Overexpression of angiotensin II type 1 receptor in cardiomyocytes induces cardiac hypertrophy and remodeling. Proc Natl Acad Sci 97:931–936
Rivard K, Grandy SA, Douillette A, Paradis P, Nemer M, Allen BG, Fiset C (2011) Overexpression of type 1 angiotensin II receptors impairs excitation-contraction coupling in the mouse heart. Am J Physiol Heart Circ Physiol 301:H2018–H2027
Zeng WT, Chen WY, Leng XY, Tang LL, Sun XT, Li CL, Dai G (2012) Impairment of cardiac function and remodeling induced by myocardial infarction in rats are attenuated by the nonpeptide angiotensin-(1-7) analog AVE 0991. Cardiovasc Ther 30(3):152–161
Ma Y, Huang H et al (2016) AVE 0991 attenuates cardiac hypertrophy through reducing oxidative stress. Biochem Biophys Res Commun 474(4):621–625
Funding
This work was supported by the National 973 Basic Research Program of China (No. 2013CB530700), National Natural Science Foundation of China (No. 81570729, 81170207, 81500339), Program of State Chinese Medicine Administration Bureau (No. JDZX2012113), and the Key Research & Development Plan of Shandong Province (NO. 2019GSF108013).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 4.61 mb)
Rights and permissions
About this article
Cite this article
Ma, H., Wang, YL., Hei, NH. et al. AVE0991, a nonpeptide angiotensin-(1–7) mimic, inhibits angiotensin II–induced abdominal aortic aneurysm formation in apolipoprotein E knockout mice. J Mol Med 98, 541–551 (2020). https://doi.org/10.1007/s00109-020-01880-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-020-01880-4