Abstract
Abdominal aortic aneurysm (AAA) is a common disease that causes progressive expansion and rupture of the aorta with high mortality. There is a large and unmet need for nonsurgical treatment for AAA. Research has shown that an intricate network of inflammatory cells and interstitial cells contributes to the formation of AAA by producing pro-inflammatory mediators that activate enzymes to degrade the extracellular matrix (ECM) and impair ECM biosynthesis. Pharmacological agents such as statins and angiotensin-converting enzyme inhibitors may promote tissue stabilization in AAA by diminishing pro-inflammatory signaling and normalizing metabolism of the ECM. Our recent experiments in animal models demonstrate that inhibition of c-Jun N terminal kinase (JNK) inhibits multiple pathological processes and causes regression of established AAA. Thus, emerging evidence indicates that pharmacological intervention targeting pro-inflammatory signaling and abnormal ECM metabolism is a promising strategy for treatment of AAA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abdominal aortic aneurysm (AAA) is caused by a segmental weakening of the abdominal aortic walls, which leads to progressive aortic dilation. Although patients with AAA usually have no symptoms, it progresses with time, resulting in rupture of the diseased aorta. Aortic rupture frequently causes sudden death, with the mortality rate exceeding 50% even when the patient arrives at the hospital in time for surgical treatment. AAA poses a significant healthcare problem, affecting 6–9% of men over 65 years of age. In the United States, it is the tenth leading cause of death in men over 55 years of age [1]. Because AAA patients usually have no symptoms, the therapeutic goal is rupture prevention. The clinical strategy depends on the diameter of the aneurysm, which is the strongest predictor of rupture risk [2]. With aneurysms greater than 5.5 cm in diameter, the risk of rupture exceeds the risk for elective surgery. Thus, these large aneurysms are treated by surgical procedures which are currently the only established therapeutic option to prevent the aortic rupture. The diseased aorta can be replaced with an artificial graft by open surgery or by endovascular repair where an artificial graft is attached to a metal stent and inserted in the aorta through a catheter. In contrast, there is no effective therapy for small AAA. Graft replacement does not offer a survival advantage for small AAA [3, 4], and clinical trials to determine the effectiveness of endovascular repair for patients with small aneurysms are not yet complete [5]. Therefore, the standard practice for small aneurysms is “watchful waiting,” in which periodical observations are made to assess AAA progression, until the risk of rupture reaches or exceeds the surgical risk. Thus, a nonsurgical therapy that slows progression of the disease would be a significant advance. An even greater advance would be a therapy that not only arrests disease progression but also induces healing and regression of the aneurysm.
Recently, we identified c-Jun N terminal kinase (JNK) as a key molecule in the pathogenesis of AAA [6]. JNK regulates various aspects of the molecular pathogenesis of AAA, promoting the destruction of extracellular matrix (ECM). Inhibition of JNK not only prevents the development of AAA in vivo but also causes regression of established AAA in animal models. Excellent textbooks and reviews of the AAA field are already available ([7, 8] among others). Rather than presenting a comprehensive review, this article summarizes current knowledge of the molecular pathogenesis of AAA as it relates to our study. Putative nonsurgical therapies for altering the pathology of AAA are described and discussed together with our recent findings.
Etiological considerations
Overview
Due to the silent nature of AAA, investigating when and how AAA develops is a challenge. Consequently, little is known about the initiation of AAA, but investigation has primarily consisted of case-control studies of genetic and environmental factors predisposing individuals to AAA. Although familial clustering of AAA has been reported and 15% of AAA patients has a family history of the disease [9], decades of studies reveal that AAA is most likely a polygenic disease under the influence of multiple environmental factors.
Genetic factors
As familial accumulation of AAA has been observed clinically, efforts have been made to identify genetic factors that predispose carriers to the development of AAA (reviewed in [10, 11]). Genome-wide screening in case-control studies has identified several genetic loci associated with AAA, including HLA class II, 19q13, and 4q31. The candidate gene approach has also revealed several genetic polymorphisms that predispose carriers to AAA development. These include polymorphisms of the genes for angiotensin-converting enzyme (ACE), matrix metalloproteinase (MMP)-9, plasminogen activator inhibitor-1 (PAI-1), and interleukin (IL)-10 among others. The reported odds ratios range from 1.34 (PAI-1) to 2.94 (MMP-9). These results have been difficult to replicate in some cases, as with other complex diseases, supporting the idea that AAA is multigenic and multifactorial.
Environmental factors
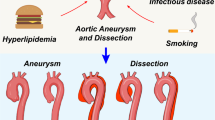
Smoking, age, gender, existence of coronary heart disease, hyperlipidemia, and hypertension all affect the development of AAA. Male gender is a strong risk factor, the effect of which may be mediated by multiple factors including genetic predisposition, hormonal environment, and anatomical factors such as relatively larger aortic diameter than female. Gender, as well as the remaining risk factors, is common to both AAA and atherosclerosis, and nearly all cases of AAA involve atherosclerotic changes. The causative relationship between atherosclerosis and AAA, however, is not firmly established. Indeed, diabetes mellitus, which is strongly linked to atherosclerosis, has repeatedly been shown to negatively correlate with AAA development and progression [9]. Thus, it seems that AAA and atherosclerosis are clinically distinct, although they share some common pathological features such as chronic inflammation and macrophage infiltration.
Chlamydia pneumoniae is a pathogen that is implicated in both AAA development and atherogenesis [9]. Its presumed role in AAA is based on the high prevalence of C. pneumoniae antibodies in the serum of AAA patients and on data showing greater progression of experimental AAA after C. pneumoniae infection. A clinical trial of macrolide roxithromycin for small AAA showed a beneficial effect of the antibiotic [12]. However, the pathogenetic role of C. pneumoniae is still elusive [12], in part, because not all AAA patients appear to be infected with C. pneumoniae, and infection of C. pneumoniae does not correlate with MMP production [9]. Thus, the effect of macrolide may be attributable to its anti-inflammatory or antimicrobial activities [12, 13].
Etiology-oriented therapy
Because the etiology of AAA is largely unknown and probably multifactorial, development of etiology-oriented therapy has been difficult. Notable exceptions are certain monogenic diseases associated with AAA, including Marfan syndrome, Ehlers–Danlos syndrome type IV, and Loeys–Dietz syndrome. Although the genetic defects associated with these monogenic diseases are not yet correctable, a recent study demonstrated the therapeutic effectiveness of the angiotensin AT1 receptor antagonist that ameliorate overactive signaling of transforming growth factor-β (TGF-β) in a mouse model of Marfan syndrome [14]. Interestingly, it has been reported that ACE inhibitors retard the progression of experimental AAA [15] and may suppress aortic rupture in human AAA [16]. It remains to be seen whether AT1 signaling is involved in the etiology of AAA in general and AT1 antagonists are effective in treating human AAA; two reports have shown no beneficial effect of the AT1 antagonists on experimental or human AAA [15, 16].
Molecular pathogenesis of AAA
Overview
There has been extensive effort to unravel the molecular pathogenesis of AAA, understanding of which is requisite to the development of a nonsurgical therapy for the disease. Research has demonstrated the importance of chronic inflammation and degradation of ECM by various proteases to AAA. In addition, impairment of ECM biosynthesis is thought to play a role in the pathogenesis of AAA because AAA is accompanied by a progressive decrease in the number of vascular smooth muscle cells that normally synthesize ECM [17–21]. These pathological processes—inflammation, degradation of the ECM, and impairment of biosynthesis of the ECM—act in concert to promote the progressive destruction of the ECM. During chronic inflammation, inflammatory cells and interstitial cells secrete ECM-degrading proteases and pro-inflammatory cytokines; such cytokines further activate inflammatory signaling and may interfere with the normal biosynthesis of the ECM by interstitial cells. However, our knowledge of the molecular pathogenesis of AAA remains incomplete. For example, it is not known what triggers chronic inflammation and how it is maintained over a period of years or what interferes with the ordered biosynthesis of the ECM that should occur during tissue repair. In addition, the mechanisms for coordination of these events during AAA pathogenesis remain largely unknown.
Proteases
The mechanical strength of the aortic wall is maintained by the ECM, which is mainly composed of collagen and elastin fibers. The most prominent pathological feature of AAA is disruption of the ordered layers of the ECM, including the disappearance of elastic lamellae in the early stage of the disease. Disruption of elastin is sufficient for aneurysmal dilation of the aorta, and degradation of collagen is responsible for rupture [22, 23].
For these reasons, there has been a major effort to elucidate the mechanism for the degradation of the ECM, with a focus on elastolytic factors. This has led to the identification of various proteases in AAA tissue. Among them, the MMPs have drawn much attention, with MMP-9 and MMP-2 being the most extensively studied. A major breakthrough in AAA research was the finding that deletion of the genes for MMP-9 [24] and/or MMP-2 [25] completely protects mice from development of AAA. Subsequent to this finding, it was proposed that MMP inhibition is a potentially effective therapy for AAA.
Pro-inflammatory mediators
The chronic inflammation in AAA seems to be initiated and maintained by a complex interplay between innate and acquired immunity [26]. Infiltrating cellular components include macrophages, T cells, and B cells. Chronic inflammation is an essential component of AAA pathogenesis, as cytokine-stimulated macrophages are the major source of matrix-degrading enzymes such as MMP-9 and pro-inflammatory cytokines such as tumor necrosis factor (TNF)-α.
The degradation products of elastin [27] or collagen [28] can initiate the inflammatory response, and cleavage of IL-8 by MMP-9 potentiates its ability to activate leukocytes [29]. These facts exemplify the intimate interplay between inflammatory signaling and MMP activities. However, these processes are experimentally separable: Mice deficient in MMP-9 and/or MMP-2 are protected from the development of AAA by infusion of elastase or CaCl2 treatment of the aorta, but not protected from inflammatory responses [24, 25]. Doxycycline treatment inhibits the development of experimental AAA, but does not eliminate the inflammatory response [30], suggesting that the inflammatory response is maintained independently of MMP activities.
Various pro-inflammatory mediators are present in AAA tissue, including TNF-α, IL-1β, IL-6, and interferon (IFN)-γ [1]. In addition to these peptide mediators, lipid mediators such as prostaglandin E2 [31–33] and leukotriene D4 (LTD4) [34] and the gaseous mediator nitric oxide [35, 36] have also been reported to play important roles in AAA. However, the precise roles of these inflammatory mediators and the relationships among them have not been elucidated and are likely to vary during the course of the disease.
These mediators affect not only inflammatory cells but also interstitial cells such as vascular smooth muscle cells, endothelial cells, and fibroblasts. For example, prostaglandin E2 inhibits the growth of vascular smooth muscle cells [32]. It was proposed that LTD4, a metabolic product of arachidonic acid 5-lipoxygenase (ALOX5), induces macrophage inflammatory protein-1α (MIP-1α) in macrophages and MIP-2 in endothelial cells, which in turn, recruit leukocytes into the aortic walls [34]. IFN-γ suppresses collagen I expression during tissue repair [37], and TNF-α suppresses the wound repair response of vascular smooth muscle cells [38] and decreases the expression of collagen type I and III in fibroblasts in a JNK-dependent manner [39]. Taken together, these findings suggest that inflammatory signaling suppresses normal ECM biosynthesis and tissue repair independent of ECM-degrading activities.
Impairment of ECM biosynthesis
In the healthy artery, interstitial cells such as vascular smooth muscle cells maintain the ordered structure of the ECM through active biosynthesis. Because vascular smooth muscle cells are depleted in human AAA, it has been hypothesized that impaired biosynthesis of the ECM plays a critical role in the pathogenesis of AAA [17–21].
Biosynthesis of collagen and elastin fibers, the major components of aortic ECM, is regulated at the level of expression as well as by post-translational modifications such as prolyl and lysyl hydroxylation and lysyl oxidation. These post-translational modifications are catalyzed by prolyl 4-hydroxylase (P4H), pro-collagen lysyl hydroxylase (PLOD), and lysyl oxidase (LOX). These ECM biosynthetic enzymes are essential for stable trimerization of collagen fibrils and cross-linking of collagen and elastin fibrils to form durable fibers. The critical role of ECM biosynthesis in maintaining the integrity of aortic walls is demonstrated by the finding that disruption of the LOX gene leads to aneurysm formation and aortic rupture [20]. In addition, it has been reported that expression of LOX is reduced in aneurysm-prone mice [18] and in experimental AAA [6, 17]. This may explain the ineffective maturation of the ECM in human AAA [19, 21]. A PLOD1 mutation in patients with Ehlers–Danlos syndrome causes a high risk of arterial rupture [40]. Taken together, these observations demonstrate the profound effect of impaired ECM biosynthesis on the integrity of arterial walls. Indeed, we found that adenoviral expression of exogenous LOX inhibits the development of experimental AAA in which endogenous LOX activity is suppressed [6].
Therapeutic targets in AAA
Overview
Based on their proposed roles in the pathogenesis of AAA, chronic inflammation, degradation of ECM by MMPs, and impaired biosynthesis of the ECM have been targeted with therapeutic interventions. These therapeutic strategies have proven effective to various extents in preventing the progression of experimental AAA, providing strong support for the working model of AAA pathogenesis.
Inhibition of MMP
MMP inhibition is the therapeutic strategy that has been most extensively explored in clinical trials involving AAA [41]. This is partly because of the prominent role of MMPs in AAA pathogenesis and partly because of the clinical availability of the MMP inhibitor doxycycline. Inhibition of MMP prevents the development of AAA in animal models; this has been demonstrated using both doxycycline [17, 30, 42] and another MMP inhibitor, BB-94 [43]. This underscores the critical role of MMPs in the pathogenesis of AAA. In addition, clinical trials of doxycycline show the feasibility of this approach and some favorable effects [44, 45], although these studies were designed to evaluate the safety of doxycycline and the therapeutic effect was not as clear as that demonstrated in animal models.
Another experimental approach for inhibiting MMP activity is the forced expression of tissue inhibitor of metalloproteinases (TIMP)-1 in smooth muscle cells and the seeding of these cells into an aortic xenograft. This has been shown to stabilize grafts and prevent rupture [46]. However, clinical application of the gene transfer approach awaits further technical advancements such as improved vector design and improved control of gene expression. The enduring nature of gene transfer may have advantages over conventional pharmacotherapy, as a one-time treatment may last for years. However, this may also be a disadvantage if adverse effects occur due to uncontrolled gene expression or faulty vector function.
Anti-inflammatory therapy
Experiments in animal models of AAA have demonstrated that immunosuppression with prednisone, cyclosporine [47], or rapamycin [48] prevents the development of experimental AAA induced by elastase infusion. However, general immunosuppression by steroids or cyclosporine may not be sufficient to suppress the progression of AAA in humans [9], suggesting that more specific targets need to be identified.
Inhibition of the pro-inflammatory cytokine TNF-α [49] or the chemokine MCP-1 [50] suppresses the development of AAA in animal models. Interestingly, inhibition of IL-1β, another potent pro-inflammatory cytokine present in human AAA, is ineffective [49], suggesting that the various pro-inflammatory mediators play specialized roles in this context. More recently, it was shown that inhibition of NFκB, a critical transcription factor in cytokine signal transduction, by NFκB/Ets decoy oligonucleotide [51] or by a chemical inhibitor [52], prevents the development of experimental AAA.
The nonselective cyclooxygenase inhibitor indomethacin [31] and the selective cyclooxygenase-2 inhibitor celecoxib [33] have been reported to prevent AAA in animal models, demonstrating the critical roles of arachidonate metabolites in the development of AAA. A case-control study showed that AAA patients taking nonsteroidal anti-inflammatory drugs (NSAIDs) have aneurysms with a lower expansion rate than those in patients who do not take NSAIDs [32], suggesting that this class of drugs may be beneficial in this population. The gaseous mediator nitric oxide may be a therapeutic target, as it directly activates MMP-9 [53]. Furthermore, an inhibitor of inducible nitric oxide synthase (iNOS) prevents elastase-induced AAA development in animal models [36]. However, targeted deletion of the iNOS gene does not protect mice from elastase-induced AAA [54], suggesting that nitric oxide plays a context-specific role.
Other pharmacological interventions, including 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors (statins) [55–58] and ACE inhibitors [15, 16, 59], have been reported to prevent the progression of AAA possibly by suppressing inflammation. ACE inhibition is a promising therapy; a large-scale case-control study showed that treatment with ACE inhibitors is associated with reduced AAA rupture [16]. In contrast, AT1 receptor blockers do not show a beneficial effect with regard to AAA [15, 16], suggesting that the renin–angiotensin system plays a complex role in the pathogenesis of AAA. Statins, in addition to their lipid-lowering effect, suppress inflammatory signaling possibly by inhibiting the Rho family of small G-proteins. Case-control studies have demonstrated an association between use of statins and reduction in the levels of some MMPs [60] as well as a lower rate of expansion of AAA [58, 61]. ACE inhibitors and statins would merit larger systematic randomized clinical trials to confirm their benefits and to determine the optimal regimen for preventing the expansion and rupture of AAA.
MMP inhibition alone does not suppress infiltration of inflammatory cells [24, 25, 30]. Conversely, suppression of inflammatory signaling does not always reduce levels of MMP [31, 36]. Because pro-inflammatory mediators may promote the progression of AAA independent of MMPs, anti-inflammatory therapies may be a good strategy for treating AAA possibly in combination with MMP inhibition.
Stabilization of the ECM
ECM biosynthesis and stabilization have not been studied as extensively for AAA therapy as have MMP inhibitors and pro-inflammatory mediators. One reason for this is that although impairment of ECM biosynthesis has been demonstrated in experimental animals [17, 18] and is suspected in clinical settings [19, 21], the causal role of the impaired ECM biosynthesis in AAA pathogenesis is unclear. Other reasons include lack of knowledge regarding the molecular mechanisms underlying impaired ECM biosynthesis and the lack of reagents that specifically promote the biosynthesis of well-ordered and durable ECM. One proposed method for promoting ECM biosynthesis is seeding smooth muscle cells in an AAA model induced by xenografting a guinea pig aorta into a rat. Seeding of syngeneic rat vascular smooth muscle cells stabilizes aortic tissue [62], and this effect is enhanced by adenoviral expression of TGF-β1 [63]. These findings support the feasibility of therapy that increases ECM biosynthesis. This approach may be as effective as, and perhaps complementary to, inhibition of MMP. However, activation of the TGF-β pathway must be approached cautiously. Recent studies indicate that overactivation of TGF-β signaling in the aortic wall exacerbates inflammation and causes progression of AAA in humans [64, 65] and in an animal model of Marfan syndrome [14].
Regression of AAA via pharmacotherapy
Overview
Regression of AAA via pharmacotherapy, if clinically applicable, would offer a therapeutic option for patients with small aneurysms. Patients with larger aneurysms and a high risk of rupture might not immediately benefit from pharmacotherapy, as it would not instantaneously reduce rupture risk. However, pharmacotherapy could be used to treat patients with both high rupture risk and high surgical risk, for example, patients with AAA and multiple comorbidities such as pulmonary failure and renal failure.
It is becoming increasingly clear that the tissue degeneration observed in AAA is a consequence of an imbalance between tissue degradation and repair. However, active tissue repair is ongoing in aneurysms, as evidenced by increased expression of tropoelastin [21] and collagen [66]. It is thought that inhibition of MMP [17] or endovascular seeding of vascular smooth muscle cells [62] may sometimes cause regression of experimental AAA. Tissue repair in AAA also manifests clinically. Endovascular repair by insertion of stent-grafts often causes shrinkage of the aneurysmal aorta [67] and remission of the tissue degradation process [68], suggesting that regression of AAA is possible in certain situations.
As discussed above, the current view of AAA pathogenesis is that it is the result of a complex interplay among distinct pathological processes: chronic inflammation, ECM degradation, and impaired ECM biosynthesis. Each pathological process involves a network of signaling molecules and effector molecules whose levels of expression are differentially regulated [69–71]. In this regard, AAA progression is a highly ordered and regulated process. Although intervention in each process has proven effective in preventing the development or progression of experimental AAA, none of these therapeutic strategies reverses disease progression. This suggests that either AAA is a fundamentally irreversible destructive process or that we do not yet understand the key molecular mechanisms that prevent the healing of AAA. Alternatively, several simultaneous interventions may be required to induce efficient healing.
Although the mechanisms responsible for initiation of AAA are not known and may well be heterogeneous, the clinical course and pathology are known and fairly predictable. This suggests that various environmental and genetic stimuli may activate a final common pathway or “node” in the AAA signaling network that orchestrates chronic inflammation, ECM degradation, and impairment of ECM biosynthesis. Such a node, if it exists, would be an ideal therapeutic target for affecting multiple pathological processes and promoting healing of AAA.
Identification of JNK as a therapeutic target
In an attempt to identify a key therapeutic target for AAA, we assessed the phosphorylation status of signaling molecules in human AAA samples, including JNK, p38, extracellular signal-regulated kinase (ERK), signal transducer and activator of transcription (STAT) 2, STAT3, activating transcription factor (ATF) 2, inhibitor of κ light polypeptide gene enhancer in B cells (IκB)-α, Akt, glycogen synthase kinase (GSK) 3β, 70 kDa ribosomal protein S6 kinase (p70S6K), and 90 kDa ribosomal protein S6 kinase (p90RSK), all of which are regulated by reversible phosphorylation. Screening revealed increased phosphorylation of JNK, ERK, and STAT3 compared with a non-aneurysmal control. Of these proteins, JNK was a prime candidate because it is activated by stimuli that have been implicated in AAA pathogenesis: mechanical stress, oxidative stress, angiotensin II, TNF-α, IL-1β, IL-6, and IFN-γ. In addition, JNK induces MMP-9 in several cell lines [72–75]. A transcriptome analysis in vascular smooth muscle cells revealed that JNK upregulates pro-inflammatory molecules such as IL-1α, iNOS, ALOX5-activating protein (ALOX5AP), and the ECM-degrading MMP-9. At the same time, JNK downregulates TIMP-3, an endogenous inhibitor of MMPs, and critical ECM biosynthetic enzymes including PLOD1, P4HA1, and LOX. Therefore, JNK is an ideal therapeutic target because it coordinately regulates multiple pathological processes involved in tissue degradation, thus, serving as a node in the AAA signaling network (Fig. 1).
JNK-regulated gene expression. JNK is activated in macrophages and in vascular smooth muscle cells (VSMCs) in AAA tissue. JNK induces the expression of MMPs and pro-inflammatory mediators, including TNF-α, IL-1α, and arachidonate 5-lipoxygenase-activating protein (ALOX5AP). Inducible nitric oxide synthase (iNOS) generates nitric oxide (NO), which activates MMP-9 by S-nitrosylation [53]. Lipocalin-2 binds to MMP-9 and maintains its activity [99]. In addition, JNK suppresses tissue inhibitor of metalloproteinase-3 (TIMP-3), an endogenous inhibitor of MMPs, and critical ECM biosynthetic enzymes, including prolyl 4-hydroxylase (P4H), pro-collagen lysyl hydroxylase (PLOD), and lysyl oxidase (LOX)
JNK inhibition by SP600125 in vivo completely prevented the development of AAA in response to abluminal application of CaCl2 in mouse aorta (Fig. 2). Importantly, JNK inhibition strongly suppressed macrophage infiltration of the periaortic tissue, whereas doxycycline did not [30], suggesting that JNK is critically involved in the pro-inflammatory signaling process [76, 77]. In vivo JNK inhibition was also effective in treating established AAA induced by CaCl2 treatment in wild-type mice and by continuous infusion of angiotensin II in ApoE knockout mice [78]. SP600125 caused significant regression of established AAA and normalized tissue architecture, indicating that JNK inhibition is a promising therapeutic modality.
JNK inhibition therapy for AAA. a CaCl2 treatment of mouse aorta causes an increase in expression of MMP-9, infiltration of macrophages (Mφ, arrowheads), and development of AAA after 10 weeks in mice treated with vehicle. Inhibition of JNK by SP600125 (SP) completely prevents development of AAA and suppresses MMP-9 and Mφ infiltration. b Adenoviral gene transfer of LOX partially prevents the development of AAA. Compared to LacZ-transduced aorta (control), LOX-transduced aorta exhibit less disruption of elastic lamellae, as shown by elastica van Gieson (EVG) stain, and less cellular infiltration, as shown by hematoxylin–eosin (H&E) stain. c The mouse model of AAA was established 6 weeks after CaCl2 treatment. After AAA was established, JNK inhibition was initiated via treatment with SP600125 (SP). After 6 weeks of SP600125 treatment, there was regression of AAA and repair of tissue architecture (modified from [6])
Implications and future directions
Despite decades of effort, the exact etiology of AAA remains elusive and is likely to be heterogeneous. However, emerging evidence supports the notion that the vicious cycle of chronic inflammation and abnormal ECM metabolism is the final common pathway in the molecular pathogenesis of AAA. Central to this pathway is the signaling network, including JNK pathway, that coordinates inflammation and abnormal metabolism of the ECM. Pro-inflammatory mediators such as chemokines, cytokines, and angiotensin II cause infiltration and activation of inflammatory cells and increase in hemodynamic stress. This causes activation of the intracellular signaling network to dictate the destructive metabolism of the ECM and production of pro-inflammatory mediators. Abnormal ECM metabolism weakens the aortic wall, causing expansion of AAA and exposure of interstitial cells to higher mechanical and metabolic stress. This, in turn, exacerbates abnormal intracellular signaling. The central role of JNK in chronic inflammation and the abnormal metabolism of the ECM in AAA provides a framework for understanding the coordination of these pathological processes (Fig. 3) and an opportunity to develop a therapeutic intervention for reversing AAA.
The AAA signaling network. The current working hypothesis for the molecular pathogenesis of AAA is that JNK coordinates a pattern of gene expression that promotes tissue destruction and progression of AAA. Inhibition of JNK decreases chronic inflammation and degradation of the ECM and simultaneously allows recovery of ECM biosynthesis. Thus, JNK inhibition increases tissue repair and causes AAA to regress
A critical unanswered question is what triggers the abnormal activation of intracellular signaling and keeps it continuously active in human AAA. If the aforementioned vicious cycle maintains the chronic inflammation observed in AAA, what is the most effective point of intervention to end the cycle? Although our data support the JNK pathway as an important candidate, answering this question requires understanding of the complex network of inflammatory signaling in AAA and the relationship of the JNK pathway to other signaling pathways. For example, pro-inflammatory cytokines frequently activate both activator protein-1 (AP-1), the downstream target of the JNK pathway, and NFκB, and these transcription factors have been reported to synergistically activate downstream genes including MMP-9 [79] and pro-inflammatory cytokines [80, 81]. However, the JNK and NFκB pathways sometimes antagonize each other [82], exemplifying the complexity of the inflammatory signaling network. STAT3, another transcription factor activated in human AAA, may also cooperate with AP-1 in the IL-6-induced response to injury [83, 84] and in IL-17-induced expression of MMP-9 [85]. It remains to be seen whether intervention in these parallel signaling pathways promotes healing in AAA.
Concerning the molecular mechanisms by which JNK promotes the progression of AAA, pathological processes other than ECM metabolism may be involved. Numerous reports and our transcriptional profiling [6] indicate that JNK affects many cellular processes [76, 77], including cell proliferation, cell differentiation, metabolic pathways, cell migration [86], cell survival, and cell death [87, 88]. JNK may also be involved in the loss of vascular smooth muscle cells in the medial layer of the diseased aorta. Different JNK isoforms play different roles in various physiological [89, 90] and pathophysiological settings [91, 92], including AAA (KY and HA, unpublished observation). Thus, the isoform-specific role of JNK in AAA should be explored in detail. Isoform-specific inhibition of JNK may circumvent the possible adverse effects of systemic inhibition of all JNK isoforms.
With regard to reducing the side-effects of pharmacotherapy, local delivery of pharmacological agents should be considered. The efficacy of this approach was demonstrated in a recent study using doxycycline and a rat model of AAA [93]. The rapid advancement of drug-eluting stent technology and the growing prevalence of endovascular repair make stent-grafts an obvious choice for drug delivery. Regression of AAA by pharmacotherapy, if validated in humans, will improve graft fitting. JNK inhibition may also prevent thrombus formation, as recently demonstrated for coronary stent thrombosis [94]. Although the intramural thrombus may pose a barrier to the passive diffusion of pharmacological agents from an eluting stent-graft, the thrombus per se may be a therapeutic target [95, 96] because the mural thrombus may promote the progression and rupture of AAA [97] by actively producing proteases [98]. On the other hand, systemically administrated pharmacological agents may have better access to the adventitia, the site of inflammation in AAA, than agents released from inside the aorta. Further progress with drug delivery systems, including drug-eluting stent-grafts, and validation of their efficacy in vivo will advance the development of less invasive therapeutic strategies for AAA.
Conclusions
We are witnessing a rapid progress in understanding the molecular pathogenesis of AAA. This led to the proposal of promising pharmacotherapy with statins, ACE inhibitors, and JNK inhibitor among others. Accumulating knowledge obtained in the research of AAA may also create new avenues for improved therapeutic strategies not only for AAA but also for other diseases. Chronic inflammation and destructive remodeling of the ECM are widely observed in a variety of diseases, including rheumatoid arthritis, osteoarthritis, valvular heart disease, vulnerable atheromatous plaque, chronic obstructive pulmonary disease, and cancer. There may be a common abnormality of cellular signaling that positively regulates the destructive processes underlying these diseases and AAA. Then, how does the signaling network that is centered on the JNK pathway fit into the molecular pathogenesis of these diseases? How can therapeutic manipulation of the signaling pathways decrease the chronic inflammation and progressive tissue destruction observed in all of these pathologies? We are optimistic that the answers to these questions will lead to better future treatment of AAA and other diseases.
References
Curci JA, Lee JK, Thompson RW (2001) Pathogenesis of abdominal aortic aneurysm. In: Ernst CB, Stanley JC (eds) Current therapy in vascular surgery. Elsevier, Philadelphia, pp 199–206
Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM Jr, White CJ, White J, White RA, Antman EM, Smith SC Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Hunt SA, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B (2006) ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (writing committee to develop guidelines for the management of patients with peripheral arterial disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 113:e463–654
Participants UKSAT (2002) Long-term outcomes of immediate repair compared with surveillance of small abdominal aortic aneurysms. N Engl J Med 346:1445–1452
Lederle FA, Wilson SE, Johnson GR, Reinke DB, Littooy FN, Acher CW, Ballard DJ, Messina LM, Gordon IL, Chute EP, Krupski WC, Busuttil SJ, Barone GW, Sparks S, Graham LM, Rapp JH, Makaroun MS, Moneta GL, Cambria RA, Makhoul RG, Eton D, Ansel HJ, Freischlag JA, Bandyk D (2002) Immediate repair compared with surveillance of small abdominal aortic aneurysms. N Engl J Med 346:1437–1444
Cao P, Collaborators CT (2005) Comparison of surveillance vs aortic endografting for small aneurysm repair (CAESAR) trial: study design and progress. Eur J Vasc Endovasc Surg 30:245–251
Yoshimura K, Aoki H, Ikeda Y, Fujii K, Akiyama N, Furutani A, Hoshii Y, Tanaka N, Ricci R, Ishihara T, Esato K, Hamano K, Matsuzaki M (2005) Regression of abdominal aortic aneurysm by inhibition of c-Jun N-terminal kinase. Nat Med 11:1330–1338
Bergoeing MP, Thompson RW, Curci JA (2006) Pharmacological targets in the treatment of abdominal aortic aneurysms. Expert Opin Ther Targets 10:547–559
Dawson J, Choke E, Sayed S, Cockerill G, Loftus I, Thompson MM (2006) Pharmacotherapy of abdominal aortic aneurysms. Curr Vasc Pharmacol 4:129–149
Curci JA, Baxter BT, Thompson RW (2005) Arterial aneurysms: etiologic considerations. In: Rutherford RB (ed) Vascular surgery. Saunders, Philadelphia, pp 475–492
van Vlijmen-van Keulen CJ, Pals G, Rauwerda JA (2002) Familial abdominal aortic aneurysm: a systematic review of a genetic background. Eur J Vasc Endovasc Surg 24:105–116
Golledge J, Muller J, Daugherty A, Norman P (2006) Abdominal aortic aneurysm: pathogenesis and implications for management. Arterioscler Thromb Vasc Biol 26:2605–2613
Vammen S, Lindholt JS, Ostergaard L, Fasting H, Henneberg EW (2001) Randomized double-blind controlled trial of roxithromycin for prevention of abdominal aortic aneurysm expansion. Br J Surg 88:1066–1072
Gibbs R (2002) Randomized double-blind controlled trial of roxithromycin for prevention of abdominal aortic aneurysm expansion. Br J Surg 89:491–492
Habashi JP, Judge DP, Holm TM, Cohn RD, Loeys BL, Cooper TK, Myers L, Klein EC, Liu G, Calvi C, Podowski M, Neptune ER, Halushka MK, Bedja D, Gabrielson K, Rifkin DB, Carta L, Ramirez F, Huso DL, Dietz HC (2006) Losartan, an AT1 antagonist, prevents aortic aneurysm in a mouse model of Marfan syndrome. Science 312:117–121
Liao S, Miralles M, Kelley BJ, Curci JA, Borhani M, Thompson RW (2001) Suppression of experimental abdominal aortic aneurysms in the rat by treatment with angiotensin-converting enzyme inhibitors. J Vasc Surg 33:1057–1064
Hackam DG, Thiruchelvam D, Redelmeier DA (2006) Angiotensin-converting enzyme inhibitors and aortic rupture: a population-based case-control study. Lancet 368:659–665
Huffman MD, Curci JA, Moore G, Kerns DB, Starcher BC, Thompson RW (2000) Functional importance of connective tissue repair during the development of experimental abdominal aortic aneurysms. Surgery 128:429–438
Rowe D, McGoodwin E, Martin G, Grahn D (1977) Decreased lysyl oxidase activity in the aneurysm-prone, mottled mouse. J Biol Chem 252:939–942
Bode MK, Mosorin M, Satta J, Risteli L, Juvonen T, Risteli J (2002) Increased amount of type III pN-collagen in AAA when compared with AOD. Eur J Vasc Endovasc Surg 23:413–420
Maki J, Rasanen J, Tikkanen H, Sormunen R, Makikallio K, Kivirikko K, Soininen R (2002) Inactivation of the lysyl oxidase gene Lox leads to aortic aneurysms, cardiovascular dysfunction, and perinatal death in mice. Circulation 106:2503–2509
Krettek A, Sukhova GK, Libby P (2003) Elastogenesis in human arterial disease: a role for macrophages in disordered elastin synthesis. Arterioscler Thromb Vasc Biol 23:582–587
Dobrin PB, Mrkvicka R (1994) Failure of elastin or collagen as possible critical connective tissue alterations underlying aneurysmal dilatation. Cardiovasc Surg 2:484–488
Dobrin PB, Baker WH, Gley WC (1984) Elastolytic and collagenolytic studies of arteries. Implications for the mechanical properties of aneurysms. Arch Surg 119:405–409
Pyo R, Lee JK, Shipley JM, Curci JA, Mao D, Ziporin SJ, Ennis TL, Shapiro SD, Senior RM, Thompson RW (2000) Targeted gene disruption of matrix metalloproteinase-9 (gelatinase B) suppresses development of experimental abdominal aortic aneurysms. J Clin Invest 105:1641–1649
Longo GM, Xiong W, Greiner TC, Zhao Y, Fiotti N, Baxter BT (2002) Matrix metalloproteinases 2 and 9 work in concert to produce aortic aneurysms. J Clin Invest 110:625–632
Curci JA, Thompson RW (2004) Adaptive cellular immunity in aortic aneurysms: cause, consequence, or context? J Clin Invest 114:168–171
Hance KA, Tataria M, Ziporin SJ, Lee JK, Thompson RW (2002) Monocyte chemotactic activity in human abdominal aortic aneurysms: role of elastin degradation peptides and the 67-kD cell surface elastin receptor. J Vasc Surg 35:254–261
Weathington NM, van Houwelingen AH, Noerager BD, Jackson PL, Kraneveld AD, Galin FS, Folkerts G, Nijkamp FP, Blalock JE (2006) A novel peptide CXCR ligand derived from extracellular matrix degradation during airway inflammation. Nat Med 12:317–323
Van den Steen PE, Proost P, Wuyts A, Van Damme J, Opdenakker G (2000) Neutrophil gelatinase B potentiates interleukin-8 tenfold by aminoterminal processing, whereas it degrades CTAP-III, PF-4, and GRO-alpha and leaves RANTES and MCP-2 intact. Blood 96:2673–2681
Petrinec D, Liao S, Holmes DR, Reilly JM, Parks WC, Thompson RW (1996) Doxycycline inhibition of aneurysmal degeneration in an elastase-induced rat model of abdominal aortic aneurysm: preservation of aortic elastin associated with suppressed production of 92 kD gelatinase. J Vasc Surg 23:336–346
Miralles M, Wester W, Sicard GA, Thompson R, Reilly JM (1999) Indomethacin inhibits expansion of experimental aortic aneurysms via inhibition of the cox2 isoform of cyclooxygenase. J Vasc Surg 29:884–892; discussion 892–883
Walton LJ, Franklin IJ, Bayston T, Brown LC, Greenhalgh RM, Taylor GW, Powell JT (1999) Inhibition of prostaglandin E2 synthesis in abdominal aortic aneurysms: implications for smooth muscle cell viability, inflammatory processes, and the expansion of abdominal aortic aneurysms. Circulation 100:48–54
King VL, Trivedi DB, Gitlin JM, Loftin CD (2006) Selective cyclooxygenase-2 inhibition with celecoxib decreases angiotensin II-induced abdominal aortic aneurysm formation in mice. Arterioscler Thromb Vasc Biol 26:1137–1143
Zhao L, Moos MP, Grabner R, Pedrono F, Fan J, Kaiser B, John N, Schmidt S, Spanbroek R, Lotzer K, Huang L, Cui J, Rader DJ, Evans JF, Habenicht AJ, Funk CD (2004) The 5-lipoxygenase pathway promotes pathogenesis of hyperlipidemia-dependent aortic aneurysm. Nat Med 10:966–973
Johanning JM, Franklin DP, Han DC, Carey DJ, Elmore JR (2001) Inhibition of inducible nitric oxide synthase limits nitric oxide production and experimental aneurysm expansion. J Vasc Surg 33:579–586
Armstrong PJ, Franklin DP, Carey DJ, Elmore JR (2005) Suppression of experimental aortic aneurysms: comparison of inducible nitric oxide synthase and cyclooxygenase inhibitors. Ann Vasc Surg 19:248–257
Amento EP, Ehsani N, Palmer H, Libby P (1991) Cytokines and growth factors positively and negatively regulate interstitial collagen gene expression in human vascular smooth muscle cells. Arterioscler Thromb 11:1223–1230
Villacorta L, Graca-Souza AV, Ricciarelli R, Zingg JM, Azzi A (2003) Alpha-tocopherol induces expression of connective tissue growth factor and antagonizes tumor necrosis factor-alpha-mediated downregulation in human smooth muscle cells. Circ Res 92:104–110
Verrecchia F, Tacheau C, Wagner EF, Mauviel A (2003) A central role for the JNK pathway in mediating the antagonistic activity of pro-inflammatory cytokines against transforming growth factor-beta-driven SMAD3/4-specific gene expression. J Biol Chem 278:1585–1593
Ha VT, Marshall MK, Elsas LJ, Pinnell SR, Yeowell HN (1994) A patient with Ehlers–Danlos syndrome type VI is a compound heterozygote for mutations in the lysyl hydroxylase gene. J Clin Invest 93:1716–1721
Thompson RW, Baxter BT (1999) MMP inhibition in abdominal aortic aneurysms. Rationale for a prospective randomized clinical trial. Ann N Y Acad Sci 878:159–178
Prall AK, Longo GM, Mayhan WG, Waltke EA, Fleckten B, Thompson RW, Baxter BT (2002) Doxycycline in patients with abdominal aortic aneurysms and in mice: comparison of serum levels and effect on aneurysm growth in mice. J Vasc Surg 35:923–929
Bigatel DA, Elmore JR, Carey DJ, Cizmeci-Smith G, Franklin DP, Youkey JR (1999) The matrix metalloproteinase inhibitor BB-94 limits expansion of experimental abdominal aortic aneurysms. J Vasc Surg 29:130–138
Mosorin M, Juvonen J, Biancari F, Satta J, Surcel HM, Leinonen M, Saikku P, Juvonen T (2001) Use of doxycycline to decrease the growth rate of abdominal aortic aneurysms: a randomized, double-blind, placebo-controlled pilot study. J Vasc Surg 34:606–610
Baxter BT, Pearce WH, Waltke EA, Littooy FN, Hallett JW Jr, Kent KC, Upchurch GR Jr, Chaikof EL, Mills JL, Fleckten B, Longo GM, Lee JK, Thompson RW (2002) Prolonged administration of doxycycline in patients with small asymptomatic abdominal aortic aneurysms: report of a prospective (Phase II) multicenter study. J Vasc Surg 36:1–12
Allaire E, Forough R, Clowes M, Starcher B, Clowes AW (1998) Local overexpression of TIMP-1 prevents aortic aneurysm degeneration and rupture in a rat model. J Clin Invest 102:1413–1420
Dobrin PB, Baumgartner N, Anidjar S, Chejfec G, Mrkvicka R (1996) Inflammatory aspects of experimental aneurysms. Effect of methylprednisolone and cyclosporine. Ann N Y Acad Sci 800:74–88
Lawrence DM, Singh RS, Franklin DP, Carey DJ, Elmore JR (2004) Rapamycin suppresses experimental aortic aneurysm growth. J Vasc Surg 40:334–338
Hingorani A, Ascher E, Scheinman M, Yorkovich W, DePippo P, Ladoulis CT, Salles-Cunha S (1998) The effect of tumor necrosis factor binding protein and interleukin-1 receptor antagonist on the development of abdominal aortic aneurysms in a rat model. J Vasc Surg 28:522–526
Ishibashi M, Egashira K, Zhao Q, Hiasa K, Ohtani K, Ihara Y, Charo IF, Kura S, Tsuzuki T, Takeshita A, Sunagawa K (2004) Bone marrow-derived monocyte chemoattractant protein-1 receptor CCR2 is critical in angiotensin II-induced acceleration of atherosclerosis and aneurysm formation in hypercholesterolemic mice. Arterioscler Thromb Vasc Biol 24:e174–e178
Nakashima H, Aoki M, Miyake T, Kawasaki T, Iwai M, Jo N, Oishi M, Kataoka K, Ohgi S, Ogihara T, Kaneda Y, Morishita R (2004) Inhibition of experimental abdominal aortic aneurysm in the rat by use of decoy oligodeoxynucleotides suppressing activity of nuclear factor kappaB and ets transcription factors. Circulation 109:132–138
Parodi FE, Mao D, Ennis TL, Bartoli MA, Thompson RW (2005) Suppression of experimental abdominal aortic aneurysms in mice by treatment with pyrrolidine dithiocarbamate, an antioxidant inhibitor of nuclear factor-kappaB. J Vasc Surg 41:479–489
Gu Z, Kaul M, Yan B, Kridel SJ, Cui J, Strongin A, Smith JW, Liddington RC, Lipton SA (2002) S-nitrosylation of matrix metalloproteinases: signaling pathway to neuronal cell death. Science 297:1186–1190
Lee JK, Borhani M, Ennis TL, Upchurch Jr GR, Thompson RW (2001) Experimental abdominal aortic aneurysms in mice lacking expression of inducible nitric oxide synthase. Arterioscler Thromb Vasc Biol 21:1393–1401
Nagashima H, Aoka Y, Sakomura Y, Sakuta A, Aomi S, Ishizuka N, Hagiwara N, Kawana M, Kasanuki H (2002) A 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, cerivastatin, suppresses production of matrix metalloproteinase-9 in human abdominal aortic aneurysm wall. J Vasc Surg 36:158–163
Kalyanasundaram A, Elmore JR, Manazer JR, Golden A, Franklin DP, Galt SW, Zakhary EM, Carey DJ (2006) Simvastatin suppresses experimental aortic aneurysm expansion. J Vasc Surg 43:117–124
Steinmetz EF, Buckley C, Shames ML, Ennis TL, Vanvickle-Chavez SJ, Mao D, Goeddel LA, Hawkins CJ, Thompson RW (2005) Treatment with simvastatin suppresses the development of experimental abdominal aortic aneurysms in normal and hypercholesterolemic mice. Ann Surg 241:92–101
Schouten O, van Laanen JH, Boersma E, Vidakovic R, Feringa HH, Dunkelgrun M, Bax JJ, Koning J, van Urk H, Poldermans D (2006) Statins are associated with a reduced infrarenal abdominal aortic aneurysm growth. Eur J Vasc Endovasc Surg 32:21–26
da Cunha V, Tham DM, Martin-McNulty B, Deng G, Ho JJ, Wilson DW, Rutledge JC, Vergona R, Sullivan ME, Wang YX (2005) Enalapril attenuates angiotensin II-induced atherosclerosis and vascular inflammation. Atherosclerosis 178:9–17
Wilson WR, Evans J, Bell PR, Thompson MM (2005) HMG-CoA reductase inhibitors (statins) decrease MMP-3 and MMP-9 concentrations in abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 30:259–262
Sukhija R, Aronow WS, Sandhu R, Kakar P, Babu S (2006) Mortality and size of abdominal aortic aneurysm at long-term follow-up of patients not treated surgically and treated with and without statins. Am J Cardiol 97:279–280
Allaire E, Muscatelli-Groux B, Guinault AM, Pages C, Goussard A, Mandet C, Bruneval P, Melliere D, Becquemin JP (2004) Vascular smooth muscle cell endovascular therapy stabilizes already developed aneurysms in a model of aortic injury elicited by inflammation and proteolysis. Ann Surg 239:417–427
Dai J, Losy F, Guinault AM, Pages C, Anegon I, Desgranges P, Becquemin JP, Allaire E (2005) Overexpression of transforming growth factor-beta1 stabilizes already-formed aortic aneurysms: a first approach to induction of functional healing by endovascular gene therapy. Circulation 112:1008–1015
Nataatmadja M, West J, West M (2006) Overexpression of transforming growth factor-beta is associated with increased hyaluronan content and impairment of repair in Marfan syndrome aortic aneurysm. Circulation 114:I371–377
Loeys BL, Chen J, Neptune ER, Judge DP, Podowski M, Holm T, Meyers J, Leitch CC, Katsanis N, Sharifi N, Xu FL, Myers LA, Spevak PJ, Cameron DE, De Backer J, Hellemans J, Chen Y, Davis EC, Webb CL, Kress W, Coucke P, Rifkin DB, De Paepe AM, Dietz HC (2005) A syndrome of altered cardiovascular, craniofacial, neurocognitive and skeletal development caused by mutations in TGFBR1 or TGFBR2. Nat Genet 37:275–281
Rizzo RJ, McCarthy WJ, Dixit SN, Lilly MP, Shively VP, Flinn WR, Yao JS (1989) Collagen types and matrix protein content in human abdominal aortic aneurysms. J Vasc Surg 10:365–373
Buth J, Harris P (2005) Endovascular treatment of aortic aneurysms. In: Rutherford RB (ed) Vascular surgery. Elsevier, Philadelphia, pp 1452–1475
Sangiorgi G, D’Averio R, Mauriello A, Bondio M, Pontillo M, Castelvecchio S, Trimarchi S, Tolva V, Nano G, Rampoldi V, Spagnoli LG, Inglese L (2001) Plasma levels of metalloproteinases-3 and -9 as markers of successful abdominal aortic aneurysm exclusion after endovascular graft treatment. Circulation 104:I288–295
Tung WS, Lee JK, Thompson RW (2001) Simultaneous analysis of 1176 gene products in normal human aorta and abdominal aortic aneurysms using a membrane-based complementary DNA expression array. J Vasc Surg 34:143–150
Yajima N, Masuda M, Miyazaki M, Nakajima N, Chien S, Shyy JY (2002) Oxidative stress is involved in the development of experimental abdominal aortic aneurysm: a study of the transcription profile with complementary DNA microarray. J Vasc Surg 36:379–385
Absi TS, Sundt TM 3rd, Tung WS, Moon M, Lee JK, Damiano RR Jr, Thompson RW (2003) Altered patterns of gene expression distinguishing ascending aortic aneurysms from abdominal aortic aneurysms: complementary DNA expression profiling in the molecular characterization of aortic disease. J Thorac Cardiovasc Surg 126:344–357; discussion 357
Gum R, Wang H, Lengyel E, Juarez J, Boyd D (1997) Regulation of 92 kDa type IV collagenase expression by the jun aminoterminal kinase- and the extracellular signal-regulated kinase-dependent signaling cascades. Oncogene 14:1481–1493
Lakka SS, Jasti SL, Kyritsis AP, Yung WK, Ali-Osman F, Nicolson GL, Rao JS (2000) Regulation of MMP-9 (type IV collagenase) production and invasiveness in gliomas by the extracellular signal-regulated kinase and jun amino-terminal kinase signaling cascades. Clin Exp Metastasis 18:245–252
Shin M, Yan C, Boyd D (2002) An inhibitor of c-jun aminoterminal kinase (SP600125) represses c-Jun activation, DNA-binding and PMA-inducible 92-kDa type IV collagenase expression. Biochim Biophys Acta 1589:311–316
Wu C, Hsieh HL, Jou MJ, Yang CM (2004) Involvement of p42/p44 MAPK, p38 MAPK, JNK and nuclear factor-kappa B in interleukin-1beta-induced matrix metalloproteinase-9 expression in rat brain astrocytes. J Neurochem 90:1477–1488
Ip YT, Davis RJ (1998) Signal transduction by the c-Jun N-terminal kinase (JNK)-from inflammation to development. Curr Opin Cell Biol 10:205–219
Manning AM, Davis RJ (2003) Targeting JNK for therapeutic benefit: from junk to gold? Nat Rev Drug Discov 2:554–565
Daugherty A, Manning MW, Cassis LA (2000) Angiotensin II promotes atherosclerotic lesions and aneurysms in apolipoprotein E-deficient mice. J Clin Invest 105:1605–1612
Sato H, Seiki M (1993) Regulatory mechanism of 92 kDa type IV collagenase gene expression which is associated with invasiveness of tumor cells. Oncogene 8:395–405
Xiao W, Hodge DR, Wang L, Yang X, Zhang X, Farrar WL (2004) NF-kappaB activates IL-6 expression through cooperation with c-Jun and IL6-AP1 site, but is independent of its IL6-NFkappaB regulatory site in autocrine human multiple myeloma cells. Cancer Biol Ther 3:1007–1017
Wolf JS, Chen Z, Dong G, Sunwoo JB, Bancroft CC, Capo DE, Yeh NT, Mukaida N, Van Waes C (2001) IL (interleukin)-1alpha promotes nuclear factor-kappaB and AP-1-induced IL-8 expression, cell survival, and proliferation in head and neck squamous cell carcinomas. Clin Cancer Res 7:1812–1820
Papa S, Zazzeroni F, Pham CG, Bubici C, Franzoso G (2004) Linking JNK signaling to NF-kappaB: a key to survival. J Cell Sci 117:5197–5208
Schuringa JJ, Timmer H, Luttickhuizen D, Vellenga E, Kruijer W (2001) c-Jun and c-Fos cooperate with STAT3 in IL-6-induced transactivation of the IL-6 respone element (IRE). Cytokine 14:78–87
Leu JI, Crissey MA, Leu JP, Ciliberto G, Taub R (2001) Interleukin-6-induced STAT3 and AP-1 amplify hepatocyte nuclear factor 1-mediated transactivation of hepatic genes, an adaptive response to liver injury. Mol Cell Biol 21:414–424
Jovanovic DV, Martel-Pelletier J, Di Battista JA, Mineau F, Jolicoeur FC, Benderdour M, Pelletier JP (2000) Stimulation of 92-kd gelatinase (matrix metalloproteinase 9) production by interleukin-17 in human monocyte/macrophages: a possible role in rheumatoid arthritis. Arthritis Rheum 43:1134–1144
Huang C, Rajfur Z, Borchers C, Schaller MD, Jacobson K (2003) JNK phosphorylates paxillin and regulates cell migration. Nature 424:219–223
Aoki H, Kang PM, Hampe J, Yoshimura K, Noma T, Matsuzaki M, Izumo S (2002) Direct activation of mitochondrial apoptosis machinery by c-Jun N-terminal kinase in adult cardiac myocytes. J Biol Chem 277:10244–10250
Tournier C, Hess P, Yang DD, Xu J, Turner TK, Nimnual A, Bar-Sagi D, Jones SN, Flavell RA, Davis RJ (2000) Requirement of JNK for stress-induced activation of the cytochrome c-mediated death pathway. Science 288:870–874
Dong C, Yang DD, Wysk M, Whitmarsh AJ, Davis RJ, Flavell RA (1998) Defective T cell differentiation in the absence of Jnk1. Science 282:2092–2095
Yang DD, Conze D, Whitmarsh AJ, Barrett T, Davis RJ, Rincon M, Flavell RA (1998) Differentiation of CD4+ T cells to Th1 cells requires MAP kinase JNK2. Immunity 9:575–585
Xiong W, Zhao Y, Prall A, Greiner TC, Baxter BT (2004) Key roles of CD4+ T cells and IFN-gamma in the development of abdominal aortic aneurysms in a murine model. J Immunol 172:2607–2612
Ricci R, Sumara G, Sumara I, Rozenberg I, Kurrer M, Akhmedov A, Hersberger M, Eriksson U, Eberli FR, Becher B, Boren J, Chen M, Cybulsky MI, Moore KJ, Freeman MW, Wagner EF, Matter CM, Luscher TF (2004) Requirement of JNK2 for scavenger receptor A-mediated foam cell formation in atherogenesis. Science 306:1558–1561
Sho E, Chu J, Sho M, Fernandes B, Judd D, Ganesan P, Kimura H, Dalman RL (2004) Continuous periaortic infusion improves doxycycline efficacy in experimental aortic aneurysms. J Vasc Surg 39:1312–1321
Camici GG, Steffel J, Akhmedov A, Schafer N, Baldinger J, Schulz U, Shojaati K, Matter CM, Yang Z, Luscher TF, Tanner FC (2006) Dimethyl sulfoxide inhibits tissue factor expression, thrombus formation, and vascular smooth muscle cell activation: a potential treatment strategy for drug-eluting stents. Circulation 114:1512–1521
Kazi M, Thyberg J, Religa P, Roy J, Eriksson P, Hedin U, Swedenborg J (2003) Influence of intraluminal thrombus on structural and cellular composition of abdominal aortic aneurysm wall. J Vasc Surg 38:1283–1292
Satta J, Laara E, Juvonen T (1996) Intraluminal thrombus predicts rupture of an abdominal aortic aneurysm. J Vasc Surg 23:737–739
Stenbaek J, Kalin B, Swedenborg J (2000) Growth of thrombus may be a better predictor of rupture than diameter in patients with abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 20:466–469
Fontaine V, Jacob MP, Houard X, Rossignol P, Plissonnier D, Angles-Cano E, Michel JB (2002) Involvement of the mural thrombus as a site of protease release and activation in human aortic aneurysms. Am J Pathol 161:1701–1710
Yan L, Borregaard N, Kjeldsen L, Moses MA (2001) The high molecular weight urinary matrix metalloproteinase (MMP) activity is a complex of gelatinase B/MMP-9 and neutrophil gelatinase-associated lipocalin (NGAL). Modulation of MMP-9 activity by NGAL. J Biol Chem 276:37258–37265
Acknowledgments
We would like to thank our collaborators. We regret that many excellent studies related to this topic could not be mentioned because of space limitations. This work was supported by: Grant-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Science (HA, KY, and MM), Japan Heart Foundation/Zeria Pharmaceutical Grant for Research on Cardiovascular Disease (HA), a New Frontier Project from Yamaguchi University (HA and KY), a grant from the Takeda Science Foundation (HA), and a grant from the Sankyo Company to the Department of Molecular Cardiovascular Biology, Yamaguchi University School of Medicine.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aoki, H., Yoshimura, K. & Matsuzaki, M. Turning back the clock: regression of abdominal aortic aneurysms via pharmacotherapy. J Mol Med 85, 1077–1088 (2007). https://doi.org/10.1007/s00109-007-0213-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-007-0213-2