Abstract
Background
The optimal treatment strategy for stage I–II glottic squamous cell carcinoma (SCC) is not well-defined. This study analyzed treatment results and prognostic factors.
Patients and methods
This is a single-institution retrospective analysis of 244 patients with T1–2 glottic SCC who underwent normofractionated radiotherapy (RT) and/or surgery between 1990 and 2013. The primary endpoint was relapse-free survival (RFS).
Results
Median age was 65 years (range: 36–92 years), the majority (82%) having stage I disease. Definitive RT was used in 82% (median dose: 68 Gy, 2 Gy per fraction). Median follow-up was 59 months. The 5‑year RFS rates were 83 and 75% (p = 0.05) for stage I and 62 and 50% (p = 0.47) for stage II in the RT and surgery groups, respectively. Multivariate analyses indicate T1 vs. T2 and RT vs. surgery as independent prognostic factors for RFS, with hazard ratios of 0.38 (95% confidence interval, CI: 0.21–0.72) and 0.53 (95% CI: 0.30–0.99), respectively (p < 0.05). The 5‑year overall and cause-specific survival rates in the whole cohort were 92 and 96%, respectively, with no significant differences between treatment groups. Anterior commissure involvement was neither a prognostic nor a predictive factor. The incidence of secondary malignancies was not significantly different between patients treated with and without RT (22 vs. 9% at 10 years, respectively, p = 0.18).
Conclusion
Despite a possible selection bias, our series demonstrates improved RFS with RT over surgery in stage I glottic SCC.
Zusammenfassung
Hintergrund
Die optimale Behandlungsstrategie für ein Plattenepithelkarzinom (SCC) der Stimmbänder im Stadium I–II ist nicht gut definiert. In dieser Studie wurden Behandlungsergebnisse und prognostische Faktoren untersucht.
Patienten und Methoden
In dieser retrospektiv unizentrischen Studie wurden 244 Patienten mit einem frühen Glottis-SCC (T1–2) zwischen 1990 und 2013 strahlentherapeutisch (RT) und/oder chirurgisch behandelt. Primärer Endpunkt war das rezidivfreie Überleben (RFS).
Ergebnisse
Das mediane Alter betrug 65 Jahre (Spanne 36–92). Die Mehrheit (82 %) hatte ein Stadium I. Die mediane Tumornachsorge betrug 59 Monate. Von den Patienten wurden 82% bestrahlt, die Übrigen wurden operiert. Die mediane RT-Dosis war 68 Gy (2 Gy/Fraktion). Für die radiotherapeutisch und chirurgisch behandelten Gruppen betrug das 5‑Jahres-RFS 83 bzw. 75 % mit einem Stadium I (p = 0,05) und 62 bzw. 50 % mit einem Stadium II (p = 0,47). Die multivariaten Analysen zeigen T1- vs. T2-Karzinome und RT vs. Chirurgie als unabhängige prognostische Faktoren für das RFS, mit Hazard Ratios von jeweils 0,38 (95 %-Konfidenzintervall [KI] 0,21–0,72) und 0,53 (95 %-KI 0,30–0,99; p < 0,05). Die 5‑Jahres-Gesamt- und krankheitsspezifische Überlebensrate der ganzen Studienpopulation betrugen 92 % und 96 %, ohne signifikanten Unterschied zwischen beiden Therapiestrategien. Die Infiltration der vorderen Kommissur war weder prognostisch noch prädiktiv. Bezüglich der Inzidenz von Zweitmalignomen bei Patienten mit und ohne RT konnten keine signifikanten Unterschiede gefunden werden (22 vs. 9 % nach 10 Jahren; p = 0,18).
Schlussfolgerung
Trotz einer möglichen Stichprobenverzerrung zeigen unsere Daten eine im Vergleich zur Chirurgie bessere RFS bei bestrahltem Stadium-I-Glottis-SCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
About 50–60% of laryngeal squamous cell carcinomas (SCC) arise from the glottic region [1] and over 80% of these patients present in an early stage [2]. The larynx has important roles in production of voice, coordination of deglutition, and respiration. Therefore, the treatment aim of laryngeal cancer is not only achievement of maximum disease control, but also maintenance of function. In the absence of large randomized studies providing clear evidence for the best strategy to treat early stage glottic SCC, many retrospective studies reported comparable control rates following radiotherapy (RT) and/or surgery. The 5‑year local control rate (LC) following RT ranges from 80 to 95% for T1 and from 61 to 82% for T2 glottic SCC [3, 4]. The 5‑year LC with transoral laser microsurgery is in the order of 82 to 100% for T1 and 66 to 88% for T2 tumors, which is comparable to the results of open partial laryngectomy [5,6,7]. For these early stages, 5‑year overall and disease-free survival rates are in the range of 89–100% and 60–100%, respectively. In this regard, no significant differences between surgery and RT are expected [8].
The aim of this retrospective single-institution study was to assess the oncologic outcome and influencing factors in treatment of stage I and II (Union for International Cancer Control, UICC) glottic SCC with a sufficient follow-up period.
Patients and methods
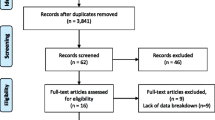
Approval of institutional and regional review boards was obtained. The charts of all patients presented in our Head and Neck Cancer multidisciplinary tumor board between 1990 and 2013 with histologically proven T1 and T2 invasive purely glottic SCC were reviewed. Staging was revised according to the 7th edition of the UICC staging system. Patients with preexisting neoplastic disease were excluded. Treatment decisions were discussed by board members to determine the best strategy to preserve laryngeal function in the absence of a protocol with any predefined selection criteria. The patients either received definitive RT alone or underwent surgery.
Radiotherapy was delivered using a two-dimensional conventional or three-dimensional conformal technique (2D/3D-RT) in the majority of the cases, which was followed by an era of intensity-modulated radiotherapy (IMRT). No bolus was used. Treatment was planned with 6‑MV photons. Definitive RT to a total dose of 72 Gy was delivered in 2 Gy per fraction to the larynx in T2 tumors. The remaining cases (T1 definitive or T1/2 adjuvant) were treated to 68 Gy. Target volume encompassed the whole larynx. Elective neck irradiation encompassing levels II–IV bilaterally with a dose of 54 Gy was performed for T2 primaries treated with definitive RT. Surgery involved transoral laser microsurgery or open partial laryngectomy. Adjuvant RT was indicated in cases of close or positive resection margins.
All patients underwent regular follow-up for at least 5 years after treatment including physical examination with flexible transnasal endoscopy. There was no standard for regular imaging studies.
All time-to-event intervals were calculated based on the date of initial positive biopsy. The follow-up time was not censored at a given time point. A two-sided log-rank test was used to evaluate possible prognostic factors such as age, gender, stage, anterior commissure involvement (ACI), RT treatment time, and treatment modality for relapse-free survival (RFS). Variables with p-values ≤0.05 in univariate analyses were used to build multivariate models to identify possible independent risk factors through backwards elimination. Statistical analyses were performed with JMP (version 12.1; SAS Institute, Cary, NC, USA).
Results
A total of 244 patients with a median age of 65 years (range 36–92 years) were diagnosed with stage I–II SCC of the glottic larynx. The median follow-up was 59 months. Primary treatments included either definitive RT (82%) or surgery (18%). Surgery was received by 16 patients, followed by adjuvant RT (37% of the cohort with primary surgery). The majority (85%) were treated with 2D/3D-RT rather than IMRT techniques. Median treatment time was 49 days (range 38–56 days) without any statistically significant impact on outcome parameters. Table 1 summarizes the patient, disease, and treatment characteristics.
The 5‑year overall survival (OS), cause-specific survival (CSS), and RFS rates for the whole cohort were 92, 96, and 78%, respectively. Compared to T1, T2 tumors relapsed more frequently (39 vs. 19%) at 5 years, p < 0.01 (Fig. 1a). With definitive RT vs. surgery, 5‑year RFS rates were 79 and 73%, respectively (p = 0.09; Fig. 1b). Among primary treatment modalities, OS rates at 2, 5, and 10 years were 98, 91, and 84% with RT; 100, 97, and 90% with surgery, respectively (p = 0.10).
The 5‑year RFS was higher for patients who received RT as any part of their treatment (either definitive or adjuvant) than for those who underwent surgery alone (80 vs. 65%; p < 0.01; Fig. 2a). In patients with T1 primaries, the 5‑year RFS rates with primary RT vs. surgery were 83 and 75%, respectively (p = 0.05; Fig. 2b). This difference was not statistically significant in T2 cases (62 vs. 50%; p = 0.47). The 5‑year CSS rates of patients with T1 and T2 were 98 vs. 88%, respectively (p < 0.01; Fig. 3).
For RFS, ACI was neither prognostic nor predictive when comparing RT to surgery and IMRT to non-IMRT. Multivariate analysis indicated stage and treatment modality as independent prognostic variables for RFS with hazard ratios (HR) of 0.38 (95% confidence interval, CI: 0.21–0.72) for T1 vs. T2 and 0.53 (95% CI: 0.30–0.99) for RT vs. surgery (both p < 0.05). Detailed results of the univariate and multivariate analyses are provided in Table 2.
We observed a median time to relapse of 25 months. The majority of relapses occurred locally. The 2‑ and 5‑year RFS rates after salvage treatment were 75 and 65%, respectively. The patterns of relapse and subsequent treatments are shown in Table 3.
A second primary cancer developed in 30 patients (12%), of which 10 were diagnosed as head and neck cancer (HNC), all being SCC, and 22 as non-HNC (two patients had both). Localizations are provided in the supplementary table. The incidence rates of second malignancies showed an increase in patients with vs. without definitive or adjuvant RT, but without statistical significance (Fig. 4).
Among patients who did not experience any relapse; 1 needed a permanent feeding tube and 2 had tracheotomy due to laryngeal stenosis at last follow-up; 2 further patients had both. No patient suffered from aspiration or underwent a functional laryngectomy. The laryngectomy rates among survivors at 2, 5, and 10 years were 5, 8, and 14% in stage I; 17, 28, and 32% in stage II, respectively (p < 0.01). All laryngectomies were performed as salvage surgery and not due to functional deterioration.
Discussion
The main objective of this study was to report the outcome of stage I–II glottic SCC patients treated by our multidisciplinary HNC team and to identify possible factors which may influence the outcome. Through the analyses, two prognostic factors emerged. First, stage as a well-known prognostic factor [9]; and second, treatment modality. To our knowledge, there are no prospective randomized trials providing a proper comparison of RT and surgery of early glottic SCC in terms of oncologic or functional outcome. In 1990, a multicenter randomized controlled trial was published [10] which compared the outcomes of open surgery, RT, or chemoradiotherapy in early glottic SCC. The available English abstract draws concerns about trial design and methodology. Another prospective randomized study comparing laser microsurgery vs. normofractionated RT for the treatment of T1a glottic SCC was published by Aaltonen et al. [11], where the primary endpoint was voice quality. The trial was stopped after 10 years due to low accrual, with only 20% of the planned sample size reached. Recurrence rates were comparable, but repeated-measure analyses demonstrated statistically significant improvements in voice quality with RT in assessments of breathiness, asthenia, glottal closure (expert-rated), and impact on everyday life (patient-rated).
In the absence of prospective randomized trials, a variety of meta-analyses and systematic reviews were published comparing RT to surgery with various methodologies and findings. In a meta-analysis including 27 studies comparing RT to laser microsurgery, no significant difference in oncologic outcome, but a trend toward improved voice quality following RT was reported [12]. Similarly, another systematic review and meta-analysis included 19 studies with T1a glottic larynx cancer showed no significant differences in LC, OS, disease-specific survival, or voice quality following RT or surgery [13]. A recent extensive systematic review reported similar oncologic outcomes for stage I patients who received RT or underwent surgery with or without laser [14]. Hai-Lan et al. showed in a meta-analysis that laser surgery delivered significantly better OS and laryngeal preservation than RT in T1 primaries, without, however, significant differences in LC in T1 tumors, which puts a question mark on the quality of the analysis concerning patient selection bias [15]. Similarly, a recent Surveillance, Epidemiology, and End Results (SEER) data analysis showed superior OS with surgery over RT without reporting any LC or disease-specific outcome rates [16]. A recent systematic review of LC outcomes explicitly for T2 glottic tumors treated with either RT or laser surgery didn’t show any difference in 5‑year LC between the two treatment groups [17]. The last update of the Cochrane review on this topic showed no significant differences in 5‑year OS or disease-free survival in stage I and II glottic SCC with RT or surgery [8]. The authors emphasized the lack of consistent and high-level evidence needed to draw any conclusions. In our cohort, RFS was higher in T1 patients treated with RT than those who underwent surgery. However, our cohort is subject to selection bias due to its retrospective nature. First of all, there is a clear imbalance between the numbers of patients treated with primary RT and surgery. A concerning number (around one third) of the surgically treated patients underwent adjuvant RT instead of re-resection. Additionally, our recurrence rates are higher than those reported in the literature. This may be explained by our previous institutional policy apparently favoring RT over surgery in early-stage laryngeal cancer, not only as the first treatment option but also in cases of close and positive resection margins, which underwent a major change few years ago.
Altered fractionation with shorter overall treatment times corresponds to better tumor control and survival benefit in HNC [18,19,20,21,22,23]. During the last decade, two prospective randomized trials answered this fractionation question specifically in early-stage glottic SCC [24, 25], favoring hypofractionation (2.25 Gy). On the other hand, contrary to what was expected, Radiation Therapy Oncology Group (RTOG) 9512 showed increased toxicity and futility with hyperfractionation in T2 glottic larynx cancer [26]. Using accelerated RT, the results of the DAHANCA 6 trial showed a significant improvement in locoregional control of glottic SCC with a HR of 0.60 (CI: 0.41–0.89) with a median follow-up of 14.5 years. There were no significant differences in long-term toxicity among accelerated RT and normofractionation [27]. In our cohort, this observation could not be reproduced, probably due to the fact that the majority of the patients were treated once daily and RT time was normally distributed, with a prominent accumulation around the median value of 49 days. The outliers were patients whose treatments were either arbitrarily accelerated or delayed for various reasons.
In our series, all patients in stage II received elective nodal irradiation to the levels II–IV bilaterally. However, recently published large series showed the futility of this practice [3, 27]. Some retrospective studies demonstrated that ACI is a poor prognostic factor for RT outcomes [28,29,30,31,32], but these results are not consistent in the literature [7]. Some authors pointed out the possible underdosage of tumors with ACI close to the skin caused by the air–tissue interface [33]. In our series, we did not observe a prognostic impact of ACI, regardless of technique. However, patients treated with IMRT represented only 15% of our whole cohort.
While IMRT is known to be used for its general benefits in terms of decreasing toxicity in the treatment of laryngeal cancer [34], the still widely used approach for early-stage glottis SCC is to treat the whole larynx as a compartment. This approach is based on the traditional conventional field design, which was established in an era where image guidance in RT was poor. Another reason was the laryngeal displacement due to swallowing during RT, which was later reported not to be a serious concern [35, 36]. This approach has two major consequences. First, it exposes an unnecessary volume of healthy tissue to a high dose (i. e., overtreatment), which may increase the risk of functional loss through inflammation and fibrosis, at the same time depleting the reserves for future re-irradiation, if required. Second, the carotid arteries are exposed to a high dose, which increases the incidence of stenosis and cerebrovascular events [37, 38]. Chera et al. [39] overcame this problem through modified target volumes and IMRT. With a newer technique developed by the Rotterdam group, it is possible to apply 58.08 Gy in 16 fractions just to the involved vocal cord, with a significant dose reduction in the vicinity [40]. Recently, this group reported the clinical results of a prospective study with the primary endpoint of voice quality [41]. With a median follow-up of 30 months, 2‑year LC and OS were 100 and 90%, respectively, without any grade ≥3 toxicity. When compared with a historical cohort treated to the whole larynx (66/2 Gy), single vocal cord irradiation yielded less grade ≥2 acute toxicity (17 vs. 66%, p < 0.01) and lower Voice Handicap Index scores in all follow-up visits performed in regular short intervals until the 18th month (p < 0.01).
High second malignancy rates in HNC patients is a major problem. With each passing year, about 3% of the treated early-stage head and neck SCC (HNSCC) patients are expected to develop a second primary malignancy [42, 43]. In the SEER database analysis (n = 27,985) published by Rusthoven et al. [44], a reduced incidence of secondary HNC was observed in patients treated with vs. without RT (HR 0.71, p < 0.01). The difference was still significant in the laryngeal subsite on multivariate analysis. The authors suggested that RT had a preventive effect on transformation of the subclinical malignant foci. This observation is consistent with results of another analysis of 987 laryngeal cancer patients treated between 1967 and 2004, where RT was not found to increase the risk of second primary tumor incidence [45]. In our study, 12% of patients developed a second primary cancer with a non-significant increase in patients treated definitively or adjuvantly with RT (RT 22%; surgery only 9%). However, our median follow-up of 5 years is not enough to observe any meaningful difference or exclude the long-term possibility of an increased incidence of second malignancies in any of the treatment groups. Furthermore, the hypothesis regarding ablation of the premalignant foci with RT may be invalid or less prominent in the IMRT era, and if still present, this effect might be limited in the treatment of early glottic SCC, where elective nodal irradiation is often omitted.
Our present study has limitations due to its retrospective nature, which predisposes the results to potential bias. It represents two imbalanced treatment groups, therefore limiting the robustness of comparisons (RT vs. surgery). Additionally, due to its retrospective nature, we were not able to report on toxicities, smoking and alcohol consumption status.
Conclusion
Our series demonstrate a better RFS with RT compared surgery for stage I glottic SCC with a given risk of possible selection bias. The lack of level 1 evidence comparing these treatment modalities compels careful interpretation of our results.
References
Mastronikolis N, Papadas T, Goumas P et al (2011) Head and neck: laryngeal tumors: an overview. Atlas Genet Cytogenet Oncol Haematol 13(11):888–893
Lyhne NM, Johansen J, Kristensen CA et al (2016) Pattern of failure in 5001 patients treated for glottic squamous cell carcinoma with curative intent – a population based study from the DAHANCA group. Radiother Oncol 118(2):257–266
Chera BS, Amdur RJ, Morris CG, Kirwan JM, Mendenhall WM (2010) T1N0 to T2N0 squamous cell carcinoma of the glottic larynx treated with definitive radiotherapy. Int J Radiat Oncol Biol Phys 78(2):461–466
Ermiş E, Teo M, Dyker KE, Fosker C, Sen M, Prestwich RJ (2015) Definitive hypofractionated radiotherapy for early glottic carcinoma: experience of 55 Gy in 20 fractions. Radiat Oncol 10(1):203
Mendenhall WM, Werning JW, Hinerman RW, Amdur RJ, Villaret DB (2004) Management of T1–T2 glottic carcinomas. Cancer 100(9):1786–1792
Ambrosch P (2007) The role of laser microsurgery in the treatment of laryngeal cancer. Curr Opin Otolaryngol Head Neck Surg 15(2):82–88
Hartl DM, Ferlito A, Brasnu DF et al (2011) Evidence-based review of treatment options for patients with glottic cancer. Head Neck 33(11):1638–1648
Warner L, Chudasama J, Kelly CG et al (2014) Radiotherapy versus open surgery versus endolaryngeal surgery (with or without laser) for early laryngeal squamous cell cancer. Cochrane Database Syst Rev 12(12):CD002027. doi:10.1002/14651858.cd002027
Chen JJ, Stessin A, Christos P, Wernicke AG, Nori D, Parashar B (2015) Differences in survival outcome between stage I and stage II glottic cancer: a SEER-based analysis. Laryngoscope 125(9):2093–2098
Ogol’tsova ES, Paches AI, Matiakin EG et al (1990) Comparative evaluation of the effectiveness of radiotherapy, surgery and combined treatment of stage I–II laryngeal cancer (T1–2NoMo) based on the data of a cooperative randomized study. Vestn Otorinolaringol 3:3–7
Aaltonen L‑M, Rautiainen N, Sellman J et al (2014) Voice quality after treatment of early vocal cord cancer: a randomized trial comparing laser surgery with radiation therapy. Int J Radiat Oncol Biol Phys 90(2):255–260
Higgins KM, Shah MD, Ogaick MJ, Enepekides D (2009) Treatment of early-stage glottic cancer: meta-analysis comparison of laser excision versus radiotherapy. J Otolaryngol Head Neck Surg 38(6):603–612
Abdurehim Y, Hua Z, Yasin Y, Xukurhan A, Imam I, Yuqin F (2012) Transoral laser surgery versus radiotherapy: systematic review and meta-analysis for treatment options of T1a glottic cancer. Head Neck 34(1):23–33
Yoo J, Lacchetti C, Hammond JA, Gilbert RW, Head and Neck Cancer Disease Site Group (2014) Role of endolaryngeal surgery (with or without laser) versus radiotherapy in the management of early (T1) glottic cancer: a systematic review. Head Neck 36(12):1807–1819
Mo H‑L, Li J, Yang X et al (2017) Transoral laser microsurgery versus radiotherapy for T1 glottic carcinoma: a systematic review and meta-analysis. Lasers Med Sci 32(2):461–467
Megwalu UC, Panossian H (2016) Survival outcomes in early stage laryngeal cancer. Anticancer Res 36(6):2903–2907
Warner L, Lee K, Homer JJ (2016) Transoral laser microsurgery versus radiotherapy for T2 glottic squamous cell carcinoma: a systematic review of local control outcomes. Clin Otolaryngol:. doi:10.1111/coa.12790
Le QT, Fu KK, Kroll S et al (1997) Influence of fraction size, total dose, and overall time on local control of T1–T2 glottic carcinoma. Int J Radiat Oncol Biol Phys 39(1):115–126
Overgaard J, Hansen HS, Specht L et al (2003) Five compared with six fractions per week of conventional radiotherapy of squamous-cell carcinoma of head and neck: DAHANCA 6 and 7 randomised controlled trial. Lancet 362(9388):933–940
Rosenthal DI, Ang KK (2004) Altered radiation therapy fractionation, chemoradiation, and patient selection for the treatment of head and neck squamous carcinoma. Semin Radiat Oncol 14(2):153–166
Bourhis J, Overgaard J, Audry H et al (2006) Hyperfractionated or accelerated radiotherapy in head and neck cancer: a meta-analysis. Lancet 368(9538):843–854
Sakata K, Someya M, Hori M, Nakata K, Takagi M, Hareyama M (2008) Hyperfractionated accelerated radiotherapy for T1,2 glottic carcinoma. Consideration of time-dose factors. Strahlenther Onkol 184(7):364–369
Becker-Schiebe M, Christiansen H (2014) Non-inferior moderate hypofractionated irradiation of glottis T1/T2 laryngeal cancer. Strahlenther Onkol 190(7):694–695
Yamazaki H, Nishiyama K, Tanaka E, Koizumi M, Chatani M (2006) Radiotherapy for early glottic carcinoma (T1N0M0): results of prospective randomized study of radiation fraction size and overall treatment time. Int J Radiat Oncol Biol Phys 64(1):77–82
Moon SH, Cho KH, Chung EJ et al (2013) A prospective randomized trial comparing hypofractionation with conventional fractionation radiotherapy for T1–2 glottic squamous cell carcinomas: results of a Korean Radiation Oncology Group (KROG-0201) study. Radiother Oncol 110(1):98–103
Trotti A, Zhang Q, Bentzen SM et al (2014) Randomized trial of hyperfractionation versus conventional fractionation in T2 squamous cell carcinoma of the vocal cord (RTOG 9512). Int J Radiat Oncol Biol Phys 89(5):958–963
Lyhne NM, Primdahl H, Kristensen CA et al (2015) The DAHANCA 6 randomized trial: effect of 6 vs 5 weekly fractions of radiotherapy in patients with glottic squamous cell carcinoma. Radiother Oncol 117(1):91–98. doi:10.1016/j.radonc.2015.07.004
Garden AS, Forster K, Wong PF, Morrison WH, Schechter NR, Ang KK (2003) Results of radiotherapy for T2N0 glottic carcinoma: Does the “2” stand for twice-daily treatment? Int J Radiat Oncol Biol Phys 55(2):322–328
Cellai E, Frata P, Magrini SM et al (2005) Radical radiotherapy for early glottic cancer: results in a series of 1087 patients from two Italian radiation oncology centers. I. The case of T1N0 disease. Int J Radiat Oncol Biol Phys 63(5):1378–1386
Laccourreye O, Muscatello L, Laccourreye L, Naudo P, Brasnu D, Weinstein G (1997) Supracricoid partial laryngectomy with cricohyoidoepiglottopexy for “early” glottic carcinoma classified as T1-T2N0 invading the anterior commissure. Am J Otolaryngol 18(6):385–390
Marshak GG, Brenner B, Shvero J et al (1999) Prognostic factors for local control of early glottic cancer: rhe Rabin Medical Center retrospective study on 207 patients. Int J Radiat Oncol Biol Phys 43(5):1009–1013
Smee RI, Meagher NS, Williams JR, Broadley K, Bridger GP (2010) Role of radiotherapy in early glottic carcinoma. Head Neck 32(7):850–859
Tong C‑C, Au K‑H, Ngan RKC et al (2011) Impact and relationship of anterior commissure and time-dose factor on the local control of T1N0 glottic cancer treated by 6 MV photons. Radiat Oncol 6(1):53
Modesto A, Laprie A, Vieillevigne L et al (2015) Intensity-modulated radiotherapy for laryngeal and hypopharyngeal cancer: minimization of late dysphagia without jeopardizing tumor control. Strahlenther Onkol 191(3):225–233
van Asselen B, Raaijmakers CPJ, Lagendijk JJW, Terhaard CHJ (2003) Intrafraction motions of the larynx during radiotherapy. Int J Radiat Oncol Biol Phys 56(2):384–390
Bradley JA, Paulson ES, Ahunbay E, Schultz C, Li XA, Wang D (2011) Dynamic MRI analysis of tumor and organ motion during rest and deglutition and margin assessment for radiotherapy of head-and-neck cancer. Int J Radiat Oncol Biol Phys 81(5):e803–12
Dorresteijn LDA, Kappelle AC, Boogerd W et al (2002) Increased risk of ischemic stroke after radiotherapy on the neck in patients younger than 60 years. J Clin Oncol 20(1):282–288
Smith GL, Smith BD, Buchholz TA et al (2008) Cerebrovascular disease risk in older head and neck cancer patients after radiotherapy. J Clin Oncol 26(31):5119–5125
Chera BS, Amdur RJ, Morris CG, Mendenhall WM (2010) Carotid-sparing intensity-modulated radiotherapy for early-stage squamous cell carcinoma of the true vocal cord. Int J Radiat Oncol Biol Phys 77(5):1380–1385
Kwa SLS, Al-Mamgani A, Osman SOS, Gangsaas A, Levendag PC, Heijmen BJM (2015) Inter- and Intrafraction target motion in highly focused single vocal cord irradiation of T1a larynx cancer patients. Int J Radiat Oncol Biol Phys 93(1):190–195
Al-Mamgani A, Kwa SLS, Tans L et al (2015) Single vocal cord irradiation: image guided intensity modulated hypofractionated radiation therapy for T1a glottic cancer: early clinical results. Int J Radiat Oncol Biol Phys 93(2):337–343
Yamamoto E, Shibuya H, Yoshimura R, Miura M (2002) Site specific dependency of second primary cancer in early stage head and neck squamous cell carcinoma. Cancer 94(7):2007–2014
Cooper JS, Pajak TF, Rubin P et al (1989) Second malignancies in patients who have head and neck cancer: incidence, effect on survival and implications based on the RTOG experience. Int J Radiat Oncol Biol Phys 17(3):449–456
Rusthoven K, Chen C, Raben D, Kavanagh B (2008) Use of external beam radiotherapy is associated with reduced incidence of second primary head and neck cancer: a SEER database analysis. Int J Radiat Oncol Biol Phys 71(1):192–198
Farhadieh RD, Rees CGG, Yang JL, Salardini A, Russell P, Smee R (2009) Radiotherapy in larynx squamous cell carcinoma is not associated with an increased diagnosis of second primary tumours. Clin Oncol 21(4):315–319
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Shelan, L. Anschuetz, A.D. Schubert, B. Bojaxhiu, A. Dal Pra, F. Behrensmeier, D.M. Aebersold, R. Giger, and O. Elicin declare that they have no competing interests.
Additional information
Both first (M. Shelan and L. Anschuetz) and last (R. Giger and O. Elicin) authors contributed equally to this article.
Caption Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Shelan, M., Anschuetz, L., Schubert, A.D. et al. T1–2 glottic cancer treated with radiotherapy and/or surgery. Strahlenther Onkol 193, 995–1004 (2017). https://doi.org/10.1007/s00066-017-1139-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-017-1139-4