Abstract
Transoral laser microsurgery (TLM) and radiotherapy (RT) are both accepted treatment modalities for glottic cancer. The objective of the study was to assess the oncologic outcomes and life quality of TLM in comparison with RT for T1 glottic carcinoma. We searched Medline/PubMed, Web of knowledge, EMBASE, the Cochrane Library, the Wiley online library, Springer, Google, China National Knowledge Infrastructure (CNKI), etc. We screened the literature, assessed the quality of the studies, and extracted the relevant data through the establishment of inclusion and exclusion criteria. Meta-analysis was done using the Cochrane collaboration’ s RevMan 5.0 for data analysis. A total of 11 studies were included in this meta-analysis. The laryngeal preservation for patients undergoing TLM was significantly better than that for RT (P < 0.00). The laser surgery significantly improved the overall survival of patients with T1 glottic carcinoma (P = 0.04). No statistically significant differences were found between TLM and RT regarding the local control (P = 0.91). The funnel plot demonstrates no apparent publication bias in the overall survival and laryngeal preservation comparison. Our meta-analysis suggested that laser surgery was a preferred method than radiotherapy with respect to significantly better overall survival and laryngeal preservation. But the local control was not significant different. Further prospective randomized controlled studies will be needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laryngeal cancer is the second most common type of head and neck malignancy worldwide, with estimated 151,000 new cases and 82,000 deaths annually in the word [1, 2]. Glottic carcinomas represent the majority of laryngeal cancer cases, which is mainly confined to the anterior portion of the vocal cord [2]. Due to lack of lymphatic vessels in the glottic area and the early symptom of hoarseness, glottic tumors can usually be diagnosed at an early stage, and favorable outcomes can be achieved. Therefore, optimal management option should be applied to achieve better oncologic outcomes and lower incidence of complications [3]. It is generally assumed that transoral laser microsurgery (TLM) and radiotherapy (RT) are both accepted modalities of treatment for patients with T1 glottic carcinoma, but not with equal results [4]. Decision-making has become complex, mainly depending on the clinical characteristics, patients, and physician preference, as well as institutional preference [5, 6]. However, no internationally accepted standard on the preferred treatment is available, and to our knowledge, no randomized trial exists to aid decision-making.
Since TLM was introduced to treat malignant lesions of the larynx in 1972 [7], a large number of ear nose throat (ENT) doctors compared it with RT. However, the oncologic outcome of transoral laser microsurgery (TLM) and radiotherapy (RT) for T1 glottic cancers is still a subject of controversy in literature. To date, no prospective randomized controlled study has been conducted to compare the effectiveness of TLM with that of radiotherapy (RT) [5]. Although nonrandomized studies have numerous flaws, such as the selection bias, the nonstandard therapies, and different types of staging, they are quite important because they provide the only available basis for treatment decision-making [4]. Thus, the purposes of this study were to systematically review the literature using a meta-analysis, and to analyze the oncologic results of patients undergoing TLM compared to those of patients receiving RT. The primary endpoints of this study included local control rate, overall survival rate, and laryngeal preservation rate.
Methods
Literature search strategy
Medline/PubMed, Web of Knowledge, EMBASE, Cochrane Library, Wiley online library, Springer, NCBI, and Google were searched for relevant articles through January 2012. The full texts or abstracts for all potentially relevant trials were obtained. The search was designed using the following terms: early glottic carcinoma, laryngeal cancer/tumor, laryngeal squamous cell carcinoma, transoral laser microsurgery (TLM), laser surgery, and radiotherapy (RT).
Inclusion and exclusion criteria
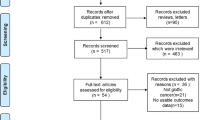
In this review, 11 comparative cohort studies published from April 1990 to January 2012 were assessed (Fig. 1). The titles and abstracts were screened for the following inclusion criteria: (1) patients with previously untreated T1N0M0 glottic carcinoma; (2) comparative studies that took TLM or RT as the first treatment for T1 glottic carcinoma; (3) one or more oncologic outcomes including the local control rate, the overall survival rate, and the laryngeal preservation rate should included. Exclusion criteria are as follows: (1) studies reporting on laryngeal cancer in general without specifying the location of the tumor; (2) studies reporting only on functional results; (3) studies with incomplete data or similar data of the outcome; and (4) single-arm studies that reported only one of the two therapy methods.
Data extraction
Studies were carefully searched independently by two investigators (Mo Hai-Lan and Jie Li) according to the inclusion and exclusion criteria. Information that revealed authors and their affiliations was then blinded before assessing the methodological quality and eligibility for inclusion criteria in this review. The full texts of eligible studies were obtained, and for each study, the following data were recorded: (1) publication information, first authors, and their affiliations; (2) patient and tumor characteristics; (3) media follow-up time (month), and (4) treatment and outcome measures as described earlier.
Study quality
The methodological quality of the articles and eligibility for inclusion were graded based on standards by Wasserman et al. [8] in otolaryngology journals. According to the established standards, the levels of evidence were scored as follows: level I: randomized controlled trials; level II: prospective study with internal control group; level III: retrospective study with internal control group; level IV: case series without an internal control group; and level V: consensus or expert opinion without critical appraisal. Besides, the clarity and completeness of the information were evaluated, including baseline characteristics, diagnosis and treatment staging standards, and the reliability of the treatment outcomes.
Statistical analysis
Meta-analysis was performed by pooling the oncologic outcomes of patients undergoing both treatments. All statistic analysis was carried out using the statistical package (RevMan 5.0) by the Cochrane collaboration. Significant heterogeneities between studies were examined using the chi-square statistic and I square (I 2) test. Due to the small number of studies in some strata, significance was set at P < 0.10 for the I 2 test. I-squared value of less than 25 % is considered low heterogeneity, 25–50 % moderate heterogeneity, and more than 50 % high heterogeneity [9]. When statistically significant heterogeneity was confirmed (P < 0.10), a random effect model was used to combine the results. Otherwise, in the absence of statistically significant heterogeneity (P > 0.1), a fixed effect model was used. The overall effect was tested using z scores with significance set at P < 0.05. A pooled odds ratio (OR) with 95 % confidence interval (CI) was performed. A funnel plot was used to assess the potential publication bias.
Results
Retrieval result
Baseline characteristics of the respective studies are summarized in table 1. A total of 11 studies were included in this meta-analysis. One of the studies involved patients with T1/T2 glottic carcinoma, only the data of T1 were included in our study [11]. The majority of the studies had local control (LC), overall survival (OS), or laryngeal preservation (LP) as the primary outcomes. Characteristics and oncologic outcomes of these studies are summarized in Table 2. The TNM classification was staged by the Union Internationale Contre le Cancer (UICC), the American Joint Committee on Cancer (AJCC), or the commonly accepted staging systems.
According to the score method, none of the comparative studies were considered to be high quality (level I). Only two of the studies [14, 17] were prospective in design (level II), and the remaining were retrospective cohort studies (level III). Seven of the studies had addressed selection bias, including age, sex, anterior commissure involvement (AC), TNM staging, tumor depth, and follow-up time (shown in table 1). In some studies, the results were presented in the form of percentages of favorable subjects. We converted the percentages into event numbers so as to analyze the combined values of different studies. Follow-up periods among studies were inconsistent and dropouts were not considered.
Detailed results according to different managements
Local control
Of the 11 studies comparing transoral laser microsurgery (TLM) with radiotherapy (RT), two had not detailed local control rate, so only nine studies were included (shown in Fig. 2). The total patient population was 565 in the TLM group, and 673 in the RT group. There were very low heterogeneities among the nine retrospective cohort studies (chi2 = 8.47, P = 0.39, I 2 = 6 %), and the fixed effect model was then applied. The pooled OR for local control was 0.98 (95 % CI 0.7, 1.38). No statistically significant differences were found between TLM and RT regarding the local control (P = 0.91). The funnel plot demonstrates no apparent publication bias (data not shown).
Overall survival
Regarding overall survival, eight studies with 562 participants in the TLM group and 706 in the RT group were included. The chi2 and I 2 heterogeneity tests were assessed revealing no significant differences between the two treatments (chi2 = 1.95, P = 0.96, I 2 = 0 %), and a fixed effect model was used. The pooled analysis showed that laser surgery significantly improved the overall survival of patients with T1 glottic carcinoma (P = 0.04) (OR = 1.35; 95 % CI 1.02, 1.79) (Fig. 3). No significant publication bias was discovered using the funnel plot methods.
Laryngeal preservation
Ten of the included studies compared the laryngeal preservation between patients undergoing TLM and those undergoing RT. There were a total of 666 patients in the laser group and 786 patients in the radical group. The chi-square and I-squared analysis revealed low heterogeneity among studies (chi2 = 11.17, P = 0.26, I 2 = 19 %). So a fixed model was used in the test for overall effect. The pooled OR was 5.81 (95 % CI 3.36, 10.05), showing significantly better laryngeal preservation for patients undergoing TLM (P < 0.00). (Fig. 4). No publication bias was discovered using the funnel plot method.
Discussion
Organ preservation strategies are critical in the treatment of laryngeal cancer and have developed over the last 3 decades in the form of larynx-preservation surgery and radiotherapy [5, 20, 21]. With increased anatomic understanding, clinical experience, and long-term results demonstrating oncologic efficacy, TLM has become a more and more accepted optimal laryngeal preservation approach for early and moderately advanced tumors in place of primary radiotherapy [9, 22]. However, the current available evidence is insufficient to support the oncologic safety of TLM compared. Therefore, this study used meta-analysis method on the basis of previous studies, the previous literature data for a comprehensive analysis of the results of the two treatments for T1 glottic carcinoma.
Currently, the comparison between transoral laser microsurgery (TLM) and radiotherapy (RT) for T1 glottic carcinoma is complicated. In previous single-arm studies, the oncologic results of TLM appear to be similar to those of radiotherapy [23, 24]. To our knowledge, a recent meta-analysis by Abdurehim presented significantly better laryngeal preservation rate for laser surgery [25]. However, in our study, we revealed not only significantly better laryngeal preservation rate but also better overall survival rate for patients treated with laser surgery, compared to that for those treated with radiotherapy. Besides, the pooled local control rate in our study was similar to that in Abdurehim’ s [25].
Although TLM appeared to yield better results than RT in our analysis, some limitations may affect the quality of this review. In some studies, patients with surgical risk factors, larger and more infiltrating tumors, or tumors slightly invading the anterior commissure, radiotherapy was a preferred choice in some studies [6, 10]. On the other hand, patients with superficial lesions, with T1a tumor away from the anterior commissure, and the vocal process were more often treated by TLM. Taken together, only T1 glottic carcinoma was included in this comparison, and no significant heterogeneity among the studies was observed. Therefore, under the premise of not taking into account the above factors, our research shows that laser therapy is superior to radiotherapy for T1 glottic carcinoma.
In general, the optimal treatment strategy for T1 glottic carcinoma could offer the best cure rates, the best functional results, and the least complications and cost [10]. As very few validated or standardized functional assessment (mainly for voice and life quality) instruments exist, the evaluation of quality of voice and life had been challenged. Among the included studies, only three described the voice and/or life quality, and no differences were detected in these studies [13, 14, 17]. Our study is mainly concerned with the oncological outcomes, and future studies involving more detailed functional outcome and cost are needed. With these limitations of our study, more strictly designed, randomized controlled, multicenter trials will be needed.
Conclusions
Our meta-analysis revealed that ultimate overall survival and laryngeal preservation were significantly better for patients initially treated with transoral laser microsurgery (TLM) compared to the results of patients undergoing radiotherapy (RT). However, the results are inconclusive concerning the other outcome measures because of the limitations of this analysis. There is a trend that radiotherapy should be reserved for patients with surgical risk factors, advanced stage, deeper layers, or in cases of refusal of surgical intervention, and laser surgery for superficial T1 mid cord lesions [6]. Further studies considering the selection bias including the tumor depth and extent, the TNM staging, and the anterior commissure (AC) involvement with more detailed functional outcome and cost are needed. More high-quality, well-designed, prospectively randomized controlled, multicenter studies are required to validate the efficacy of laser surgery, and the standard treatment therapy for T1 glottic carcinoma is still underway.
TLM, transoral laser microsurgery; RT, radiotherapy; ENT, ear nose throat; LC, local control; OS, overall survival; LP, laryngeal preservation; AC, anterior commissure.
References
Ferlay J, Shin HR, Bray F et al (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127(12):2893–2917
Chu EA, Kim YJ (2008) Laryngeal cancer: diagnosis and preoperative work-up. Otolaryngol Clin North Am 41(4):673–695
Aqrawal N, Ha PK (2008) Management of early-stage laryngeal cancer. Otolaryngol Clin North Am 41(4):757–769
Mendenhall WM, Werning JW, Hinerman RW et al (2004) Management of T1-T2 glottic carcinoma. Cancer 100(9):1786–1792
Dey P, Arnold D, Wight R et al (2002) Radiotherapy versus open surgery versus endolaryngeal surgery (with or without laser) for early laryngeal squamous cell carcinoma. Cochrane Database Syst Rev 2:CD002027
Thurnher D, Erovic BM, Frommlet F et al (2008) Challenging a dogma—surgery yields superior long-term results for T1a squamous cell carcinoma of the glottic llarynx compared to radiotherapy. Eur J Surg Oncol 34(6):692–698
Strong MS, Jako GJ (1972) Laser surgery in the larynx. Early clinical experience with continuous CO2 laser. Ann Otol Rhinol Laryngol 81:791–798. 132:147–152
Wasserman JM, Wynn R, Bash TS et al (2006) Level of evidence in otolaryngology journals. Otolaryngol Head Neck Surg 134(5):717–723
Hatala R, Keitz S, Wyer P, Guyatt G, Evidence-based Medicine Teaching Tips Working Group (2005) Tips for learners of evidence-based medicine: 4. Assessing heterogeneity of primary studies in systematic reviews and whether to combine their results. CMAJ 172(5):661–665
Rosier JF, Gregoire V, Counoy H et al (1998) Comparison of external radiotherapy, laser microsurgery and partial laryngectomy for the treatment of T1N0M0 glottic carcinomas: a retrospective evaluation. Radiother Oncol 48(2):175–183
Puxeddu R, Argiolas F, Bielamowicz S et al (2000) Surgical therapy of T1 and selected cases of T2 glottic carcinoma: cordectomy, horizontal glottectomy and CO2 laser endoscopic resection. Tumori 86(4):277–282
Goor KM, Peeters AJ, Manieu HF et al (2007) Cordectomy by CO2 laser or radiotherapy for small T1a glottic carcinomas: costs, local control, survival, quality of life, and voice quality. Head Neck 29(2):128–136
Sjogren EV, Langeveld TP, Baatenburg de Jong RJ (2008) Clinical outcome of T1 glottic carcinoma since the introduction of endoscopic CO2 laser surgery as treatment option. Head Neck 30(9):1167–1174
Mahler V, Boysen M, Brondbo K (2010) Radiotherapy or CO(2) laser surgery as treatment of T(1a) glottic carcinoma. Eur Arch Otorhinolaryngol 267(5):743–750
Spector JG, Sessions DG, Chao KS et al (1999) StageI(T1N0M0) squamous cell carcinoma of the laryngeal glottis: therapeutic results and voice preservation. Head Neck 21(8):707–717
Schrijvers ML, Van Riel EL, Langendijk JA et al (2009) Higher laryngeal preservation rate after CO2 laser surgery compared with radiotherapy in T1a glottic laryngeal carcinoma. Head Neck 31(6):759–764
Kujath M, Kerr P, Myers C et al (2011) Functional outcomes and laryngectomy-free survival after transoral CO2 laser microsurgery for stage 1 and 2 glottic carcinoma. J Otolaryngo Head Neck Surg 40(suppl 1):S49–S58
Osborn HA, Hu A, Venkatessan V et al (2011) Comparison of endoscopic laser resection versus radiation therapy for the treatment of early glottic carcinoma. J Otolaryngol Head Neck Surg 40(3):200–204
Brandenburg JH (2001) Laser cordotomy versus radiotherapy: an objective cost analysis. Ann Otol Rhinol Laryngol 110(4):312–318
Chawla S, Carney AS (2009) Organ preservation surgery for laryngeal cancer. Head Neck Oncol 1:12
Pfister DG, Laurie SA, Weinstein GS et al (2006) American Society of Clinical Oncology clinical practice guideline for the use of larynx-preservation strategies in the treatment of laryngeal cancer. J Clin Oncol 24:3693–3704
Rubinstein M, Armstrong WB (2011) Transoral laser microsurgery for laryngeal cancer: a primer and review of laser dosimetry. Laser Med Sci 26(1):113–124
Peretti G, Piazza C, Cocco D et al (2010) Transoral CO(2) laser treatment for T(is)-T(3) glottic cancer: the University of Brescia experience on 595 patients. Head Neck 32:977–983
Chera BS, Amdur RJ, Morris CG et al (2010) T1N0 to T2N0 squamous cell carcinoma of the glottic larynx treated with definitive radiotherapy. Int J Radiat Oncol Biol Phys 78:461–466
Abdurehim Y, Hua Z, Yasin Y et al (2012) Treatment laser surgery versus radiotherapy: systematic review and meta-analysis for treatment options of T1a glottic cancer. Head Neck 34(1):23–33
Acknowledgments
We would like to thank Hai-Lan Mo and Jie Li for the assistance in performing this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Role of funding source
There was no external funding source.
Ethical approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.” Our study is a retrospective review. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Mo, HL., Li, J., Yang, X. et al. Transoral laser microsurgery versus radiotherapy for T1 glottic carcinoma: a systematic review and meta-analysis. Lasers Med Sci 32, 461–467 (2017). https://doi.org/10.1007/s10103-016-2103-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-016-2103-8