Abstract
Purpose
Intra-arterial (IA) infusion of calcium channel blockers (CCBs) has been widely applied in treating medically refractory vasospasm; however, surprisingly little is known regarding their vasodilatory duration. This study was undertaken to compare attributes of nicardipine and dantrolene, focusing on efficacy and capacity for sustained vasodilation.
Methods
In New Zealand white rabbits (N = 22), vasospasm was individually provoked through experimentally induced subarachnoid hemorrhage and confirmed via conventional angiography, grouping animals by IA-infused drug (nicardipine vs. dantrolene). Controls received normal saline. After chemoangioplasty, follow-up angiography was performed at intervals of 1–3 h for 6 h to compare vasospastic and dilated (i.e., treated) arterial diameters. Drug efficacy, duration of action, and changes in mean arterial pressure (relative to baseline) were analyzed by group.
Results
Compared with controls, effective vasodilation was evident in both nicardipine and dantrolene test groups after IA infusion. Vasodilatory effects of nicardipine peaked at 1 h, returning to former vasospastic states at 3 h. In dantrolene recipients, vasodilation endured longer, lasting >6 h. Only the nicardipine group showed a significant 3‑h period of lowered blood pressure.
Conclusion
Unlike the vasodilatory action of a CCB, sustained for < 3 h after IA infusion, the effect of dantrolene endured for > 6 h. This outcome suggests that IA dantrolene infused alone or together with a conventional CCB infusion may be a new means of prolonging vasodilatory effect. Further research is needed to assess durations of IA-infused vasodilatory drug based on perfusion status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although surgical and endovascular treatment of cerebral aneurysms have rapidly advanced, morbidity and mortality currently remain unchanged due to vasospasm. The etiology of vasospasm is not entirely clear, and there are no definitive therapies as yet to resolve severe symptomatic states, preventing delayed cerebral ischemia. A conservative remedy for vasospasm is thus a high priority.
Oral nimodipine is the only medical intervention to date with proven efficacy for vasospasm [1,2,3]. In practice, however, various alternatives for vasodilation, e.g., chemical angioplasty by intra-arterial (IA) or intrathecal drug infusion and mechanical angioplasty via balloon or retrievable stent, have been implemented for severe symptomatic vasospasm refractory to medical treatment [2,3,4]. Calcium channel blockers (CCBs) are the preferred IA agents at present for chemical angioplasty as many reports on safety and efficacy attest [2, 3, 5,6,7,8,9,10,11,12,13,14]. Nevertheless, the limitations of IA-infused CCBs, particularly their duration of action, have raised concerns. Some patients with severe vasospasm seem to experience neurologic deterioration within hours after IA drug-infused recovery, necessitating two or three daily treatments. The short-lived vasodilation that IA-infused CCBs afford may be responsible. Lim et al. [15] have reported that in an animal model of vasospasm, such effects were not sustained more than 2 h after IA infusion.
Dantrolene is a known ryanodine receptor (RyR) inhibitor, already FDA approved for treating malignant hyperthermia and muscle spastic disorder. Its mechanism of action on smooth muscle cells differs from that of CCBs. Ortiz Torres et al. [16] have suggested that IA-infused dantrolene is a safe and effective novel treatment option for vasospasm, reporting its use in two patients. The present investigation was launched to examine characteristics of nicardipine (a CCB popular in IA chemoangioplasty) and dantrolene. A rabbit animal model enabled side-by-side comparisons of these agents, based on angiographic assessments of vasodilatory efficacy and duration.
Material and Methods
Animal Selection and Preparation
The study protocol complied with provisions of our institutional committee for ethical animal experimentation and was granted approval. We selected 35 commercially available New Zealand white rabbits (weight 2.5–3.0 kg) for testing. In a fasted state (6 h prior), each animal received a dual-agent (ketamine, 35 mg/kg; xylazine, 5 mg/kg) anesthetic intramuscular (IM) injection of the thigh, supplemented at 20-min intervals during procedures as needed. Depilatory cream removed inguinal and occipital hair during anesthesia. Each rabbit was then secured supine to the examination table. All were subjected to skin testing and given IM injections of a first-generation cephalosporin (50 mg/day) for 3 days after experiment completion.
Puncture of Femoral Artery and Introducer Insertion
We sterilized (75% alcohol) inguinal regions of anesthetized animals, each positioned as above. Femoral artery was palpated and exposed within its neurovascular bundle, making an inguinal incision (~ 20 mm) under local anesthesia (1% lidocaine). Next, a 4-Fr introducer was installed (Seldinger technique) via femoral artery puncture and secured to femoral artery, filling it with heparin/normal saline solution for subsequent transducer passage. Blood pressure (BP) readings were thereby obtained. At completion of cerebral angiography, introducers were secured within subcutis (5‑0 nylon skin suture) to facilitate follow-up angiography 3 days after inducing subarachnoid hemorrhage (SAH).
SAH Induction in Animal Model
Occipital regions of anesthetized animals (positioned supine, 90º left-rotated heads) were sterilized (75% alcohol). Contiguous occipital-cervical areas were epilated and heads bent for puncture of dura mater under local anesthesia (1% lidocaine) and with fluoroscopic guidance, using a 23‑G spinal needle to pierce atlanto-occipital membranes. To identify subarachnoid space, cisternal delivery of mixed contrast medium and normal saline (1:1 ratio) commenced at first sign of cerebrospinal fluid (CSF). A modicum (~ 2 ml) of CSF was then withdrawn, instilling a 2 ml sample of femoral arterial blood as replacement via spinal needle. Thereafter, animal heads were lowered (~ 30º) and allowed 20 min of stabilization [12, 14]. Angiography equipment (Allura Xper FD20/10; Philips Healthcare, Best, The Netherlands) used for Xper computed tomography (CT) enabled verification of SAH.
Cerebral Angiography and IA Drug Infusion
Cerebral angiography (Allura Xper FD20/10; Philips Healthcare) entailed iso-osmolar contrast delivery. For IA drug infusion, microcatheters (Excelsior SL-10; Stryker Neurovascular, Fremont, CA, USA) and microguidewires (Synchro14; Stryker Neurovascular) were engaged. Routine angiographic assessments of vertebral and basilar arterial diameters at baseline (i.e., before SAH induction) provided reference points for later comparisons. Angiography was repeated on day 3 of the SAH model to confirm basilar arterial vasospasm, defined as > 30% luminal compromise relative to baseline level. Luminal constriction < 30% was disqualifying, eliminating animals from further involvement. Rabbits demonstrating vasospasm of acceptable level were then randomly assigned to IA therapeutics as follows: group N nicardipine (0.06 mg/kg), group D dantrolene (1 or 2 mg/kg) or group C normal saline controls.
Established dosing of nicardipine, known to exert maximum physiologic effects in terms of arterial vasodilation, was applied [17, 18]. Loading/maintenance dosing of dantrolene seemed to be in the range of 1 or 2 mg/kg. Each IA agent was separately admixed with normal saline for microcatheter infusion in a period of 10 min. A 20% drop in BP (relative to baseline) warranted 50% dose reduction, any further decline calling for cessation Once administered, immediate therapeutic effects were determined by extent of vasospastic easing at points of maximum luminal compromise. Follow-up angiography was pursued at intervals of 1–3 h for a total of 6 h, tracking luminal magnitudes (Fig. 1) to monitor potential vasospastic reversions.
Digital subtraction angiograms of vertebrobasilar artery in rabbits over time (nicardipine group, a–d; dantrolene group, e–h). a Angiographic image prior to hemorrhage. b Follow-up angiographic image 3 days after subarachnoid hemorrhage (vasospasm). c,d Angiographic images 1 and 3 h after intra-arterial (IA) drug infusion. e Angiographic image prior to hemorrhage. f Follow-up angiographic image 3 days after subarachnoid hemorrhage (vasospasm) and g,h angiographic images 3 and 6 h after IA drug infusion
Angiographic Gauging of Arterial Diameters
Arterial diameters (primarily of basilar artery) were assessed using a proprietary double-blind computer application (Vascular Quantification Software; Philips Healthcare) designed for cerebral angiography. Images selected were in arterial phase, least prone to motion artifact, measuring magnitudes in transverse plane. Two investigators, blinded to any pertinent input, measured diameters of normal and most severely vasospastic arteries, recording the average of two measurements taken at respective time intervals. Grading of luminal spasm reflected percent compromise in arterial diameter (relative to baseline), vasospastic reversal percentage corresponding with vasodilatory effect after IA infusion.
Statistical Analysis
Continuous variables were expressed as median and range values. The Wilcoxon signed-rank test was used accordingly for pairwise analysis of vasodilatory effects and change in BP after IA infusion. To compare group vasodilatory effects, durations of action, and BP changes after IA infusion, the Kruskal-Wallis test was applied, invoking the Bonferroni correction for multiple comparisons of statistically significant outcomes. A linear mixed model (LMM) served to identify associations of time effect, group effect, and interaction between the two. Group pairwise comparisons were conducted through LMM. The analytics were powered by standard software (SAS v9.4; SAS Institute, Cary, NC, USA). All tests were 2‑sided, with 0.05 denoting statistical significance.
Result
Data Summary
The 35 rabbits initially selected suffered 9 deaths and 8 induction failures (insufficient vasospasm), leaving 18 animals for our 3 experimental groups (each n = 6). There were no instances in which BP declines forced interruption of drug infusion. Compared with baseline status (prior to SAH), the overall median for vasoconstriction of basilar artery was 54.7% (range 36.6–62.5%) in this animal model of vasospasm. Groupwise medians were as follows: nicardipine 55.3% (range 36.6–60.6%), dantrolene 49.0% (range 36.9–61.2%) and controls 61.7% (range 47.2–62.5%). See Table 1 for summary of data.
Efficacy of IA CCB Infusion
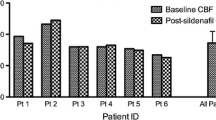
Upon induction of vasospasm, changes in diameters of basilar arteries (relative to baseline levels) were measured immediately and at 1–3 h intervals after IA infusion (Table 1). Immediate vasodilatory effects were regularly noted (group N, 35.1%; group D, 49.4%), showing statistical significance (p = 0.031 and p = 0.031, respectively) in both test groups, compared with controls (no vasodilation). Repeat angiograms at 1 h indicated peak vasodilation in group N (51.5%; p = 0.031) and sustained vasodilation in group D (40.8%; p = 0.031). At 3 h, significant vasodilation remained in group D (57.3%; p = 0.031), having dissipated in group N and returned to former vasospastic states. At 6 h, vasodilatory effect persisted in group D only (Fig. 2). Supplementary Table 1 shows differing pairwise time frames for each group in the LMM. Estimates of least square means and p-values are shown, adjusted using Bonferroni correction.
In groupwise comparisons of maximum vasodilatory efficacy, both agents achieved similar effects immediately and at 1 h after IA infusion. Subgroup analysis of group D revealed that dantrolene at higher dose (2 mg/kg) outperformed the lower dose (1 mg/kg) in terms of potency (Fig. 3); however, statistical significance was not reached, given so few animals (Supplementary Table 2). Vasodilation in group D (either dose) lasted > 6 h, enduring for < 3 h in group N.
Mean Arterial Pressure Flux During and After IA Drug Infusion
The BP decline was observed during and after IA infusion of nicardipine (group N), an average loss of 10 mm Hg recorded within 1 h after administration. There was gradual recovery after 2 h, with normalization after 3 h. Almost no change in BP was evident after IA infusion of dantrolene (groups D) or in saline-infused controls (group C).
Discussion
Impaired cerebral perfusion due to effects of SAH on cerebral vessels has been associated with delayed cerebral ischemia and currently is deemed the largest contributor to morbidity and mortality in this setting. The therapeutic priority for treating vasospasm after subarachnoid hemorrhage (SAH) is preservation of cerebral blood flow, ostensibly through acceptably sustained central perfusion pressures. Although the mechanisms responsible for delayed cerebral ischemia are not fully understood, a critical issue reportedly is cellular influx of calcium [7, 19]. The CCBs serve to suppress this influx, which is key in preventing and treating vasospasm and explains why oral intake of nimodipine is strongly advised [2]. As IA-infused agents of chemoangioplasty, they have been used for some time to treat severely symptomatic patients refractory to medical remedies, amassing an abundance of evidentiary support during the past three decades.
In practice, we have often observed that many patients improve clinically and angiographically after IA CCB infusion; however, the chief limitation of such interventions is durability of vasodilatory effect. Specifically, there is no consensus on how long the vasodilation of IA chemoangioplasty is sustained or how frequently chemoangioplasty must be performed to avoid cerebral ischemia. Lim et al. [15] have already determined that more than 2 h after IA infusion, CCB vasodilatory effects are lacking in an animal model of vasospasm.
Dantrolene is a RyR blocker approved for treatment of malignant hyperthermia, chronic spasticity, and neuroleptic malignant syndrome [20, 21]. Its mechanism of action differs from that of CCBs. Vasospasm is related to vascular tone, based on persistent elevation of intracellular Ca++ in vascular smooth muscle [22]. This rise in intracellular Ca++ may be secondary to increased entry of extracellular Ca++ upon activation of L‑type voltage-dependent Ca++channels [23] or to heightened RyR release of Ca++ from sarcoplasmic reticulum. The CCBs are L‑type channel blockers, whereas dantrolene imposes RyR blockade. Salomone et al. [24] have therefore suggested that combined use of these drugs may reduce both incidence and severity of vasospasm, achieved by dual activity. Moreover, both dantrolene and CCBs exert neuroprotective effects through increased antioxidant defense [25].
In rabbits with induced vasospasm, we have demonstrated that the vasodilatory effect of dantrolene (> 6 h) significantly outlasts that of IA-infused nicardipine (< 3 h) after IA infusion. According to Lim et al. [15], neither nicardipine nor nimodipine show sustained vasodilation more than 2 h after IA infusion. Intravenous (IV) nicardipine has a rapid onset of action (major effects 10–15 min; plasma elimination half-life 40–60 min) but its plasma concentrations decline triexponentially once infusion is ceased, displaying rapid early distribution (alpha half-life 2.7 min), an intermediate phase (beta half-life 44.8 min) and a slow terminal phase (gamma half-life 14.4 h) detectable only after long-term infusion. This means that its onset is quick and its duration of action is relatively short. Dantrolene, on the other hand, has a comparatively longer half-life (~ 12 h according to available data). In adults, cumulative IV dosing of 2.2–2.5 mg/kg produces steady plasma concentrations for > 5 h [26]. Majidi et al. [27] and Ortiz Torres et al. [16] have claimed in separate case reports that IA dantrolene infusion appears safe and effective in treating refractory vasospasm, affirming that its vasodilatory effect may exceed 24 h (based on 24‑h and 48‑h follow-up angiography); however, these publications involved just 1 or 2 patients and 1‑day or 2‑day follow-up studies, failing to pinpoint vasodilatory limits with precision. To our knowledge, the present effort is the first to directly compare a CCB with dantrolene in terms of vasodilatory capacity and duration, using an animal model of cerebral vasospasm. Ultimately, we have demonstrated that the vasodilatory effect of dantrolene (> 6 h) endures significantly longer than that of nicardipine (< 3 h).
There are a few reports in which single dose IV dantrolene (1.25 or 2.5 mg/kg) given to patients with cerebral vasospasm (after SAH) significantly reduced spasm and aided in patient recovery [28, 29]. Regarding the safety of dantrolene, Muehlschlegel et al. [30] have found IV dantrolene (1.25 mg/kg) treatment of vasospasm to be feasible, tolerable, and safe in a randomized, double-blind, and placebo-controlled trial. Investigations by Majidi et al. [27] and Ortiz Torres et al. [16] also support the efficacy of IA dantrolene infusion for refractory vasospasm at dosages of 15–30 mg (< 1 mg/kg) in adult patients. In our study, we administered dantrolene at 1 or 2 mg/kg, having no real dosing standards for IA infusion. Its vasodilatory effect seemed dose-dependent (greater potency at 2 vs. 1 mg/kg), proving similar to nicardipine (at maximum-effect dosage) when administered at 2 mg/kg; however, duration of action was the same (> 6 h) for both dantrolene subsets. Roman et al. [22] have likewise shown in a rat model that improved endothelial-dependent relaxation and reduced vascular contractility conferred by dantrolene are dose-dependent phenomena. Given our findings, we feel that dantrolene alone or added to a conventional CCB for IA infusion may offer a new means of prolonging vasodilatory relief in patients with cerebral vasospasm.
This study has some acknowledged limitations. We equated the presence of vasospasm as well as its degree or later improvement, with the most severe points of arterial compromise. Because the vasodilatory effects of IA-infused drugs impact both large arteries and small arterioles, such measurements may not reflect actual perfusion states. We must also concede that the number of animals servicing this experiment was marginal for 3‑group comparison. In addition, there are no established dosing equivalents for treating cerebral blood vessels with these medications, and studies focused on drug potencies have generated conflicting results. Hence, the IA drug dosages used for comparison herein may not be equivalent. Finally, we magnified photoimages to determine basilar arterial diameters, making it difficult to distinguish boundaries of small vessels and perhaps introducing measurement errors. In aggregate, these drawbacks are considerable and should be appropriately resolved going forward.
Conclusion
In a rabbit model of cerebral vasospasm, both nicardipine and dantrolene achieved effective vasodilation after IA drug infusion; however, the vasodilatory action of IA-infused CCB proved significantly shorter in duration (< 3 h) than that of IA-infused dantrolene (> 6 h). Thus, dantrolene alone or combined with a conventional CCB for IA infusion may be a reasonable means of prolonging vasodilatory action. Further study is needed to determine duration of IA-infused vasodilatory drugs based on perfusion status.
References
Allen GS, Ahn HS, Preziosi TJ, Battye R, Boone SC, Boone SC, Chou SN, Kelly DL, Weir BK, Crabbe RA, Lavik PJ, Rosenbloom SB, Dorsey FC, Ingram CR, Mellits DE, Bertsch LA, Boisvert DP, Hundley MB, Johnson RK, Strom JA, Transou CR. Cerebral arterial spasm--a controlled trial of nimodipine in patients with subarachnoid hemorrhage. N Engl J Med. 1983;308:619–24.
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, Hoh BL, Kirkness CJ, Naidech AM, Ogilvy CS, Patel AB, Thompson BG, Vespa P; American Heart Association Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Clinical Cardiology. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43:1711–37.
Hejčl A, Cihlář F, Smolka V, Vachata P, Bartoš R, Procházka J, Cihlář J, Sameš M. Chemical angioplasty with spasmolytics for vasospasm after subarachnoid hemorrhage. Acta Neurochir (Wien). 2017;159:713–20.
Feng L, Fitzsimmons BF, Young WL, Berman MF, Lin E, Aagaard BD, Duong H, Pile-Spellman J. Intraarterially administered verapamil as adjunct therapy for cerebral vasospasm: safety and 2-year experience. AJNR Am J Neuroradiol. 2002;23:1284–90.
Hoh BL, Ogilvy CS. Endovascular treatment of cerebral vasospasm: transluminal balloon angioplasty, intra-arterial papaverine, and intra-arterial nicardipine. Neurosurg Clin N Am. 2005;16:501–16, vi.
Hänggi D, Turowski B, Beseoglu K, Yong M, Steiger HJ. Intra-arterial nimodipine for severe cerebral vasospasm after aneurysmal subarachnoid hemorrhage: influence on clinical course and cerebral perfusion. AJNR Am J Neuroradiol. 2008;29:1053–60.
Keuskamp J, Murali R, Chao KH. High-dose intraarterial verapamil in the treatment of cerebral vasospasm after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2008;108:458–63.
Kumar A, Phalak M. Is intra arterial nimodipine really beneficial in vasospasm following aneurysmal subarachnoid hemorrhage? Br J Neurosurg. 2017;31:290.
Lele A, Lyon T, Pollack A, Husmann K, Reeves A. Intra-arterial nicardipine for the treatment of cerebral vasospasm in postpartum cerebral angiopathy: a case study and review of literature. Int J Neurosci. 2011;121:537–42.
Godfraind T, Miller RC. Specificity of action of Ca++ entry blockers. A comparison of their actions in rat arteries and in human coronary arteries. Circ Res. 1983;52(2 Pt 2):I81–91.
Huang RQ, Jiang FG, Feng ZM, Wang TY. Nicardipine in the treatment of aneurysmal subarachnoid haemorrhage: a meta-analysis of published data. Acta Neurol Belg. 2013;113:3–6.
Jansen I, Tfelt-Hansen P, Edvinsson L. Comparison of the calcium entry blockers nimodipine and flunarizine on human cerebral and temporal arteries: role in cerebrovascular disorders. Eur J Clin Pharmacol. 1991;40:7–15.
Katz AM, Leach NM. Differential effects of 1,4-dihydropyridine calcium channel blockers: therapeutic implications. J Clin Pharmacol. 1987;27:825–34.
Linfante I, Delgado-Mederos R, Andreone V, Gounis M, Hendricks L, Wakhloo AK. Angiographic and hemodynamic effect of high concentration of intra-arterial nicardipine in cerebral vasospasm. Neurosurgery. 2008;63:1080–6; discussion 1086–7.
Lim J, Cho YD, Kwon HJ, Byoun SH, Koh HS, Park B, Choi SW. Duration of Vasodilatory Action After Intra-arterial Infusions of Calcium Channel Blockers in Animal Model of Cerebral Vasospasm. Neurocrit Care. 2021;34:867–75.
Ortiz Torres MJ, Jahngir M, Qualls K, Litofsky NS, Nattanmai P, Qureshi AI. Intra-Arterial Dantrolene for Refractory Cerebral Vasospasm in Patients with Aneurysmal Subarachnoid Hemorrhage. World Neurosurg. 2019;125:247–52.
Yui H, Imaizumi U, Beppu H, Ito M, Furuya M, Arisaka H, Yoshida K. Comparative effects of verapamil, nicardipine, and nitroglycerin on myocardial ischemia/reperfusion injury. Anesthesiol Res Pract. 2011;2011:521084. https://doi.org/10.1155/2011/521084.
Toshima M, Kassell NF, Sasaki T, Tanaka Y, Machi T. The effect of hemoglobin on vasodilatory effect of calcium antagonists in the isolated rabbit basilar artery. J Neurosurg. 1992;76:670–8.
Tallarico RT, Pizzi MA, Freeman WD. Investigational drugs for vasospasm after subarachnoid hemorrhage. Expert Opin Investig Drugs. 2018;27:313–24.
Aslan A, Cemek M, Buyukokuroglu ME, Altunbas K, Bas O, Yurumez Y, Cosar M. Dantrolene can reduce secondary damage after spinal cord injury. Eur Spine J. 2009;18:1442–51.
Neylon CB, Richards SM, Larsen MA, Agrotis A, Bobik A. Multiple types of ryanodine receptor/Ca2+ release channels are expressed in vascular smooth muscle. Biochem Biophys Res Commun. 1995;215:814–21.
Román M, Ramírez JM, Morales M, Crespo MJ. Significant reduction of vascular reactivity with dantrolene and nimodipine in diabetic rats: a potential approach to cerebral vasospasm management in diabetes. Pharmacol Rep. 2020;72:126–34.
Navedo MF, Takeda Y, Nieves-Cintrón M, Molkentin JD, Santana LF. Elevated Ca2+ sparklet activity during acute hyperglycemia and diabetes in cerebral arterial smooth muscle cells. Am J Physiol Cell Physiol. 2010;298:C211–20.
Salomone S, Soydan G, Moskowitz MA, Sims JR. Inhibition of cerebral vasoconstriction by dantrolene and nimodipine. Neurocrit Care. 2009;10:93–102.
Torres BB, Caldeira FM, Gomes MG, Serakides R, de Marco Viott A, Bertagnolli AC, Fukushima FB, de Oliveira KM, Gomes MV, de Melo EG. Effects of dantrolene on apoptosis and immunohistochemical expression of NeuN in the spinal cord after traumatic injury in rats. Int J Exp Pathol. 2010;91:530–6.
Flewellen EH, Nelson TE, Jones WP, Arens JF, Wagner DL. Dantrolene dose response in awake man: implications for management of malignant hyperthermia. Anesthesiology. 1983;59:275–80.
Majidi S, Grigoryan M, Tekle WG, Qureshi AI. Intra-arterial dantrolene for refractory cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2012;17:245–9.
Sabouri M, Momeni M, Khorvash F, Rezvani M, Tabesh H. The Effect of a Single dose Dantrolene in Patients with Vasospasm Following Aneurysmal Subarachnoid Hemorrhage. Adv Biomed Res. 2017;6:83.
Muehlschlegel S, Rordorf G, Sims J. Effects of a single dose of dantrolene in patients with cerebral vasospasm after subarachnoid hemorrhage: a prospective pilot study. Stroke. 2011;42:1301–6.
Muehlschlegel S, Carandang R, Hall W, Kini N, Izzy S, Garland B, Ouillette C, van der Bom IM, Flood TF, Gounis MJ, Weaver JP, Barton B, Wakhloo AK. Dantrolene for cerebral vasospasm after subarachnoid haemorrhage: a randomised double blind placebo-controlled safety trial. J Neurol Neurosurg Psychiatry. 2015;86:1029–35.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. NRF-2020R1F1A1075087).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Lim, Y.D. Cho and H.S. Byoun declare that they have no competing interests.
Supplementary Information
Rights and permissions
About this article
Cite this article
Lim, J., Cho, Y.D. & Byoun, H.S. Comparative Study of Vasodilatation After Intra-arterial Nicardipine or Dantrolene Infusion in Animal Model of Cerebral Vasospasm. Clin Neuroradiol 32, 1011–1017 (2022). https://doi.org/10.1007/s00062-022-01151-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-022-01151-4