Abstract
Background
Diabetics have a higher risk of developing cerebral vasospasms (CVSPs) than non-diabetics. Current therapies are ineffective in reducing CVSPs, but a a combination of dantrolene and nimodipine may be a viable treatment. Considering the potentially harmful secondary effects of dantrolene, however, we evaluated the efficacy of 10 μM dantrolene compared to 50 μM dantrolene alone or in combination with 50 nM nimodipine.
Methods
Dose–response curves for the phenylephrine (PHE)-induced contraction and acetylcholine (ACh)-induced relaxation were performed on aortic rings from diabetic and non-diabetic rats, before and after a 30-min incubation period with dantrolene (50 μM and 10 μM), alone or in combination with 50 nM nimodipine.
Results
Whereas 50 μM dantrolene reduced PHE-induced contraction by 47% in diabetic rats and 29% in controls, 10 μM dantrolene failed to reduce this parameter in either group. Furthermore, 50 μM dantrolene reduced PHE-induced contraction by about 80% in both diabetic and controls when combined with nimodipine (N = 9, P < 0.05). The combination of 10 μM dantrolene and 50 nM nimodipine, however, was ineffective. Only 50 μM dantrolene improved endothelial dysfunction.
Conclusions
Improved endothelial-dependent relaxation and reduced vascular contractility with dantrolene are dose dependent. Thus, although dantrolene appears to be a promising alternative for the treatment of CVSPs when added to conventional therapies, careful titration should be performed to achieve a significant reduction in vascular hyperreactivity. Moreover, if our findings with rats are applicable to humans, the combined use of dantrolene and nimodipine at optimal doses may reduce CVSPs, especially in the diabetic population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic patients have a higher incidence of cardiovascular disease (CVD) and are more prone to developing stroke than non-diabetics [1]. Moreover, after suffering a stroke, diabetics have a greater predisposition for developing cerebral vasospasms (CVSPs), even when under glycemic control [2]. CVSPs have been associated with increased vascular tone due to persistent elevation of intracellular Ca+2 in vascular smooth muscle (VSM). The rise in intracellular Ca+2 may be secondary to increased extracellular Ca+2 entry upon activation of L-type voltage-dependent Ca+2 channels (VDCC) [3], or to increased ryanodine receptor (RyR) release of Ca+2 from the sarcoplasmic reticulum (SR) [4].
Increased oxidative stress, endothelial dysfunction, and vascular hyperreactivity have been linked to the genesis of diabetic vascular complications, including CVSPs [5,6,7]. Unlike in non-diabetics, alterations in the status of nitric oxide synthase (NOS) are present in both diabetic animal models and patients [8,9,10], suggesting that reduced nitric oxide (NO) availability contributes to increased vascular tone, which is a hallmark of diabetes. In addition, hyperglycemia alters Ca+2 influx through L-type voltage-dependent Ca+2 channels [3, 11]. Thus, alterations in Ca+2 channel activity and homeostasis may also participate in the genesis of vascular dysfunction and predispose the vasculature to CVSPs in diabetes [11]. Together, these findings support the notion that diabetes-induced endothelial dysfunction and vascular hyperreactivity underlie the higher incidence of CVSPs in diabetic patients, and that the pathophysiology of this condition is multifactorial and differs between diabetics and non-diabetics.
Despite the pathophysiologic differences between diabetics and non-diabetics, the current pharmacological treatment for CVSPs is similar for both groups, and includes the use of nimodipine, nicardipine, and other Ca+2 channel blockers (CCB) [1]. These drugs are not completely effective in reducing CVSPs, however, because Ca+2 antagonists only block the influx of Ca+2 into the cytosol without interfering with the Ca+2 released from the SR. Therefore, cerebral infarction, neurological complications, and death rates remain elevated in patients, despite the use of Ca+2 antagonists [12]. Thus, it is crucial to evaluate the effectiveness of additional pharmacological interventions other than CCBs to reduce the incidence and severity of CVSPs, particularly in the diabetic population.
Dantrolene is a RyR blocker approved for the treatment of chronic spasticity, malignant hyperthermia, and the management of neuroleptic malignant syndrome [13, 14]. Dantrolene depresses excitation–contraction coupling in the muscle fiber by inhibiting Ca+2 release from the SR throughout the blockade of RyRs [15]. The three subtypes of the RyR family (RyR1, RyR2, and RyR3) are present in the VSM of the thoracic aorta [16], the mesenteric arteries [14], the large cerebral arteries [17], and the cerebral microcirculation [4]. Dantrolene effectively blocks all the RyR subtypes [18, 19], reduces malondialdehyde (MDA) levels [20, 21], and provides neuroprotection by increasing the antioxidant defenses in spinal cord-injured rats [22]. Moreover, concomitant administration of dantrolene and nimodipine significantly decreases serotonin-induced contraction in isolated basilar and femoral arteries of rats [23], which suggests that the combined use of these drugs reduces the incidence and severity of CVSPs by simultaneously blocking Ca+2 entry through the L-type VDCC and Ca+2 release by RyR from the SR.
Although dantrolene has not been approved for the clinical management of CVSPs, it has been used for this purpose with a limited number of patients in the clinical setting. The administration of 2.5 mg/kg (IV) to three non-diabetic patients with CVSPs attenuated cerebral vasoconstriction, and decreased middle cerebral artery blood flow velocities without affecting cerebral perfusion pressure, intracranial pressure, or central venous pressure [24], and a dose of 1.25 mg/kg (IV) dantrolene proved even more effective in five non-diabetic CVSP patients [12]. Moreover, the administration of 1.25 mg/kg dantrolene to 16 patients with subarachnoid hemorrhage (SAH) was well tolerated and did not cause hyponatremia, liver toxicity, brain edema, or systemic hypotension, suggesting that the drug can serve as an alternative pharmacological tool for the management of this condition [25]. The latter results suggest that the effectiveness of dantrolene is not dose dependent. By contrast, Salomone and colleagues [23] found that pre-incubation of rat femoral artery with 30 or 100 µM dantrolene significantly reduced 5-HT-induced contraction, whereas a low concentration of 10 µM was ineffective in reducing this parameter. Thus, it is important to determine if the reduction of vascular reactivity with dantrolene is dose dependent, or a property of the drug that is independent of the dose. Previous studies from our laboratory showed that the combination of 50 µM dantrolene and 50 nM nimodipine significantly decreased arterial tone by reducing phenylephrine (PHE)-induced contraction of aortic rings of both diabetic and non-diabetic rats and by improving endothelial function in diabetic rats [21]. Due to the potentially harmful secondary systemic effects of dantrolene [25], which may be amplified by the addition of a CCB, we evaluated and compared the efficacy of a low (10 µM) versus a high (50 µM) concentration of dantrolene in streptozotocin (STZ)-induced diabetic rats to determine if the reduction in vascular reactivity found with the 50 µM concentration is also achieved at a significantly lower concentration to minimize the secondary effects.
Drugs
Dantrolene, nimodipine, phenylephrine (PHE), acetylcholine (ACh), sodium nitroprusside (SNP), and NG-nitro-l-arginine (l-NAME) were obtained from Sigma Chemical Co. (San Louis, MO). The concentrations of nimodipine (50 nM) and dantrolene (10 µM and 50 µM) were selected based on comparable studies in different vascular beds from rats [23, 26, 27].
Materials and methods
Experimental animal model
Forty male Sprague–Dawley rats (Taconic Biosciences Inc, Germantown, NY), of approximately 4 weeks of age were divided into a diabetic group and a non-diabetic group, with each group containing 20 animals. To induce diabetes, we used the following method as described previously [21]. Rats were fasted overnight and then injected intraperitoneally (IP) with streptozotocin (STZ; 65 mg/kg) dissolved in a 0.1 M citrate buffer (pH 4.5). Non-diabetic animals, which were used as controls, were only injected with the citrate buffer solution. Hyperglycemia was verified 24 h after the STZ injection with a TRUEtrack blood glucose monitoring system (NIPRO Diagnostics, Fort Lauderdale, FL). Blood glucose levels were monitored once a week in all animals. All the experiments were performed at 4 weeks following diabetes induction. The diabetic rats never received insulin supplementation. All animals were housed in a temperature-controlled room on a 12-h light/dark cycle. Water and food (Harlan Rodent Diet, 18% protein) were provided ad libitum. All procedures involving the animals were approved by the Institutional Animal Care and Use Committee (Protocol #2590115) and adhered to the Guide and Care for the Use of Laboratory Animals published in 2011 by the National Institutes of Health (USA).
Tissue preparation for isometric tension studies
Endothelial-dependent relaxation was verified following the methods of Quidgley and colleagues [28]. Briefly, rats were anesthetized with a combination of ketamine (50 mg/kg, i.p.) and xylazine (4 mg/kg, i.p.). After full anesthesia, aortic rings, approximately 5 mm in length, were obtained from the proximal segment of each aorta for use in the contraction and relaxation studies. The connective tissue adjacent to the aortic adventitia was carefully removed, avoiding damages to the smooth muscle and the endothelium. The entire preparation was mounted in a two-hook, 50 ml organ chamber (Radnoti Co, Monrovia, CA) and bathed in Krebs’ bicarbonate solution (aerated with a mixture of 95% O2 and 5% CO2 at 37°C). The rings were suspended horizontally with a resting tension of 2.3g, and connected to a FT03C Grass transducer (Warwick, RI). Once the optimal tension was reached, the rings were subjected to a 1 h equilibration. The signal was analyzed with a data acquisition card (National Instruments, Austin, TX; PC-LPM-16/PnP), and changes in isometric tension were recorded with LabView software (National Instruments).
Measurement of aortic ring relaxation and contraction
To determine the effect of 10 µM and 50 µM dantrolene, 50 nM nimodipine, and the combination of these drugs on endothelial-dependent relaxation, aortic rings were pre-contracted with PHE (1.0 µM), following the protocol described previously [21, 28]. When the maximal contraction reached a plateau, cumulative concentration–response curves (from 0.1 nM to 10 µM) for ACh were generated. After completion of the curves, the rings were washed and stabilized. Additional concentration–response curves were then generated after a 30-min incubation period with the drugs. In each experiment, the relaxation was expressed as a percentage of the relaxation relative to the maximal contraction induced by 1.0 µM of PHE. The maximal relaxation achieved (Emax) and the concentrations inducing 50% of maximal relaxation (EC50) for ACh were determined before and after incubation with dantrolene, nimodipine, and these drugs in combination through mathematical analysis of the concentration–response curves, and then compared. Sodium nitroprusside (SNP, 1.0 μM) was also used to fully relax aortic rings after completion of each protocol to assess endothelial-independent relaxation.
To evaluate the role of nitric oxide (NO) in ACh-induced relaxation after incubation with dantrolene, nimodipine, or these drugs in combination, aortic rings were incubated concomitantly with 1 mM NG-nitro-l-arginine (l-NAME), an inhibitor of NOS. The rings were pre-contracted with 1.0 µM of PHE, and ACh concentration–response curves were generated before and after incubation with l-NAME and each drug, either alone or in combination.
The effects of 10 and 50 µM dantrolene, 50 nM nimodipine, and the combination of these drugs, on the PHE-induced contraction were tested by analyzing the cumulative concentration–response curves generated by PHE (0.1 nM to 10.0 μM) in aortic rings before and after incubation with the drugs. The maximal contraction (Emax) and the concentration inducing 50% of maximal contraction (EC50) for PHE were also determined through analysis of the concentration–response curves for each individual group.
Statistical analysis
Results are presented as the mean ± SEM using statistical software (GraphPad-Prism 5.03, GraphPad Software, Inc., San Diego, CA). Statistical comparisons between groups were performed using Student’s t test when comparing only two variables, and the analysis of variance (ANOVA) when comparing more than two groups. Student–Newman–Keuls test for post hoc analysis was used to further evaluate significant ANOVAs. Values were considered statistically significant at a P value less than 0.05.
Results
The general characteristics of the experimental animals are shown in Tables 1 and 2. Blood glucose levels in diabetic rats were higher than 400 mg/dl during the study period, ranging from 550.8 ± 20.3 mg/dl at 24 h following STZ administration to 526.8 ± 28.8 mg/dl after 4 weeks. In control animals, by contrast, glucose concentration remained within the normal range throughout the study, with a mean value of 135.7 ± 5.4 mg/dl. In addition, whereas body weight increased in both diabetic and control rats over the course of this study, it remained significantly lower in the diabetic rats at 4 weeks following diabetes induction (255.0 ± 11.3 g in diabetics vs. 341.5 ± 5.4 g in controls; n = 20, P < 0.05).
Effects of dantrolene and nimodipine on PHE-induced vascular contraction
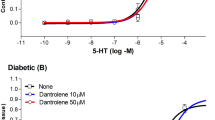
Cumulative concentration–response curves for the PHE-induced contraction of aortic rings are shown in Fig. 1a for control rats, and in Fig. 1b for STZ-diabetic rats. In non-diabetic controls, a 30-min incubation period with either 10 or 50 µM dantrolene increased EC50 value for PHE from 34.10 ± 10.10 nM, before incubation, to 122.20 ± 23.40 nM after incubation with 10 µM dantrolene (P < 0.05), and to 116.60 ± 23.16 nM with 50 µM dantrolene (P < 0.05; Fig. 1a, Table 3). In STZ-diabetic rats, EC50 value for PHE increased from 39.27 ± 7.33, before incubation, to 67.38 ± 9.74 nM after incubation with 10 µM dantrolene (P > 0.05; n = 5), and to 129.30 ± 23.83 nM after incubation with 50 µM dantrolene (P < 0.05; Fig. 1b, Table 3). Nimodipine (50 nM) alone reduced the PHE-induced contraction by 40% (P < 0.05; n = 9) in both non-diabetic control (Fig. 2a, Table 3) and diabetic (Fig. 2b, Table 3) rats. The addition of 10 µM dantrolene to nimodipine did not increase this relaxation, while the combination of nimodipine and 50 µM dantrolene reduced the PHE-induced contraction by about 80% (P < 0.05; n = 9) in both non-diabetic control (Fig. 2a, Table 3) and diabetic (Fig. 2b, Table 3) animals.
Cumulative concentration–response curves (from 0.1 nM to 10 µM) for the phenylephrine (PHE)-induced contraction of aortic rings of control (CT, a) and diabetic (STZ, b) rats. Rings were incubated for a 30-min period with 10 µM and 50 µM dantrolene. The values shown are the mean ± SEM of five to nine animals per group. *P < 0.05, when comparing with untreated aortic rings within the same group
Cumulative concentration–response curves (from 0.1 nM to 10 µM) for the phenylephrine (PHE)-induced contraction of aortic rings of control (CT, a) and diabetic (STZ, b) rats. Rings were incubated for a 30-min period with 10 µM dantrolene plus 50 nM nimodipine and with 50 µM dantrolene plus 50 nM nimodipine. The values shown are the mean ± SEM of six to nine animals per group. *P < 0.05, when compared with untreated rings within the same group. †P < 0.05, when comparing dantrolene 50 µM with dantrolene 10 µM-treated rings within the same group
Effects of dantrolene and nimodipine on ACh-induced relaxation
Figure 3 illustrates the effect of a 30-min incubation with 10 µM and 50 µM dantrolene on the ACh-induced relaxation in controls (Fig. 3a) and in STZ-diabetic rats (Fig. 3b). In controls, EC50, and Emax values for the ACh-induced relaxation were not affected by either concentration of dantrolene (Table 4). In diabetic rats, by contrast, endothelial function was significantly improved after incubation with the higher concentration of dantrolene, although no effect was observed with the lower concentration. With 50 µM dantrolene, the Emax values for the ACh-induced relaxation increased from 64.02 ± 3.01% before incubation to 95.71 ± 6.15% after dantrolene (n = 7, P < 0.05). EC50 values, however, remained unchanged (Fig. 3a, b, Table 4). The improvement in relaxation by 50 µM dantrolene was fully blocked by l-NAME, suggesting that it is NO dependent.
Cumulative concentration–response curves for the acetylcholine (ACh)-induced relaxation of aortic rings of control (CT, a) and diabetic (STZ, b) rats. Rings were incubated for a 30-min period with 10 µM and 50 µM dantrolene and pre-contracted with 0.1 µM phenylephrine (PHE) before the addition of cumulative concentrations of ACh. The values shown are the mean ± SEM of 5–11 animals per group. Note that the addition of 1 mM l-NAME to the incubation bath inhibited the ACh-induced relaxation of dantrolene-treated aortic rings of diabetic rats. *P < 0.05, when comparing with untreated rings within the same group. †P < 0.05, when comparing dantrolene 50 µM with dantrolene 10 µM-treated aortic rings within the same group
The addition of nimodipine to 10 µM or to 50 µM dantrolene does not affect endothelial-dependent relaxation in control rats (Fig. 4a, Table 4). In diabetic rats, however, an increase of approximately 50% in the ACh-induced relaxation was obtained with the combination of nimodipine and 50 µM dantrolene (n = 7, P < 0.05; Fig. 4b, Table 4). Nonetheless, this improvement was similar to that obtained with 50 µM dantrolene in the absence of nimodipine (Fig. 4b). The combination of nimodipine and 10 µM dantrolene did not modify EC50 or Emax values in either diabetic or non-diabetic control rats (Fig. 4a, b, Table 4).
Cumulative concentration–response curves for the acetylcholine (ACh)-induced relaxation of aortic rings of control (CT, a) and diabetic (STZ, b) rats. Rings were incubated for a 30-min period with 10 µM dantrolene plus 50 nM nimodipine and with 50 µM dantrolene plus 50 nM nimodipine, and pre-contracted with 0.1 µM phenylephrine (PHE) before the addition of cumulative concentrations of ACh. The values shown are the mean ± SEM of five to eight animals per group. Note that the addition of 1 mM l-NAME to the incubation bath inhibited the ACh-induced relaxation of dantrolene-treated aortic rings of diabetic rats. *P < 0.05, when compared with untreated rings within the same group. †P < 0.05, when comparing dantrolene 50 µM with dantrolene 10 µM-treated aortic rings within the same group
Effects of dantrolene and nimodipine on endothelial-independent relaxation
Figure 5 shows the effects of a 30-min incubation period with 10 µM dantrolene (Panel a), 50 µM dantrolene (Panel b), nimodipine, and both drugs in combination on the VSM relaxation elicited by 1.0 µM SNP in aortic rings of control and diabetic rats. The addition of SNP to aortic rings that were pre-contracted with 0.1 µM PHE produced similar endothelial-independent relaxation before and after incubation in both diabetics and controls, indicating that neither of these two drugs, alone or in combination, modified the endothelial-independent relaxation in diabetic or non-diabetic control rats.
Effects of a 30-min incubation period with 10 µM dantrolene alone or in combination with 50 nM nimodipine on the endothelial-independent relaxation of aortic rings of control and STZ-diabetic rats (a). Effects of a 30-min incubation period with 50 µM dantrolene alone or in combination with 50 nM nimodipine on the endothelial-independent relaxation of aortic rings of control and STZ-diabetic rats (b). Aortic rings were pre-contracted with 0.1 µM phenylephrine (PHE) before the addition of 1.0 µM sodium nitroprusside (SNP) to directly relax vascular smooth muscle. The values shown are the mean ± SEM of six to nine animals per group. Note that the drugs, either alone or in combination, did not modify endothelial-independent relaxation in control or STZ-diabetic rats
Discussion
Acute treatment of aortic rings with a high concentration (50 µM) of dantrolene, alone or in combination with nimodipine, proved to be effective in decreasing vascular hyperreactivity in the STZ-diabetic rats, a well-known animal model of type 1 diabetes [21]. Adverse secondary systemic effects are present, however, at high concentrations of dantrolene [2, 25, 29, 30]. Thus, we investigated whether a much lower concentration (10 µM) of this drug minimizes the adverse secondary effects, while at the same time reducing vascular hyperreactivity. We found that only the higher concentration of dantrolene significantly reduces vascular hyperreactivity in both diabetic and non-diabetic rats.
Previous reports in CVSP patients indicate that whereas a 1.25 mg/kg dose of dantrolene significantly decreases both peak systolic velocity (PSV) and mean flow velocity (MFV) in the middle cerebral artery, a higher dose of 2.5 mg/kg fails to significantly decrease these parameters [12]. Thus, the beneficial effects of dantrolene in reducing arterial vasoconstriction appear to be dose independent. Our findings, however, indicate that regardless of the animal glycemic status, the reduction of the PHE-induced contraction with dantrolene is dose dependent. Similarly, Salomon and colleagues [23], reported a reduction in the PHE-induced contractility in the femoral artery of non-diabetic rats after acute incubation with 100 µM dantrolene, but not after incubation with 10 µM and 30 µM of the drug.
That only the high concentration of dantrolene increases the EC50 values for the PHE-induced contraction suggests that the mechanisms underlying this beneficial effect involves alterations in the kinetics of the agonist–alpha1 receptor interaction, and that these alterations require that the drug surpasses a threshold concentration. Alternatively, because Ca+2 released upon activation of RyRs acts as a positive feedback mechanism for inositol 1,4,5-trisphosphate receptor response [31], dantrolene may interrupt this feedback and reduce the response of agonist-induced inositol 1,4,5-trisphosphate receptors by blocking RyR Ca+2 release. Additional studies are needed to evaluate either possibility.
Diabetes has been linked to endothelial dysfunction and to increased oxidative stress and vascular tone [5, 6, 28]. We reported previously that 50 µM dantrolene has antioxidant properties and increases significantly the endothelial-dependent relaxation in aortic rings of diabetic rats by an NO-dependent mechanism [21]. In the current work, however, we found that a low concentration of dantrolene alone, or in combination with nimodipine, fails to improve endothelial dysfunction in diabetic rats, suggesting that the antioxidant effect of the drug is also dose dependent. This dose dependence, may explain, at least in part, the mixed results reported for the antioxidant effects of the drug. While dantrolene treatment in rabbits results in a significant decrease in MDA levels in cerebrospinal fluid and augments endogenous antioxidant defenses after traumatic spinal cord injury [13], it fails to prevent the myocardial dysfunction in rats resulting from oxidative stress following intracranial hypertension [32]. In addition, genetic differences in animal strains, tissues and pharmacokinetic variability may also account for the variability in antioxidant effects of the drug.
We propose that the combined use of nimodipine and dantrolene may reduce the incidence and severity of CVSPs by simultaneously blocking Ca+2 entry through the L-type VDCC and Ca+2 release by RyR from the SR. It has been reported, however, that the constriction of resistance arteries due to increases in blood pressure is buffered by activation of Ca+2-sensitive potassium (BK) channels controlled by local RyR-mediated Ca+2 sparks [4, 33]. This mechanism is critical in the regulation of myogenic tone and requires the activation of cGMP-dependent protein kinase (PKG) by reactive oxygen species (ROS). Thus, oxidant-activated PKG is required to trigger Ca+2 sparks, BK channel activity, and vasodilation in response to pressure [33]. By acting as an antioxidant agent [13, 21, 22], dantrolene may block BK–RyR coupling, because the absence of oxidative activation of PKG disables the BK channel-mediated negative feedback regulation of vasoconstriction [33].
VSM has been suggested to be functionally impaired and to contribute to the increased incidence of macrovascular complications in diabetes [34]. Nonetheless, endothelial-independent relaxation with SNP is similar in diabetic and non-diabetic rats, suggesting that at least the cGMP-relaxing pathway is not affected by hyperglycemia at 4 weeks following diabetes induction. Moreover, neither dantrolene, nimodipine, nor their combination alters the relaxing responses of VSM to the NO-donor. It is possible, however, that functional abnormalities in VSM occur only at the latest stages of diabetes and are not present in the STZ-diabetic rats at the stage investigated.
One limitation of this study is that the effects of dantrolene and nimodipine were only evaluated in rings of the thoracic aorta (systemic artery), rather than in rings of the cerebral vasculature. These vascular beds differ anatomically and physiologically. Whereas the blood brain–barrier limits and regulates access of circulating hormones, ions, and catecholamines to brain structures, these substances have free access to VSM in systemic vessels. Cerebral vessels also have less smooth muscle and adventitia than systemic vessels [35]. In addition, because autoregulation is present in the cerebral microcirculation due to the myogenic mechanisms, cerebral blood flow is independent of cerebral perfusion pressure, being instead regulated largely by changes in cerebral arterial resistance [36]. Owing to the thinner layer of vascular smooth muscle and lower intravascular pressure, the intracranial vessels have less vasoconstrictor capacity than systemic vessels. Thus, extrapolating the effects of dantrolene to the cerebral vasculature should be done with caution. Nevertheless, our finding that the reduction in aortic vascular contractility in diabetic and non-diabetic rats is similar in extent to that reported for the femoral artery of control rats [23] suggests that the effects of the drug are similar in different vascular beds. Furthermore, this possibility is supported by previous reports, which indicate that RyR1, RyR2, and RyR3 subtypes are present not only in the thoracic aorta [16] and the mesenteric arteries [14], but also in the large cerebral arteries [17] and the cerebral microcirculation [4]. Thus, the results of the current study may offer the first step in developing a targeted and more efficient therapy for reducing CVSPs in diabetics. Future experiments, however, such as measuring blood flow velocities in the middle cerebral artery of diabetic rats, are needed to evaluate the effects of dantrolene on the cerebral circulation and further validate the relevance of our results with the aorta to cranial vasculature.
Conclusion
The current study may contribute valuable information regarding new pharmacological approaches aimed at reducing CVSPs, especially in the diabetic population. Careful titration, however, should be performed when adding dantrolene to CCBs to achieve a significant reduction in vascular hyperreactivity. Furthermore, if our findings with rats are applicable to humans, the combined use of dantrolene and nimodipine at optimal doses may be effective in reducing CVSPs, particularly in the diabetic population.
References
Hill MD. Stroke and diabetes mellitus. Handb Clin Neurol. 2014;126:167–74.
Dumont T, Rughani A, Silver J, Tranmer BI. Diabetes mellitus increases risk of vasospasm following aneurysmal subarachnoid hemorrhage independent of glycemic control. Neurocrit Care. 2009;11:183–9.
Navedo MF, Takeda Y, Nieves-Cintrón M, Molkentin JD, Santana LF. Elevated Ca2+ sparklet activity during acute hyperglycemia and diabetes in cerebral arterial smooth muscle cells. Am J Physiol Cell Physio. 2010;298:C211–20.
Dabertrand F, Nelson MT, Brayden JE. Ryanodine receptors, calcium signaling, and regulation of vascular tone in the cerebral parenchymal microcirculation. Microcirculation. 2013;20:307–16.
Giacco F, Brownlee M. Oxidative stress and diabetic complications. Circ Res. 2010;107:1058–70.
Potenza MA, Gagliardi S, Nacci C, Carratu’ MR, Montagnani M. Endothelial dysfunction in diabetes: from mechanisms to therapeutic targets. Curr Med Chem. 2009;16:94–112.
Hadi HA, Suwaidi JA. Endothelial dysfunction in diabetes mellitus. Vasc Health Risk Manag. 2007;3:853–76.
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39:44–84.
Crespo MJ, Quigley J. Simvastatin, atorvastatin, and pravastatin equally improve the hemodynamic status of diabetic rats. World J Diabetes. 2015;6:1168–78.
Santos KG, Crispim D, Canani LH, Ferrugem PT, Gross JL, Roisenberg I. Relationship of endothelial nitric oxide synthase (eNOS) gene polymorphisms with diabetic retinopathy in Caucasians with type 2 diabetes. Ophthalmic Genet. 2012;33:23–7.
Biessels GJ, ter Laak MP, Hamers FP, Gispen WH. Neuronal Ca2+ disregulation in diabetes mellitus. Eur J Pharmacol. 2002;447:201–9.
Muehlschlegel S, Rordorf G, Sims J. Effects of a single dose of dantrolene in patients with cerebral vasospasm after subarachnoid hemorrhage: a prospective pilot study. Stroke. 2011;42:1301–6.
Aslan A, Cemek M, Buyukokuroglu ME, Altunbas K, Bas O, Yurumez Y, et al. Dantrolene can reduce secondary damage after spinal cord injury. Eur Spine J. 2009;18:1442–51.
Neylon CB, Richards SM, Larsen MA, Agrotis A, Bobik A. Multiple types of ryanodine receptor/Ca2 + release channels are expressed in vascular smooth muscle. Biochem Biophys Res Commun. 1995;21:814–21.
Fruen BR, Mickelson JR, Louis CF. Dantrolene inhibition of sarcoplasmic reticulum Ca2+ release by direct and specific action at skeletal muscle ryanodine receptors. J Biol Chem. 1997;272(43):26965–71.
Tykocki NR, Thompson JM, Jackson WF, Watts SW. Ryanodine receptors are uncoupled from contraction in rat vena cava. Cell Calcium. 2013;53:112–9.
Vaithianathan T, Narayanan D, Asuncion-Chin MT, Jeyakumar LH, Liu J, Fleischer S, et al. Subtype identification and functional characterization of ryanodine receptors in rat cerebral artery myocytes. Am J Physiol Cell Physiol. 2010;299:C264–78.
Roden DM, Knollmann BC. Dantrolene: from better bacon to a treatment for ventricular fibrillation. Circulation. 2014;129:834–6.
Zhao F, Li P, Chen SR, Louis CF, Fruen BR. Dantrolene inhibition of ryanodine receptor Ca2+ release channels. Molecular mechanism and isoform selectivity. J Biol Chem. 2001;276:13810–6.
Ucuncu H, Taysi S, Aktan B, Buyukokuroglu ME, Elmastas M. Effect of dantrolene on lipid peroxidation, glutathione and glutathione-dependent enzyme activities in experimental otitis media with effusion in guinea pigs. Hum Exp Toxicol. 2005;24:567–71.
Crespo MJ, Roman M, Matias J, Morales M, Torres H, Quidgley J. Synergistic effects of dantrolene and nimodipine on the phenylephrine-induced contraction and ACh-induced relaxation in aortic rings from diabetic rats. Int J Endocrinol 2018:9790303.
Torres BB, Caldeira FM, Gomes MG, Serakides R, de Marco Viott A, Bertagnolli AC, et al. Effects of dantrolene on apoptosis and immunohistochemical expression of NeuN in the spinal cord after traumatic injury in rats. Int J Exp Pathol. 2010;91:530–6.
Salomone S, Soydan G, Moskowitz MA, Sims JR. Inhibition of cerebral vasoconstriction by dantrolene and nimodipine. Neurocrit Care. 2009;10:93–102.
Muehlschlegel S, Rordorf G, Bodock M, Sims JR. Dantrolene mediates vasorelaxation in cerebral vasoconstriction: a case series. Neurocrit Care. 2009;10:116–21.
Muehlschlegel S, Carandang R, Hall W, Kini N, Izzy S, Garland B, et al. Dantrolene for cerebral vasospasm after subarachnoid haemorrhage: a randomised double blind placebo-controlled safety trial. J Neurol Neurosurg Psychiatry. 2015;86:1029–35.
Byron KL, Taylor CW. Spontaneous Ca2+ spiking in a vascular smooth muscle cell line is independent of the release of intracellular Ca2+ stores. J Biol Chem. 1993;268:6945–52.
Ru XC, Qian LB, Gao Q, Li YF, Bruce IC, Xia Q. Alcohol induces relaxation of rat thoracic aorta and mesenteric arterial bed. Alcohol. 2008;43:537–43.
Quidgley J, Cruz N, Crespo MJ. Atorvastatin improves systolic function, but does not prevent the development of dilated cardiomyopathy in streptozotocin-induced diabetic rats. Ther Adv Cardiovasc Dis. 2014;8:133–44.
Flewellen EH, Nelson TE, Jones WP, Arens JF, Wagner DL. Dantrolene dose response in awake man: implications for management of malignant hyperthermia. Anesthesiology. 1983;59(4):275–80.
Fraser JF, Stieg PE. Hyponatremia in the neurosurgical patient: epidemiology, pathophysiology, diagnosis, and management. Neurosurgery. 2006;59:222–9.
Pierobon N, Renard-Rooney DC, Gaspers LD, Thomas AP. Ryanodine receptors in liver. J Biol Chem. 2006;281:34086–95.
Hall SR, Wang L, Milne B, Hong M. Mannitol but not dantrolene prevents myocardial dysfunction following intra-cranial hypertension in rats. Am J Transpl. 2005;5:2862–9.
Khavandi K, Baylie RA, Sugden SA, Ahmed M, Csato V, Eaton P, et al. Pressure-induced oxidative activation of PKG enables vasoregulation by Ca2+ sparks and BK channels. Sci Signal. 2016;9(449):100. https://doi.org/10.1126/scisignal.aaf6625.
Li T, Yang GM, Zhu Y, et al. Diabetes and hyperlipidemia induce dysfunction of VSMCs: contribution of the metabolic inflammation/miRNA pathway. Am J Physiol Endocrinol Metab. 2015;308:E257–69.
Heistad DD. What’s new in the cerebral microcirculation? Landis Award lecture. Microcirculation. 2001;8(6):365–75.
Wahl M, Schilling L. Regulation of cerebral blood flow–a brief review. Acta Neurochir Suppl (Wien). 1993;59:3–10.
Acknowledgements
The authors would like to recognize the assistance of Dr. Donald C. Dunbar for editing the manuscript. This work was supported by Grants from the National Institute of Health (NIGMS-RISE Grant R25GM061838), the NIMHD-CCRHD-RCMI Program (U54-MD007600), and the Anesthesiology Department of the University of Puerto Rico-School of Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Román, M., Ramírez, J.M., Morales, M. et al. Significant reduction of vascular reactivity with dantrolene and nimodipine in diabetic rats: a potential approach to cerebral vasospasm management in diabetes. Pharmacol. Rep 72, 126–134 (2020). https://doi.org/10.1007/s43440-019-00038-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-019-00038-5