Abstract
Purpose
To analyze the angiographic and clinical results of transarterial embolization with Onyx (Medtronic-Covidien, Irvine, CA) in dural arteriovenous fistulas (DAVFs) partially fed by arteries arising from the carotid siphon or the vertebral arteries.
Methods
We isolated 40 DAVFs supplied by either the tentorial artery of the internal carotid artery (ICA) or the posterior meningeal artery of the vertebral artery. These DAVFs were embolized with Onyx through the middle meningeal artery or the occipital artery. We reviewed the occurrence of reflux into the arteries of carotid or vertebral origin.
Results
In all the cases, reflux occurred into the first millimeters of the DAVF arterial feeders arising from carotid or vertebral arteries but slowly enough to be controlled by interruption of Onyx injection. Reflux was always minimal and Onyx never reached the ostium of the arteries. No cerebral ischemic complications occurred in our series.
Conclusion
The behavior of Onyx is clearly different from that of cyanoacrylate glue, resulting in superior control during injection. Reflux into arteries arising from the ICA or vertebral artery during DAVF treatment always carries a risk of unintentional non-target embolization of normal cerebral vasculature but Onyx appears to be safe in this situation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of Onyx (Medtronic-Covidien, Irvine, CA) injection through an arterial approach for the treatment of intracranial dural arteriovenous fistulas (DAVFs) is a well-established technique at many institutions and has yielded very favorable results [1,2,3]. Recent reports in the literature have demonstrated that endovascular embolization with Onyx injection may offer a number of advantages over the use of cyanoacrylates, including greater control during injection of the embolization agent, longer injection times, favorable angiographic obliteration and cure rates, fewer complications related to microcatheter removal, and fewer overall complications [1, 4]. In addition to these advantages, we believe that, in cases of DAVFs with feeding arterial vessels arising from the internal carotid or vertebrobasilar system, which are especially dangerous, the use of Onyx provides greater control over migration of the embolic agent, thus preventing serious complications [5].
This report describes our results with embolization of DAVFs with contribution of arterial branches of the internal carotid or vertebrobasilar system and demonstrates that Onyx injection is both safe and effective.
Methods
Patients
Between January 2005 and January 2015, the Division of Interventional Neuroradiology at the Lariboisière Hospital in Paris, France, performed 94 endovascular procedures for the treatment of 90 intracranial DAVFs diagnosed in 87 patients. All fistulas were treated via the endovascular route, with an initial arterial approach and Onyx as the embolic agent. From this series, we isolated 40 cases of skull-base DAVFs fed partially by arterial branches arising from the internal carotid artery (ICA) or posterior meningeal artery from the vertebral artery (VA). This subsample comprised 16 women and 24 men, with a mean age of 58 years (range, 36–86 years).
All procedures were performed using digital subtraction angiography (DSA) on an AXIOM Artis dBC biplane flat-detector system (Siemens Medical, Erlangen, Germany) or single-plane Advantx LCV (GE Healthcare Systems, Milwaukee, WI, USA).
Clinical Presentation and DAVF Classification
The most common initial clinical presentation was hemorrhage (n = 15), followed by pulsatile tinnitus (n = 10) and seizure (n = 7). Three patients presented with neuralgia, and five cases were detected incidentally. After DSA, the DAVFs were classified as per the Lariboisière Hospital classification [6].
Treatment and Follow-Up
The treatment protocol established at the Division of Interventional Neuroradiology at the Lariboisière Hospital in Paris, France, was followed [4]. All treatment procedures were performed with the patient under general anesthesia and double femoral access, with the first catheter devoted to the external carotid artery (ECA) and the second to secure control of the ICA or vertebral artery during Onyx injection. An intravenous bolus of heparin (3000 IU) was administered at the start of each procedure. A 6 or 5‑Fr guiding catheter was then advanced to the proximal portion of the ECA and perfused with 3 mg/l nimodipine in normal saline. Selective catheterization was performed using dimethyl sulfoxide (DMSO)-compatible microcatheters to perform Onyx embolization. The identification of optimal working projections is one of the most important steps of DAVF treatment. The projections need to differentiate the venous collection system from the feeding arterial branches, and correct visualization of the venous sinus and cortical draining vein systems is critical. Adequate visualization of the ICA and/or VA feeders is also important to avoid excessive reflux into these vessels. Interval follow-up DSA was performed in all patients 1–6 months after embolization. All patients were also evaluated clinically.
Results
The majority of the DAVFs treated (38 out of 40, Table 1) had high-grade features involving either reflux into cortical veins (grade IIB) or direct drainage into cortical veins (grades III, IV or V).
In 92.5% of cases (n = 37), no significant residual shunts were observed after Onyx embolization. In 30 DAVFs, a single microcatheterization was required for treatment (Figs. 1, 2 and 3). The remaining lesions required a second microcatheterization in six instances (n = 5), and two fistulas required a third microcatheter placement for treatment completion. A significant residual shunt was observed in three patients. In two of these, treatment was completed by transvenous access and embolization with coil placement (one during the same procedure) and one was treated by conventional surgery (Table 2).
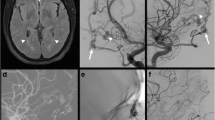
Lateral external (a) and internal (b) carotid artery injection in the early phase, showing a high-flow type IV DAVF of the foramen magnum with cortical venous aneurysm fed by meningeal branches from the occipital artery and internal carotid. Cast of Onyx (c) after embolization through the occipital artery, showing arterial reflux without reaching the internal carotid. Final lateral internal carotid artery injection shows complete occlusion of the DAVF (d)
Lateral external carotid artery injection (a) and anterior vertebral (b) artery injection in the early phase (a), showing a type III tentorial DAVF fed by meningeal branches from the middle and posterior meningeal arteries. Note the posterior meningeal arising from the vertebral artery. Cast of Onyx (c) after embolization through the occipital artery showing reflux to the posterior meningeal artery, without reaching the internal carotid. Reflux was safely controlled. Final anterior vertebral artery injection shows complete occlusion of the DAVF (d)
Lateral internal (a) and external (b) carotid artery injection in the early phase, showing a type IIa sigmoid DAVF fed by meningeal branches from the middle meningeal artery and meningohypophyseal trunk (thin arrow). The asterisks demonstrate early flow to the lateral sinus. Lateral view of initial steps of Onyx injection from the middle meningeal artery (c), showing reflux to the petrosal branch of the middle meningeal artery (black arrow). Cast of Onyx (d) after embolization through the middle meningeal artery, showing reflux to the petrosal branch (black arrow). Final lateral internal carotid artery injection shows complete occlusion of the DAVF (e). Axial Maximum intensity projection (MIP) reconstruction of CT images (f) demonstrates reflux to the meningeal petrosal branch (black arrow). This patient developed facial paresis, which gradually resolved over the clinical follow-up period
A total of 51 arterial pedicles were catheterized. The middle meningeal artery (MMA) was the main artery branch targeted (n = 39), followed by the occipital artery (OA) (n = 12). The average time of Onyx injection was 30 min (range, 15–60 min), and the average volume injected per pedicle was 2.5 ml (range, 0.6–6.5 ml). During all procedures, Onyx reflux occurred up to the first few millimeters of different DAVF feeding arteries, but was slow enough to be controlled by interruption of injection. This reflux was always minimal and Onyx never reached the vertebral or internal carotid arteries. No cerebral ischemic complications occurred in this series. We observed early complications related to cranial neuropathy in three patients: two had facial paresis and one had neuropathic pain in the distribution area of the trigeminal nerve. These symptoms gradually resolved over the clinical follow-up period.
Discussion
The embolization of DAVFs through an arterial approach has, for many years, been reserved as a last resort, used only when venous embolization was not feasible or conventional surgery was not possible. Part of the problem was that the embolic materials available until recently were poorly suited to arterial approaches. In the early 2000s, the introduction of Onyx, an embolic material with significantly improved handling characteristics, revolutionized possibilities for this technique [5]. In 2006, Rezende et al. first reported DAVF closure with Onyx in a patient with a lesser sphenoid wing region fistula with direct cortical venous drainage [2]. Few other case reports and series have been published since then [3, 7, 8].
Increasing experience with this technique has resulted in the successful primary treatment of many DAVFs using Onyx, with reported occlusion rates ranging from 62.5% to 100% [1,2,3,4,5, 9]. In our series, we had a 92.5% occlusion rate with Onyx injection. Most fistulas were treated with injection of a single pedicle, preferably by the meningeal artery, followed by meningeal branches from the occipital artery. Of the three fistulas that could not be approached transarterially, two were successfully finalized by venous access and coil placement and the other was treated by conventional surgery. It is noteworthy that our success rate was higher than in our previous publication [4], in which we described treatment of our first cases and that we included fistulas without a dangerous supply. This is probably attributable to the learning curve. Even fewer published series have compared Onyx to other methods. Rabinov et al. found significantly higher efficacy with Onyx compared with n‑Butyl Cyanoacrylate (n -BCA) in a series of 56 DAVFs. Patients embolized with Onyx underwent surgery less frequently compared with those treated with n -BCA [10]. More recently, in 2016, Choo and Shankar compared the outcome of DAVF treated by an endovascular approach with Onyx arterial embolization versus n -BCA and coil embolization. The odds of not requiring post-embolization surgery were significantly higher in the Onyx group (81.8% vs. 22.2%), and the complication rate tended to be lower with Onyx (9.1%) than with n -BCA (22.22%) [11]. In a series of 170 DAVFs treated by different endovascular modalities, Baltsavias and Valavanis reported that in 49 patients treated only with cyanoacrylate by an arterial approach, only 1 had emboli to the middle cerebral artery during arterial embolization by a meningeal branch. The number of patients with feeding branches arising from ICA or VA was not reported. The authors reported that the event occurred through migration of collateral circulation to the ICA. In this case, the patient had a severe infarction in the MCA territory [12]. Kim et al. also described a migratory event with cyanoacrylate, this time during vertebral artery embolization of the occipital artery. At the end of the procedure, the vertebral artery was sacrificed by coil embolization, with no clinical impact on the patient [13]. In these situations, we believe the flow characteristics of Onyx provide greater control. The behavior of injected glue is sometimes unpredictable, and glue embolization carries a risk of embolic migration to the ICA and VA or cortical veins [14]. Onyx has the characteristics of a gelling solution, formulated as a polymer suspended in a solvent. On injection into an artery, the volatile carrier diffuses away within the arterial blood flow and the polymer is deposited within the artery. In practice, the progression of this deposition process can be controlled very accurately [15]. By interrupting injection, the operator can actually redirect the embolus away from its original course. Thus, Onyx provides the ability to control the DAVF embolization process with greater accuracy. By capitalizing on this property of Onyx, DAVFs with multiple arterial supplies can be embolized, by allowing the embolic material to diffuse into the feeding arteries in a controlled fashion before it can affect the draining venous system.
We found that the availability of a posterior branch of the MMA is critical to the success of Onyx embolization for tentorial DAVFs. The posterior branch of the MMA is a relatively straight vessel and is often enlarged when feeding a DAVF. These characteristics enable distal catheterization adjacent to the point of the fistula, unlike in other common feeders, such as the OA, which is often excessively tortuous making distal catheterization difficult if not impossible. Conversely, the size of the dorsal branches of the MMA is not a limiting factor as long as the catheter can be navigated into the branch; therefore, although this branch may be very small and appear to play no role in feeding the artery, this approach can still be worth trying [4].
Distal catheterization almost in a wedge position enables forward progression of the embolic material, while limiting reflux to a minimum. When embolizing from the posterior MMA branch it is critical to avoid reflux, which should not be allowed in the proximity to the level of the foramen spinosum to avoid inadvertent compromise of the arterial supply to the trigeminal and facial nerves [5]. More recently, dual lumen balloon microcatheters have become available that allow unopposed forward penetration of Onyx without the time-consuming effort of plug formation, while concurrently decreasing the risk of premature proximal reflux [16].
In 2014 Chapot et al. described a technique for permanent control of reflux called the pressure cooker technique (PCT) [17]. Although this technique allows definitive control of reflux, it has some drawbacks. Its potential dangers are basically related to the need for simultaneous positioning of two microcatheters in the feeding artery, with subsequent greater manipulation. A modified PCT was also described in 2016, using double microcatheterization with a detachable catheter tip and a second microcatheter to enable application of glue on the fragile portion of the first microcatheter [18].
The OA has been reported to be a poor option for the embolization of DAVFs. Arterial feeders from the OA are transosseous, resulting in poor flow control and Onyx penetration into the shunt. The use of a dual lumen balloon catheter with injection of Onyx through the OA may help overcome this limitation by increasing proximal resistance and enhancing distal penetration; however, navigation and especially inflation of this type of balloon catheter in such a small artery might be associated with a significant risk of complications, including vessel rupture [16, 19]. In our series, we had no embolic complications related to inadvertent migration of the embolic agent into the internal carotid or vertebrobasilar system. This is probably due to the nature of the Onyx product. It should be noted that in all cases in our series, we established bilateral femoral access and placed a second catheter in the internal carotid or vertebral artery system to perform control angiography and monitor for dangerous reflux. The reflux reached close proximity to the ostium of the carotid/vertebral feeding branch in some cases, but never entered the parent artery. Another important technical consideration is that we do not use intraluminal balloons to protect the parent artery.
In our series, complications were observed in three patients. All were related to cranial nerve injury (two with facial palsy and one with trigeminal neuralgia), and all had resolved partially or completely at the last clinical follow-up. These complications can be attributed to excessive reflux of Onyx in the middle meningeal artery up to the foramen spinosum or excessive retrograde diffusion of Onyx into other arterial feeders, which may have induced occlusion of the vasa nervorum and subsequent cranial nerve injury [4]. Other complications reported in the literature, such as Onyx migration into the heart and pulmonary arteries, venous infarction and hemorrhage [9, 20, 21], were not observed in our series. Although some authors have described rare recurrences of DAVF in patients treated with Onyx [21], we had no recurrence in our series. We always aimed for total closure of the arteriovenous shunt, knowing that fistulas partially treated with arterial Onyx injection rarely progress to total occlusion, unlike DAVFs treated with cyanoacrylate [13, 14, 22].
In conclusion, the material properties of Onyx are clearly different from those of cyanoacrylate glue, resulting in superior control during injection. As reflux into arteries arising from the carotid siphon or vertebral artery during DAVF treatment carries a risk of unintended non-target embolization into normal cerebral arteries, Onyx appears to be safe in this situation.
References
Cognard C, Januel AC, Silva NA Jr, Tall P. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: new management using Onyx. AJNR Am J Neuroradiol. 2008;29:235–41.
Rezende MT, Piotin M, Mounayer C, Spelle L, Abud DG, Moret J. Dural arteriovenous fistula of the lesser sphenoid wing region treated with Onyx: technical note. Neuroradiology. 2006;48:130–4.
Trivelato FP, Abud DG, Ulhôa AC, Menezes Tde J, Abud TG, Nakiri GS, Colli BO, Gusmão SN, Rezende MT (2010) Dural arteriovenous fistulas with direct cortical venous drainage treated with onyx: a case series. Arq Neuropsiquiatr 68:613–618
Abud TG, Nguyen A, Saint-Maurice JP, Abud DG, Bresson D, Chiumarulo L, Enesi E, Houdart E. The use of Onyx in different types of intracranial dural arteriovenous fistula. AJNR Am J Neuroradiol. 2011;32:2185–91.
Puffer RC, Daniels DJ, Kallmes DF, Cloft HJ, Lanzino G. Curative Onyx embolization of tentorial dural arteriovenous fistulas. Neurosurg Focus. 2012;32:E4.
Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, Chiras J, Merland JJ. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995;194:671–80.
Macdonald JH, Millar JS, Barker CS. Endovascular treatment of cranial dural arteriovenous fistulae: a single-centre, 14-year experience and the impact of Onyx on local practise. Neuroradiology. 2010;52:387–95.
Lee B, Mehta VA, Amar AP, Tenser MS, Mack WJ. Transarterial embolization of an anterior fossa cranial base dural arteriovenous fistula. Neurosurg Focus. 2014;37:1.
Lv X, Jiang C, Zhang J, Li Y, Wu Z. Complications related to percutaneous transarterial embolization of intracranial dural arteriovenous fistulas in 40 patients. AJNR Am J Neuroradiol. 2009;30:462–8.
Rabinov JD, Yoo AJ, Ogilvy CS, Carter BS, Hirsch JA. Onyx versus n‑BCA for embolization of cranial dural arteriovenous fistulas. J Neurointerv Surg. 2013;5:306–10.
Choo DM, Shankar JJ. Onyx versus nBCA and coils in the treatment of intracranial dural arteriovenous fistulas. Interv Neuroradiol. 2016;22:212–6.
Baltsavias G, Valavanis A. Endovascular treatment of 170 consecutive cranial dural arteriovenous fistulae: results and complications. Neurosurg Rev. 2014;37:63–71.
Kim DJ, Willinsky RA, Krings T, Agid R, Terbrugge K. Intracranial dural arteriovenous shunts: transarterial glue embolization-experience in 115 consecutive patients. Radiology. 2011;258:554–61.
Miyamoto N, Naito I, Shimizu T, Yoshimoto Y. Efficacy and limitations of transarterial acrylic glue embolization for intracranial dural arteriovenous fistulas. Neurol Med Chir (Tokyo). 2015;55:163–72.
Tekle WG, Grigoryan M, Tummala RP. Marginal sinus fistula supplied exclusively by vertebral artery feeders. J Vasc Interv Neurol. 2013;6:30–3.
Kim ST, Jeong HW, Seo J. Onyx embolization of dural arteriovenous fistula, using scepter C balloon catheter: a case report. Neurointervention. 2013;8:110–4.
Chapot R, Stracke P, Velasco A, Nordmeyer H, Heddier M, Stauder M, Schooss P, Mosimann PJ. The pressure cooker technique for the treatment of brain AVMs. J Neuroradiol. 2014;41:87–91.
Abud DG, de Castro-Afonso LH, Nakiri GS, Monsignore LM, Colli BO (2016) Modified pressure cooker technique: an easier way to control onyx reflux. J Neuroradiol 43(3):218–222
Gabrieli J, Clarencon F, Di Maria F, Chiras J, Sourour N (2015) Occipital artery: a not so poor artery for the embolization of lateral sinus dural arteriovenous fistulas with onyx. J Neurointerv Surg 9(e1):e8–e9.
Natarajan SK, Ghodke B, Kim LJ, Hallam DK, Britz GW, Sekhar LN. Multimodality treatment of intracranial dural arteriovenous fistulas in the Onyx era: a single center experience. World Neurosurg. 2010;73:365–79.
Adamczyk P, Amar AP, Mack WJ, Larsen DW. Recurrence of “cured” dural arteriovenous fistulas after Onyx embolization. Neurosurg Focus. 2012;32:E12.
Guedin P, Gaillard S, Boulin A, Condette-Auliac S, Bourdain F, Guieu S, Dupuy M, Rodesch G. Therapeutic management of intracranial dural arteriovenous shunts with leptomeningeal venous drainage: report of 53 consecutive patients with emphasis on transarterial embolization with acrylic glue. J Neurosurg. 2010;112:603–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T.G. Abud, E. Houdart, J.-P. Saint-Maurice, D.G. Abud, C.E. Baccin, A.D. Nguyen and N. Abdala declare that they have no competing interests.Please confirm or correct the statement on the conflict of interest.
Ethical standards
This study was approved by the research ethics committee of Universidade Federal de São Paulo (UNIFESP), registration number 0534/2016, protocol number 1.550.934. Informed consent was obtained from all patients. All procedures were in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Contributors
Thiago G. Abud: analysis and interpretation of cases, writing the article, figure editing.
Emmanuel Houdart: execution of the procedures and clinical follow-up.
Jean-Pierre Saint-Maurice: execution of the procedures and clinical follow-up.
Daniel G. Abud: analysis and interpretation of cases.
Carlos E. Baccin: writing the article.
Andrew D. Nguyen: writing the article.
Nitamar Abdala: supervision and critical revision of the article.
All authors have approved the final version.
Rights and permissions
About this article
Cite this article
Abud, T.G., Houdart, E., Saint-Maurice, JP. et al. Safety of Onyx Transarterial Embolization of Skull Base Dural Arteriovenous Fistulas from Meningeal Branches of the External Carotids also Fed by Meningeal Branches of Internal Carotid or Vertebral Arteries. Clin Neuroradiol 28, 579–584 (2018). https://doi.org/10.1007/s00062-017-0615-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-017-0615-7