Abstract
This study aims to evaluate a single-center experience with endovascular treatment of cranial dural arterievenous fistulae (CDAVF). The clinical and radiological records of 170 consecutive patients harboring a CDAVF and treated endovascularly in a 16-year period were reviewed. A variety of data related to demographics, features of the lesion, treatment, outcome, and follow-up were analyzed with emphasis to the results and complications. Half of the lesions had cortical venous drainage (CVD) in the initial angiographic investigation, whereas 26 % had exclusively CVD. Sixty-seven percent of our patients presented with benign symptoms and 33 % with aggressive symptoms. In 60.5 % of the patients with benign lesion (without CVD), an anatomic cure in the immediate postinterventional angiogram without complication or permanent morbidity was achieved, whereas 69 % of the patients with aggressive lesions (with CVD) had an anatomic cure in the postinterventional final angiogram with all permanent-morbidity cases belonging to this group. The average of endovascular operation sessions per patient was 1.2. In a mean follow-up period of 2.8 years, the overall complete occlusion rate was 85.5 % (78 % for the benign group and 89.5 % for the aggressive group) and clinical cure and/or improvement rate of 93 %. The operative mortality was zero, and permanent neurologic morbidity was 2.3 %. In 73 % of our cases, N-butyl cyanoacrylate (NBCA) was used as the only or main embolic material. Endovascular embolization is the treatment of choice for CDAVF. High rates of good anatomical and clinical results, associated with very low operative complication rate can be achieved with few embolization sessions. Although mastering of a permanent embolic material is important, the therapeutic strategy should be individulized and not material based.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Embolization for the treatment of cranial dural arteriovenous fistulae (CDAVF) was developed as an alternative to open surgical approach and soon appeared as a more attractive treatment mainly due to less invasiveness.
Still many aspects regarding etio-pathogenesis, pathophysiology, natural history of CDAVF, as well as treatment strategies, effectiveness of endovascular approach, acceptable rate of complications, and embolic materials need exploration, better understanding, and answers based on real evidence.
Aiming to contribute mainly in aspects related to the treatment, we studied retrospectively patients treated in our Institution during the last 16 years.
Patients and methods
This series includes 173 consecutive adult patients who were evaluated and treated at our institution by the senior author (AV) in a 16-year period between January 1995 and December 2010. Six patients of this series were treated by the first author (GB), after joining the department in 2009. Patients treated before 1995 were excluded because of difficulties to collect complete data. A retrospective analysis of medical files and angiographic and MR/CT imaging studies was undertaken. The last 10 patients were studied prospectively. The angiographic images and/or videos of 39 patients could not be accessed; therefore the data for these patients were collected from the history chart, interventional report, and CT-MR imaging.
There were 75 women and 98 men. Their age ranged from 22 to 82 years, with a mean age of 56.3 years.
The interval from initial presentation of symptoms to treatment was recorded in 78 patients and varied from 1 week to 10 years, with a mean interval of 10.8 months.
Factors that could be considered as predisposing were recorded in 19 patients (11 %). History of head surgery related to the location of the fistula was reported in six patients, severe upper respiratory infection in three patients, documented sinus thrombosis in one patient, and incompletely embolized pial arteriovenous fistula in one patient. In eight cases, a history of severe head injury was recorded.
We described as aggressive symptoms those related to either focal or global neurological disturbance (paresis, aphasia, ataxia, seizures, etc.) attributed to a hemorrhagic or nonhemorrhagic central nervous system (CNS) disorder. We described as benign symptoms those related to local factors outside or not directly related to the CNS, such as venous congestion in the orbit with or without cranial nerve deficit, tinnitus, headache, etc. [13].
Presentation with benign symptoms was recorded in 116 patients (67 %), including 2 patients with incidentally discovered lesions, whereas 57 patients (33 %) presented with aggressive symptoms. Fourteen patients (8 %) had extensive and complex lesions with the majority (12 patients) of these having multiple lesions. Five more patients had bilateral lesions.
The clinical presentation appears in Table 1.
All procedures were performed on a biplane angiographic unit. Percutaneous femoral artery catheterization was used to achieve access in all patients. Patients were not systematically heparinized. Standard coaxial techniques were used. The “Valavanis” 5F catheter (Cook Medical Inc., Bloomington, IN, USA) was constantly used as both angiographic and guiding catheter. Microcatheter Elite 1.5F (Stryker Neurovascular, Fremont, CA, USA) was used in all cases over a soft microwire, preferably Mizzen (Boston Scientific) and lately Mirage (ev3 Neurovascular, Irvine, CA, USA). Balloon assistance was employed for distal protection during polyvinyl alcohol (PVA) injection for very small feeders.
Fifteen patients were treated under neuroleptic anaesthesia. All other embolizations were undertaken under general endotracheal anaesthesia.
Results
Classification
Classification of CDAVF according to location is sometimes a very difficult task especially in complex and extensive lesions, which often extend to a certain length along adjacent dural sinuses and structures with morphologically undistinguishable borders. In such lesions, the definition of multiplicity may be also questionable. In order to preserve accuracy, we list our cases according to the exact location avoiding round groups, but still divided in two tables, one with more ordinary locations (Table 2) and the second with complex topography (Table 3).
The classifications according to the venous drainage by Borden et al. [3] and Cognard et al. [7] have been validated as the best predictors of clinical behavior of a CDAVF and were used as the main criterion for therapeutic decision making. Eighty-seven patients (50 %) presented CVD in the initial angiographic investigation, whereas 45 (26 %) of the whole population had exclusively CVD.
The type of venous drainage according to the above classiffications is summarized in Table 4.
As proposed by Geibprasert et al. [13], the craniospinal epidural spaces can be categorized into three different compartments related to their specific drainage role of the bone and central nervous system, the ventral epidural (VE), dorsal epidural (DE), and lateral epidural (LE) groups. In 60 patients, the CDAVF was allocated in the VE group, in 44 patients in the DE group, and in 41 patients in the LE group. Twenty-three patients had a fistula extending into both VE and DE spaces, five patients in both DE and LE.
Management
Three of the patients of this series were treated conservatively with manual carotid compression. All three lesions were located in the cavernous sinus and had small supply and slow flow. After this treatment, two patients were asymptomatic and one improved. The remaining 170 patients were treated with embolization. Curative embolization was the strategy for the vast majority of the patients. Palliative or targeted endovascular treatment was reserved for patients with very extensive lesions without a chance of complete eradication by either embolization or surgery.
Combined treatment with surgery was applied in two cases. In one case of a very extensive shunt and after failure of palliative treatment to control the patient’s symptoms, a surgical occlusion of the transverse-sigmoid sinuses was performed, combined with a venous by-pass connecting the proximal transverse sinus with the jugular vein. In one more case, surgical intervention was employed after an incomplete endovascular occlusion. No case was refered for g-knife treatment.
Embolization procedures
Overall, 209 procedures were performed to treat 170 patients, with an average of 1.2 sessions per patient and a maximum of 5 sessions, in a single case. The vast majority, namely, 145 patients, (85 %) was treated with a single endovascular procedure, whereas 25 patients were treated with staged procedures (Table 6). Three of our patients had been treated before (in a total of six embolization sessions) in other institutions.
In 177 (85 %) sessions, the transarterial approach (TA) was exclusively used. In 21 sessions (10 %), the transvenous (TV) approach was used exclusively. This was applied mainly for cavernous sinus lesions and occasionally for some lesions in the transverse or/and sigmoid sinus. Combination of TA and TV approach was used in 11 sessions.
In 124 patients (73 %), glue was used as the only or main embolic material. In 49 of these patients, NBCA alone was used. In 62 patients, NBCA was the main agent with PVA as supplementary material for residuals, which persisted following significant obliteration or the shunt with NBCA. In 13 cases, coils were used in addition. In 19 cases (11 %), mostly cavernous sinus lesions, coils were used as the only embolic material. In another 27 cases (16 %) pertaining to lesions with either a slow flow shunt, or to lesions with diffuse supply from very tortuous distal or just dangerous feeders, solely PVA was used. In six lesions, balloon assistance was employed.
Immediate angiographic results
Complete occlusion of the CDAVF was strictly considered the absence of any arteriovenous shunt in the late angiographic phases. As subtotal occlusion, was defined an occlusion rate of more than 90 % or a faint opacification of the shunt in the late arterial phase. Extensive occlusion was considered an occlusion of approximately 70–90 % of the shunt. An occlusion rate of <70 % was reported as partial occlusion.
In Table 5 appears the relation of operative sessions with obtained immediate angiographic results.
By summarizing the angiographic results, 112 patients (66 %) had an immediate complete angiographic occlusion of their CDAVF, 36 patients (21 %) had a subtotal occlusion, 17 patients (10 %) presented extensive occlusion, and 5 patients (3 %) had a partial occlusion (2 palliative, one aborted because of a complication).
Considering the immediate angiographic results in relation to the venous drainage pattern, a complete occlusion was achieved in 52 of the 86 patients (60.5 %) with benign lesions and in 60 of the 87 patients (69 %) with aggressive lesions.
Early clinical outcomes
Early clinical outcome is defined as the clinical condition of the patient during the period of postoperative hospitalization. For most of our patients who presented without bleeding, this period corresponded to 3–5 days.
One hundred sixty patients showed either complete disappearance (tinnitus in most of these cases) or clear improvement of their presenting symptoms (mainly applies to orbital symptomatology) or did not present a new neurological deficit postoperatively. This latter refers to patients who (a) were suffering of some neurological deficit due to presenting bleeding/ischemia, (b) the presenting symptom was not permanent in nature (as epileptic fit), and (c) it was too early to be evaluated during the immediate postoperative period (as in cases of dementia or nerve paresis).
Two patients presented temporary worsening of pre-existing symptoms (decreased visual acuity and chemosis with exophthalmos and diplopia, respectively). Both patients showed improvement after steroid administration during their hospitalization time.
Four patients developed new and permanent symptoms as a result of an operative complication. Four more patients developed new but temporary symptoms.
Complications of endovascular treatment
There were four cases of permanent neurological deficit (2.3 %) due to an operative complication and four cases of temporary neurological deficit (2.3 %) not clearly related to an operative complication. There was no mortality connected to an operative complication in this series.
The first case of permanent neurological deficit is related to an unwanted NBCA migration through a nonidendified collateral, the artery of the foramen lacerum to the middle cerebral artery and then to middle cerebral artery (MCA) territory, which resulted to a severe infarction of the MCA.
In the second case with permanent deficit, spasm of the superior cerebellar artery (SCA) was detected at the end of the procedure. However, dissection of the vessel could not be confidently excluded. The immediate postembolization employment of an open surgical operation aiming to a radical excision and the resulting cerebellar infarct makes the exact estimation of cause and effect difficult. Nevertheless, we included this case in the embolization-related complications due to the possible relation of cerebellar infarct with the alteration of the SCA detected in the angiogram.
The third case with permanent morbidity was a patient with X and XII nerve paresis after glue embolization of a jugular-hypoglossal foramen lesion.
The fourth patient with a torcular CDAVF and cerebellar cortical drainage through a varicose vein presented 2 days after embolization cerebellar signs and edema with later infarction presumably due to venous thrombosis. A decompressive craniectomy was performed, and the patient showed improvement during the ensuing weeks.
Three patients presented temporary diplopia immediately (one patient) and several hours after embolization (two patients). The two patients improved rapidly after 24 h, whereas the third patient recovered over several days.
One more patient with a transverse-sigmoid sinus CDAVF who presented with a first epileptic attack postoperatively did not suffer of any detected operative complication.
Follow-up
As a general rule, the first postoperative imaging with CT was performed on the same day or the day after the operation. MR was undertaken during the first 3–5 days after the operation.
Patients were usually evaluated at yearly intervals after treatment, but in many cases, an individualized approach was applied. In total, 158 patients were followed-up for 447 patient-years (mean of 2.8 years ranging from 1 to 15 years). For patients with known incomplete (subtotal or extensive or partial) immediate angiographic occlusion (InCAO) or cases of previously complete angiographic occlusion (CAO) with clinical or imaging signs of recurrence, the strategy was defined according to the specific symptomatology in combination with the findings of MR. The time of follow-up MR ranged from 3 months to 1 year after the embolization. Patients with aggressive lesions and incomplete immediate angiographic occlusion would come for MR imaging early (3–6 months) if their presentation was bleeding, or later (up to 1 year) if their presentation was other than bleeding. In case of suspicion of CVD, further DSA and embolization was planned. In case of failure to eliminate the CVD, surgery was considered.
For 95 patients, the clinical and MR follow-up confirmed the known CAO of their lesion, whereas 9 patients with previously CAO had a recurrence. Four patients presented recurrent clinical symptoms (one with new bleeding) during follow-up and underwent DSA and further embolization. In three of these patients a complete occlusion was achieved whereas for the fourth patient the occlusion was subtotal. Five patients with a previous CAO, in their regular MR imaging follow-up presented a recurrent shunt without CVD and without clinical manifestation. They are just followed-up.
Seven recently treated patients with CAO, have no follow-up examination yet, whereas one more patient with complete angiographic occlusion died few weeks after his admission as a consequence of his initial brainstem hemorrhage.
Thirty-five patients with an InCAO in the last embolization presented a dissapearance of vascular abnormalities (arterial feeding vessels, shunt, and dilated veins) in the follow-up MR examination (two had additional surgery) indicating a progression to complete occlusion of the lesion.
For 13 patients the MR follow-up imaging confirmed the known InCAO of their shunt; one patient of this group with persistent CVD presented cerebral bleeding and died. The remaining 12 patients had no clinical worsening, and 7 of them had no evidence of CVD; therefore, further follow-up and neither new embolization nor DSA control were suggested. The remaining five patients with CVD await further endovascular treatment.
Five recently treated patients with InCAO have no follow-up yet.
Another five patients were lost to follow-up.
In total, of the 165 embolized and followed-up patients, 141 patients (85.5 %) demonstrated a complete occlusion of their shunt. Sixty-five of the above patients had benign lesions; therefore, the complete occlusion rate for the benign group was 78 %, whereas 76 patients had aggressive lesions. Therefore, the complete occlusion rate for the aggressive group was 89.5 % (Table 6).
In terms of late clinical outcome, 134 patients presented either clinical cure or no new neurological deficit. Another 14 patients presented improvement of their symptoms during follow-up period, and 6 more patients had also improvement after subsidence of postoperative temporary neurological manifestations. In total, 154 (93 %) of treated and followed-up patients presented clinical cure or improvement of their symptoms.
As mentioned, four patients suffered a clinical worsening related to a complication. Another nine patients (from the group of InCAO) developed recurrent symptoms.
Three patients died. One died during the initial hospitalization due to his presenting intracerebral hemorrhage (ICH). The second patient died of myocardial infarction, and the third one died of cerebral bleeding in the follow-up period.
Discussion
Many reports appeared in the literature during the past years regarding treatment of CDAVFs [6, 8, 12, 15, 16, 20, 22, 25, 27, 38]. This is one of the largest series of CDAVF including typical, multiple, and extensive lesions from all intracranial locations, focusing on endovascular treatment, operative results, and complications and having a long-term follow-up. It comprises 170 consecutive patients treated exclusively endovascularly with the exception of two cases where surgical intervention was secondarily employed and three cases, which were treated conservatively.
Aspects of the disease related to the aetiopathogenesis and pathophysiology do not belong to the scope of this report.
Regarding the clinical presentation, a correlation between the venous drainage pattern of CDAVFs and the clinical course has been established [1, 4, 17, 24, 26]. Further aspects related to presentation and pathophysiology as well as presentation and location in regard to the venous epidural space will be addressed in future publications.
Generally, conservative treatment and follow-up in benign lesions with mild or no symptoms is the management of choice [11]. The patient’s tolerance to otherwise benign symptoms and his attitude towards active or conservative treatment in relation with the anticipated risks played a decisive role in the management of benign lesions in our series and explain the high treatment rate.
Complete elimination of the lesion is certainly the ultimate goal. However, there are extensive and complex lesions, which involve distal, multiple, and tortuous arterial feeders, with no possibility of selective approach to the shunting zone neither transarterially nor transvenously.
In such cases, palliative treatment for control of symptoms even with a nonpermanent embolic agent or targeted treatment for elimination of the CVD, if detected, may be a reasonable alternative.
If we examine the patients treated in the present series divided in two groups, the “benign” group (without CVD) and the “aggressive” group (those with CVD) including 86 and 87 patients respectively, we will notice that the “benign” group had no operative complication and permanent morbidity, whereas all permanent-morbidity cases belong to the “aggressive” group. This is a crucial point to emphasize. Acceptable treatment for a lesion with low natural risk means treatment with even lower risk of complications, namely, complication rate zero or nearly zero.
Progression of some lesions from InCAO to complete occlusion based on MR-imaging criteria is related to the fact that some cases with an angiographically demonstrated subtotal occlusion at the end of embolization developed progressive thrombosis of their shunt and draining vein in the immediate postoperative MR or during follow-up. This could be explained by the observation that a subtotal occlusion of a dural shunt with faint opacification of the collecting vein in the late arterial phase, in many cases, represents one step before the complete thrombosis, which is just a matter of time to occur. This observation applies also to some cases of partial embolization with NBCA targeted to the dominant part of the shunt (our data still anecdotal). However, the limitation of the diagnostic inferiority of MR in comparison with the catheter angiogram should be always kept in mind.
The total percentages of complete occlusion and clinical cure (85.5 % total—78 % for benign lesions and 89.5 % for aggressive lesions) and clinical cure (93 %) are among the highest reported with an associated complication rate among the lowest [15, 21, 23, 39].
Selectivity is the quintessence of endovascular treatment, and the core of the lesion is the only target of a selective endovascular operation.
NBCA is an adhesive, permanent, thrombogenic, and cheap embolic material with adjustable penetration according to the mixture, good visibility, and known long-term behavior. Mastering the use of a material with such properties in the dural vasculature enables selective, effective, and safe embolization even through single small feeders. Needless to emphasize, the material can never be the protagonist of a neuroendovascular operation. Good anatomical knowledge and elegant technique are the primary factors for success [14].
Lately, a new liquid nonadhesive polymer (Onyx, ev3 Neurovascular, Irvine, CA, USA) has been introduced and is meanwhile recommended as the material of choice for the embolization of CDAVF [8, 30, 35]. The reported series on the use of Onyx in the treatment of CDAVF are not comparable with this series in terms of number and composition of cases. Therefore, at this point in time, no conclusions can be drawn over the superiority of one over the other material. In any case, the results presented here, with high anatomic and clinical cure, low complication rate, and few embolization sessions per patient using the mentioned embolic materials and especially NBCA makes comparison with other materials not meaningful. In addition, it is known that deep penetration of Onyx to the shunt requires reflux around the microcatheter and frequently leads to a surprisingly extensive occlusion of the vascular network around the actual lesion. This is sometimes associated with an unacceptable rate and/or kind of complications especially for lesions of the cavernous sinus [18, 25, 34].
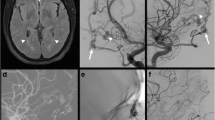
Despite its invasiveness, six-vessel angiography remains the most reliable modality for diagnosing, assessing, and classifying CDAVF [28].
Magnetic resonance angiography and venography provide a noninvasive method which despite its limitations related to suboptimal resolution and definition of flow dynamics [2, 5, 37] offer a reliable and noninvasive alternative for follow-up of treated patients [31, 33]. In our institution, conventional MR imaging, MR angiography (3D-TOF-MRA), and TR contrast-enhanced MRA are used for the visualization of CDAVF. Based on our experience and published reports [29, 32], even slightly dilated cortical veins that signify CVD can be detected with flow sensitive MR techniques.
The indisputable exclusion of a small and slow-flow lesion [41] or recurrence during follow-up requires a DSA control. However, in an asymptomatic patient, such a small and/or slow flow shunt would be rather benign without clinical significance, and longer follow-up is enough to ensure the safety of the patient and exclude potential progression to a higher-grade lesion.
A curative g-knife treatment for benign lesions is, in our experience, rather unnecessary because it is not completely clear whether the long-term morbidity rate outweighs the benign natural course of the disease [36]. Lesions with CVD have a contraindication for radiosurgery mainly because its result is not achievable in a timely fashion. Consequently, g-knife treatment can be used only in the treatment of benign CDAVF with intolerable symptoms or aggressive CDAVF, not accessible or not responsive to endovascular treatment or surgery.
Surgery for the obliteration of CDAVF is frequently associated with higher risks [19, 40]. However, some groups have suggested selective surgical disconnection of the draining cortical vein as a minimally invasive and effective treatment for lesions with CVD [9, 10]. Actually, simple surgical disconnection of the cortical venous reflux may be a good option in the management of patients with aggressive and easily aproachable lesions, when anatomic features prevented endovascular access or embolization failled.
Combined endovascular and surgical treatment was practically a rare exception in our series.
Conclusion
Endovascular embolization is the treatment of choice for CDAVFs. High percentage of anatomical cure or subtotal-extensive occlusion of the lesion with even higher rates of excellent clinical results, associated with very low operative complication rate can be achieved with few embolization sessions per patient. According to our experience, these results can be reliably achieved with a concept of selective attack of the arteriovenous shunt and specifically its venous component, by mastering atraumatic superselective microcatheterization as well as the use of certain permanent embolic materials. Tailoring the therapeutic strategy according to the individual case is mandatory. Overtreatments and aggressive material-based approaches, ignoring the actual angioarchitecture, the clinical aspect and course of the disease should be avoided.
References
Awad IA, Little JR, Akarawi WP, Ahl J (1990) Intracranial dural arteriovenous malformations: factors predisposing to an aggressive neurological course. J Neurosurg 72:839–850
Bink A, Berkefeld J, Wagner M, You SJ, Ackermann H, Lorenz MW et al (2011) Detection and grading of dAVF: prospects and limitations of 3T MRI. Eur Radiol 22:429–438
Borden JA, Wu JK, Shucart WA (1995) A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg 82:166–179
Castaigne P, Bories J, Brunet P, Merland JJ, Meininger V (1976) Les fistules arterioveineuses meningres pures drainage veineux cortical. Rev Neurol 132:169–181
Chen JC, Tsuruda JS, Halbach VV (1992) Suspected dural arteriovenous fistula: results with screening MR angiography in seven patients. Radiology 183:265–271
Chung SJ, Kim JS, Kim JC, Lee SK, Kwon SU, Lee MC et al (2002) Intracranial dural arteriovenous fistulas: analysis of 60 patients. Cerebrovasc Dis 13:79–88
Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A et al (1995) Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology 194:671–680
Cognard C, Januel AC, Silva NA Jr, Tall P (2008) Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: new management using Onyx. AJNR Am J Neuroradiol 29:235–241
Collice M, D’Alberti G, Talamonti G, Branca V, Boccardi E, Scialfa G, Versari P (1996) Surgical interruption of leptomeningeal drainage as treatment for intracranial dural arteriovenous fistulas without dural sinus drainage. J Neurosurg 84:810–817
DaCosta LB, Terbrugge K, Farb R, Wallace MC (2007) Surgical disconnection of cortical venous reflux as a treatment for Borden type II dural arteriovenous fistulae. Acta Neurochir (Wien) 149:1103–1110
Davies MA, Saleh J, Ter Brugge K, Willinsky R, Wallace MC (1997) The natural history and management of intracranial dural arteriovenous fistulae. Part 1: benign lesions. Interv Neuroradiol 3:295–302
Fermand M, Reizine D, Melki JP, Riche MC, Merland JJ (1987) Long term follow-up of 43 pure dural arteriovenous fistulae (AVF) of the lateral sinus. Neuroradiology 29:348–353
Geibprasert S, Pereira V, Krings T, Jiarakongmun P, Toulgoat F, Pongpech S et al (2008) Dural arteriovenous shunts: a new classification of craniospinal epidural venous anatomical bases and clinical correlations. Stroke 39:2783–2794
Geibprasert S, Pongpech S, Armstrong D, Krings T (2009) Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: vessels the neurointerventionalist needs to know. AJNR Am J Neuroradiol 30:1459–1468
Guedin P, Gaillard S, Boulin A, Condette-Auliac S, Bourdain F, Guieu S et al (2010) Therapeutic management of intracranial dural arteriovenous shunts with leptomeningeal venous drainage: report of 53 consecutive patients with emphasis on transarterial embolization with acrylic glue. J Neurosurg 112:603–610
Halbach VV, Higashida RT, Hieshima GB, Goto K, Norman D, Newton TH (1987) Dural fistulas involving the transverse and sigmoid sinuses: results of treatment in 28 patients. Radiology 163:443–447
Houser OW, Baker HL Jr, Rhoton AL Jr, Okazaki H (1972) Intracranial dural arteriovenous malformations. Radiology 105:55–64
Jankowitz BT, Vora N, Jovin T, Horowitz M (2009) Ear necrosis resulting from the endovascular onyx-18 embolization of a dural arteriovenous fistula fed by the posterior auricular artery. J Neuroimaging 19:259–262
Kakarla UK, Deshmukh VR, Zabramski JM, Albuquerque FC, McDougall CG, Spetzler RF (2007) Surgical treatment of high-risk intracranial dural arteriovenous fistulae: clinical outcomes and avoidance of complications. Neurosurgery 61:447–457, discussion 457-449
Kim DJ, Kim DI, Suh SH, Kim J, Lee SK, Kim EY et al (2006) Results of transvenous embolization of cavernous dural arteriovenous fistula: a single-center experience with emphasis on complications and management. AJNR Am J Neuroradiol 27:2078–2082
Kim DJ, Willinsky RA, Krings T, Agid R, Terbrugge K (2011) Intracranial dural arteriovenous shunts: transarterial glue embolization–experience in 115 consecutive patients. Radiology 258:554–561
Kirsch M, Henkes H, Liebig T, Weber W, Esser J, Golik S et al (2006) Endovascular management of dural carotid-cavernous sinus fistulas in 141 patients. Neuroradiology 48:486–490
Kirsch M, Liebig T, Kuhne D, Henkes H (2009) Endovascular management of dural arteriovenous fistulas of the transverse and sigmoid sinus in 150 patients. Neuroradiology 51:477–483
Lasjaunias P, Chiu M, ter Brugge K, Tolia A, Hurth M, Bernstein M (1986) Neurological manifestations of intracranial dural arteriovenous malformations. J Neurosurg 64:724–730
Lv X, Jiang C, Li Y, Wu Z (2008) Results and complications of transarterial embolization of intracranial dural arteriovenous fistulas using Onyx-18. J Neurosurg 109:1083–1090
Malik GM, Pearce JE, Ausman JI, Mehta B (1984) Dural arteriovenous malformations and intracranial hemorrhage. Neurosurgery 15:332–339
Meyers PMHV, Dowd CF, Lempert TE, Malek AM, Phatouros CC, Lefler JE, Higashida RT (2002) Dural carotid cavernous fistula: definitive endovascular management and long-term follow-up. Am J Ophthalmol 134:85–92
Nishimura S, Hirai T, Sasao A, Kitajima M, Morioka M, Kai Y et al (2010) Evaluation of dural arteriovenous fistulas with 4D contrast-enhanced MR angiography at 3T. AJNR Am J Neuroradiol 31:80–85
Noguchi K, Kuwayama N, Kubo M, Kamisaki Y, Kameda K, Tomizawa G et al (2011) Flow-sensitive alternating inversion recovery (fair) imaging for retrograde cortical venous drainage related to intracranial dural arteriovenous fistula. Neuroradiology 53:153–158
Panagiotopoulos V, Moller-Hartmann W, Asgari S, Sandalcioglu IE, Forsting M, Wanke I (2009) Onyx embolization as a first line treatment for intracranial dural arteriovenous fistulas with cortical venous reflux. Rofo 181:129–138
Pekkola J, Kangasniemi M (2011) Posterior fossa dural arteriovenous fistulas: diagnosis and follow-up with time-resolved imaging of contrast kinetics (TRICKS) at 1.5T. Acta Radiol 52:442–447
Saini J, Thomas B, Bodhey NK, Periakaruppan A, Babulal JM (2009) Susceptibility-weighted imaging in cranial dural arteriovenous fistulas. AJNR Am J Neuroradiol 30:E6
Sakamoto S, Shibukawa M, Kiura Y, Matsushige T, Abe N, Kurisu K (2010) Evaluation of dural arteriovenous fistulas of cavernous sinus before and after endovascular treatment using time-resolved MR angiography. Neurosurg Rev 33:217–222, discussion 222-213
Saraf R, Shrivastava M, Kumar N, Limaye U (2010) Embolization of cranial dural arteriovenous fistulae with ONYX: indications, techniques, and outcomes. Indian J Radiol Imaging 20:26–33
Saraf R, Shrivastava M, Siddhartha W, Limaye U (2010) Evolution of endovascular management of intracranial dural arteriovenous fistulas: single center experience. Neurol India 58:62–68
Satomi J, van Dijk JM, Terbrugge KG, Willinsky RA, Wallace MC (2002) Benign cranial dural arteriovenous fistulas: outcome of conservative management based on the natural history of the lesion. J Neurosurg 97:767–770
Schanker BD, Walcott BP, Nahed BV, Ogilvy CS, Kiruluta AJ, Rabinov JD et al (2011) Time-resolved contrast-enhanced magnetic resonance angiography in the investigation of suspected intracranial dural arteriovenous fistula. J Clin Neurosci 18:837–839
Shah SB, Lalwani AK, Dowd CF (1999) Transverse/sigmoid sinus dural arteriovenous fistulas presenting as pulsatile tinnitus. Laryngoscope 109:54–58
Stiefel MF, Albuquerque FC, Park MS, Dashti SR, McDougall CG (2009) Endovascular treatment of intracranial dural arteriovenous fistulae using Onyx: a case series. Neurosurgery 65:132–139, discussion 139-140
Sundt TM Jr, Piepgras DG (1983) The surgical approach to arteriovenous malformations of the lateral and sigmoid dural sinuses. J Neurosurg 59:32–39
Willems PW, Brouwer PA, Barfett JJ, terBrugge KG, Krings T (2011) Detection and classification of cranial dural arteriovenous fistulas using 4D-CT angiography: initial experience. AJNR Am J Neuroradiol 32:49–53
Financial support
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Timo Krings, Toronto, Canada
This is one of the largest single-center series on the treatment of dural arteriovenous fistulae that highlights the high success rates and the low complication rates if anatomy is respected and the nature of the disease is understood. One of the major benefits of this article is the long follow-up that allows the reader to deduce that once stable obliteration of the DAVF is obtained, chances of recurrence are very low. The manuscript also demonstrates the goal of treatment in cranial dural arteriovenous fistulae, i.e., the obliteration of the transition between the arterial and venous segment. It is not the type of embolizing agent that will make a difference in complication and cure rate but instead the knowledge of the supply to the cranial nerves and prediction of the existence and location of the so-called “dangerous” EC-IC anastomoses especially at the level of the cavernous sinus that has to be mastered to obtain the results presented in this article. Or, as Pierre Lasjaunias used to phrase it: “Anatomy is the cheapest way to safe.”
Giuseppe Lanzino, Rochester, USA
With better understanding of their angioarchitecture and pathophysiology, continuous refinement of endovascular materials and techniques, most intracranial dural arteriovenous fistulas (DAVFs) can nowadays be effectively treated with very low morbidity and mortality. In their monumental series encompassing 16 years, Baltsavias and Valavanis report their experience with embolization of 170 consecutive patients with intracranial DAVFs. Sixty-seven percent of patients suffered from benign symptoms (usually related to high-flow conditions) such as bruit and conjunctival injection, while the remaining presented with an aggressive clinical picture. Immediate anatomic cure was achieved in 60.5 % of patients with benign symptoms and 69 % of those with aggressive lesions. These rates of complete anatomical obliteration increased to 78 % for the benign group and 89.5 % for the aggressive DAVFs. There was no mortality in this series, and the permanent morbidity rate was very low (in the low single digits). This remarkable experience illustrates what can be achieved today with endovascular techniques in the hands of a recognized master with incredible skills and experience.
The availability of different treatment modalities (which are often complementary) allows the treating physician to individualize treatment based on the clinical and radiological characteristics of the specific patients. Patients with minimally symptomatic fistulas without retrograde cortical venous drainage can be safely managed conservatively, and in several cases, I have observed remarkable spontaneous regression of the fistula, including spontaneous occlusion. Because of this, I believe that some of those cases that have been described to resolve after intermittent carotid compressions might indeed represent just the benign natural history and evolution of some of these lesions independent of the intermittent compression. Patients with disabling symptoms associated with high-flow conditions, in the absence of retrograde cortical venous drainage, are offered at our Institution, transarterial particulate embolization with the idea of “palliate” their symptoms. This approach (using particles greater than 150 μm in the external carotid artery branches) is extremely safe and effective in resolving patients’ symptoms. Often, this strategy of transarterial PVA embolization is combined with gamma knife radiosurgery. Gamma knife is extremely effective in achieving complete obliteration within usually 1 year, especially in the case of transverse/sigmoid sinus and cavernous sinus DAVFs. In patients with aggressive clinical symptoms, we try to achieve a rapid cure. In these cases, coil embolization of the involved venous drainage usually through a transvenous approach remains our treatment of choice particularly for indirect cavernous sinus fistulas. Patients with exclusive retrograde cortical venous drainage are in our hands often effectively treated with transarterial Onyx embolization, especially when a straight feeder such as the posterior branch of the middle meningeal artery is available for embolization. With the availability of these complementary non invasive solutions, it is uncommon nowadays to recur to surgical interruption of the fistula. However, surgery is still a valid option when endovascular techniques are not effective, and patients have presented with aggressive symptoms or have significant retrograde cortical venous drainage.
Karel terBrugge, Toronto, Canada
I have read with great interest the manuscript by Baltsavias and Valavanis regarding their large experience with endovascular management of patients with intracranial dural arteriovenous fistulas (SDAVFs). The team of Professor Valavanis is well known and well accomplished, and their management outcome resulted in an 89.5 % obliteration rate of DAVFs with cortical venous reflux using predominantly glue as the embolic agent of choice. The associated permanent complication rate was 2.3 %. In the so-called benign DAVFs, a cure was confirmed on follow up in 78 % of treated patients and no permanent complications occurred. Publication of this experience is very timely in view of the shift towards the use of ONYX as the embolic material of choice for the endovascular management of this condition, and the current publication will serve as a standard against which other treatment modalities outcomes can be compared. We congratulate the Zurich team on this excellent work. KTB
Rights and permissions
About this article
Cite this article
Baltsavias, G., Valavanis, A. Endovascular treatment of 170 consecutive cranial dural arteriovenous fistulae: results and complications. Neurosurg Rev 37, 63–71 (2014). https://doi.org/10.1007/s10143-013-0498-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-013-0498-2