Abstract
The right ventricle (RV) is the main determinant of prognosis in pulmonary hypertension. Adaptation and maladaptation of the RV are of crucial importance. In the course of disease, RV contractility increases through changes in muscle properties and muscle hypertrophy. At a certain point, the point of “uncoupling,” the afterload exceeds contractility, and maladaptation as well as dilation occurs to maintain stroke volume (SV). To understand the adaptational processes and to further develop targeted medication directly affecting load-independent contractility, an accurate and precise assessment of contractility and RV–pulmonary artery (PA) coupling should be performed. In this review, we shed light on existing methods to assess RV function, including the gold standard measurement of contractility and RV–PA coupling, and we evaluate existing surrogates of RV–PA coupling.
Zusammenfassung
Die Funktion des rechten Ventrikels (RV) ist für die Prognose der pulmonalen Hypertonie (PH) ein entscheidender Faktor. Dabei spielen adaptive und maladaptive Prozesse eine wichtige Rolle. Ein entscheidender Faktor der Adaptation ist die Erhöhung der nachlastunabhängigen Kontraktilität des RV als Reaktion auf die Nachlast. Diese wird zu Beginn der Erkrankung durch z. B. muskuläre Hypertrophie gesteigert. Am Beginn der Maladaptation kann jedoch die Kontraktilität den Anstieg der Nachlast nicht kompensieren, und es kommt zu einem „Entkoppeln“ der Achse zwischen RV und Pulmonalarterien (PA) und zu einer Maladaptation und Dilatation, um das das Schlagvolumen (SV) zu erhalten. Um einerseits diese adaptiven und maladaptiven Prozesse zu analysieren und andererseits therapeutische Strategien zu entwickeln, die auf die lastunabhängige Kontraktilität zielen, sollte die Kontraktilität des RV bestmöglich gemessen werden. In diesem Übersichtsartikel werden Methoden vorgestellt, die nach derzeitigem Stand die Funktion der RV-PA-Achse am genauesten darstellen, und Methoden beurteilt, die als Surrogate dafür verwendet werden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In the past decade, the right ventricle and right ventricular (RV) function have become the focus of increased scientific interest and the RV is no longer “the forgotten chamber”. Right ventricular function is the main determinant of symptomatology and outcome in patients with pulmonary arterial hypertension (PAH; [73]). The response of the RV to the increasing afterload in pulmonary circulation is a complex process and maladaptation or RV failure predominantly determines the prognosis of patients with PAH [73]. Right heart failure in pulmonary hypertension (PH) is caused by increased afterload and therefore a description of the cardiopulmonary unit is indispensable. This is best described as the interplay between RV contractility, ventricular elastance (Ees), and arterial elastance (Ea), a measure of afterload [72].
However, in the current literature there are several measures of RV contractility and its relation to the load it faces (Ees/Ea). The present review focuses on existing measures of RV contractility and measures of the RV–pulmonary artery (PA) unit and summarizes the existing noninvasive measures of RV function.
Adaptation and maladaptation
Right ventricular failure can be described as a clinical syndrome, consisting of dyspnea, fatigue, and congestion, which is characterized by a decrease in RV function, leading to elevated filling pressures and reduced cardiac output [34]. However, there is currently a debate about accessible bedside tools for assessing RV function and physiological parameters describing the relation of RV contractility to its load. In certain states of the adaptational process to increased afterload, the RV ejection fraction (EF) might be decreased, whereas Ees might be elevated [54]. This fact emphasizes the current dilemma of, firstly, adequately describing RV function and, secondly, how to cope with the existing data on physiological parameters derived from pressure–volume loops in daily clinical practice.
In the course of disease, and owing to increasing afterload in PAH, RV contractility (Ees) increases in order to maintain RV–PA coupling (Ees/Ea). At a certain point, “the point of uncoupling,” Ea significantly exceeds Ees, leading to a significantly reduced Ees/Ea relationship. At this point, the RV dilates to maintain stroke volume (SV).
Recently it was shown that the coupling of RV contractility to increased afterload in PH has considerable reserve, as Ees/Ea has to decrease from normal values of 1.5–2 to below 0.8 before an increase in volumes and a decrease in EF below the critical value of 35% occur [59].
The onset of RV dilatation due to uncoupling and eventual RV failure are not entirely clear. It appears that the homeometric (contractile) adaptation of the RV to afterload buffers the Ees/Ea ratio in the presence of significant worsening of PH [73]. In animal models, the RV dilated when the Ees/Ea ratio decreased to 0.7–1.0 [13, 19], and the Ees/Ea ratio was not sensitive to interventions that effectively decreased Ea because Ees decreased proportionally to Ea [49]. Experimental work on isolated canine hearts showed that maximal stroke work (volume × pressure) occurs at Ea/Ees = 0.80 ± 0.16, whereas ventricular efficiency (stroke work/myocardial oxygen consumption) is maximal at Ea/Ees = 0.70 ± 0.15. This suggests that optimal RV–arterial coupling might occur at values lower than the range of 1.5–2 predicted by mathematical models [10]. Recently, Axell and coworkers defined the Ees/Ea threshold below which SV or cardiac output decreased in either animal models or patients with chronic thromboembolic PH as around 0.7 [2], which is lower than the cut-off defined by Tello and coworkers [59].
Patients with PAH receiving targeted therapies may remain stable for several years but may present with increased RV dimensions and decreased EF, heralding clinical deterioration and decreased survival [66, 67, 73]. As increased RV dimensions and decreased EF can only be the consequence of RV–PA uncoupling, a definition of the Ees/Ea ratio—the gold standard measure of RV–PA coupling—at which relevant RV maladaptation begins is crucial for linking physiological measurements to noninvasively assessed measures of RV function.
The transition from adaptation to maladaptation and failure is progressive and cut-off values on volumes are difficult to define. An RVEF of <35% has consistently been shown to be associated with decreased survival in severe PH [5, 7, 66, 69] and is easily modeled to be associated with rapid increases in end-diastolic volume (EDV) and end-systolic volume (ESV) when SV is to be preserved [70].
Reports of Ees and Ea measured with gold standard pressure volume–loop catheters in patients with PH are scarce. Kuehne et al. used high-fidelity catheters in 2004 [33]. The authors measured RV pressures in animals and reported an approximately threefold increase in Ees in the presence of a sixfold increase in Ea, resulting in a substantially decreased Ees/Ea ratio (on average from 2 to 1) in PH. Subsequent studies showed similarly increased Ees but decreased Ees/Ea in idiopathic PAH [54, 57], PAH associated with systemic sclerosis [28, 57], and chronic thromboembolic PH [40, 54]. Two of the studies also reported measurements during exercise, showing decreased Ees/Ea even in patients with PAH who had persistently normal values at rest [28, 54], in contrast to controls who maintained their Ees/Ea ratio during exercise. Decreased Ees/Ea during exercise in PAH was associated with increased RV ESV and EDV [28].
With gold standard high-fidelity pressure–volume technology for the measurement of RV volumes, Ees and Ea measurements have relied either on a multiple-beat method allowing for elastance calculations on a family of pressure–volume loops generated during a decrease of venous return ([28, 57]; Fig. 1) or a single-beat method with Pmax calculations and measurement of relative change in volume on just one pressure–volume loop [33, 54]. The single-beat method has been validated in normotensive dogs with or without acute hypoxia-induced PH [8]. Most recently, Inuzuka and coworkers demonstrated an association of the aforementioned single-beat estimation with the multi-beat approach [31]. The single-beat method was tightly correlated with the multiple-beat method for assessment of RV–PA coupling in patients with and without PH [31]. In that study, the “standard” single-beat method assuming linearity of the Ees curve was less well correlated with the multiple-beat method for assessment of RV–PA coupling.
Assessment of right ventricular (RV) contractility and RV–pulmonary artery (PA) coupling with the gold standard multi-beat approach (original measurement). a Ultrasound-guided insertion of pressure–volume (PV) catheter (blue asterisk). b Balloon occlusion of the inferior vena cava (IVC; red asterisk). c Deflation of the IVC balloon (yellow asterisk). d Original PV–loop measurement, with load-independent contractility (end-systolic elastance, Ees), arterial elastance as a measure of afterload (Ea), and end-diastolic elastance (Eed) as a measure of diastolic function
Methods to measure function of RV–PA unit
Right ventricular function can be characterized by the pressure–volume loop relation. The gold standard for measurement of ventricular contractility is the construction of multiple pressure–volume loops as described by Suga et al. [55] for the left ventricle and adopted for the RV by Maughan et al. in the canine ventricle and by Redington et al. in the human RV ([38, 48]; Fig. 1). To measure Ees, a linear regression is set through the end-systolic pressure–volume relationship (ESPVR) of each one of several cardiac cycles during load alterations [55].
With the development and the validation of the conductance catheter for the volume measurement [11], research in RV pressure–volume loops has become more widespread, as the assessment is simpler to perform than with previous methods.
The conductance catheter (Fig. 1) measures pressure and volume simultaneously. Volume is measured by setting up an electrical field between the proximal and distal electrodes of the catheter when positioned (via echocardiography (Fig. 1) or radiography) in the RV apex. Electrical conductivity is measured by the electrodes, and changes in conductivity reflect segmental volume changes. The catheter is mostly volume-calibrated via cardiac magnetic resonance imaging (CMRI) as the gold standard for measurement of volume.
There are several clinical studies in which conductance catheters were used to assess contractility and/or RV–arterial coupling. The studies included patients with idiopathic PAH, systemic sclerosis-associated PAH [28, 57], systemic sclerosis without PH [57], chronic thromboembolic PH and chronic thromboembolic disease without PH [2, 39].
The main difference between these studies is the method used to assess RV–arterial coupling. Tedford et al. [57] and Tello and coworkers [60] measured Ees using a multi-beat method (Fig. 1) with preload reduction either by balloon occlusion of the inferior vena cava (IVC) or through the Valsalva maneuver [75]. By contrast, Tello and colleagues [59, 61, 62]and McCabe et al. [39], for instance, used the conductance catheter to measure precisely the end-systolic pressure (ESP) as one of the essential values required for determination of coupling via the single-beat method described by Brimioulle et al. [8]. In the single-beat method, Ea is calculated as ESP/SV and Ees is calculated as (Pmax − ESP)/SV, while Pmax is estimated as the maximal theoretical pressure that would build up through clamping of the pulmonary valve. Some groups used a right heart catheter-based approach, in order to avoid pressure–volume loop measurement [63]. In that approach, ESP is replaced by mean PA pressure [63] and Pmax is calculated using the sine wave extrapolation [8]. However, recently this approach has been shown to be misleading as especially in higher pressures ESP is significantly underestimated by mPAP [62].
The Eed of the ventricle is a load-independent representation of the diastolic function. The clinical relevance of RV diastolic function in patients with PH is a new area of interest in our understanding of RV function. Recent studies in patients with pulmonary hypertension have shown that increased RV diastolic stiffness is significantly associated with outcomes including mortality and lung transplantation [64, 69]. Patients on PAH-specific therapy for 3 months showed a significant decrease in RV diastolic stiffness compared with pretreatment values [68]. On the left side of the heart, it has long been recognized that diastolic dysfunction and stiffening of the left ventricle are major contributors to heart failure, and an integral part of the routine evaluation of patients presenting with heart failure is the assessment of left ventricular diastolic dysfunction using echocardiography [42]. Recent studies have started to develop clinical methods to assess RV diastolic stiffness. Tello et al. recently showed that RV diastolic stiffness is highly associated with impaired RV strain measured with feature tracking [61] and they introduced a novel parameter (RV longitudinal strain/EDV [BSA]) to estimate Eed in chronic pressure overload.
Right ventricular diastolic function is typically quantified from the end-diastolic pressure–volume relationship (EDPVR). Under ideal conditions, the EDPVR would be measured from multi-beat pressure–volume loops with preload reduction (Fig. 1). The ESV/beginning-diastolic pressure (BDP) and end-diastolic volume (EDV)/end-diastolic pressure (EDP) would be determined from each pressure–volume loop and then fitted to an EDPVR. However, EDPVR has also been determined from single-beat pressure–volume loops (Fig. 1). Right ventricular pressure traces from right heart catheterization are used to determine begin-diastolic pressure and end-diastolic pressure, while CMRI is used to determine ESV and EDV. Studies on RV diastolic function have used an exponential fit [P = α exp(βV) − 1] to describe RV diastolic stiffness [47, 59, 61, 64, 68, 69]. The derivative of the EDPVR is a measure of chamber stiffness or the change of pressure for a given change in volume.
Surrogates of RV–PA coupling
The description of RV function in relation to its load is of high interest for clinicians. Currently, several methods exist to define Ees/Ea RV–PA coupling in a semi-invasive or even noninvasive approach.
Sanz et al. described a method to simplify measurements of elastance and avoid pressure measurements when assessing contractility and RV–arterial coupling [51]. The method assumed that Emax is defined as ESP/ESV; ESP was replaced by mPAP and Ea was calculated as mPAP/SV. Thus, Ees/Ea was simplified to SV/ESV without validation by the gold standard of Ees assessment (the multi-beat method with preload reduction and simultaneously measured pressure–volume loops). It should be emphasized that SV/ESV is inversely related to RVEF, as demonstrated by the formula SV/ESV = EF/(1 − EF); SV/ESV and RVEF have a prognostic meaning, and should be taken as parameters of functional interaction and of not coupling. Furthermore, RVEF and SV/ESV have been shown to be predictive of outcome in patients with PAH [7]. Cut-off values for RVEF shown to be associated with mortality are 35% [66] and for SV/ESV, 54% [7].
Kuehne et al. were the first to describe assessment of pressure–volume loops in patients with PAH (n = 6). They measured volume using CMRI and synchronized this with pressure measurements from a fluid-filled catheter [33]. The Ees was calculated using the single-beat method described before [8].
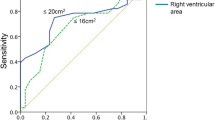
Other surrogates of RV–PA coupling rely solely on echocardiographic data [25]. Since measuring Ees and Ea via pressure–volume loops is invasive and expensive, simpler noninvasive surrogates are being sought. One of these is the Doppler echocardiography measurement of the ratio of tricuspid annular plane systolic excursion (TAPSE) to systolic pulmonary artery pressure (PASP; [25]). The TAPSE/PASP ratio has been shown to be a potent independent predictor of pre-capillary PH and prognosis in heart failure [6, 18, 20, 25,26,27], with a defined prognostic cut-off value of 0.36 mm/mm Hg [24]. The TAPSE/PASP ratio has also been shown to be an independent predictor of outcome in PAH [58]. Initially thought of as an indirect assessment of the ventricular length–tension relationship [25], TAPSE/PASP has been considered a surrogate of Ees/Ea, based on the assumption that TAPSE estimates contractility and PASP estimates afterload [6, 18, 20, 24, 26, 27, 58]. Other suggested echocardiographic surrogates are the ratios of RV fractional area change (FAC) to mean pulmonary artery pressure (mPAP, invasively measured; [45, 46, 50]) RV area change to RV end-systolic area (ESA; [15]) TAPSE to pulmonary artery acceleration time (PAAT; [36]) and SV to ESA (derived by dividing PASP/ESA as a surrogate of Ees; [9, 44] by PASP/SV as a surrogate of Ea). None of these parameters has been validated against pressure–volume loop-derived parameters yet.
Conventional imaging parameters to assess RV function
Cardiac MRI is of crucial importance for imaging in PAH (Table 1) and it gives information on RV function and fibrosis (Table 1).
Right ventricular dilation has been associated with a worse prognosis [56]. Furthermore, an RVEF below 35% was identified as the leading parameter in predicting mortality in PAH [5]. Badagliacca and colleagues demonstrated more clinical worsening events in patients with an elevated mass/volume ratio [4]. Beside conventional parameters describing volume and mass, delayed enhancement imaging on MRI is well known and established. Magnetic resonance imaging is very important for assessing the impact of drugs on cardiac function, as it is noninvasive. A study by an Amsterdam group included 80 patients with incident PAH (hereditary, idiopathic, or drug-induced). Patients were in functional class II or III. The benefits of either upfront combination therapy with an endothelin-receptor antagonist (ETRA) and a phosphodiesterase-5 inhibitor (PDE5i) or each of these agents given as monotherapy were examined. The authors found that RV volumes, as RV end-diastolic volume, improved in patients with upfront combination therapy but not in patients with monotherapy [65]. The Euro-MR Study [43] found improvements in RV systolic and diastolic volumes as well as in stroke volume.
The RV-insertion point enhancement is strongly associated with elevated PA pressures and showed worse outcomes in patients with PAH [14]. In addition to the link with reduced regional contractility [53], delayed enhancement is an interesting and important tool for the diagnosis of PH patients.
Delayed enhancement imaging reveals regional myocardial abnormalities, whereas T1 mapping, an emerging tool in CMRI identifies diffuse myocardial abnormalities by measuring native RV T1 based on pre- and post-contrast T1 times [41]. T1 mapping (Table 1) has the potential to be a marker of fibrosis [17, 30], which has recently been highlighted as part of an adaptive response to prevent cardiomyocyte overstretch and to maintain RV shape for optimal function, and of a maladaptive response that increases diastolic stiffness [1]. Recently, Tello et al. showed the association of invasively measured pressure–volume loop-derived end-diastolic RV stiffness with T1 mapping, emphasizing its diagnostic value for fibrosis and end-diastolic stiffness [59].
Magnetic resonance imaging strain is an emerging tool for assessing regional myocardial deformation. Myocardial deformation analysis using feature tracking is advantageous as it is applied to bSSFP (balanced steady-state free precession imaging) cine image data, yielding reliable strain data without the need for further image acquisitions. Recently Tello et al. demonstrated that in chronic pressure overload, radial strain is increasingly impaired with increasing RV EDV, which emphasizes the fact that volume overload is one of the central underlying processes that further worsens myocardial deformation [61]. Earlier, Sato and colleagues found that combination therapy was associated with a significant improvement in both RV and LV function, as assessed by CMR-derived feature tracking strain [52].
Echocardiography is one of the key screening tools in the evaluation of PH (Fig. 2). Beside conventional and well-established measures of RV function, newer and very interesting nonconventional techniques were introduced in recent years.
Echocardiographic functional parameter of the right ventricle. GLS global longitudinal strain, TDI tissue Doppler imaging, TAPSE tricuspid annular plane systolic excursion, FAC fractional area change, RV-EDD right ventricular end-diastolic diameter, RA right atrium, RV right ventricle, LV left ventricle
Right atrial size as an indirect measure of RV function has proven to be associated with prognosis [21, 22]. Tricuspid annular plane during systolic excursion is mostly taken as a surrogate for RV function (Fig. 2). In some studies, a prediction of survival was demonstrated [12] and was introduced in the Guidelines of 2009 [16]; however, it failed to predict mortality [22] in subsequent studies, especially in NYHA III–IV and RV dilation. It predominantly mirrors longitudinal RV function and, furthermore, it is dependent on volume [22]. The longitudinal peak velocity at the basal segment of the free wall measured via tissue Doppler imaging (TDI) is another tool for assessing RV function, and tissue velocity changing at the isovolumic phase has been shown to be load-independent, in contrast to TAPSE [71]. Right ventricular size, assessed at the end-diastole, and fractional area shortening (RV-FAC) have been shown to predict survival [22]. The RV–myocardial performance index (RVMPI) is a composite measure of systolic and diastolic function. An RVMPI above 0.688 or 0.88 was predictive of survival [22, 74].
Due to the complex RV geometry, two-dimensional (2D) echocardiography cannot capture the inflow and the outflow tract in one acquisition. Real-time three-dimensional (3D) echocardiography is a very promising tool with which to quantitate RV function, as the complex RV structure is captured [23, 37]. Three-dimensional RVEF has been shown to be correlated with hemodynamics and severity in PH [32]. In addition, RV strain, especially RV longitudinal strain, has emerging potential in predicting survival in PH patients [29]. Badagliacca et al. demonstrated that RV dyssynchrony measured via 2D echo-strain had the highest predictive capability of peak V’O2, even when conventional parameters such as RV FAC were included in the multivariate analyses [3]. Lamia et al. demonstrated an impaired RV strain in borderline PAH, emphasizing the beginning of impaired RV deformation even in borderline PAH in mPAP ranges of 20–24 mm Hg [35]. Recently 3D echo free-wall strain, RVEF, and FAC were shown to serve as outcome predictors in pediatric PH patients [32].
Conclusion
Whether the reported improvements are also a consequence of improved contractility facing the presented afterload cannot be answered. However, to assess the impact of medication on the RV and especially on the load-independent contractility, measures of volume, irrespective of their importance, are misleading as they do not mirror an alteration of the inherent RV performance. Therefore, studies are needed that aim to measure the direct impact of targeted medication on the load-independent contractility, such as our ongoing Right Heart 3 Study (Clinical Trials identifier NCT03362047).
References
Andersen S, Nielsen-Kudsk JE, Vonk Noordegraaf A et al (2019) Right ventricular fibrosis. Circulation 139:269–285
Axell RG, Messer SJ, White PA et al (2017) Ventriculo-arterial coupling detects occult RV dysfunction in chronic thromboembolic pulmonary vascular disease. Physiol Rep 5(7):e13227
Badagliacca R, Papa S, Valli G et al (2017) Right ventricular dyssynchrony and exercise capacity in idiopathic pulmonary arterial hypertension. Eur Respir J 49(6):1601419. https://doi.org/10.1183/13993003.01419-2016
Badagliacca R, Poscia R, Pezzuto B et al (2015) Right ventricular remodeling in idiopathic pulmonary arterial hypertension: Adaptive versus maladaptive morphology. J Heart Lung Transplant 34:395–403
Baggen VJ, Leiner T, Post MC et al (2016) Cardiac magnetic resonance findings predicting mortality in patients with pulmonary arterial hypertension: A systematic review and meta-analysis. Eur Radiol 26:3771–3780
Bosch L, Lam CSP, Gong L et al (2017) Right ventricular dysfunction in left-sided heart failure with preserved versus reduced ejection fraction. Eur J Heart Fail 19:1664–1671
Brewis MJ, Bellofiore A, Vanderpool RR et al (2016) Imaging right ventricular function to predict outcome in pulmonary arterial hypertension. Int J Cardiol 218:206–211
Brimioulle S, Wauthy P, Ewalenko P et al (2003) Single-beat estimation of right ventricular end-systolic pressure-volume relationship. Am J Physiol Heart Circ Physiol 284:H1625–H1630
Claessen G, La Gerche A, Voigt JU et al (2016) Accuracy of echocardiography to evaluate pulmonary vascular and RV function during exercise. JACC Cardiovasc Imaging 9:532–543
De Tombe PP, Jones S, Burkhoff D et al (1993) Ventricular stroke work and efficiency both remain nearly optimal despite altered vascular loading. Am J Physiol 264:H1817–H1824
Dickstein ML, Yano O, Spotnitz HM et al (1995) Assessment of right ventricular contractile state with the conductance catheter technique in the pig. Cardiovasc Res 29:820–826
Forfia PR, Fisher MR, Mathai SC et al (2006) Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med 174:1034–1041
Fourie PR, Coetzee AR, Bolliger CT (1992) Pulmonary artery compliance: Its role in right ventricular-arterial coupling. Cardiovasc Res 26:839–844
Freed BH, Gomberg-Maitland M, Chandra S et al (2012) Late gadolinium enhancement cardiovascular magnetic resonance predicts clinical worsening in patients with pulmonary hypertension. J Cardiovasc Magn Reson 14:11
French S, Amsallem M, Ouazani N et al (2018) Non-invasive right ventricular load adaptability indices in patients with scleroderma-associated pulmonary arterial hypertension. Pulm Circ. https://doi.org/10.1177/2045894018788268
Galie N, Hoeper MM, Humbert M et al (2009) Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 34:1219–1263
García-Álvarez A, García-Lunar I, Pereda D et al (2015) Association of myocardial T1-mapping CMR with hemodynamics and RV performance in pulmonary hypertension. JACC Cardiovasc Imaging 8:76–82
Gerges M, Gerges C, Pistritto AM et al (2015) Pulmonary hypertension in heart failure. Epidemiology, right ventricular function, and survival. Am J Respir Crit Care Med 192:1234–1246
Ghuysen A, Lambermont B, Kolh P et al (2008) Alteration of right ventricular-pulmonary vascular coupling in a porcine model of progressive pressure overloading. Shock 29:197–204
Gorter TM, van Veldhuisen DJ, Voors AA et al (2018) Right ventricular-vascular coupling in heart failure with preserved ejection fraction and pre- vs. post-capillary pulmonary hypertension. Eur Heart J Cardiovasc Imaging 19:425–432
Grapsa J, Gibbs JS, Cabrita IZ et al (2012) The association of clinical outcome with right atrial and ventricular remodelling in patients with pulmonary arterial hypertension: Study with real-time three-dimensional echocardiography. Eur Heart J Cardiovasc Imaging 13:666–672
Grapsa J, Pereira Nunes MC, Tan TC et al (2015) Echocardiographic and hemodynamic predictors of survival in precapillary pulmonary hypertension: Seven-year follow-up. Circ Cardiovasc Imaging. https://doi.org/10.1161/CIRCIMAGING.114.002107
Grewal J, Majdalany D, Syed I et al (2010) Three-dimensional echocardiographic assessment of right ventricular volume and function in adult patients with congenital heart disease: Comparison with magnetic resonance imaging. J Am Soc Echocardiogr 23:127–133
Guazzi M (2018) Use of TAPSE/PASP ratio in pulmonary arterial hypertension: An easy shortcut in a congested road. Int J Cardiol 266:242–244
Guazzi M, Bandera F, Pelissero G et al (2013) Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: An index of right ventricular contractile function and prognosis. Am J Physiol Heart Circ Physiol 305:H1373–H1381
Guazzi M, Dixon D, Labate V et al (2017) RV contractile function and its coupling to pulmonary circulation in heart failure with preserved ejection fraction: Stratification of clinical phenotypes and outcomes. JACC Cardiovasc Imaging 10:1211–1221
Guazzi M, Naeije R, Arena R et al (2015) Echocardiography of right Ventriculoarterial coupling combined with cardiopulmonary exercise testing to predict outcome in heart failure. Chest 148:226–234
Hsu S, Houston BA, Tampakakis E et al (2016) Right ventricular functional reserve in pulmonary arterial hypertension. Circulation 133:2413–2422
Hulshof HG, Eijsvogels TMH, Kleinnibbelink G et al (2018) Prognostic value of right ventricular longitudinal strain in patients with pulmonary hypertension: A systematic review and meta-analysis. Eur Heart J Cardiovasc Imaging 20(4):475–484
Iles L, Pfluger H, Phrommintikul A et al (2008) Evaluation of diffuse myocardial fibrosis in heart failure with cardiac magnetic resonance contrast-enhanced T1 mapping. J Am Coll Cardiol 52:1574–1580
Inuzuka R, Hsu S, Tedford RJ et al (2018) Single-beat estimation of right ventricular contractility and its coupling to pulmonary arterial load in patients with pulmonary hypertension. J Am Heart Assoc 7(10):e7929
Jone PN, Schäfer M, Pan Z et al (2018) 3D echocardiographic evaluation of right ventricular function and strain: A prognostic study in paediatric pulmonary hypertension. Eur Heart J Cardiovasc Imaging 19:1026–1033
Kuehne T, Yilmaz S, Steendijk P et al (2004) Magnetic resonance imaging analysis of right ventricular pressure-volume loops: In vivo validation and clinical application in patients with pulmonary hypertension. Circulation 110:2010–2016
Lahm T, Douglas IS, Archer SL et al (2018) Assessment of right ventricular function in the research setting: Knowledge gaps and pathways forward. An official American Thoracic Society research statement. Am J Respir Crit Care Med 198:e15–e43
Lamia B, Muir JF, Molano LC et al (2017) Altered synchrony of right ventricular contraction in borderline pulmonary hypertension. Int J Cardiovasc Imaging 33(9):1331–1339
Levy PT, El Khuffash A, Woo KV et al (2018) Right ventricular-pulmonary vascular interactions: An emerging role for pulmonary artery acceleration time by echocardiography in adults and children. J Am Soc Echocardiogr 31:962–964
Maffessanti F, Muraru D, Esposito R et al (2013) Age-, body size-, and sex-specific reference values for right ventricular volumes and ejection fraction by three-dimensional echocardiography: A multicenter echocardiographic study in 507 healthy volunteers. Circ Cardiovasc Imaging 6:700–710
Maughan WL, Shoukas AA, Sagawa K et al (1979) Instantaneous pressure-volume relationship of the canine right ventricle. Circ Res 44:309–315
McCabe C, White PA, Hoole SP et al (2014) Right ventricular dysfunction in chronic thromboembolic obstruction of the pulmonary artery: A pressure-volume study using the conductance catheter. J Appl Physiol 116:355–363
McCabe C, White PA, Rana BS et al (2014) Right ventricle functional assessment: Have new techniques supplanted the old faithful conductance catheter? Cardiol Rev 22(5):233–240
Mewton N, Liu CY, Croisille P et al (2011) Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol 57:891–903
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 17:1321–1360
Peacock AJ, Crawley S, McLure L et al (2014) Changes in right ventricular function measured by cardiac magnetic resonance imaging in patients receiving pulmonary arterial hypertension-targeted therapy: The EURO-MR study. Circ Cardiovasc Imaging 7:107–114
Pratali L, Allemann Y, Rimoldi SF et al (2013) RV contractility and exercise-induced pulmonary hypertension in chronic mountain sickness: A stress echocardiographic and tissue Doppler imaging study. JACC Cardiovasc Imaging 6:1287–1297
Prins KW, Archer SL, Pritzker M et al (2018) Interleukin-6 is independently associated with right ventricular function in pulmonary arterial hypertension. J Heart Lung Transplant 37:376–384
Prins KW, Weir EK, Archer SL et al (2016) Pulmonary pulse wave transit time is associated with right ventricular-pulmonary artery coupling in pulmonary arterial hypertension. Pulm Circ 6:576–585
Rain S, Handoko ML, Trip P et al (2013) Right ventricular diastolic impairment in patients with pulmonary arterial hypertension. Circulation 128:2016–2025
Redington AN, Gray HH, Hodson ME et al (1988) Characterisation of the normal right ventricular pressure-volume relation by biplane angiography and simultaneous micromanometer pressure measurements. Br Heart J 59:23–30
Rex S, Missant C, Claus P et al (2008) Effects of inhaled iloprost on right ventricular contractility, right ventriculo-vascular coupling and ventricular interdependence: A randomized placebo-controlled trial in an experimental model of acute pulmonary hypertension. Crit Care (Lond) 12:R113
Richter MJ, Ghofrani HA, Gall H (2018) Beyond interleukin-6 in right ventricular function: Evidence for another biomarker. J Heart Lung Transplant 37:674–675
Sanz J, García-Alvarez A, Fernández-Friera L et al (2012) Right ventriculo-arterial coupling in pulmonary hypertension: A magnetic resonance study. Heart 98:238–243
Sato T, Ambale-Venkatesh B, Lima JAC et al (2018) The impact of ambrisentan and tadalafil upfront combination therapy on cardiac function in scleroderma associated pulmonary arterial hypertension patients: Cardiac magnetic resonance feature tracking study. Pulm Circ. https://doi.org/10.1177/2045893217748307
Shehata ML, Lossnitzer D, Skrok J et al (2011) Myocardial delayed enhancement in pulmonary hypertension: Pulmonary hemodynamics, right ventricular function, and remodeling. AJR Am J Roentgenol 196:87–94
Spruijt OA, De Man FS, Groepenhoff H et al (2015) The effects of exercise on right ventricular contractility and right ventricular-arterial coupling in pulmonary hypertension. Am J Respir Crit Care Med 191:1050–1057
Suga H, Sagawa K, Shoukas AA (1973) Load independence of the instantaneous pressure-volume ratio of the canine left ventricle and effects of epinephrine and heart rate on the ratio. Circ Res 32:314–322
Swift AJ, Capener D, Johns C et al (2017) Magnetic resonance imaging in the prognostic evaluation of patients with pulmonary arterial hypertension. Am J Respir Crit Care Med 196(2):228–239
Tedford RJ, Mudd JO, Girgis RE et al (2013) Right ventricular dysfunction in systemic sclerosis-associated pulmonary arterial hypertension. Circ Heart Fail 6:953–963
Tello K, Axmann J, Ghofrani HA et al (2018) Relevance of the TAPSE/PASP ratio in pulmonary arterial hypertension. Int J Cardiol 266:229–235
Tello K, Dalmer A, Axmann J et al (2019) Reserve of right ventricular-arterial coupling in the setting of chronic overload. Circ Heart Fail 12:e5512
Tello K, Dalmer A, Husain-Syed F et al (2019) Multi-beat right ventricular-arterial coupling during a positive acute vaso-reactivity test. Am J Respir Crit Care Med. https://doi.org/10.1164/rccm.201809-1787IM
Tello K, Dalmer A, Vanderpool R et al (2019) Cardiac magnetic resonance imaging-based right ventricular strain analysis for assessment of coupling and diastolic function in pulmonary hypertension. JACC Cardiovasc Imaging. https://doi.org/10.1016/j.jcmg.2018.12.032
Tello K, Richter MJ, Axmann J et al (2018) More on single-beat estimation of right ventriculoarterial coupling in pulmonary arterial hypertension. Am J Respir Crit Care Med 198:816–818
Trip P, Kind T, van de Veerdonk MC et al (2013) Accurate assessment of load-independent right ventricular systolic function in patients with pulmonary hypertension. J Heart Lung Transplant 32:50–55
Trip P, Rain S, Handoko ML et al (2015) Clinical relevance of right ventricular diastolic stiffness in pulmonary hypertension. Eur Respir J 45:1603–1612
van de Veerdonk MC, Huis in ’t Veld AE, Marcus JT et al (2017) Upfront combination therapy reduces right ventricular volumes in pulmonary arterial hypertension. Eur Respir J. https://doi.org/10.1183/13993003.00007-2017
van de Veerdonk MC, Kind T, Marcus JT et al (2011) Progressive right ventricular dysfunction in patients with pulmonary arterial hypertension responding to therapy. J Am Coll Cardiol 58:2511–2519
van de Veerdonk MC, Marcus JT, Westerhof N et al (2015) Signs of right ventricular deterioration in clinically stable patients with pulmonary arterial hypertension. Chest 147:1063–1071
Vanderpool RR, Desai AA, Knapp SM et al (2017) How prostacyclin therapy improves right ventricular function in pulmonary arterial hypertension. Eur Respir J. https://doi.org/10.1183/13993003.00764-2017
Vanderpool RR, Pinsky MR, Naeije R et al (2015) RV-pulmonary arterial coupling predicts outcome in patients referred for pulmonary hypertension. Heart 101:37–43
Vanderpool RR, Rischard F, Naeije R et al (2016) Simple functional imaging of the right ventricle in pulmonary hypertension: Can right ventricular ejection fraction be improved? Int J Cardiol 223:93–94
Vogel M, Schmidt MR, Kristiansen SB et al (2002) Validation of myocardial acceleration during isovolumic contraction as a novel noninvasive index of right ventricular contractility: Comparison with ventricular pressure-volume relations in an animal model. Circulation 105:1693–1699
Vonk Noordegraaf A, Chin KM, Haddad F et al (2018) Pathophysiology of the right ventricle and of the pulmonary circulation in pulmonary hypertension: An update. Eur Respir J. https://doi.org/10.1183/13993003.01900-2018
Vonk Noordegraaf A, Westerhof BE, Westerhof N (2017) The relationship between the right ventricle and its load in pulmonary hypertension. J Am Coll Cardiol 69:236–243
Wang J, Prakasa K, Bomma C et al (2007) Comparison of novel echocardiographic parameters of right ventricular function with ejection fraction by cardiac magnetic resonance. J Am Soc Echocardiogr 20:1058–1064
Wang Z, Yuan LJ, Cao TS et al (2013) Simultaneous beat-by-beat investigation of the effects of the Valsalva maneuver on left and right ventricular filling and the possible mechanism. PLoS ONE 8:e53917
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K. Tello, H. Gall, M. Richter, A. Ghofrani, and R. Schermuly declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Tello, K., Gall, H., Richter, M. et al. Right ventricular function in pulmonary (arterial) hypertension. Herz 44, 509–516 (2019). https://doi.org/10.1007/s00059-019-4815-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-019-4815-6