Abstract
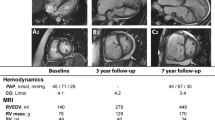
Pulmonary arterial hypertension (PAH) is a right heart failure syndrome. The dominant symptom of PAH is shortness of breath. However, in spite of widespread pulmonary vascular remodeling and obstruction, gas exchange in PAH is generally well maintained, with moderate hypoxemia mainly caused by a low cardiac output. Patients with PAH are hypocapnic, but this is explained by increased chemosensitivity, and there is no ventilatory limitation to exercise capacity. Thus lung function is normal or near-normal in PAH. The symptomatology of PAH is principally related to right ventricular (RV) failure. Right ventricular function is altered as soon as pulmonary vascular resistance increases. In early stage PAH, the RV tends to remain adapted to afterload, with little or no increase in right heart chamber dimensions, but less than optimal RV-arterial coupling is a cause of decreased aerobic exercise capacity by limiting maximum cardiac output. In more advanced stages, homeometric adaptation of the RV becomes insufficient for daily life activities resulting in a progressive dilatation of right heart chambers and systolic dysfunction. Along with decreased contractile reserve of the RV, diastolic dysfunction occurs, due to RV fibrosis and sarcomeric stiffening; these changes lead to limitation of flow output and increased right sided filling pressures. These in turn lead to a combination of systemic venous congestion and dyspnea occurring at lower levels of exercise and, eventually, at rest. Imaging of RV function is of major diagnostic and prognostic relevance. Treatment of RV failure in PAH relies on decreasing afterload with therapies targeting the pulmonary circulation, optimal fluid management of ventricular diastolic interaction, and inotropic interventions to reverse cardiogenic shock states. The potential of chronic low-dose β-blocker therapies is currently investigated.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pulmonary Hypertension
- Right Ventricular
- Pulmonary Arterial Hypertension
- Pulmonary Vascular Resistance
- Right Ventricular Function
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Pulmonary arterial hypertension (PAH) is a rare dyspnea-fatigue syndrome with clear lungs, caused by a progressive pulmonary vascular remodeling and eventual right ventricular (RV) failure [1]. The hemodynamic definition of PAH rests on invasive measurements of a mean pulmonary artery pressure (Ppa) equal or higher than 25 mmHg, a wedged Ppa (Ppw) lower than or equal to 15 mmHg and a pulmonary vascular resistance (PVR) higher than 3 Wood units. The diagnosis of PAH relies on a step-by-step work-up to exclude causal left heart conditions with increased pulmonary venous pressures, chronic lung diseases and chronic thromboembolic pulmonary hypertension (CTEPH).
Pulmonary arterial hypertension is either idiopathic or, in approximately half of the patients, associated with a series of conditions including intake of appetite suppressant drugs, connective tissue diseases (mainly systemic sclerosis), congenital cardiac left-to-right shunts, portal hypertension, schistosomiasis and human immunodeficiency viral infection [2]. Idiopathic PAH may be heritable in up to 20 % of cases.
In spite of progress with the advent of targeted therapies with prostacyclins, endothelin receptor antagonists and phosphodiesterase-5 inhibitors, PAH remains incurable, with a 3-year survival rate of 65–70 %. More basic and clinical research is needed for further improvement.
Pulmonary Gas Exchange
Shortness of breath is almost always the first and dominant symptom in PAH. Accordingly, PAH patients are often referred to chest physicians. The lungs will be found to be clear at auscultation, and the chest roentgenogram may be unremarkable. An electrocardiogram showing right ventricular strain and hypertrophy may be overlooked, and the clinical probability of acute pulmonary embolism low, or excluded by lung scintigraphy. A diagnosis of asthma is then often entertained, but excluded by lung function tests showing normal lung volumes with no or minimally increased airway obstruction. Arterial blood gases will typically show a normal or only mildly decreased arterial PO2 (PaO2) and, more constantly a decreased PaCO2, indicating preserved gas exchange [3].
The apparent paradox of extensive pulmonary vascular remodeling and preserved gas exchange has been previously explored using the multiple inert gas elimination technique at rest [4, 5] and at exercise [6]. The approach allows for a quantification of all the pulmonary and extra-pulmonary determinants of the arterial blood gases. The results have invariably shown relatively well preserved matching of alveolar ventilation (VA) to perfusion (Q), with little lower than normal VA/Q, no diffusion limitation, and mild to moderate decrease in PaO2 explained by a low mixed venous PO2 (PvO2). Significant shunting (VA/Q = 0) was found only in patients with right-to-left shunting on a patent foramen ovale or reversal of left-to-right cardiac shunts. Typical VA/Q distributions in patients with idiopathic PAH, one without and one with shunting through a patent foramen ovale, are shown in Fig. 14.1. It can be seen that the VA and Q modes remain matched, that there is no high higher than normal VA/Q thus excluding an increased physiologic dead space, and that foramen ovale in allows for shunting of 20 % of cardiac output in one of the patients as a cause of severe hypoxemia.
Thus hypoxemia in PAH is cardiac rather than pulmonary origin, in the majority of cases
Hyperventilation
Patients with PAH more are more typically hypocapnic than hypoxemic [3]. Patients with PAH hyperventilate at rest and at exercise, and even during sleep. Hyperventilation in PAH would be intuitively attributed to an increased dead space caused by extensive pulmonary vascular obliteration. However, this does not explain decreased PaCO2. Inert gas elimination studies showed a shift of mean VA/Q to higher VA/Q ratios, also illustrated in Fig. 14.1, reflecting an increased ventilation, but no higher than normal VA/Q matching, indicating absence of lung regions with relative excess of alveolar ventilation [3]. Thus wasted ventilation in PAH would rather be a consequence of increased chemosensitivity than of an increased physiologic dead space. Physiologic dead space calculated by the Bohr equation shows high values but this is entirely explained by hyperventilation [3].
Chemosensitivity is increased in PAH in proportion to disease severity [3, 7–11]. Accordingly, hypocapnia, increased ventilation to CO2 output relationships (VE/VCO2) and sympathetic nervous system hyper-activity a predictors of decreased survival in PAH [8–10], much like in congestive heart failure (CHF) [12, 13]. The reasons for increased chemosensitivity and related sympathetic nervous system activation in (right) heart failure are not exactly known. Both increased filling pressures of the right heart and altered baroreflex control are thought to be involved [11]. Increased chemosensitivity contributes to dyspnea. Sympathetic nervous system activation has deleterious effects in the long term on the heart and the pulmonary circulation.
The contributions of chemosensitivity and dead space to hyperventilation can be assessed by a graphical representation of the alveolar ventilation equation. Accordingly, VE/VCO2 is plotted as a function of either alveolar (end-expiratory) or arterial PCO2. A P(a-A)CO2 gradient of less than 5 mmHg reasonably excludes an impact of increased dead space on ventilation [3]. An increase in VE/VCO2 along with a decrease in PACO2 indicates an increased chemosensitivity, but measurements of PaCO2 are needed to identify a contribution of increased dead space [3, 11]. This is illustrated in Fig. 14.2 showing VE/VCO2 and PCO2 measurements in groups of 12 patients with PAH and 12 with CHF. In that study, the measurements in each patient were collected at the anaerobic threshold to limit the effects of relative changes in dead space with increased tidal volumes during exercise The PCO2 gradient was slightly higher than 5 mmHg in some patients with CHF, on average of 1 mmHg in patients with PAH, but with some variability, compatible with a minimal to moderate contribution of dead space on ventilation in both conditions.
Ventilation (V E ) versus CO2 output (VCO 2 ) as a function of end-tidal PCO2 (P ET CO 2 ) in normal subjects and in patients with congestive heart failure (CHF) or pulmonary arterial hypertension (PAH), left panel, and as a function of PaCO2 in patients with PAH or CHF, right panel. Increased VE/VCO2 at lower PCO2 indicates increased chemosensitivity. The gradient between PaCO2 and PETCO2 remained within the limit of normal of 5 mmHg in the majority of the patients, but with variability, indicating minimal to moderate contribution of increased dead space ventilation in both conditions
Exercise Capacity
In spite of increased ventilation, there is no ventilatory limitation to aerobic exercise capacity in patients with PAH. The cardiopulmonary exercise test (CPET) in PAH is characterized by decreased maximum workload, VO2max, VO2 at the anaerobic threshold and VO2pulse, increased VE/VCO2, increased resting but decreased maximum heart rates, and slower rates of increase and recovery of heart rate indicating altered chronotropy [7]. This is typical of a cardiac limitation to exercise capacity. Not surprisingly, CPET in patients with either PAH or CHF is similar [12, 13]. Relevant CPET measurements in patients with mild or severe PAH compared to normal subjects are shown in Fig. 14.3.
Panels showing CO2 production and heart rate as a function of oxygen uptake (VO 2 ), left, (a) and (c), and changes in VO2 as a function of changes in work rate and ventilatory equivalent for CO2 (V E /VCO 2 ) as a function of time, left, (b) and (d) in a normal subject (empty circles) and two patients with moderately severe or very severe. idiopathic pulmonary arterial hypertension (PPH). Patients with PPH have decreased maximal values for VCO2 and VO2, increased resting heart rate but decreased maximal heart rate, decreased rate of increase in VO2 as a function of rate of increase in work rate, and increased ventilatory equivalents for CO2 in proportion to disease severity (Reprinted from Sun et al. [7]. With permission from Wolters Kluwer Health)
However, patients with PAH compared to CHF patients at similar functional impairment have a relatively lower VO2max, higher VE/VCO2 and more limited increase in O2 pulse, indicating more limited increase in stroke volume contribution to increased cardiac output at exercise [13]. In both cases, the ventilatory reserve (maximum voluntary ventilation minus maximum ventilation at exercise) is normal, in the range of 40–60 L/min or more, and certainly higher than the critical level of 11 L/min diagnostic of a ventilatory limitation in patients with obstructive lung diseases.
In summary, in PAH, hypoxemia reflects a decrease in cardiac output, hypocapnia reflects increased chemosensitivity and CPET discloses a cardiac output limitation to exercise capacity. The main suspect accounting for PAH symptomatology is the RV.
Right Ventricular Failure
How does the RV fail in PAH? The normal RV is a thin-walled crescent-shape structure, designed to function as a flow generator accommodating the entire systemic venous return to the heart [14]. Its thin walls leave it vulnerable to failure with any acute rise in wall stress. A brisk increase in PVR, for example produced by pulmonary arterial constriction to mimic massive pulmonary embolism, induces acute dilatation and rapid pump failure of the RV, showing that the structure is intrinsically poorly adapted to cope with a rapid increase in afterload [15]. However, a gradually progressive increase in PVR can allow for RV adaptation and remodeling, basically like the LV facing a progressive increase in systemic vascular resistance, such as in the setting of systemic hypertension [16]. Beat-to-beat changes in preload or afterload are accompanied by a heterometric dimension adaptation described by Starling’s law of the heart. Sustained changes in load are associated with a homeometric contractility adaptation [17] referred to as Anrep’s law of the heart after the initial observation by Gleb von Anrep in 1912 of rapid increase in LV contractility in response to an aortic constriction [18].
Homeometric adaptation to afterload (that is, without chamber dilatation) has been demonstrated on RV exposed to pulmonary arterial constriction and in conditions of constant coronary perfusion [19, 20]. Failure of systolic function, or contractility, to increase in response to loading conditions results in a heterometric adaptation allowing for maintained stroke volume (SV) at the price of increased end-diastolic volume (EDV) [16]. Homeometric versus heterometric adaptations of the RV to afterload are illustrated in Fig. 14.4.
It is therefore possible to define RV failure as a dyspnea-fatigue syndrome with eventual systemic venous congestion, caused by the inability of the RV to maintain flow output in response to metabolic demand without heterometric adaptation, and consequent rise in right heart filling pressures. This definition encompasses a spectrum of clinical situations, from preserved maximum cardiac output and aerobic exercise capacity at the price of increased RV end-diastolic volumes and wall thickness (and thence raised diastolic filling pressures) to low-output states with small RV volumes at rest. This definition has been endorsed at a recent world symposium on pulmonary hypertension held in 2013, in Nice [21].
It is noteworthy that RV failure is a very late clinical finding in one particular form of PAH; that is, in Eisenmenger Syndrome (ES, where congenital cardiac left to right communications are complicated by progressive pulmonary vascular disease with eventual shunt reversal and right to left flow through the initial cardiac defect). Despite similar structural changes in the pulmonary vasculature, life expectancy in ES is decades longer than for idiopathic PAH [22]. Whereas this is in part due to the existence of a “decompressing” cardiac communication allowing the relief of excess right heart pressures, the RV likely performs better in this setting as it has never “detrained” after birth and remained hypertrophied and well adapted to pressure loading, throughout life [23].
Systolic Function of the RV
Because of the importance of homeometric adaptation of the RV in PAH, measurements have to be referred to a gold standard. In vivo, this is maximal elastance (Emax), or the maximum value of the ratio between ventricular pressure and volume measured continuously during the cardiac cycle (i.e. the “pressure-volume loop”) [16, 21]. The Emax of the LV coincides with end-systole, and is thus equal to the ratio between end-systolic pressure (ESP) and end-systolic volume (ESV) defining an end-systolic elastance (Ees). Left ventricular Ees is equal to Emax measured at the upper left corner of a square-shaped pressure-volume loop [24]. Because of naturally low pulmonary vascular impedance, however, the normal RV pressure-volume loop has a triangular rather than square shape and Emax occurs before the end of ejection, or end-systole [25]. However, a satisfactory definition of Emax can be obtained by the generation of a family of pressure-volume loops at decreasing venous return (generated, for example, by progressive inferior vena cava occlusion with balloon inflation) [25]. With increasing impedance in pulmonary hypertension, the shape of the RV pressure-volume loop changes. Pressure rises throughout ejection and peaks at or near end-systole. Maximum elastance then typically occurs at ESP like on a LV pressure-volume loop [26]. Thus the gold standard measurement of systolic function is Emax for the RV, as it is for the LV [16, 20, 27].
Instantaneous measurements of RV volumes are difficult to obtain at the bedside, and so are manipulations of venous return. This is why single beat methods have been developed, for the LV [28] and thence adapted to the RV [29]. The single beat method relies on a maximum pressure Pmax calculation from a nonlinear extrapolation of the early and late portions of a RV pressure curve, an integration of pulmonary flow and synchronization of the signals. Emax is estimated from the slope of a tangent from Pmax to the pressure-volume curve.
Examples of Pmax and Emax calculations are shown in Fig. 14.5.
Right ventricular (RV) pressure and volume curves with illustrative magnetic resonance imaging which was used for volume measurements (left) and derived maximal RV pressure (Pmax) and maximal elastance (Emax) in a normal control subject and in a patient with severe pulmonary arterial hypertension (PAH) (right). The normal subject had a Emax/Ea ratio of 1.7–2. The Emax/Ea ratio was decreased to 1 in the PAH patients, because of insufficient increase in Emax to match the increased Ea. Ves end-systolic volume. (Reprinted from Kuehne et al. [30]. With permission from Wolters Kluwer Health)
The single beat method can be applied with relative changes in volume measured by integration of ejected flow rather than with measurements of absolute volumes. This is because Emax is not dependent on preload, or EDV [16]. An excellent agreement between directly measured Pmax by clamping the main pulmonary artery for one beat and calculated Pmax has been demonstrated in a large animal experimental preparation with no pulmonary hypertension or a mild increase in Ppa induced by low oxygen breathing [29].
Measurements of RV Emax with conductance catheter technology and inferior vena cava balloon obstruction have been reported in normal volunteers [31]. A limited number of Emax determinations have been reported in patients with PAH either using the single beat approach, fluid-filled catheters and magnetic resonance imaging (MRI) [30] or a multiple beat approach with venous return decreased by a Valsalva maneuver and conductance catheters [32]. Pressure-volume loops from a patient with PAH compared to a normal control and MRI RV volume measurements are also shown in Fig. 14.5.
The single beat approach with high fidelity Millar catheters and integration of a transonic measurement of pulmonary flow were reported in a patient with a systemic RV in the setting of congenitally corrected transposition of the great arteries (where the RV is the subaortic ventricle) [33].
Most recently high-fidelity RV pressure and volume measurements and single beat Emax calculations have been reported in a small series patients with CTEPH, a condition with similar symptomatology to that of PAH [34]
These limited size reports confirm the importance of systolic function adaptation with an increased Emax to maintain RV-arterial coupling in the face of severe increases in Ppa, in agreement with previous studies in various animal species [35], or experimental models of acute [36–39] or chronic [40–43] pulmonary hypertension.
Coupling of Systolic Function to Afterload
Measurements of systolic function are ideally constant over a wide range of preload or afterload. This requirement is met by Emax in intact hearts, because this measurement is the only point of the pressure-volume curve that is common in systole to ejecting and non-ejecting beats. Therefore, Emax offers the optimal intact heart counterpart of an isolated muscle active tension length relationship. However, Emax adapts to afterload as soon as after several beats, starting after 20–30 s, with full expression of homeometric adaptation replacing initial heterometric adaptation in a couple of minutes – without requirement of a hypertrophic response [17, 19]. It is therefore important to correct Emax for afterload.
There are three possible measurements of afterload [27]. The first is maximum ventricular wall stress, which is approximated by the maximum value of the product of volume by pressure, divided by wall thickness. This is an adaptation of Laplace’s law for spherical structures, and thus problematic for the RV because of its irregular shape and thus considerable regional variations in internal radius. The second is the forces that oppose flow ejection, or hydraulic load. This calculation optimally requires a spectral analysis for the integration of arterial pressure and flow waves. The third and more straightforward approach is to derive arterial elastance (Ea) as it is “seen” by the ventricle by dividing maximal elastance pressure by SV (Fig. 14.5). The advantage of Ea to estimate afterload is that the measurement is obtained together with Emax on the same pressure-volume loop, and thus convenient to evaluate the adequacy of systolic function adaptation to afterload [16].
Thus contractility corrected for afterload is defined by a ratio of Emax to Ea. Experimental work and mathematical modeling have allowed the definition of an optimal mechanical coupling of Emax to Ea equal to one, but an optimal energy transfer from the ventricle to the arterial system at an Emax/Ea ratio of 1.5–2 [16].
RV-Arterial Coupling in Experimental Pulmonary Hypertension
RV-arterial coupling measured with the Emax/Ea ratio has been investigated in various models of pulmonary hypertension. Hypoxic pulmonary vasoconstriction, acute pulmonary microembolism, pulmonary artery banding, early stage endotoxic shock and PH on chronic aorta-pulmonary shunting were associated with a preserved RV-arterial coupling because of increased RV contractility matching the increased afterload [29, 35–40]. By contrast, insufficient increase in Emax to match increased afterload has been observed in late stage endotoxic shock [37], long-term chronic aorta-pulmonary shunting [41], monocrotaline-induced PH [42] and mild PH in overpacing-induced CHF [43].
Altogether, these studies support the notion of predominant RV systolic function adaptation to increased afterload in various models of pulmonary hypertension, but with RV-arterial uncoupling and increased RV volumes in the context of inflammation (endotoxemia, monocrotaline), long-term increase in PVR, or secondary to left heart failure.
RV-Arterial Coupling Measurements in Patients with Pulmonary Hypertension
Measurements of both Emax and Ea have been reported in a limited number of patients with PAH. In a first study on six patients with idiopathic PAH (IPAH) but no clinical RV failure, compared to six controls, Kuehne measured RV volumes with magnetic resonance imaging (MRI) and RV pressures using fluid-filled catheters, synchronized the signals and calculated Emax and Ea using the single beat method [30]. RV-arterial coupling in a patient with PAH and in a control are shown in Fig. 14.5. Emax was increased threefold, from 1.1 ± 0.1 to 2.8 ± 0.5 mmHg/ml, but Ea was increased from 0.6 ± 0.5 to 2.7 ± 0.2, so that the Emax/Ea ratio decreased from 1.9 ± 0.2 to 1.1 ± 0.1. Yet RV volumes were not increased, indicating “sufficient” coupling, at least in resting conditions.
Tedford reported on RV-arterial coupling in five patients with IPAH and seven with systemic sclerosis (SSc)-associated PAH [32]. In that study, RV volumes and pressures were measured with conductance catheters and Emax defined by a family of pressure-volume loops as venous return decreased by a Valsalva maneuver (validated against inferior vena cava obstruction). In IPAH patients, Emax was 2.3 ± 1.1, Ea 1.2 ± 0.5, and Emax/Ea preserved at 2.1 ± 1.0. In SSc-PAH patients, Emax was decreased to 0.8 ± 0.3 in the presence of an Ea at 0.9 ± 0.4, so that Emax/Ea was decreased to 1.0 ± 0.5.The authors also showed that the time constant of the pulmonary circulation, or the product of PVR by pulmonary arterial compliance, was not decreased in SSc-PAH as compared to IPAH, indicating that depressed Emax in SSc-PAH was not caused by a relatively higher pulsatile hydraulic load. Additionally, seven patients with SSc but without pulmonary hypertension maintained preserved coupling (Emax/Ea 2.3 ± 1.2). Two examples are shown in Fig. 14.6.
Right ventricular pressure-volume loops at decreasing venous return in a patient with systemic sclerosis (SSc)- associated pulmonary arterial hypertension (PAH), left, and in a patient with idiopathic PAH (IPAH), right The slope of linearized maximum elastance pressure-volume relationship is higher at similar mean pulmonary artery pressure in IPAH (Reprinted from Tedford et al. [32]. With permission from Wolters Kluwer Health)
Along with these studies on patients with PAH, there is a case report of a systemic RV in an asymptomatic young adult with a congenitally corrected transposition of the great arteries [33]. The systemic RV had a Emax of 1.26, while Ea was of 1.1 and Emax/Ea 1.2. The pulmonary LV had a Emax of 0.39 while Ea was 0.23 and Emax/Ea 1.7. In this patient, low absolute values for Emax of the pulmonary LV are related to a low pulmonary Ea, both probably in relation to the fact that the measurements were done during general anesthesia for surgical correction of an asymptomatic atrial septal defect [33].
McCabe reported on Emax and Ea measurements in ten patients with CTEPH [34]. Pressures and volumes were measured with with a conductance catheter. The results were compared with those of seven patients with thromboembolic pulmonary vascular disease (CTE) but no pulmonary hypertension and seven normal controls. In the CTEPH patients, Emax was 1.1 ± 0.4, Ea 1.9 ± 0.7 and Emax/Ea 0.6 ± 0.1. In the CTE patients Emax was 0.6 ± 0.3, Ea 0.5 ± 0.2 and Emax/Ea 1.3 ± 0.4. In the controls, Emax was 0.4 ± 0.2, Ea 0.3 ± 0.1 and Emax/Ea 1.5 ± 0.3.
Altogether, these results confirm the predominant role of homeometric adaptation of the RV to increased afterload, but uncoupling when the hydraulic load remains too high for too long time, or in the presence of systemic disease. On the methodological side, it is apparent that Emax and Ea show variability with possibly a trend to higher control values when measurements are based on families of pressure-volume loops rather than on the single beat method. RV volumes measured using a conductance catheter appear to underestimate ESV and EDV compared with MRI measurements [34]. Targeted therapies in PAH patients might also have affected these results.
In the above enumerated clinical studies, RV volumes remained normal, showing adequacy of RV-arterial coupling at rest with Emax/Ea ratios around 1 or even less. The level of RV-arterial decoupling needed to observe the onset of RV dilatation is not defined. Reported measurements were obtained at rest. Requirements of higher cardiac output at exercise probably triggers a heterometric adaptation with increased EDV to ensure sufficient RV flow output. This remains to be explored.
Patients with PAH at some point start to develop signs and symptoms of RV failure, with signs including positive hepato-jugular reflux, increased liver size, edema and ascites [1]. The pathobiological events leading to RV-arterial uncoupling and increased RV volumes remain to be identified.
The current understanding of the pathophysiology of RV failure involves neuro-humoral activation, expression of inflammatory mediators, apoptosis, capillary loss, oxidative stress and metabolic shifts, with variable fibrosis and hypertrophy [21, 44, 45]. In later stages, RV ischemia may play a role [46]. The exact sequence of events and interactions are being explored, and each has still to be referred to sound measurements of function, as illustrated in recent studies which showed inflammation and apoptosis correlated to decreased Emax/Ea in acute [47] as well as chronic [48] models of RV failure as a universal mechanism.
Pharmacology of RV-Arterial Coupling in Pulmonary Hypertension
Right ventricular function is a major determinant of quality of life, exercise capacity and outcome in PAH [1, 21]. Treatment strategies in these patients logically aim at decreasing RV afterload, often assessed by a measurement of PVR – or improvement in maximum cardiac output obtained by unloading the RV assessed by exercise capacity. However, it has been hypothesized that some of the vasodilators used for this purpose might also have intrinsic positive inotropic effects. There are data suggesting that this could be the case of prostacyclins [49] or phosphodiesterase-5 inhibitors [50]. On the other hand, treatments specifically targeting the RV are currently under consideration. The most obvious would be interventions aimed at the excessive neuro-humoral activation, which have been shown to improve survival in LV failure. Finally, patients with pulmonary hypertension may be exposed to the cardiovascular effects of general anesthesia or require treatments with inotropic drugs in case of severe RV failure [51, 52]. In all these circumstances, it is important to know the effects of the interventions on the components of RV-arterial coupling.
Catecholamines are sometimes believed to cause pulmonary vasoconstriction and to induce excessive tachycaredia [51]. Moreover, catecholamines have been associated with increased mortality in RV failure [52]. The latter effect is probably due to the fact that these drugs are prescribed in the most severely ill patients, but the data nevertheless cause concern. Low-dose dobutamine increased RV-arterial coupling by an inotropic effect without [29, 53] or with [54] a decreased afterload. Low-dose norepinephrine improved RV-arterial coupling through an exclusive positive inotropic effect, which was however less pronounced than with low-dose dobutamine [54]. Acute administration of propranolol reduced RV-arterial coupling through combined negative inotropy and pulmonary vasoconstriction during an acute hypoxic exposure [29]. Chronic administration of bisoprolol improved RV-arterial coupling by an improved contractility in monocrotaline-induced pulmonary hypertension [42]. Inhaled anesthetics worsen RV-arterial coupling by combined decrease in Emax and increase in Ea [55].
Acute administration of epoprostenol or inhaled nitric oxide improved RV-arterial coupling through exclusive pulmonary vasodilating effects in overcirculation-induced pulmonary hypertension [56]. Acute epoprostenol partially restored RV-arterial coupling through an exclusive pulmonary vascular effect in pulmonary banding-induced persistent RV failure [57] or was associated with maintained RV-arterial coupling because of decreased contractility in proportion to decreased PVR in hypoxia [58]. Levosimendan improved RV-arterial coupling through combined inotropy and vasodilation in pulmonary banding-induced persistent RV failure [53, 59]. Sildenafil improved RV-arterial coupling in hypoxia because of exclusive pulmonary vasodilating effects [60], but improved the coupling with by a positive inotropic effect in monocrotaline-induced pulmonary hypertension [61]. Bosentan had no intrinsic effect on contractility in pulmonary hypertension on 3 months of aorta-pulmonary shunting [40]. Milrinone improved RV-arterial coupling by an improved contractility in overpacing-induced congestive heart failure with mild pulmonary hypertension, while nitroprusside or inhaled nitric oxide had no effect in this model [43].
It is interesting that acute and chronic effects of interventions on RV-arterial coupling in experimental pulmonary hypertension may be quite different, as shown for β-blockers or sildenafil. This calls for testing of drugs in multiple experimental models, and extrapolation to patients with pulmonary hypertension whenever possible.
At present, there are no reports on the effects of pharmacological interventions on RV-arterial coupling in patients with PAH. One is thus limited to extrapolation from experimental animal studies, sound pathophysiological reasoning and clinical judgment.
Simplified Methods for the Measurement of RV-Arterial Coupling
Volume Measurements
A ratio of elastances can be simplified to a ratio of volumes, provided ESV is measured at the point of maximal elastance, not at the end of ejection. This is dependent on loading conditions. Pressure-volume relationships of the RV chronically exposed to increased Ppa tend to resemble LV pressure-volume loops [26], so that the approximation seems reasonable.
Sanz measured ESV and SV by MRI and showed that the SV/ESV ratio is initially preserved in patients with mild pulmonary hypertension but decreases with increasing severity of the disease [62]. A problem with the SV/ESV ratio is the inherent assumption that the ESP-ESV relationship is linear and crosses the origin. This is incorrect, because ventricular volume at a zero filling pressure has to be positive. Therefore the ESP/ESV under-estimates Emax. There could be compensation by ESV being decreased compared to the ventricular volume at the point of Emax, but probably insufficiently so in pulmonary hypertension. Thus the SV/ESV as a simple volume measurement of RV-arterial coupling requires further evaluation and estimation of functional and prognostic relevance. It can ideally be reasoned that the SV/ESV ratio includes the information of RV ejection fraction (EF), or SV/EDV in a less preload-dependent manner, but the relevance of this remains to be established.
A recent study reported on the negative impact on outcome of decreased RVEF in spite of targeted therapies-associated decreased PVR in patients with PAH [63]. While this study shows the importance of RV function in the prognostication of PAH, vasodilating therapies may be a confounding factor. Systemic vasodilating effects of targeted therapies in PAH may increase systemic venous return and increase EDV, which decreases EF if SV remains essentially unchanged, while increased cardiac output may decrease PVR without any change in the functional state of the pulmonary circulation [64]. In any case, studies such as this re-emphasise the critical role of RV function in prognosis in PAH.
Current progress in echocardiography makes more accurate measurements of the pulmonary circulation and RV function increasingly possible [65] even though precision may remain an issue for individual decision-making based on cut-off values [66]. Advances in 3-dimensional echocardiography now offer the prospect of easier bedside measurements of RV volumes, [67] and thus of EF or SV/ESV for the evaluation of RV-arterial coupling. It should be noted, however, that 3D echo estimates tend to systematically underestimate RV volumes at high values [68]
Pressure Measurements
Another simplified approach for the measurement of RV-arterial coupling introduced by Trip relies on a Pmax calculated from a RV pressure curve, which is easily obtained during a right heart catheterization, mean Ppa (mPpa) taken as a surrogate of ESP, and RV volume measurements by MRI [69]. The authors calculated Emax as (Pmax−mPpa)/(EDV−ESV) and Emax assuming V0 = 0 as mPpa/ESV. V0 is the extrapolated volume intercept of the linear best fit of a multipoint maximum elastance pressure-volume relationship. The results showed that mPpa/ESV was lower than (Pmax−mPpa)/SV, on average about half the value, while V0 ranged from –8 to 171 ml and was correlated to EDV and ESV. From this the authors concluded that V0 is dependent on RV dilatation, and thus the estimated Emax more preload-dependent than previously assumed.
An alternative explanation may be in the uncertainties of extrapolations from linear fits of relationships that have been demonstrated to be curvilinear [70]. End-systolic elastance or Emax is best determined by interpolation of pressure-volume coordinates [70], with tightening by a correction for EDV [32]. Further uncertainty is related to the use of a mPpa/SV ratio or slope of (Pmax−mPpa)/SV as a surrogate of Emax determination from single or (better) multiple beat pressure-volume relationships. Extrapolations amplify errors that are made by the use of surrogate pressures and volumes.
Alternative Methods to Evaluate RV-Arterial Coupling
The Pump Function Graph
The coupling of RV function to the pulmonary circulation can also be described by pump function curves relating mean RV pressure to SV [71]. A pump function graph is built from measurements of mean RV pressure and SV, a calculated Pmax at zero SV and a parabolic extrapolation to a zero pressure SV [21, 27]. In this representation, an increase in preload shifts the curve to greater SV with no change in shape, while an increased contractility leads to a higher Pmax with no change in maximum SV. The pump function graph helps to understand that at high PVR, a fall in pressure markedly increases SV while at low PVR pressure is more affected than SV [27].
The pump function graph has been used to demonstrate more severe RV failure at any given level of mPpa in SSc-PAH as compared to idiopathic PAH [72]. This is illustrated in Fig. 14.7.
The pump function graph of patients with idiopathic pulmonary arterial hypertension (IPAH) and patients with systemic sclerosis associated PAH (SScPAH), with indication of mean ± SEM. Stroke volume (SV) and maximal SV were not different but isovolumic right ventricular pressure (P RV ) was higher in IPAH (Reprinted from Overbeek et al. [72]. With permission from European Respiratory Society)
The limitations of the pump function graph are in its sensitivity to changes in preload and, as already mentioned, to the use of mean RV pressure or mPpa as surrogates of maximum elastance RV pressure.
The Contractile Reserve
Systolic function adaptation to afterload can also be tested dynamically to determine a contractile reserve, or the capacity to increase contractility at a given level of loading. Contractile or ventricular reserve determined using exercise or pharmacological stress tests (typically an infusion of dobutamine) has been shown to be a strong predictor of outcome in heart failure [73]. The evaluation of RV contractile reserve has not been reported until now in patients with pulmonary hypertension. In rats with pulmonary arterial banding, Emax was shown to increase to the same extent in response to 2.5 μg/kg/min than in controls, suggesting preserved systolic function in this pulmonary hypertension model [39].
A simple noninvasive approach was recently introduced by Grunig et al. [74]. In that study, Doppler echocardiography was used to measure RV systolic pressure from the maximum velocity of tricuspid regurgitation at rest and at exercise in 124 patients with either PAH or chronic thrombo-embolic pulmonary hypertension (CTEPH). An exercise-induced increase by more 30 mmHg was a strong predictor of exercise capacity and survival; the inference being that if RV contractile reserve remains good, then a pressure response to exercise can be successfully mounted despite increased afterload. Further studies will explore improved indices with incorporation of volume measurements and end-systolic pressure determinations, as this is now becoming possible using bedside noninvasive methodology.
Surrogate Measurements of RV-Arterial Coupling
Right ventricular systolic function can be estimated by a series of invasive and noninvasive measurements easily available in daily clinical practice.
Right heart catheterization allows for measurements of Ppa, right atrial pressure and cardiac output (Fick or thermodilution) and thus calculations of RV function curves such as cardiac output, SV or stroke work (SW, mean Ppa × SV). Stroke work calculated as mPpa × SV ignores the pulsatile component of work. It has been recently estimated that the pulsatile component of SW amounts to 23 % of total work independently of type and severity of pulmonary hypertension, so that total SW = 1.3 mPpa × SV [75]. This fixed relationship is explained by the constancy of the time constant of the pulmonary circulation, or PVR × pulmonary arterial compliance (Ca), or RC-time in normal subjects and in patients with pulmonary hypertension [76]. The RC-time is actually decreased in left heart failure [77] and in patients with proximal operable CTEPH [78], but increased in purely distal pulmonary micro-vascular obstruction [79]. However, the deviations are relatively mild. The pulsatile component of RVSW would vary on average from 20 to 26 %, with extremes of from 15 to 30 %. Therefore, total work is then estimated to vary between 1.2 and 1.4 times steady-flow work. The near-constancy of the RC-time thus implies a relatively stable prediction of total RVSW. It remains that right atrial pressure is an imperfect surrogate of preload, which is measured in the intact heart by an EDV.
Right ventricular contractility can be measured by preload recruitable SW (PRSW) defined by SW–EDV relationships at variable venous return [80]. The slope of PRSW has been shown to be reproducible and sensitive to changes in contractile state. However, whether PRSW is useful to evaluate RV-arterial coupling has not been clearly shown. The measurement requires invasive volume and high-fidelity pressure measurements with a manipulation of venous return, and is thus difficult to implement at the bedside.
Imaging techniques such as MRI or 3-dimensional echocardiography allow for measurements of RV volumes, ejection fraction, and SV/ESV ratios. The limitation of imaging is in the absence of direct pressure measurements. Guazzi has recently been proposed to use noninvasive echocardiographic measurements of a tricuspid annular plane excursion (TAPSE) as a measure of RV systolic function and of the maximum velocity of tricuspid regurgitation-derived systolic Ppa (SPpa) as a measure of afterload, and derive a TAPSE/SPpa ratio as an estimation of RV-arterial coupling [81]. This indirect index of RV-arterial coupling may be useful as it has been shown to predict survival in patients with left heart failure and decreased or preserved ejection fraction.
A series of imaging-derived indices of RV systolic function, such as MRI-determined EF or Doppler echocardiographic measurements of fractional area change measured in the 4-chamber view (a surrogate of EF), TAPSE, tissue Doppler imaging (TDI) of the tricuspid annulus systolic velocity S wave and isovolumic acceleration (IVA) or maximum velocity (IVV), strain or strain rate have been shown to be related to functional state and prognosis in severe pulmonary hypertension [21, 65]. Isovolumic phase indices such as the IVA or IVV are probably the less preload-dependent, and as such the closest estimates of Emax measurements [82, 83].
Diastolic Function
The present review has focused on RV systolic function and RV-arterial coupling as the essential biomechanical mechanism of ventricular function adaptation to increased afterload in PAH. However, a Starling heterometric adaptation may occur at any stage of disease progress depending on rate of progression, more or less inflammatory nature of pulmonary hypertension and systemic conditions affecting cardiac function. There is thus interest in taking into account diastolic function in the RV adaptation to pulmonary hypertension.
Diastolic function is described by a diastolic elastance curve determined by a family of pressure-volume loops at variable loading. It is curvilinear thus impossible to summarize as a single number. Several formulas have been proposed [27]. Most recently Rain reported on 21 patients with PAH in whom RV diastolic stiffness was estimated by fitting a non-linear exponential curve through the diastolic pressure-volume relationships, with the formula P = α (eVβ−1), where α is a curve fitting constant and β a diastolic stiffness constant [84]. In that study, the diastolic stiffness constant β was closely associated to disease severity. The pathogenesis of RV diastolic dysfunction was related to increased RV collagen content (ie fibrosis) and stiffness of the RV sarcomeres, in turn due to reduced phosphorylation of titin, a key protein regulating myocyte stiffness
A series of surrogate measurements of diastolic function are provided by Doppler echocardiography: isovolumic relaxation time and a decreased ratio of transmittal E and A waves or mitral annulus tissue Doppler imaging E′/A′ waves, increased right atrial or RV surface areas on apical 4-chamber views, altered eccentricity index on a parasternal short axis view, estimates of right atrial pressure from RV diastolic function indices or inferior vena cava dimensions, pericardial effusion, and the so-called Tei index, which is the ratio of isovolumetric time intervals to ventricular ejection time and thus integrates diastolic and systolic function. [65].
Ventricular Interaction
Right ventricular function has to be understood in the context of its direct and indirect interactions with LV function. Direct interaction, or ventricular interdependence, is defined as the forces that are transmitted from one ventricle to the other ventricle through the myocardium and pericardium, independent of neural, humoral or circulatory effects [85]. Diastolic ventricular interaction refers to the competition for space within indistensible pericardium when the RV dilates, which alters LV filling and may be a cause of inadequate cardiac output response to metabolic demand. Right heart catheterization and imaging studies have shown that in patients with severe pulmonary hypertension, pulmonary artery wedge pressure and LV peak filling rate are altered in proportion to decreased RV ejection fraction [86]. Systolic interaction refers to positive interaction between RV and LV contractions. It can be shown experimentally that aortic constriction, and enhanced LV contraction, markedly improves RV function in animals with pulmonary arterial banding [87]. Similarly, in electrically isolated ventricular preparations in the otherwise intact dog heart, LV contraction contributes a significant amount (~30 %) to both RV contraction and pulmonary flow [88]. This is explained by a mechanical entrainment effect, but also by LV systolic function determining systemic blood pressure which is an essential determinant of RV coronary perfusion. Increased RV filling pressures and excessive decrease in blood pressure may be a cause of RV ischemia and decreased contractility. An additional cause of negative ventricular interaction disclosed by imaging studies is asynchrony, which has been shown to develop in parallel to increased pulmonary artery pressures, and contributes to altered RV systolic function and LV under-filling [89].
A Global View on RV Failure
Thus pulmonary hypertension increases RV afterload requiring a homeometric adaptation. When this adaptation fails, the RV enlarges, decreasing LV preloading because of competition for space within the pericardium. This decreases stroke volume and blood pressure, with negative systolic interaction as a cause of further RV-arterial uncoupling, which may be aggravated by RV ischemia from decreased coronary perfusion pressure (gradient between diastolic blood pressure and right atrial pressure).
As shown below, in Fig. 14.8, these interactions may allow one to identify targets of interventions: (1) increased PVR (prostacyclins, phosphodiesterase-5 inhibitors, inhaled NO, endothelin receptor antagonists…) (2) relative insufficiency of RV contractility (dobutamine) (3) excessive RV preload (diuretics) and systemic hypotension (norepinephrine).
Conclusions
In 1989 Jack Reeves called for more research on the pathophysiology and pathobiology of RV failure in pulmonary hypertension. It was already known at his time that pulmonary hypertension is a common complication of cardiac and pulmonary diseases, and that symptoms, exercise capacity and outcome in patients are considerably influenced by RV function. Yet, he had to deplore that the RV was getting insufficient attention in clinical and basic research programs on the pulmonary circulation [90].
The awareness of the importance of the RV in PAH has made considerable progress. There is nowadays a clearer view of the RV and the pulmonary circulation as a functional unit, and imaging is being used with improved focus on functional relevance. Robust measurements of RV-arterial coupling allows for the identification of pulmonary vascular versus RV myocardial effects of therapeutic interventions, and could serve as indispensable tools for bedside translation of cell and molecular biological discoveries.
A lot of work remains to be done to identify the most relevant measurements of RV function and RV-arterial coupling, including awareness of those that can be applied easily in clinical practice, as well as in a research setting. What is thus needed is measurements that are noninvasive, easy to implement at the bedside and in outpatient clinics, and which physiologically meaningful. At present, it appears that 3D echocardiography with portable devices offers the best perspective, as discussed in Chap. 8.
References
McLaughlin VV, Archer SL, Badesch DB, Barst RJ, Farber HW, Lindner JR, Mathier MA, McGoon MD, Park MH, Rosenson RS, Rubin LJ, Tapson VF, Varga J, Harrington RA, Anderson JL, Bates ER, Bridges CR, Eisenberg MJ, Ferrari VA, Grines CL, Hlatky MA, Jacobs AK, Kaul S, Lichtenberg RC, Lindner JR, Moliterno DJ, Mukherjee D, Pohost GM, Rosenson RS, Schofield RS, Shubrooks SJ, Stein JH, Tracy CM, Weitz HH, Wesley DJ. ACCF/AHA 2009 expert consensus document on pulmonary hypertension. A Report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association. Circulation. 2009;119:2250–94.
Simonneau G, Gatzoulis MA, Adatia I, Celermajer D, Denton C, Ghofrani A, Gomez Sanchez MA, Krishna Kumar R, Landzberg M, Machado RF, Olschewski H, Robbins IM, Souza R. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D34–41.
Mélot C, Naeije R. Pulmonary vascular diseases. Compr Physiol. 2011;1:593–619.
Dantzker DR, Bower JE. Mechanisms of gas exchange abnormality in patients with chronic obliterative pulmonary vascular disease. J Clin Invest. 1979;64:1050–5.
Mélot C, Naeije R, Mols P, Vandenbossche JL, Denolin H. Effects of nifedipine on ventilation/perfusion matching in primary pulmonary hypertension. Chest. 1983;83:203–7.
Dantzker DR, D’Alonzo GE, Bower JS, Popat K, Crevey BJ. Pulmonary gas exchange during exercise in patients with chronic obliterative pulmonary hypertension. Am Rev Respir Dis. 1984;130:412–6.
Sun XG, Hansen EJ, Oudiz R, Wasserman K. Exercise pathophysiology in patients with primary pulmonary hypertension. Circulation. 2001;104:429–35.
Hoeper MM, Pletz H, Welte T. Prognostic values of blood gas analyses in patients with idiopathic pulmonary arterial hypertension. Eur Respir J. 2007;29:944–50.
Ciarka A, Doan V, Velez-Roa S, Naeije R, van de Borne P. Prognostic significance of sympathetic nervous system activation in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2010;181:1269–75.
Deboeck G, Scoditti C, Huez S, Vachiéry JL, Lamotte M, Sharples L, Melot C, Naeije R. Exercise testing to predict outcome in idiopathic versus associated pulmonary arterial hypertension. Eur Respir J. 2012;40:1410–9.
Naeije R, van de Borne P. Clinical relevance of autonomic nervous system disturbances in pulmonary arterial hypertension. Eur Respir J. 2009;34:792–4.
Arena R, Myers J, Guazzi M. The clinical and research applications of aerobic capacity and ventilatory efficiency in heart failure: an evidence-based review. Heart Fail Rev. 2008;13:245–69.
Deboeck G, Niset G, Lamotte M, Vachiéry JL, Naeije R. Cardiopulmonary exercise testing in pulmonary arterial hypertension and in congestive heart failure: what are the differences? Eur Respir J. 2004;23:747–51.
Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, Part I. Anatomy, physiology, aging and functional assessment of the right ventricle. Circulation. 2008;117:1436–48.
Guyton AC, Lindsey AW, Gilluly JJ. The limits of right ventricular compensation following acute increase in pulmonary circulatory resistance. Circ Res. 1954;2:326–32.
Sagawa K, Maughan L, Suga H, Sunagawa K. Cardiac contraction and the pressure-volume relationship. New York: Oxford University Press; 1988.
Sarnoff SJ, Mitchell JH, Gilmore JP, Remensnyder JP. Homeometric autoregulation of the heart. Circ Res. 1960;8:1077–91.
von Anrep G. On the part played by the suprarenals in the normal vascular reactions of the body. J Physiol. 1912;45:307–17.
Rosenblueth A, Alanis J, Lopez E, Rubio R. The adaptation of ventricular muscle to different circulatory conditions. Arch Int Physiol Biochim. 1959;67:358–73.
Taquini AC, Fermoso JD, Aramendia P. Behaviour of the right ventricle following acute constriction of the pulmonary artery. Circ Res. 1960;8:315–8.
Vonk-Noordegraaf A, Haddad F, Chin KM, Forfia PR, Kawut SM, Lumens J, Naeije R, Newman J, Oudiz RJ, Provencher S, Torbicki A, Voelkel NF, Hassoun PM. Right heart adaptation to pulmonary arterial hypertension: physiology and pathobiology. J Am Coll Cardiol. 2013;62(25 Suppl):D22–33.
Hopkins WE, Ochoa LL, Richardson GW, Trulock EP. Comparison of the hemodynamics and survival of adults with severe primary pulmonary hypertension or Eisenmenger syndrome. J Heart Lung Transplant. 1996;15:100–5.
Beghetti M, Galiè N. Eisenmenger syndrome a clinical perspective in a new therapeutic era of pulmonary arterial hypertension. J Am Coll Cardiol. 2009;53:733–40.
Suga H, Sagawa K, Shoukas AA. Load independence of the instantaneous pressure-volume ratio of the canine left ventricle and effects of epinephrine and heart rate on the ratio. Circ Res. 1973;32:314–22.
Maughan WL, Shoukas AA, Sagawa K, Weisfeldt ML. Instantaneous pressure-volume relationship of the canine right ventricle. Circ Res. 1979;44:309–15.
Redington AN, Rigby RL, Shinebourne EA, Oldershaw PJ. Changes in pressure-volume relation of the right ventricle when its loading conditions are modified. Br Heart J. 1990;63:45–9.
Vonk-Noordegraaf A, Westerhof N. Describing right ventricular function. Eur Respir J. 2013;41:1419–23.
Sunagawa K, Yamada A, Senda Y, Kikuchi Y, Nakamura M, Shibahara T. Estimation of the hydromotive source pressure from ejecting beats of the left ventricle. IEEE Trans Biomed Eng. 1980;57:299–305.
Brimioulle S, Wauthy P, Ewalenko P, Rondelet B, Vermeulen F, Kerbaul F, Naeije R. Single-beat estimation of right ventricular end-systolic pressure-volume relationship. Am J Physiol Heart Circ Physiol. 2003;284:H1625–30.
Kuehne T, Yilmaz S, Steendijk P, Moore P, Groenink M, Saaed M, Weber O, Higgins CB, Ewert P, Fleck E, Nagel E, Schulze-Neick I, Lange P. Magnetic resonance imaging analysis of right ventricular pressure-volume loops: in vivo validation and clinical application in patients with pulmonary hypertension. Circulation. 2004;110:2010–6.
Dell’Italia LJ, Walsh RA. Application of a time-varying elastance model to right ventricular performance in man. Cardiovasc Res. 1988;22:864–74.
Tedford RJ, Mudd JO, Girgis RE, Mathai SC, Zaiman AL, Housten-Harris T, Boyce D, Kelemen BW, Bacher AC, Shah AA, Hummers LK, Wigley FM, Russell SD, Saggar R, Saggar R, Maughan WL, Hassoun PM, Kass DA. Right ventricular dysfunction in systemic sclerosis associated pulmonary arterial hypertension. Circ Heart Fail. 2013;6:953–63.
Wauthy P, Naeije R, Brimioulle S. Left and right ventriculo-arterial coupling in a patient with congenitally corrected transposition. Cardiol Young. 2005;15:647–9.
McCabe C, White PA, Hoole SP, Axell RG, Priest AN, Gopalan D, Taboada D, Mackenzie Ross RV, Morrell NW, Shapiro LM, Pepke-Zaba J. Right Ventricular dysfunction in chronic thromboembolic obstruction of the pulmonary artery. J Appl Physiol. 2014;116:355–63.
Wauthy P, Pagnamenta A, Vassali F, Brimioulle S, Naeije R. Right ventricular adaptation to pulmonary hypertension. An interspecies comparison. Am J Physiol Heart Circ Physiol. 2004;286:H1441–7.
de Vroomen M, Cardozo RH, Steendijk P, van Bel F, Baan J. Improved contractile performance of right ventricle in response to increased RV afterload in newborn lamb. Am J Physiol Heart Circ Physiol. 2000;278:H100–5.
Lambermont B, Ghuysen A, Kolh P, Tchana-Sato V, Segers P, Gérard P, Morimont P, Magis D, Dogné JM, Masereel B, D’Orio V. Effects of endotoxic shock on right ventricular systolic function and mechanical efficiency. Cardiovasc Res. 2003;59:412–8.
Leeuwenburgh BP, Helbing WA, Steendijk P, Schoof PH, Baan J. Biventricular systolic function in young lambs subject to chronic systemic right ventricular pressure overload. Am J Physiol Heart Circ Physiol. 2001;281:H2697–704.
Faber MJ, Dalinghaus M, Lankhuizen IM, Steendijk P, Hop WC, Schoemaker RG, Duncker DJ, Lamers JM, Helbing WA. Right and left ventricular function after chronic pulmonary artery banding in rats assessed with biventricular pressure-volume loops. Am J Physiol Heart Circ Physiol. 2006;291:H1580–6.
Rondelet B, Kerbaul F, Motte S, Van Beneden R, Remmelink M, Brimioulle S, Mc Entee K, Wauthy P, Salmon I, Ketelslegers JM, Naeije R. Bosentan for the prevention of overcirculation-induced pulmonary hypertension. Circulation. 2003;107:1329–35.
Rondelet B, Dewachter C, Kerbaul F, Kang X, Fesler P, Brimioulle S, Naeije R, Dewachter L. Prolonged overcirculation-induced pulmonary arterial hypertension as a cause of right ventricular failure. Eur Heart J. 2012;33:1017–26.
de Man FS, Handoko ML, van Ballegoij JJ, Schalij I, Bogaards SJ, Postmus PE, der Velden J, Westerhof N, Paulus WJ, Vonk-Noordegraaf A. Bisoprolol delays progression towards right heart failure in experimental pulmonary hypertension. Circ Heart Fail. 2012;5:97–105.
Pagnamenta A, Dewachter C, McEntee K, Fesler P, Brimioulle S, Naeije R. Early right ventriculo-arterial uncoupling in borderline pulmonary hypertension on experimental heart failure. J Appl Physiol. 2010;109:1080–5.
Bogaard HJ, Abe K, Vonk Noordegraaf A, Voelkel NF. The right ventricle under pressure. Cellular and molecular mechanisms of right heart failure in pulmonary hypertension. Chest. 2009;135:794–804.
Voelkel NF, Gomez-Arroyo J, Abbate A, Bogaard HJ. Mechanisms of right heart failure – a work in progress and plea for further prevention. Pulm Circ. 2013;3:137–43.
Gómez A, Bialostozky D, Zajarias A, Santos E, Palomar A, Martínez ML, Sandoval J. Right ventricular ischemia in patients with primary pulmonary hypertension. J Am Coll Cardiol. 2001;38:1137–41.
Dewachter C, Dewachter L, Rondelet B, Fesler P, Brimioulle S, Kerbaul F, Naeije R. Activation of apoptotic pathways in experimental acute afterload-induced right ventricular failure. Crit Care Med. 2010;38:1405–13.
Belhaj A, Dewachter L, Kerbaul F, Brimioulle S, Dewachter C, Naeije R, Rondelet B. Heme oxygenase-1 and inflammation in experimental right ventricular failure on prolonged overcirculation-induced pulmonary hypertension. PLoS One. 2013;8:e69470.
Rich S, McLaughlin VV. The effects of chronic prostacyclin therapy on cardiac output and symptoms in primary pulmonary hypertension. J Am Coll Cardiol. 1999;34:1184–7.
Nagendran J, Archer SL, Soliman D, Gurtu V, Moudgil R, Haromy A, St Aubin C, Webster L, Rebeyka IM, Ross DB, Light PE, Dyck JR, Michelakis ED. Phosphodiesterase type 5 is highly expressed in the hypertrophied human right ventricle, and acute inhibition of phosphodiesterase type 5 improves contractility. Circulation. 2007;116:238–48.
Hoeper MM, Granton J. Intensive care unit management of patients with severe pulmonary hypertension and right heart failure. Am J Respir Crit Care Med. 2011;184:1114–24.
Sztrymf B, Günther S, Artaud-Macari E, Savale L, Jaïs X, Sitbon O, Simonneau G, Humbert M, Chemla D. Left ventricular ejection time in acute heart failure complicating pre-capillary pulmonary hypertension. Chest. 2013;144(5):1512–20.
Kerbaul F, Rondelet B, Demester JP, Fesler P, Huez S, Naeije R, Brimioulle S. Effects of levosimendan versus dobutamine on pressure load-induced right ventricular failure. Crit Care Med. 2006;34:2814–9.
Kerbaul F, Rondelet B, Motte S, Fesler P, Hubloue I, Ewalenko P, Naeijer R, Brimioulle S. Effects of norepinephrine and dobutamine on pressure load-induced right ventricular failure. Crit Care Med. 2004;32:1035–40.
Kerbaul F, Rondelet B, Motte S, Fesler P, Hubloue I, Ewalenko P, Naeije R, Brimioulle S. Isoflurane and desflurane impair right ventricular-pulmonary arterial coupling in dogs. Anesthesiology. 2004;101:1357–61.
Wauthy P, Kafi AS, Mooi W, Naeije R, Brimioulle S. Effects of nitric oxide and prostacyclin in an over-circulation model of pulmonary hypertension. J Thorac Cardiovasc Surg. 2003;125:1430–7.
Kerbaul F, Brimioulle S, Rondelet B, Dewachter C, Hubloue I, Naeije R. How prostacyclin improves cardiac output in right heart failure in conjunction with pulmonary hypertension. Am J Respir Crit Care Med. 2007;175:846–50.
Rex S, Missant C, Segers P, Rossaint R, Wouters PF. Epoprostenol treatment of acute pulmonary hypertension is associated with a paradoxical decrease in right ventricular contractility. Intensive Care Med. 2008;34:179–89.
Missant C, Rex S, Segers P, Wouters PF. Levosimendan improves right ventriculovascular coupling in a porcine model of right ventricular dysfunction. Crit Care Med. 2007;35:707–15.
Fesler P, Pagnamenta A, Rondelet B, Kerbaul F, Naeije R. Effects of sildenafil on hypoxic pulmonary vascular function in dogs. J Appl Physiol. 2006;101:1085–90.
Borgdorff MA, Bartelds B, Dickinson MG, Boersma B, Weij M, Zandvoort A, Silié HH, Steendijk P, de Vroomen M, Berger RM. Sildenafil enhances systolic adaptation, but does not prevent diastolic dysfunction, in the pressure-loaded right ventricle. Eur J Heart Fail. 2012;14:1067–74.
Sanz J, García-Alvarez A, Fernández-Friera L, Nair A, Mirelis JG, Sawit ST, Pinney S, Fuster V. Right ventriculo-arterial coupling in pulmonary hypertension: a magnetic resonance study. Heart. 2012;98:238–43.
van de Veerdonk MC, Kind T, Marcus JT, Mauritz GJ, Heymans MW, Bogaard HJ, Boonstra A, Marques KM, Westerhof N, Vonk-Noordegraaf A. Progressive right ventricular dysfunction in patients with pulmonary arterial hypertension responding to therapy. J Am Coll Cardiol. 2011;58:2511–9.
Sniderman AD, Fitchett DH. Vasodilators and pulmonary arterial hypertension: the paradox of therapeutic success and clinical failure. Int J Cardiol. 1988;20:173–81.
Bossone E, D’Andrea A, D’Alto M, Citro R, Argiento P, Ferrara F, Cittadini A, Rubenfire M, Naeije R. Echocardiography in pulmonary arterial hypertension. J Am Soc Echocardiogr. 2013;26:1–14.
D’Alto M, Romeo E, Argiento P, D’Andrea A, Vanderpool R, Correra A, Bossone E, Sarubbi B, Calabrò R, Russo MG, Naeije R. Accuracy and precision of echocardiography versus right heart catheterization for the assessment of pulmonary hypertension. Int J Cardiol. 2013;168(4):4058–62.
Zhang QB, Sun JP, Gao RF, Lee APW, Feng YL, Liu XR, Sheng W, Liu F, Yu CM. Feasibility of single-beat full volume capture real-time three-dimensional echocardiography for quantification of right ventricular volume: validation by cardiac magnetic resonance imaging. Int J Cardiol. 2013;168(4):3991–5.
Crean AM, Maredia N, Ballard G, Menezes R, Wharton G, Forster J, Greenwood JP, Thomson JD. 3D Echo systematically underestimates right ventricular volumes compared to cardiovascular magnetic resonance in adult congenital heart disease patients with moderate or severe RV dilatation. J Cardiovasc Magn Reson. 2011;13:78.
Trip P, Kind T, van de Veerdonk MC, Marcus JT, de Man FS, Westerhof N, Vonk-Noordegraaf A. Accurate assessment of load-independent right ventricular systolic function in patients with pulmonary hypertension. J Heart Lung Transplant. 2013;32:50–5.
Kass DA, Beyar R, Lankford E, Heard M, Maughan WL, Sagawa K. Influence of contractile state on the curvilinearity of in situ end-systolic pressure-volume relationships. Circulation. 1989;79:167–78.
Elzinga G, Westerhof N. The effect of an increase in inotropic state and end-diastolic volume on the pumping ability of the feline left heart. Circ Res. 1978;42:620–8.
Overbeek MJ, Lankhaar JW, Westerhof N, Voskuyl AE, Boonstra A, Bronzwaer JG, Marques KM, Smit EF, Dijkmans BA, Vonk-Noordegraaf A. Right ventricular contractility in systemic sclerosis-associated and idiopathic pulmonary arterial hypertension. Eur Respir J. 2008;31:1160–6.
Haddad F, Vrtovec B, Ashley EA, Deschamps A, Haddad H, Denault AY. The concept of ventricular reserve in heart failure and pulmonary hypertension: an old metric that brings us one step closer in our quest for prediction. Curr Opin Cardiol. 2011;26:123–31.
Grünig E, Tiede H, Enyimayew EO, Ehlken N, Seyfarth HJ, Bossone E, D’Andrea A, Naeije R, Olschewski H, Ulrich S, Nagel C, Halank M, Fischer C. Assessment and prognostic relevance of right ventricular contractile reserve in patients with pulmonary arterial hypertension. Circulation. 2013;128:2005–15.
Saouti N, Westerhof N, Helderman F, Marcus JT, Boonstra A, Postmus PE, Vonk-Noordegraaf A. Right ventricular oscillatory power is a constant fraction of total power irrespective of pulmonary artery pressure. Am J Respir Crit Care Med. 2010;182:1315–20.
Lankhaar JW, Westerhof N, Faes TJ, Gan CT, Marques KM, Boonstra A, van den Berg FG, Postmus PE, Vonk-Noordegraaf A. Pulmonary vascular resistance and compliance stay inversely related during treatment of pulmonary hypertension. Eur Heart J. 2008;29:1688–95.
Tedford RJ, Hassoun PM, Mathai SC, Girgis RE, Russell SD, Thiemann DR, Cingolani OH, Mudd JO, Borlaug BA, Redfield MM, Lederer DJ, Kass DA. Pulmonary capillary wedge pressure augments right ventricular pulsatile loading. Circulation. 2012;125:289–97.
Mackenzie Ross RV, Toshner MR, Soon E, Naeije R, Pepke-Zaba J. Decreased time constant of the pulmonary circulation in chronic thromboembolic pulmonary hypertension. Am J Physiol Heart Circ Physiol. 2013;15(305):H259–64.
Pagnamenta A, Vanderpool RR, Brimioulle S, Naeije R. Proximal pulmonary arterial obstruction decreases the time constant of the pulmonary circulation and increases right ventricular afterload. J Appl Physiol. 2013;114:1586–92.
Karunanithi MK, Michniewicz J, Copeland SE, Feneley MP. Right ventricular preload recruitable stroke work, end-systolic pressure-volume, and dP/dtmax-end-diastolic volume relations compared as indexes of right ventricular contractile performance in conscious dogs. Circ Res. 1992;70:1169–79.
Guazzi M, Bandera F, Pelissero G. Tricuspid annular systolic excursion and pulmonary systolic pressure relationship in heart failure: an index of right ventricular contractility and prognosis. Am J Physiol Heart Circ Physiol. 2013;305(9):H1373–81.
Vogel M, Schmidt MR, Christiansen SB, Cheung M, White PA, Sorensen K, Redington AN. Validation of myocardial acceleration during isovolumic contraction as a novel non-invasive index of right ventricular contractility. Circulation. 2002;105:1693–9.
Ernande L, Cottin V, Leroux PY, Girerd N, Huez S, Mulliez A, Bergerot C, Ovize M, Mornex JF, Cordier JF, Naeije R, Derumeaux G. Right isovolumic contraction velocity predicts survival in pulmonary hypertension. J Am Soc Echocardiogr. 2013;26:297–306.
Rain S, Handoko ML, Trip P, Gan TJ, Westerhof N, Stienen G, Paulus WJ, Ottenheijm C, Marcus JT, Dorfmuller P, Guignabert C, Humbert M, Macdonald P, Dos Remedios C, Postmus PE, Saripalli C, Hidalgo CG, Granzier HL, Vonk-Noordegraaf A, van der Velden J, de Man FS. Right ventricular diastolic impairment in patients with pulmonary arterial hypertension. Circulation. 2013;128(18):2016–25.
Santamore WP, Dell’Italia LJ. Ventricular interdependence: significant left ventricular contributions to right ventricular systolic function. Prog Cardiovasc Dis. 1998;40:289–308.
Lazar JM, Flores AR, Grandis DJ, Orie JE, Schulman DS. Effects of chronic right ventricular pressure overload on left ventricular diastolic function. Am J Cardiol. 1993;72:1179–82.
Belenkie I, Horne SG, Dani R, Smith ER, Tyberg JV. Effects of aortic constriction during experimental acute right ventricular pressure loading. Further insights into diastolic and systolic ventricular interaction. Circulation. 1995;92:546–54.
Damiano Jr RJ, La Follette P, Cox Jr JL, Lowe JE, Santamore WP. Significant left ventricular contribution to right ventricular systolic function. Am J Physiol. 1991;261(5 Pt 2):H1514–24.
Marcus JT, Gan CT, Zwanenburg JJ, Boonstra A, Allaart CP, Götte MJ, Vonk-Noordegraaf A. Interventricular mechanical asynchrony in pulmonary arterial hypertension: left-to-right delay in peak shortening is related to right ventricular overload and left ventricular underfilling. J Am Coll Cardiol. 2008;51:750–7.
Reeves JT, Groves BM, Turkevich D, Morrisson DA, Trapp JA. Chapter 10. Right ventricular function in pulmonary hypertension. In: Weir EK, Reeves JT, editors. Pulmonary vascular physiology and physiopathology. New York: Marcel Dekker; 1989. p. 325–51.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Naeije, R., Lau, E.M.T., Celermajer, D.S. (2014). Assessment and Clinical Relevance of Right Ventricular Failure in Pulmonary Arterial Hypertension. In: Gaine, S., Naeije, R., Peacock, A. (eds) The Right Heart. Springer, London. https://doi.org/10.1007/978-1-4471-2398-9_14
Download citation
DOI: https://doi.org/10.1007/978-1-4471-2398-9_14
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-2397-2
Online ISBN: 978-1-4471-2398-9
eBook Packages: MedicineMedicine (R0)