Abstract
The purpose of this study is to describe both clinical and immunological features in large cohort of adult patients with IgG subclass deficiency, and response to immunoglobulin therapy. This is a retrospective study of data obtained from electronic medical records and paper charts of 78 patients with IgG subclass deficiency seen and followed at our immunology clinics from 2010 to 2016. Both isolated selective IgG subclass deficiency as well as combined (two) subclass deficiencies were observed. IgG3 subclass deficiency, isolated and in combination with other IgG subclass deficiency, is the most frequent of IgG subclass deficiency. A majority of patients presented with upper and lower respiratory tract infections, especially chronic sinusitis. Both allergic and autoimmune manifestations are common; however, there is no subclass preference. The proportions and absolute numbers of CD3+ T cells, CD4+ T and CD8+ T cells, CD19+ B cells, and CD3−CD16+CD56+ NK cells were normal in the majority of patients in all IgG subclass deficiencies. Total serum IgG levels did not correlate with IgG subclass levels across all IgG subclass deficiencies. Anti-pneumococcal polysaccharide antibody responses were impaired in 56% of patients. IgG3 subclass deficiency is the most common IgG subclass deficiency, and anti-polysaccharide antibody responses are distributed among IgG subclasses with modest preference in IgG2 subclass. The majority of patients treated with immunoglobulin responded by reduction in frequency of infections and requirement of antibiotics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
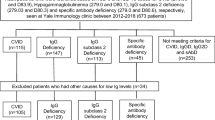
Grey and Kunkel (1964) identified four subclasses of immunoglobulin G (IgG), which were designated as γG1, γG2, γG3, and γG4. Later, their structural and biological differences were defined (Natvig et al. 1967; Kronvall and Williams 1969). IgG subclass deficiency was first described by William Terry (1968) in a patient associated with recurrent infections. Selective IgG subclass is defined by a significant decrease (below 2 SD of mean) in the serum concentrations of one or more subclasses of IgG with normal total IgG, IgA, and IgM levels. In 2009, we published clinical and immunological features of 15 patients with IgG3 subclass deficiency, and reported the beneficial effect of immunoglobulin therapy in symptomatic patients who demonstrated impaired specific anti-pneumococcal polysaccharide antibody responses (Abrahamian et al. 2010). IgG subclass deficiency has been described in association with several other primary immunodeficiency, including selective IgA deficiency, selective IgM deficiency, and ataxia–telangiectasia (Kalfa et al. 2003; Oxelius et al. 1981, 1982; Plebani et al. 1986; Yel et al. 2009), and secondary immunodeficiency diseases, including growth hormone deficiency, Down syndrome, cystic fibrosis (Annerén et al. 1992; Garside et al. 2005; Wilson et al. 1990), and those associated with the use of certain pharmacological agents (Ishizaka et al. 1992; Kato et al. 2003; Klaustermeyer et al. 1992; Leickly and Buckley 1986; Maeoka et al. 1997). In this retrospective study, we describe clinical and immunological features of 78 adult patients with reproducible selective IgG subclass deficiency (determinations made on two separate occasions at more than 1 month apart), and response to immunoglobulin therapy; other primary immunodeficiencies, secondary immunodeficiency diseases, and use of pharmacological agents known to be associated with IgG subclass deficiency were excluded from the analysis.
Materials and Methods
Study Design
This is a retrospective study of adult patients with a diagnosis of IgG subclass deficiency seen in Immunology Clinics at University of California at Irvine between the years 1998–2016. Institutional Review Board (Human) of the University of California, Irvine approved this study.
An electronic medical record (EMR) search was performed to identify patients with IgG subclass deficiency as defined by the presence of reproducible decreases in one or more IgG subclasses, with normal total IgG, IgM, and IgA. For those patients whose diagnoses were given prior to the use of EMR, paper charts were obtained and reviewed. Clinical characteristics such as infectious history and history of allergic, autoimmune, and malignant disease were recorded. Patients that had reproducible low levels of IgG subclass (es), on two separate occasions, at least 1 month apart, and measured when patients had no acute infections, were included. IgG subclass deficiency was diagnosed with levels < 2SD below the mean for controls. None of the patients were on any medications, including steroids, immunosuppressive agents, and anti-epileptics, known to produce Ig or IgG subclass deficiencies. Patients with lupus, rheumatoid arthritis, and undifferentiated mixed connective diseases were receiving Plaquenil. None of the asthma patients were on steroids. None of the patients had renal disease or proteinuria.
Laboratory data at the time of diagnosis and prior to intravenous immunoglobulin (IVIG) therapy were retrospectively gathered. Total serum IgG, IgG subclasses, IgA, and IgM were measured by nephelometry, and CD3+ (T cells), CD3+CD4+ (CD4 T cells), CD3+CD8+ (CD8 T cells), CD19+ (B cells), and CD3−CD16+CD56+ (NK cells) cells were assayed by flow cytometry with specific monoclonal antibodies and isotype controls. Complement C3, C4, (ELISA) and CH50 (functional assay) levels, and tetanus and diphtheria IgG antibodies by ELISA assay. All these tests were performed by CLIA-certified laboratories in the Department of Pathology of our institution. All normal ranges are from healthy normal donors of both genders (a requirement for CLIA-certified laboratory).
Proliferative responses of lymphocytes to recall antigens (mumps, Candida albicans, tetanus toxoid) and mitogens (PHA, Con A, PWM) were measured by 3H thymidine incorporation, and pre and 4 weeks post-vaccination (with Pneumovax-23), pneumococcal polysaccharide antibody titers were measured using multiplexed immunoassay (that remove cross-reactive antibodies) which were performed by ARUP Laboratories (Salt Lake City, UT, USA). Impaired response to Pneumovax-23 vaccine was considered if the post-vaccination titers were unprotected (< 1.3 μg/ml) or less than twofold increase over pre-vaccination titers. Normal ranges for serum immunoglobulins and lymphocyte subsets are as follows: serum immunoglobulins (mg/dl); IgM: 48–271, IgA: 81–463, IgG: 694–1618, IgG1: 342–1117, IgG2: 147–525, IgG3: 21–114, IgG4: 7–161; Lymphocyte phenotype % (absolute numbers): CD3+ (T cells): 57–85 (840–3060), CD3+CD4+ (T helper cells): 30–61 (490–1470), CD3+CD8+ (cytotoxic T cells): 12–42 (180–1170), CD19+CD3− (B cells): 6–29 (110–660), and CD3−CD16+CD56+ (NK cells): 4–25 (70–760).
Statistical analysis was done by one-way ANOVA, Brown–Forsythe test, linear regression, and unpaired T test using PRISM 7 software.
For patients on immunoglobulin treatment, dose and route of immunoglobulin administration, number of infections, severity of infections (pneumonia, meningitis) that required hospitalization, courses of antibiotics per year, and subjective patient response determined clinical responses were recorded.
Results
The demographic and clinical features of 78 adult patients with IgG subclass deficiency are summarized in Table 1.
Distribution of IgG Subclass Deficiencies
The most common subclass deficiency was isolated selective IgG3 deficiency followed by selective IgG1 subclass deficiency, and the least common was isolated selective IgG4 deficiency. In addition, combined IgG subclass deficiencies were identified. IgG3 subclass deficiency alone, and in combination with other subclasses was the most common subclass deficiency comprising of 50% of all IgG subclass deficiency patients. Serum levels of IgG subclasses are shown in Fig. 1.
Gender and Age Distribution
Table 1 shows female-to-male ratio of 3:1. All patients with IgG1, IgG1 plus IgG4, and IgG3 plus IgG4 deficiency were female (21/21). No significant difference in age distribution was observed among various IgG subclass deficiencies (Table 1).
Clinical Presenting Manifestations
Most common clinical presentation was recurrent upper respiratory infections (pharyngitis, otitis media) in 28 patients, chronic sinusitis in 27 patients, and 10 patients with recurrent pneumonia. Other clinical presentations included bronchitis, bronchiectasis, recurrent urinary tract infections, chronic fatigue, undifferentiated mixed connective tissue disease, and meningitis (Table 1). Two patients with IgG3 subclass deficiency who presented with bronchitis, and sputum cultures for bacteria and fungus were found to be positive for Hemophilus influenzae and Aspergillus fumigatus. None of these patients had pneumonia or asthma.
Several other associated diseases were noted in this population. Allergic asthma or/and allergic rhinitis were the second commonest manifestations. Other associated autoimmune diseases included pernicious anemia, Hashimoto’s thyroiditis, Addison’s disease, anti-phospholipid syndrome, systemic lupus erythematosus, discoid lupus, Graves disease, rheumatoid arthritis, undifferentiated mixed connective tissue disease, autoimmune thrombocytopenia, and celiac disease. Distribution of allergic and autoimmune diseases was observed among all subclass deficiencies without any subclass predominance.
Lymphocyte Phenotype
Data of lymphocyte subset in IgG subclass deficiency are shown in Fig. 2a–e. In general, the proportions and absolute numbers of CD3+ T, CD4+ T, CD8+, CD19+ B, and CD3−CD16+CD56+ NK lymphocyte subsets were comparable to ranges for healthy controls among various IgG subclass deficiencies. However, four patients were found to have low percentages and absolute numbers of CD19+ B cells; one in each deficiency of IgG3, IgG1plus IgG3, IgG1 plus IgG4, and IgG2 plus IgG3. Other isolated decreases were observed in the proportions and numbers of CD8+ T cells and CD3+ T cells in two patients with IgG3 deficiency, and one patient with IgG4 subclass deficiency had low total lymphocytes counts and absolute numbers of all subsets of lymphocytes.
Total IgG Levels in IgG Subclass Deficiency and Relationship with Each Subclass
Figure 3 shows that serum levels of total IgG among various IgG subclass deficiencies were similar. No significant correlation was observed between total IgG levels and various IgG subclasses (data not shown).
Response to Pneumococcal Polysaccharide Vaccination
Specific antibody responses were measured at the time of diagnosis prior to institution of immunoglobulin therapy. Impaired response was defined by either lack of protective titers (less than 1.3 μg/dl) and/or less than twofold increase over pre-vaccination titers. The responses to pneumococcal polysaccharide were assessed against individual 23 serotypes. Forty-three of seventy-two (59.7%) patients had impaired anti-pneumococcal polysaccharide antibody response. Impaired specific antibody responses were observed across all IgG subclass deficiencies, however, impaired response were more common in selective isolated IgG2, and IgG2 plus IgG3 subclass deficiency. Distribution was as follows: IgG1 deficiency—8/15 (53.3%), IgG2 deficiency—8/11 (72.7%), IgG3 deficiency—9/16 (56.2%; four patient declined vaccination), IgG4 deficiency—2/6 (33.3%), IgG1 plus IgG3 deficiency—6/10 (60%), IgG1 plus IgG4 deficiency—1/2 (50%), IgG2 plus IgG3 deficiency—4/5 (80%), IgG2 plus IgG4 deficiency—3/5 (60%), and IgG3 plus IgG4 deficiency—2/2 (data were not available on two subjects). Impaired responses were not associated with any specific or group of serotypes in any of IgG subclasses.
Complement Components
Complement data, including C3, C4, and CH50, were available for 20 patients and were within normal limits.
Antigen and Mitogen Proliferation
Data on proliferative response to recall antigen and mitogen were available for 20 patients. Two patients were found to have significantly low antigen and mitogen proliferation values; these patients had IgG1 plus IgG3 deficiency as well as IgG3 plus IgG4 deficiency. Four other patients were found to have decreased antigen-induced proliferation (one each with IgG1, IgG2, IgG1 plus IgG3, and IgG2 plus IgG4 deficiency) but normal mitogen response.
Response to Immunoglobulin Therapy
Forty-two symptomatic patients were treated with Ig replacement therapy. Thirty-three received IVIG, seven received weekly conventional subcutaneous immunoglobulin (SCIG), and two received enzyme-facilitated SCIG. The mean dose was 436 mg/kg/4 weeks for IVIG, 510 mg/kg/4 weeks divided into weekly dose for conventional SCIG, and 450 mg/kg/4 weeks for HyQvia. Patients who had normal response to pneumococcal vaccine could not get authorization for immunoglobulin administration from their health insurance carriers, and, therefore, were not treated with immunoglobulin. Two patients decline treatment. The majority of these patients responded to immunoglobulin treatment with decreased frequency of upper respiratory tract infections, chronic sinusitis, bronchitis, and urinary tract infections, and only occasional use of antibiotics. The number of infections prior to immunoglobulin therapy requiring prolonged use of oral antibiotics ranged from 4 to 8 times per year. These were reduced to none to one episode of infection annually requiring oral antibiotics with the exception of a patient with bronchiectasis who received IVIG at 800 mg/dl but lost to follow-up after 4 months. During those 4 months, he had two episodes of infections requiring antibiotics. None of the patients who had history of pneumonia or meningitis had any further episodes of pneumonia or meningitis on immunoglobulin therapy.
Discussion
In this study, we report comprehensive clinical and immunological findings in a large cohort of adult patients with IgG subclass deficiency, and response to Ig replacement therapy. IgG subclass deficiencies appear to be of clinical significance in patients who present with recurrent respiratory tract infections, and chronic sinusitis, and are benefited with immunoglobulin replacement therapy. In the present study, the frequency of isolated IgG subclass deficiency is IgG3 > IgG2 > IgG1 > IgG4. In the combined IgG subclass deficiency, the frequency is IgG1 plus IgG3 > IgG2 plus IgG3, > IgG2 plus IgG4, and > IgG1 plus IgG4. Patients with IgG subclass deficiency also have increased prevalence of allergic and autoimmune manifestations.
Since IgG1 subclass contributes to 65–70% of total IgG, it is believed that selective IgG1 deficiency with normal IgG is rare. However, in the present study, it is the second most common subclass deficiency. Majority of patients with isolated IgG1 subclass deficiency presented with upper and lower respiratory tract infections, which is in agreement with reports by Barton et al. (2016a) and Lacombe et al. (1997).
Anti-pneumococcal polysaccharide antibodies are mostly demonstrated in IgG2 subclass (Musher et al. 1990). However, Mikolajczyk et al. (2004) reported that, on a per mg of IgG subclass basis, IgG1 in seven different commercial preparations of immunoglobulin G for intravenous administration contained approximately similar amounts of anti-pneumococcal antibodies as in IgG2. Furthermore, Roberton et al. (1989) reported an increased in anti-pneumococcal-specific IgG1 and IgG3 following immunization with vaccine in patients with IgA deficiency. In our group of isolated IgG1 subclass deficiency, 53% had impaired anti-pneumococcal polysaccharide antibody response. Barton et al. (2016a) and Van Kessel et al. (1999) each reported impaired pneumococcal antibody responses in 39% of patients with selective IgG1 subclass deficiency. These observations of impaired anti-pneumococcal antibody response in isolated IgG1 subclass deficiency support that IgG1 subclass also contains significant titers of anti-pneumococcal antibodies.
IgG2 subclass deficiency is more common in children than in adults (Javier et al. 2000; Jefferis and Kumararatne 1990; Umetsu et al. 1985). In our patients group isolated and combined (with IgG3 or IgG4) IgG2 subclass deficiency was observed. Combined deficiency of IgG2 with IgG3 (Kitaura et al. 2017) or IgG4 (Oxelius 1984) has been reported. These associations of IgG2 with IgG3 and IgG4 are not surprising, since during class switch recombination, IgM switches to IgG3, and then to IgG1 and IgG2 (Kitaura et al. 2017). Furthermore, switching from IgG2 subclass produces IgG4. IgG2 is considered predominantly comprised of anti-polysaccharide antibodies, and therefore, patients with IgG2 subclass deficiency display impaired anti-polysaccharide antibody responses and are at increased risk for infections with Streptococcus pneumoniae, Hemophilus influenzae type B, and Neisseria meningitis (Bass et al. 1983; Escobar-Pérez et al. 2000; Shackelford et al. 1986; Siber et al. 1980). Impaired anti-pneumococcal antibody response was most commonly observed in IgG2 subclass deficiency. IgG2 subclass deficiency is associated with a number of autoimmune diseases (Eriksson et al. 1994; Garg et al. 2012; Jiménez et al. 1989). We also observed autoimmune diseases in our group of patients with IgG2 subclass deficiency.
IgG3 represents less than 10% of total IgG. IgG3 has higher molecular weight, and shortest half-life (7–9 days) than other subclasses, and is susceptible to proteolytic degradation. Next-generation-based antibody repertoire analysis revealed that IgG3 genes are least somatic hypermutated among all four subclasses of IgG (Kitaura et al. 2017). Our study shows that isolated selective IgG3 and combined IgG3 subclass deficiency are most common IgG subclass deficiency.
Clinically, patients with IgG3 subclass deficiency commonly present with upper and lower respiratory tract infections, recurrent pneumonia, chronic sinusitis, mastoiditis, meningitis, and asthma (Abrahamian et al. 2010; Armenaka et al. 1994; Barton et al. 2016b; Meyts et al. 2006; Popa et al. 1993). In our group of patients with IgG3 subclass deficiency, a majority of patients presented with respiratory tract infections and sinusitis. Increased prevalence of allergic disorder are observed in IgG3 subclass deficiency (Abrahamian et al. 2010, Armenaka et al. 1994; Popa et al. 1993). In the present study, 20% patients had autoimmune diseases, which is in agreement with the published reports (Abrahamian et al. 2010; Barton et al. 2016b). Our observation of impaired anti-pneumococcal antibody response in selective IgG3 subclass deficiency is similar to those reported by others (Abdou et al. 2009; Abrahamian et al. 2010; Barton et al. 2016b; Meyts et al. 2006).
IgG4 is different from other IgG subclasses as it lacks ability to fix complement and binding effectively to Fcγ receptors IgG4. Next gene sequencing-based antibody repertoire analysis has demonstrated that IgG4-specific sequences have higher somatic hypermutation than other IgG subclasses (Kitaura et al. 2017). IgG4 contributes to less than 10% to total IgG. In our present group of patients, 16.6% have isolated or combined IgG4 subclass deficiency. Forty percent of patients with IgG4 subclass deficiency have impaired anti-pneumococcal antibody responses. During class switch recombination, IgG4 is primarily produced by switching from IgG2 (Kitaura et al. 2017), which may explain combined IgG4 plus IgG2 deficiency. An association of IgG2 with IgG4 has been previously reported (Bragger et al. 1989; Moss et al. 1992; Latiff and Kerr (2007). Wilson et al. (1990) described a patient of IgG4 plus IgG2 subclass deficiency associated with autoimmune diseases and impaired response to polysaccharide antigens.
Studies of lymphocyte subsets (CD3+, CD4+, CD8+, CD19/CD20+, CD3−CD16+CD56+) and T-cell functions in IgG1, IgG2, and IgG3 subclass deficiency are limited; no report for IgG4 subclass deficiency. In general, the majority of patients with IgG subclass deficiency have normal distribution of T cells, T-cell subsets, B cells, and NK cells (Abrahamian et al. 2010; Barton et al. 2016b; Lacombe et al. 1997). In our study, only isolated cases of both T-cell (CD4+, CD8+) and B-cell abnormalities were observed. There are only few reports for lymphocyte proliferative response to mitogens and antigens in selective IgG subclass deficiency; mostly in IgG3 subclass deficiency. Abrahamian et al. (2010) reported impaired mitogen and antigen responses in 30–40% of patients with selective IgG3 subclass deficiency. In the present study, we also observed impaired response to mitogen and/or recall antigens in 30% of patients. Since the number of subjects in these studies is small, larger number of patients needs to be evaluate before a definitive statement can be made regarding T-cell functions.
CH50, C3, and C4 were studied in a small number of patients and were found to be normal. Abrahamian et al. (2010) also reported normal CH50, C3, and C4 levels in patients with IgG3 subclass deficiency.
Few studies have examined the beneficial effects of immunoglobulin replacement therapy in treating IgG subclass deficiency. Ig prophylaxis in selective IgG2 subclass deficiency is generally accepted. Olinder-Nielsen et al. (2007) in a retrospective study reported response of weekly SCIG therapy (mean duration of 5.5 years) in 132 patients with IgG1-3 subclass deficiency and respiratory tract infections that received ≥ 4 antibiotics per year. In 92 of 132 patients, a ≥ 50% reduction in the rate of respiratory tract infections requiring antibiotics was observed. Even though numbers of respiratory tract infections were higher in IgG2 and IgG3 subclass deficiency as compared to IgG1 subclass deficiency, response to Immunoglobulin treatment was similar in isolated IgG1, IgG2, and IgG3 subclass deficiencies or in combined IgG subclass deficiencies (IgG4 subclass deficiency was not studied). No difference was observed in effectiveness of treatment whether patients had lung involvement or not. In the study by Abrahamian et al. (2010), 13 of 17 patients with IgG3 deficiency who presented with recurrent infections were treated with IVIG; of those, 11 patients were reported to have an improvement in rates of infections and requirement for antibiotic. Meyts et al. (2006)also observed significant clinical improvement in the frequency of infections and use of antibiotics in children with IgG3 deficiency children treated with IVIG. Barlan et al. (1993) also reported significant improvement in the incidence of sinusitis and otitis in patients with selective IgG3 subclass deficiency which were treated with IVIG following failed a year of prophylactic antibiotic treatment. Armenaka et al. (1994) reported clinical improvement in sinusitis in a subset of patients with IgG3 subclass deficiency. Popa et al. (2002) reported improvement in symptoms, spirometry, and radiological findings in patients who had recurrent upper respiratory tract infections, interstitial lung disease, and isolated or combined IgG1, IgG2, IgG3, or IgG4 deficiencies. Abdou et al. (2009) in an open label 15 month study of ten patients with IgG subclass deficiencies treated with IVIG observed a significant improvement in quality of life scores, number of infections, antibiotic usage, and hospitalizations. In our present study, majority of patient responded to all modes of immunoglobulin therapy (IVIG, SCIG, and enzyme-facilitated subcutaneous immunoglobulin) with regard to frequency of infection, and requirement for antibiotics.
In summary, selective IgG subclass deficiency often presents with increased susceptibility to upper and lower respiratory tract infection and chronic sinusitis. Clinically symptomatic patients with IgG subclass deficiency and specific antibody deficiency respond to the treatment with immunoglobulin, regardless of mode of administration, and should be treated. The measurements of IgG subclass and specific antibody response to vaccination should be a part of work-up for humoral immunity in patients with recurrent upper and lower respiratory tract infection, chronic sinusitis, and recurrent otitis. Larger prospective studies for other subsets of T cells (e.g., follicular helper cells) and B cells (naïve, memory, transition, IgM memory, switch memory, marginal zone, germinal center, and plasmablasts), and specific antibody responses within each IgG subclass are needed.
References
Abdou NI, Greenwell CA, Mehta R et al (2009) Efficacy of intravenous gammaglobulin for immunoglobulin G subclass and/or antibody deficiency in adults. Int Arch Allergy Immunol 149:267–274
Abrahamian F, Agrawal S, Gupta S (2010) Immunological and clinical profile of adult patients with selective immunoglobulin subclass deficiency: response to intravenous immunoglobulin therapy. Clin Exp Immunol 159:344–350
Annerén G, Magnusson CG, Lilja G et al (1992) Abnormal serum IgG subclass pattern in children with Down’s syndrome. Arch Dis Child 67:628–631
Armenaka M, Grizzanti J, Rosensterich DL (1994) Serum immunoglobulins and IgG subclass levels in adults with chronic sinusitis: evidence for decreased IgG3 levels. Ann Allergy 72:507–514
Barlan IB, Geha RS, Schneider LC (1993) Therapy for patients with recurrent infections and low serum IgG3 levels. J Allergy Clin Immunol 92:353–355
Barton JC, Bertoli LF, Barton JC et al (2016a) Selective subnormal IgG1 in 54 adult index patients with frequent or severe respiratory tract infections. J Immunol Res 2016:1405950
Barton JC, Bertoli LF, Barton JC et al (2016b) Selective subnormal IgG3 in 121 adult index patients with frequent or severe bacterial respiratory tract infections. Cell Immunol 299:50–57
Bass JL, Nuss R, Mehta KA et al (1983) Recurrent meningococcemia associated with IgG2-subclass deficiency. N Engl J Med 309:430
Bragger C, Seger RA, Aeppli R et al (1989) IgG2/IgG4 subclass deficiency in a patient with chronic mucocutaneous candidiasis and bronchiectasis. Eur J Pediatr 149:168–169
Eriksson P, Almroth G, Denneberg T et al (1994) IgG2 deficiency in primary Sjögren’s syndrome and hypergammaglobulinemic purpura. Clin Immunol Immunopathol 70:60–65
Escobar-Pérez X, Dorta-Contreras AJ, Interián-Morales MT et al (2000) IgG2 immunodeficiency: association to pediatric patients with bacterial meningoencephalitis. Arq Neuropsiquiatr 58:141–145
Garg V, Lipka S, Rizvon K et al (2012) Diffused nodular lymphoid hyperplasia of intestine in selective IgG2 subclass deficiency, autoimmune thyroiditis, and autoimmune hemolytic anemia: case report and literature review. J Gastrointestin Liver Dis 21:431–433
Garside JP, Kerrin DP, Brownlee KG et al (2005) Immunoglobulin and IgG subclass levels in a regional pediatric cystic fibrosis clinic. Pediatr Pulmonol 39:135–140
Grey HM, Kunkel HG (1964) H chain subgroups of myeloma proteins and normal 7S γ-globulin. J Exp Med 120:253–266
Ishizaka A, Nakanishi M, Kasahara E et al (1992) Phenytoin-induced IgG2 and IgG4 deficiencies in a patient with epilepsy. Acta Paediatr 81:646–648
Javier FC 3rd, Moore CM, Sorensen RU (2000) Distribution of primary immunodeficiency diseases diagnosed in a pediatric tertiary hospital. Ann Allergy Asthma Immunol 84:25–30
Jefferis R, Kumararatne DS (1990) Selective IgG subclass deficiency: quantification and clinical relevance. Clin Exp Immunol 81:357–367
Jiménez A, López-Trascasa M, Fontán G (1989) Incidence of selective IgG2 deficiency in patients with vasculitis. Clin Exp Immunol 78:149–152
Kalfa VC, Roberts RL, Stiehm ER (2003) The syndrome of chronic mucocutaneous candidiasis with selective antibody deficiency. Ann Allergy Asthma Immunol 90:259–264
Kato Z, Watanabe M, Kondo N (2003) IgG2, IgG4 and IgA deficiency possibly associated with carbamazepine treatment. Eur J Pediatr 162:209–211
Kitaura K, Yamashita H, Shini T et al (2017) Different somatic hypermutation levels among antibody subclasses disclosed by a new next-generation sequencing-based antibody repertoire. Front Immunol 8:389
Klaustermeyer WB, Gianos ME, Kurohara ML et al (1992) IgG subclass deficiency associated with corticosteroids in obstructive lung disease. Chest 102:1137–1142
Kronvall G, Williams RC Jr (1969) Differences in anti-protein A activity among IgG subgroups. J Immunol 103:828–833
Lacombe C, Aucouturier P, Preud’homme JL (1997) Selective IgG1 deficiency. Clin Immunol Immunopathol 84:194–201
Latiff AH, Kerr MA (2007) The clinical significance of immunoglobulin A deficiency. Ann Clin Biochem 44(Pt 2):131–139
Leickly FE, Buckley RH (1986) Development of IgA and IgG2 subclass deficiency after sulfasalazine therapy. J Pediatr 108:481–482
Maeoka Y, Hara T, Dejima S et al (1997) IgA and IgG2 deficiency associated with zonisamide therapy: a case report. Epilepsia 38:611–613
Meyts I, Bossuyt X, Proesmans M et al (2006) Isolated IgG3 deficiency in children: to treat or not to treat? case presentation and review of literature. Pediatr Allergy Immunol 17:544–550
Mikolajczyk MG, Concepcion NF, Wang T et al (2004) Characterization of antibodies to capsular polysaccharide antigens of Haemophilus influenzae Type b and Streptococcus pneumonie. Cln Diagn Lab Immunol 11:1158–1164
Moss RB, Carkack MA, Esrig S (1992) Deficiency of IgG4 in children: association of isolated IgG4 deficiency with recurrent respiratory tract infections. J Pediatr 120:16–21
Musher DM, Luchi MJ, Watson DA et al (1990) Pneumococcal polysaccharide vaccine in young adults and older bronchitis: determination of IgG responses by ELISA and the effect of adsorption of serum with non-type-specific cell wall polysaccharide. J Infect Dis 161:728–735
Natvig JB, Kunkel HG, Litwin SD (1967) Genetic markers of the heavy chain subgroups of human γG globulin. Sympos Quarter Biol 32:173–180
Olinder-Nielsen AM, Granert C, Forsberg P et al (2007) Immunoglobulin prophylaxis in 350 adults with IgG subclass deficiency and recurrent respiratory tract infections: a long-term follow-up. Scand J Infect Dis 39:44–50
Oxelius VA (1984) Immunoglobulin G (IgG) subclasses and human disease. Am J Med 76:7–18
Oxelius VA, Laurell AB, Lindquist B et al (1981) IgG subclasses in selective IgA deficiency: importance of IgG2 IgA deficiency. N Engl J Med 304:1476–1477
Oxelius VA, Berkel AI, Hanson LA (1982) IgG2 deficiency in ataxia-telangiectasia. N Engl J Med 306:515–517
Plebani A, Monafo V, Avanzini MA et al (1986) Relationship between IgA and IgG subclass deficiencies: a reappraisal. Monogr Allergy 20:171–178
Popa V, Kim K, Heiner DC (1993) IgG deficiency in adults with recurrent upper respiratory tract infections. Ann Allergy 70:418–424
Popa V, Colby TV, Reich SB (2002) Pulmonary interstitial disease in Ig deficiency. Chet 122:1594–1603
Roberton DM, Björkander J, Henrichsen J et al (1989) Enhanced IgG1 and IgG3 responses to pneumococcal polysaccharides in isolated IgA deficiency. Clin Exp Immunol 75:201–205
Shackelford PG, Polmar SH, Mayus JL et al (1986) Sepctrum of IgG2 subclass deficiency in children with recurrent infections. Prospective study. J Pediatr 108(5 Pt 1):647–653
Siber GR, Schur PH, Aisenberg AC et al (1980) Correlation between serum IgG-2 concentrations and the antibody response to bacterial polysaccharide antigens. N Engl J Med 303:178–182
Terry WD (1968) Variations in the subclasses of IgG. Immunologic deficiency diseases in man. In: Bergsma D (ed) Birth Defects Original Article Series, vol 4. The National Foundation, New York, pp 357–363
Umetsu DT, Ambrosino DM, Quinti I et al (1985) Recurrent sinopulmonary infection and impaired antibody response to bacterial capsular polysaccharide antigen in children with selective IgG-subclass deficiency. N Engl J Med 313:1247–1251
Van Kessel DA, Horikx PE, Van Houte AJ et al (1999) Clinical and immunological evaluation of patients with mild IgG1 deficiency. Clin Exp Immunol 118:102–107
Wilson NW, Daaboul J, Bastian JF (1990) Association of autoimmunity with IgG2 and IgG4 subclass deficiency in a growth hormone-deficient child. J Clin Immunol 10:330–334
Yel L, Ramanuja S, Gupta S (2009) Clinical and immunological features in IgM deficiency. Int Arch Allergy Immunol 150:291–298
Funding
This work was in part supported by Investigator-initiated Publication and Research Grant (PRG) from CSL Behring, King of Prussia, PA, and unrestricted funds from the Division of Basic and Clinical Immunology.
Author information
Authors and Affiliations
Contributions
Amrita Khokar retrieved and tabulated data from patient’s chart and electronic medical records. She wrote an initial draft of a small segment of text. Sudhir Gupta planned the study, supervised the collection of data, helped in the interpretation, and wrote majority of the manuscript.
Corresponding author
Ethics declarations
No outside funding was obtained and is a retrospective study, and therefore, no consent from patients was required. Institutional Review Board (Human) approved this study.
Conflict of Interest
Both authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Khokar, A., Gupta, S. Clinical and Immunological Features of 78 Adult Patients with Primary Selective IgG Subclass Deficiencies. Arch. Immunol. Ther. Exp. 67, 325–334 (2019). https://doi.org/10.1007/s00005-019-00556-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00005-019-00556-3