Abstract
Vitamins are organic compounds; they help in the regulation of many bodily functions like cell proliferation and differentiation, immunological response, and metabolism. A deficiency of these molecules can cause severe medical conditions, i.e., beriberi, xerophthalmia, scurvy, Crohn’s disease, and others. Furthermore, studies have shown that vitamin deficiency might lead to many neuronal dysfunctions, even hampering the growth of neurons. This chapter explores the role of vitamins and their derivatives in the pathology of Alzheimer’s disease. Alzheimer’s disease is a multifactorial neurodegenerative disease, and the cause of this disease is still unknown. However, several hypotheses try to explain the aetiology of the disease, such as Aβ hypothesis, metal ion hypothesis, calcium homeostasis, cholinergic hypothesis, tau propagation, etc. Scientific literature reports several derivatives that show potential to treat Alzheimer’s disease. Primarily these compounds act on nuclear receptors to activate ADAM10, inhibiting AChE or BuChE, neutralisation of ROS, inhibition of GSK-3, and amyloid-beta aggregation. Moreover, some can easily pass the BBB, which is crucial in targeting neurological disease. Vitamins and their derivatives show promising results in managing Alzheimer’s disease, even several are in clinical trials.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
In 1912, Casimir Funk coined the term vitamine, which is originated from the Latin word “vita” meaning “life” since these molecules are important part of normal functioning body, and “amine” since vitamins were assumed to include amino acids. Later, scientists uncovered the true nature of the substance, and vitamine was modified to vitamin (Semba 2012). Vitamins are organic compounds required for the body’s development and normal functioning. They regulate various biological processes, including cell and tissue growth, differentiation, and mineral metabolism, and commonly act as antioxidants and enzymatic cofactors or precursors. Not all vitamins can be synthesised by the body. As a result, they must be obtained through dietary means. Vitamins can be classified into two main categories: (1) fat-soluble vitamins which includes vitamin A, D, E, K and (2) water-soluble vitamins which includes vitamin B complex and vitamin C. Generally, fat-soluble vitamins are stored in the body whereas water-soluble vitamins require a continual exogenous daily supply. Vitamin balance is necessary for biological processes and human body development.
Vitamin deficiency develops several disorders, such as night blindness, beriberi, pellagra, scurvy, megaloblastic anaemia, haemolytic anaemia, and osteomalacia. In recent years, vitamins are found to have advantageous effects in the management of numerous diseases such as peripheral vascular diseases (Collins et al. 2003), cardiovascular diseases (Czernichow and Hercberg 2001), coronavirus disease 2019 (COVID-19) (Abobaker et al. 2020), neurodegenerative diseases (Rai et al. 2021), and others. Among all neurodegenerative disorders, Alzheimer’s disease (AD) is the most prevalent worldwide and has no cure (Dong et al. 2019).
Alzheimer’s disease (AD) is named after the psychiatrist Alois Alzheimer who reported the first case of Alzheimer’s disease. Major symptoms of AD are a decline in cognitive ability and progressive memory loss. Although the nature of this disorder’s onset, progression, and severity is quite diverse, the types of symptoms, such as behavioural changes and the inability to perform everyday living tasks, are common. It is believed that the oxidative stress is a crucial factor that influences the initiation and progression of AD. Research shows that the antioxidative characteristics of vitamins are advantageous and can be utilised in the treatment and management of Alzheimer’s disease (Singh et al. 2021). As a result, vitamins have been used as adjuvants in AD therapy (Kurutas 2016).
It is widely known that amyloid-beta (Aβ) induced oxidative stress, which aids in the formation of reactive oxygen species (ROS) that results into lipid peroxidation, tau hyperphosphorylation, protein oxidation and has deleterious effects on synapses and neurons. For these reasons, antioxidant therapy might be beneficial in AD patients. Vitamins A, C, and E have antioxidant activity; these vitamins and their derivatives enhance cognition and prevent dementia. Many studies have investigated the role of vitamins in the treatment of AD and other types of dementia. Such studies suggest that vitamin A can reduce the production of Aβ plaques, whereas vitamins like B, C, D, and E can intervene the progression of neurocognitive decline. Furthermore, vitamin D deficiency is associated with an increased risk of dementia and AD (Bhatti et al. 2016). Vitamin B supplements, such as pyridoxine (B6), folate (B9), and cyanocobalamin (B12), reduce the risk of dementia since they are involved in homocysteine metabolism (Bhatti et al. 2016; Littlejohns et al. 2014; Ford et al. 2010). Dietary vitamin A deficiency disrupts the retinoid signalling pathway, resulting in amyloid-beta (Aβ) deposition in the cerebral blood vessels through down-regulation of retinoic acid receptor alpha (RAR-α) in the forebrain neurons and loss of choline acetyltransferase (ChAT) expression. Administration of retinoic acid which is a vitamin A derivative can reverse these changes. Amyloid-β (Aβ) deposition and a similar RAR-α impairment were seen in the pathological samples from AD patients. The same has been reported for thiamine (vitamin B1) insufficiency and vitamin E (La Fata et al. 2014), which is linked to significant cognitive impairment and advancing dementia. Thiamine supplementation in those who were impacted helped with these symptoms (Lu’o’ng and Nguyen 2011). Cobalamin (vitamin B12) deficiency has also been linked to reversible dementia in older persons (Osimani et al. 2005).
A significant deal of interest in vitamins has been sparked by the development of the free radical theory, which explains the pathophysiology of brain ageing and neurodegenerative disorders like AD. The theory claims that oxidative and nitrosative modifications of several biological molecules are caused by reactive oxygen species (ROS) and reactive nitrogen species (RNS). Accumulation of free radical-mediated damage to neuronal components, combined with other age-related changes, is one of the leading causes of neurodegeneration. Therefore, preventing or reducing oxidative and nitrosative stress may counteract the molecular cause of pathological brain ageing and the subsequent neurodegeneration that results in brain damage, indicating that antioxidants vitamins may be an effective preventive and therapeutic approach (Bhatti et al. 2016; Singh et al. 2022).
The first acetylcholinesterase inhibitor approved for the symptomatic treatment of AD was tacrine although it is no longer used because of its hepatotoxicity (Joe and Ringman 2019); Currently AD is managed by acetylcholinesterase inhibitors, i.e., galantamine, rivastigmine, and donepezil (Kumar et al. 2022) and antagonist of N-Methyl-d-aspartate (NMDA) receptor, i.e., memantine. Moreover, current pharmacological treatments for AD are expensive, sometimes accompanied by various side effects, and alleviate symptoms rather than halt the eventual decline in cognitive and behavioural function. Additionally, medication must be administered after a significant amount of cognitive impairment, which may be accompanied by irreversible functional deterioration. Antioxidant use might be an effective strategy that can assist in treating this illness. Apart from the excellent antioxidant properties of vitamins or their derivatives shown to have the inhibitory activities on AChE, BuChE, and GSK-3β. Several vitamin B derivatives can act as metal chelators and help to maintain the bio-metal homeostasis in the brain. Additionally, vitamins like ascorbic acid have special transporters which ensures the passage through BBB. Combining all these properties, vitamins and their derivatives can be explored to find new therapy for Alzheimer’s disease. The current chapter explores the various vitamin-based derivatives and their ability to halt AD progression.
2 Vitamins and Their Derivatives
2.1 Vitamin A
Vitamin A is one of the fat-soluble and essential vitamins which is commonly known as retinol. The body cannot synthesise Vitamin A, so it must be taken in the diet. Retinol is metabolised in our body and converted to retinoic acid (RA), specifically all-trans RA (ATRA). Retinoic acid has several stereoisomers like all-trans RA, 13-cis RA, and 9-cis RA. Vitamin A is a vital nutrient for normal vision, growth, cell division, reproduction, and immunity. Vitamin A shows strong antioxidant properties and hence protects cells against ROS. Studies have shown that free radicals can cause heart diseases, cancer, and other diseases, including neurodegenerative diseases (like AD). Studies have shown that Alzheimer’s disease (AD) patients have lower levels of Vitamin A, β-carotene, and Provitamin A in their plasma or cerebral fluid. Clinical studies have suggested that these vitamins may be effective in slowing the onset of dementia. In laboratory studies, Vitamin A (retinol, retinal, and retinoic acid) and β-carotene have been found to prevent the production, elongation, and are helpful in destabilisation of β-amyloid fibrils. Further, when transgenic animal models of AD were given, intraperitoneal infusions of Vitamin A, there was a reduction in Aβ deposition and tau phosphorylation, a slowdown in neuronal degeneration, and an enhancement of spatial learning and memory (Ding et al. 2008). Depriving mice of retinoic acid severely impairs their spatial learning and memory, demonstrating the importance of vitamin A in maintaining memory function. Retinoids have been found to suppress the expression of pro-inflammatory cytokines and chemokines in activated microglia and astrocytes in AD. Retinoid signalling has been linked to a variety of biological activities in the healthy brain, including cell proliferation, neurogenesis, dendritic spine development, and immune system modulation (Hou et al. 2015). These findings suggest that vitamin A and β-carotene or their derivatives could be a promising treatment option for managing AD. Several derivatives of vitamin A were obtained either from natural sources or via synthesis and tested for its activity in AD. Compounds like ATRA, tamibarotene, bexarotene, isotretinoin, and acitretin showed beneficial effects (Fig. 12.1).
All-trans-retinoic acid (ATRA) is a bioactive derivative of vitamin A with established clinical indications. It is approved by the United States Food and Drug Administration (FDA) for treating acute promyelocytic leukaemia (APL) and has also been used to treat acne vulgaris. Being a RA isoform, ATRA interacts with retinoic acid receptors (RARs) and retinoid X receptors (RXRs). RARs and RXRs are nuclear receptors that each have three different subtypes (α, β, and γ); each subtypes have various isoforms. These isoforms have varying affinities towards the RA stereoisomers. These nuclear receptors can affect many cellular processes, including cellular differentiation, proliferation, and apoptosis. ATRA activates the manganese superoxide dismutase (MnSOD2) gene, which translates to the antioxidant enzyme in mitochondria (Kapoor et al. 2013).
ATRA is also involved in the regulation of arachidonic acid metabolites. Excessive generation of these metabolites can cause inflammation, oxidative stress, and neurodegeneration. ATRA might be passively involved in the regulation of the amyloid precursor protein (APP) processing. RAR-α and RAR-β can activate the disintegrin metalloproteinase 10 (ADAM10). Activation of ADAM10 promotes the production of a soluble form of Amyloid-β (APP-α) (Fahrenholz et al. 2010). It is also affected by other derivatives of vitamin A, like acitretin (Tippmann et al. 2009) and Am80.
Acitretin is an orally active drug and is currently used for the treatment of psoriasis. By activating the α-secretase ADAM10, the aromatic retinoid acitretin was discovered to have an anti-amyloidogenic impact in mice models and human patients. After being administered intravenously, it has previously been shown to traverse the blood–brain barrier and boost nest-building ability in the 5xFAD mouse model. It also shows immune-modulatory potential in the 5xFAD mice model. Administration of acitretin results in significant rise of interleukin-6 (IL-6) in both mice and humans, despite the fact that some serum analytes did not alter. This shows that, in addition to inducing α-secretase, acitretin also has an immune stimulatory effect that may help to improve the learning and memory in the mouse model (Endres et al. 2014). Acitretin improves non-amyloidogenic APP processing in a human and has a protective effect against neurodegeneration.
Am80 or Tamibarotene, a selective agonist for the retinoic acid receptor alpha/beta currently being used to treat leukaemia. Due to its transcriptional regulation of numerous genes implicated in the aetiology and pathogenesis of AD, tamibarotene is regarded as a potential candidate for the treatment of AD. Administration of Am80 to APP23 AD model mice showed reduced accumulation of insoluble amyloid-β. The retinoid-induced potentiation of either phagocytosis or α-secretase transcription by alternatively activated microglia may be the cause of this decrease in insoluble amyloid-β. Tamibarotene significantly reduced the inflammation of central nervous system cells caused by LPS-interferon (IFN). Micromolar doses of Am80 restored neuronal viability in organotypic midbrain slice cultures. An LPS-induced inflammatory model also revealed tamibarotene’s neuroprotective effects on midbrain neurons. In cultured SH-SY5Y neuroblastoma cells, both RA and tamibarotene enhanced substantial neurite outgrowth and elevated expression of neurotrophic tyrosine kinase receptor B (TrkB), which encodes the cognate receptor for brain-derived neurotrophic factor (BDNF). Vitamin A derivatives, including tamibarotene, boost the gene transcription of ADAM10 (a member of the disintegrin and metalloprotease), as well as the activity of α-secretase, which cleaves the APP protein at a different site and releases the soluble neuroprotective protein sAPP (Fukasawa et al. 2012).
Bexarotene (BEXA), a retinoid X receptor agonist, is currently being used in the treatment of cutaneous T-cell lymphoma. The liver X receptor and retinoid X receptor (RXR) transcriptionally regulate the expression of apolipoprotein E (ApoE), which is essential for Aβ clearance. A possible treatment for AD that addresses amyloid pathology and memory loss might be bexarotene, which boosts ApoE expression and microglia phagocytosis (Tousi 2015). However, some investigations do not favour bexarotene as the new drug for AD due to several failures. A study has examined bexarotene’s impact in vivo at various levels in TASTPM transgenic mice. These mice did not exhibit any discernible memory enhancement, plaque reduction, or increased microglial cell activation after receiving BEXA orally for 7 days. When analysed the microglial phagocytic state, no differences were discovered (Balducci et al. 2015). Because of these irregularities in results, bexarotene remains a topic of research and discussion for its use to treat AD. Isotretinoin is another vitamin A derived drug currently used for the treatment of acne. It acts on the retinoid receptors. Isotretinoin, patented by a pharmaceutical company Hexal AG, is in phase II clinical trials for the treatment of AD.
2.2 Vitamin B
Vitamin B is a set of eight water-soluble, structurally unrelated compounds that functions in highly similar ways inside the cells. These eight compounds include thiamine (B1), riboflavin (B2), niacin (B3), pantothenic acid (B5), pyridoxine (B6), biotin (B7), folic acid (B9), and cobalamin (B12). They participate in a variety of anabolic and catabolic enzymatic processes as co-enzymes and assist in synthesising neurochemicals and signalling molecules, DNA/RNA synthesis and repair, energy generation, and methylation of molecules. Most animals require vitamin B in their diets except vitamin B7, which the body can produce. Each of these vitamins performs a particular function and is essential to cellular processes. All the functions of vitamin B can be classified into two categories; one functions in catabolic metabolism, which are associated with energy generation, and second in anabolic metabolism, which are related to the formation and modification of biomolecules (Kennedy 2016).
Vitamin B is used by brain cells in a variety of enzymatic reactions that result in the production of energy and the creation of neurotransmitters. Lack of these substances may result in the failure of these processes, which can lead to brain dysfunction, such as disruption of glucose metabolism, which might lead to AD. In mammalian brains, the pentose phosphate pathway and the Krebs cycle are the two main mechanisms for glucose metabolism; thiamine is essential for both. Thiamine depletion and the disruption of thiamine-dependent pathways in glucose metabolism have long been recognised to be linked with AD. Thiamine deficiency causes pathophysiological changes that are strikingly similar to those of AD, including tau protein hyperphosphorylation, selective neuron loss, the formation of neurofibrillary tangles, increased secretion of the Aβ protein, and abnormal deposition in the hippocampus and nearby regions. Recent research has demonstrated that thiamine shortage increases the production and deposition of Aβ in the brains of animal models for AD. Unfortunately, due to its limited bioavailability, thiamine has not demonstrated a significant therapeutic effect in clinical studies for AD (Pan et al. 2010; Tapias et al. 2018).
Fursultiamine is a thiamine derivative (Fig. 12.2) containing a disulphide moiety; Yasuyo et al. studied the effect of fursultiamine on AD and concluded that it might have a modest therapeutic effect in patients with AD. Fursultiamine therapy not only showed improvement in emotional and mental symptoms but, in some cases, intellectual abilities were also enhanced. However, they also stated that a favourable effect was only evident in certain patients; people with severe impairment showed no beneficial effect (Mimori et al. 1996). Another study performed on the transgenic mice supports the above observation, although they reported that benfotiamine performs better than fursultiamine (Pan et al. 2010). Benfotiamine is S-acyl thiamine derivative (Fig. 12.2), whereas the majority of other thiamine derivatives, including fursultiamine, are disulphide derivatives. This specific alteration may impart distinctive pharmacological effects of benfotiamine. Benfotiamine (BFT) could reduce the production of amyloid plaques by modifying glycogen synthase kinase 3 (GSK-3) activities, it promotes the phosphorylation of Akt, which is the upstream kinase of GSK-3β (Pan et al. 2010, 2016). BFT therapy has been shown to have significant positive benefits in mice models of Alzheimer’s and other brain diseases; however, to show its pharmacological action, it requires in large dosages (100–200 mg/kg per day). This would be equal to 10 g per day in people if equivalent. Though BFT has no noticeable adverse effects, it appears challenging to give patients significantly larger dosages of the drug. Thus, there is a need to identify precursors that work at lower dosages and have advantageous effects comparable to those of BFT. Recently, it was shown that dibenzoylthiamine (DBT) might fulfil these requirements. In Japan, DBT is legal as a food ingredient and has been known for a very long time. Even though no toxic or tumour-causing side effects have been documented, there is no data about its biological effects. It was more well tolerated than thiamine or BFT in salmon yearlings and increased thiamine retention over time. Moreover it can act as an anti-inflammatory agent, thiamine precursor, and antioxidant at very low concentration compared to BFT. DBT offers therapeutic promise for brain disorders connected to inflammation and oxidative stress (Sambon et al. 2020, 2021).
A thiamine derivative (Fig. 12.2) called Sulbutiamine was made in Japan in the middle of the 1960s as a beriberi therapeutic medication. Since then, other prospective uses have been proposed. Sulbutiamine, for instance, could have antioxidant, nootropic, and anti-fatigue benefits. Two thiamine molecules are fused to form sulbutiamine, after the respective thiazolium rings of each half-molecule are opened and esterification is done by an isobutyryl group to the primary alcohol of each molecule. When compared to thiamine, these changes make this derivative more lipophilic. In particular, sulbutiamine’s thiol content, which can have neuroprotective benefits and can impact antioxidant status. Since it provides a large antioxidant pool made up of (1) sulphur bound in disulphide bridges, (2) thiols bound to proteins, and (3) free thiol primarily in the form of reduced glutathione (GSH), the global thiol concentration is well known to play a significant role in the regulation of cellular redox status. It’s interesting to note that sulbutiamine and other thiol-containing substances have been demonstrated to increase GSH, which may decrease oxidative stress in neurons. Sulbutiamine administration has furthermore shown to be advantageous in AD (Starling-Soares et al. 2020).
Niacin-derived nucleotides such as nicotinamide adenine dinucleotide phosphate (NADP) and nicotinamide adenine dinucleotide (NAD) are essential for a wide range of enzymes and processes that are involved across every aspect of peripheral and nerve cell activity. These include oxidative reactions, DNA metabolism and repair, cellular signalling functions (through intracellular calcium), antioxidant protection, and folate to tetrahydrofolate conversion, in addition to energy generation (Kennedy 2016). Moreover, some vitamin B3 derivatives (Fig. 12.2) exhibit notable cholinesterase inhibitory action. In one study, the activity of the tested vitamin B3 derivatives on both cholinesterases was reversible and depended on the presence of a substituent on the side ring of the compound. The tested analogues were shown to be more selective acetylcholinesterase (AChE) inhibitors. According to this study, nicotinamide analogues 6 and 8 were the most effective AChE inhibitors. Derivative 6 shows selective inhibition of AChE which is 80 times higher than inhibition of BuChE. The nicotinamide derivative 8 was the most effective inhibitor of BuChE, indicating that the binding of both enzymes’ active site is considerably influenced by the presence of an aromatic ring as a substituent. Four of the tested analogues, however, had a cytotoxic impact on both HEK293 and SH-SY5Y cells. Although the IC50 values did not place these molecules in the category of being very cytotoxic (Zandona et al. 2020).
Vitamin B5 (Pantothenic acid) is a water-soluble B complex that serves as a coenzyme A (CoA) synthesis substrate. Vitamin B5 deficiency in the cerebral region of the brain can cause dementia and neurodegeneration in AD, which may be prevented or perhaps reversible in its early stages with oral vitamin B5 doses adequate to normalise brain levels (Xu et al. 2020). Most of the pantothenic acid derivatives can biotransform into the CoA which leads to the numerous biological activity. Because acetyl-CoA is a key molecule in choline acetylation, the effects of pantothenic acid derivatives on CoA metabolism make them a promising tool for manipulating biosynthesis of acetylcholine. These compounds can potentially be employed in the treatment of AD in conjunction with glutamatergic drugs such as memantine (MEM). To modulate the cholinergic system, acetylcholinesterase inhibitors are typically employed in combination therapy; however, many of these medications are toxic and unsafe for daily use. In such cases, pantothenic acid derivatives may be advantageous because of their low cost, availability, and most importantly safety.
Pantothenic acid and its derivatives can potentially increase GSH concentrations in the brain. Tripeptide GSH plays a vital function as an antioxidant and in redox state maintenance in neurons and glial cells in the brain. Because of its interaction with glutamate receptors, GSH can operate as a neuromodulator. Deficits in the production and metabolism of GSH plays a pivotal role in neurodegenerative disorders. These deficiencies may lead to both neural plasticity and neuronal death. It has been suggested that GSH depletion occurs before neurodegeneration. Stepanichev et al. conducted behavioural study to examine the impact of calcium pantothenate (PAC) and panthenol (PL), which are derivatives of pantothenic acid, on the rat subjects, moreover they observed the CoA content and redox state of GSH in a scopolamine-induced amnesia model. They also investigated how these substances interacted with the anti-amnesic drug MEM. In order to regulate CoA metabolism in the brain, PAC and PL were used. Derivatives of pantothenic acid shielded different tissues including nerve tissue against various harmful elements. Most of these detrimental effects are brought on by oxidative stress. Pantothenic acid preincubation was found to dramatically boost the concentration of GSH in the cells. Pantothenic acid, PL, and PAC all have preventative antioxidant actions that are related to how they affect the GSH system (Turnaturi et al. 2016).
Transition metals are dangerous for the ageing brain and many disorders, including Alzheimer’s disease (AD), despite being crucial for neuronal function. Cellular activity is hampered by oxidative stress and macromolecular damage brought on by the abnormal accumulation and distribution of reactive iron, copper, and zinc. A rear up body of research suggests that abnormal transition metal homeostasis plays a substantial role in the aetiology of AD, an age-related neurodegenerative disease that manifests massive accumulations of oxidative stress-induced damage (Turnaturi et al. 2016).
Metals’ substantial significance in AD-type neurodegeneration is intriguing, and it opens up a possible opportunity for therapeutic intervention in these disorders. Graziella Vecchio and colleagues synthesised and characterised biotin derivatives with an 8-hydroxyquinoline moiety, such as Biotin-8-hydroxyquinoline (BHQ) and 8-hydroxyquinolyl-biotin hydrazone (HBHQ), a hydrazone conjugate of biotin (Fig. 12.2) with HQ and a series of transition metal complexes. Their metal complexes were also investigated as antioxidant agents. This research found that 8-hydroxyquinoline derivatives could be utilised to treat AD by regulating metal imbalances and reducing oxidative stress. Additionally, the inclusion of biotin may enhance their pharmacokinetics, such as improving absorption in the intestine and increasing bioavailability via the sodium-dependent multivitamin transporter (SMVT) (Turnaturi et al. 2016).
Pyridoxine (vitamin B6) was long thought to have only an enzyme cofactor role. Recently, it was discovered that it is a strong antioxidant. According to studies, pyridoxine prevents the synthesis of free radicals and acts as a single oxygen quencher. Additionally, epidemiological and clinical investigations revealed that an increased homocysteine (Hcy) level in the blood is a risk factor for developing AD. Pyridoxine deficiency causes Hcy levels to rise noticeably (Kennedy 2016; Yang et al. 2017). In addition, excessive Hcy concentrations may lead to elevated Aβ levels and are shown to accumulate in a transgenic mouse model of amyloidosis similar to AD. These advantages suggest that adding pyridoxine to a supplement may help with AD therapy.
The diverse spectrum of biological activities of resveratrol, a naturally occurring compound having a stilbene structure, has been studied intensively. Resveratrol seems to be an anti-AD agent with anti-inflammatory, antioxidant, and neuroprotective properties. Studies have also demonstrated that it has the capacity to inhibit monoamine oxidase, and these biological actions depend heavily on the stilbene structure (Yang et al. 2017). Additionally compounds with phenolic Mannich base moieties may show strong antioxidant, AChE inhibitory activity, and metal chelating characteristics. These findings point to vitamin B6 and resveratrol with Mannich base moieties as possible beginning points for the development of multifunctional medicines for the treatment of AD. Pyridoxine-resveratrol hybrids Mannich base compounds were synthesised and tested for their effect in AD. The majority of them demonstrated AChE and MAO-B-specific inhibition. In general, the inhibitory action against AChE was greatly boosted by the insertion of the Mannich base moiety to the 3′ or 4′ position of the benzene ring. However, it could drastically lessen MAO-B inhibitory action. Compounds 7d and 8b, having IC50 values of 2.11 μM and 1.56 μM, respectively, had the greatest efficacy for AChE inhibition among these derivatives. According to a kinetic analysis study, molecule 7d is bound to both the catalytic anionic site (CAS) and peripheral anionic site (PAS) of AChE, exhibiting a mixed-type inhibition. The majority of these molecules were specific MAO-B inhibitors for MAO. The strongest MAO-B inhibition was seen with compound 7e, having an IC50 value of 2.68 μM (Yang et al. 2017).
For the treatment of AD, another family of pyridoxine-based triazole compounds was identified as multi-target directed ligands. According to this study, 6 of the 17 produced pyridoxine-based triazoles exhibited high AChE inhibition and antioxidant activity. AChE activity was benefited by meta- and ortho-substitution on the aromatic ring. They discovered that 5i (EeAChE IC50 = 1.56 mM) is the best molecule in this new series through additional metal chelation studies (Pal et al. 2020).
Pyridoxine-carbamate-type derivatives of pyridoxine have metal chelating characteristics that can be used to modify bio-metals. Metal homeostasis in the brain is rather restrictive in normal physiological environments for healthy neuronal tissue functioning. Metal chelators may be employed to mitigate bio-metals’ impairment. In several disorders, including Wilson’s, thalassemia, multiple sclerosis, and AD, the preventive impact of metal chelators has been studied. In cases of copper, lead, mercury, and nickel poisoning, some medications, such as penicillamine, are utilised as chelators. The pyridoxine-carbamate series compound can be used to manage AD; these classes of molecules exhibited metal chelating and AChE binding capabilities in an experimental study (Pal et al. 2021). Pyridoxine and its derivatives are given in Fig. 12.3.
Folic acid and vitamin B12 are essential for the proper functioning of the central nervous system (CNS) at all stages of life, particularly in the conversion of homocysteine to methionine through the action of methionine synthase. This process is critical for nucleotide synthesis and methylation of both genomic and non-genomic material. Folic acid and vitamin B12 may also have a preventative role in the development of CNS abnormalities, mood disorders, and various forms of dementia, such as Alzheimer’s disease and vascular dementia in the elderly (Reynolds 2006). Vitamin B12 and folate are risk factors for dementia based on their relations as cofactors in homocysteine metabolism, and homocysteine has been related to the risk of developing AD. Folic acid is also involved in the metabolic pathway for acetylcholine synthesis. Another possible biological mechanism of folate effects on dementia is folate deficiency, which may decrease acetylcholine, a neurotransmitter that helps send messages between nerve cells, thus which leads to AD. Furthermore, a lack of folate increases oxidative stress; in terms of dementia, it may contribute to cognitive impairment of the ageing brain, sometimes resulting in reversible dementia but also increasing the likelihood of AD and vascular dementia (Reynolds 2002).
2.3 Vitamin C
A class of water-soluble vitamins includes vitamin C, commonly known as ascorbic acid. Most mammalian organisms can produce ascorbic acid on their own. Unfortunately, some animals, including guinea pigs, fruit bats, humans, and other primates, lack this ability because they lack the l-gulono-1,4-lactone oxidase enzyme; this enzyme is part of the biochemical pathway that produces vitamin C from glucose. Consequently, gut bacteria do not generate vitamin C. The factors mentioned above make these species rely entirely on nutritional consumption. The general recommendation of everyday intake of vitamin C is 90 mg for men and 75 mg for women. This amount should be raised by 35 mg for smokers (Kocot et al. 2017).
Vitamin C has two forms inside the organism. One is ascorbic acid; at bodily pH, it occurs in its anion form, ascorbate. Another form is dehydroascorbic acid. Ascorbate has a wide range of actions in the central nervous system (CNS) and brain. It acts via the donation of a single electron. It can directly scavenge oxygen- or nitrogen-based reactive species produced during regular cellular metabolism in terms of its antioxidant properties. Ascorbate will efficiently scavenge superoxide at the millimolar amounts found in neurons in vivo, a significant diffusible result of fast neuronal mitochondrial metabolism. According to research, ascorbic acid interacts with sodium-dependent vitamin C transporter-2 (SVCT2) to traverse the blood–brain barrier (BBB). Dehydroascorbic acid also penetrates the BBB through glucose transporters (GLUT) in its oxidised form. Vitamin C is a well-known antioxidant and can be helpful in AD (Harrison and May 2009).
Despite the advantages mentioned, ascorbic acid has significant pharmacological disadvantages, such as limited bioavailability. At neutral pH, ascorbic acid usually exists in the anionic form, which results in a slower diffusion through the plasma membrane. The bioavailability is observed to decline with increasing oral dosage, probably because of saturation of sodium-dependent vitamin C transporter-1 (SVCT1). Additionally, active transporters are necessary for distribution from the circulation to the intended organs. As a result, the concentration of ascorbic acid in plasma is 2.5 times greater than that in tissue. Applying a greater daily dose might not be able to get around this problem (Jiaranaikulwanitch et al. 2021).
Additionally, high consumption raises the risk of haemolysis in individuals with iron excess, paroxysmal nocturnal haemoglobinuria, oxalate kidney stone formation, and glucose 6-phosphate insufficiency. Moreover, vitamin C acts as a pro-oxidant because of its reducing nature. This phenomenon produces more ROS by reducing catalytic metals like Fe3+ or Cu2+ to Fe2+ and Cu+ (Jiaranaikulwanitch et al. 2021).
Ascorbic-triazole conjugates (Fig. 12.4) containing tryptoline and phenolic moieties were effective in AD. While phenolic moieties impact oxidative stress and amyloid aggregation, tryptoline is a well-known inhibitor of BACE1 (beta-site APP-cleaving enzyme 1) and choline esterase. Six ascorbic acid derivatives containing tryptoline and phenolic moieties connected by triazole linkers were described by Jutamas et al. 2c and 5c; two of these six compounds displayed encouraging results (Jiaranaikulwanitch et al. 2021). Both compounds demonstrated effectiveness against the amyloid cascade hypothesis, including inhibition of BACE1 (2c IC50 = 725.70 μM; 5c IC50 = 593.10 μM), suppression of amyloid aggregation (2c IC50 = 92.33 μM; 5c IC50 = 136.00 μM), and antioxidant (2c IC50 = 72.26 μM; 5c IC50 = 62.89 μM), anti-inflammatory, and neuroprotective action. Additionally, authors suggested that compounds 2c and 5c could work together to enhance molecules’ anti-amyloid and BACE1 inhibitory effects. As these compounds interact with the SVCT2 transporter, in silico studies indicate their possible permeability through the BBB (Jiaranaikulwanitch et al. 2021).
Ascorbic acid can be conjugated with other molecules to treat various disorders linked with the brain since it can pass across the BBB. Diclofenamic acid conjugates of ascorbic acid (Fig. 12.4) were explored extensively for their potential use in treating Alzheimer’s disease. Inhibition of cyclooxygenase (COX) might be beneficial in managing Alzheimer’s (Manfredini et al. 2002). Axel et al. developed a natural product based on palinurin-inspired derivatives (Asc1, Asc2, and Asc3) of ascorbic acid (Fig. 12.4) that demonstrated activity against GSK-3β. IC50 values of Asc1, Asc2, and Asc3 were >50 μM, 6.1 μM and 5.8 μM, respectively, for inhibition of GSK-3β. A hydrophobic chain was attached to ascorbic acid; this modification improved the kinase inhibitory activity. GSK-3β is a well-known target for AD treatment. Moreover, the authors reported that all three derivatives (Asc1, Asc2, and Asc3) bind to the allosteric site and do not compete with ATP or peptide substrate (Bidon-Chanal et al. 2013).
2.4 Vitamin D
The word “vitamin D” refers to a group of structurally similar and fat-soluble secosteroids such as ergocalciferol, cholecalciferol, 25-hydroxyvitamin D (calcidiol), and 1,25-dihydroxyvitamin D (calcitriol). Ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3) are the two major compounds under vitamin D. Vitamin D3 (cholecalciferol) is generally synthesised by humans’ epidermis (part of skin) from precursor molecule 7-dehydrocholesterol. Additionally it can be also obtained through the consumption of animal-based foods, while vitamin D2 (ergocalciferol) is mostly manufactured and added to food. Commercially produced vitamin D3 and vitamin D2 can be found in dietary supplements and foods that have been fortified. Only the side chain structure differentiates the D2 and D3 types. Both isoforms serve as prohormones; the variations do not alter metabolism (i.e., activation). When activated, it has been shown that the D2 and D3 forms show the same bodily reactions, and their effectiveness in treating vitamin D deficiency disease is equivalent. In addition, vitamin D2 has been found to be less harmful than vitamin D3 in experimental animal tests, although this has not been proven in humans (Jurutka et al. 2001; Gall and Szekely 2021).
Vitamin D is very crucial for humans and all other vertebrates. It plays a significant role in the maintenance of calcium and phosphate concentration in blood. It promotes the development of normal bone, optimum muscular contraction maintenance, and cellular functioning in many parts of the body. It is also involved in a wide range of biological processes, including cell proliferation and differentiation, immunological response, and cytokine control, in addition to their most well-known impact of regulating calcium absorption and stimulating bone mineralisation. According to published studies in the last two decades, the vitamin D signalling pathway has been implicated in several brain illnesses and brain functions (Gall and Szekely 2021). First, animal models’ studies showed that it influences how the brain develops in infancy and supports neuroprotection, synaptic plasticity, neural connectivity, and dopaminergic system turnover in adulthood. Second, epidemiological evidence demonstrated a link between children’s cognitive development abnormalities and low mother blood calcidiol levels during pregnancy. Third, serum calcidiol levels were lower in those with neurodegenerative disorders (such as Alzheimer’s and Parkinson’s disease), neuroinflammatory diseases, and neuropsychological ailments. Based on these findings, vitamin D supplementation was tried as a treatment for many neuropsychiatric conditions, such as dementia and cognitive impairment. However, there is no proof that higher vitamin D consumption increases vitamin D receptor (VDR) activation in the human brain (Gall and Szekely 2021).
Vitamin D can influence neurocognition via various pathways, including oxidative stress modulation, neuroprotection induction, inflammatory process suppression, and calcium homeostasis regulation (Bivona et al. 2019). The vitamin D receptor (VDR) goes through a conformational shift upon binding of vitamin D that enables the retinoid X receptor (RXR) association. Being a nuclear receptor RXR can bind to various sites on DNA and leads to many activities of vitamin D. It is hypothesised that the VDR-RXR complex actively interacts with the vitamin D response region found on the DNA. Vitamin D receptor as well as the CYP450 enzyme CYP27B1 that activates vitamin D both shows the expression in brain, additionally vitamin D and its metabolites are known to have blood–brain barriers permeability. Vitamin D decreases the breakdown of amyloid precursor protein (APP) by amyloidogenic β-secretase and increases the degradation of Aβ. In accordance with this, 25(OH) vitamin D therapy raised Aβ-degradation resulting in higher neprilysin (NEP) expression along with its activity, suggesting vitamin D derivatives as a rational approach for treatment of AD (Annweiler and Beauchet 2011; Grimm et al. 2017).
Most vitamin D analogues have side-chain modifications and have less calcaemic action than vitamin D3 which is naturally found, but they nonetheless have many of the same therapeutic qualities. For example, Maxacalcitol, a 1,25-hydroxylate vitamin D3 analogue which is used in the treatment of renal patients with secondary hyperparathyroidism. In contrast, Calcipotriol, a 1,24-hydroxylated vitamin D3 analogue which is used in the treatment of psoriasis, and Alfacalcidol, a 1-hydroxylated vitamin D3 analogue which is used to treat secondary hyperparathyroidism and osteoporosis (Grimm et al. 2017; Fan et al. 2019).
Paricalcitol and Doxercalciferol are vitamin D2 analogues. Paricalcitol has hydroxyl groups at C1 and C25, just like the vitamin D3 analogue maxacalcitol; however, it has a side chain of vitamin D2 instead of a vitamin D3 side chain. The vitamin D2 analogue 1-hydroxylated doxercalciferol is equivalent to alfacalcidol in terms of hydroxylation status. Paricalcitol and doxercalciferol treat secondary hyperparathyroidism, characterised by increased plasma parathyroid hormone levels (Grimm et al. 2017; Fan et al. 2019).
Vitamin D and all of the aforementioned D2 and D3 derivatives (Fig. 12.5) were investigated for their implications on Alzheimer’s disease. Marcus et al. reported that vitamin D3, vitamin D2 and their derivatives could be beneficial in signalling pathways related to AD. They also noted that these molecules elevate Aβ-degradation which indicates that vitamin D and its analogues play a crucial role in Aβ-homeostasis (Grimm et al. 2017). Their findings support vitamin D administration as a strategy for management and possible treatment of AD by increasing rate of Aβ catabolism, reducing Aβ anabolism, and lowering pro-inflammatory cytokines. Moreover, the studied vitamin D analogues have similar potencies for reducing Aβ levels. Still, they vary slightly in the effectiveness and exact mechanism, showing that different AD patients may benefit from vitamin D analogues to varying degrees. Vitamin D molecules like calcifediol and paricalcitol show increased non-amyloidogenic APP processing; therefore, AD patients having suppressed anti-amyloidogenic β-secretase activity may show better outcome from this treatment. As per their observations, vitamin D analogues with the major impacts on Aβ-degradation, such as calcipotriol and maxacalcitol, may be most beneficial for people with impaired Aβ-degradation (Grimm et al. 2017).
Almost all the vitamin D analogues show comparable effects for β- and γ-secretase processing, suggesting that those with higher amyloidogenic secretase activity shows beneficial effect from vitamin D derivatives in a similar way. It must be emphasised that there are only small differences in effect intensity and that all of the derivatives have been demonstrated to have similar positive effects on the Aβ level. Additionally, there were no discernible differences between vitamin D derivatives and vitamin D, indicates that vitamin D analogues as a treatment of AD had no therapeutic advantage over using calcifediol (or calcitriol) (Grimm et al. 2017).
Another important derivative of vitamin D3 is Denosomin-VD3 hybrids synthesised by Kenji et al. Denosomin (1-deoxy-24-norsominone) is a derivative of sominone, which is a natural steroid and found in Ashwagandha. Denosomin shows axonal extension activity on Aβ-damaged neurons. Kenji et al. reported that the denosomin-VD3 hybrid shows beneficial activity in Alzheimer’s via a 1,25D3-MARRS pathway (Sugimoto et al. 2015).
2.5 Vitamin E
Fat-soluble vitamin E is an antioxidant that regulates the generation of RNS and ROS. The hydroxyl group of vitamin E has antioxidant activity. It also modulates several cell signalling pathways and acts as a modulator of gene expression. Vitamin E has multiple forms depending upon their chemical structure, such as α-, β-, γ-, and δ-tocopherols and their related corresponding tocotrienols (Fig. 12.6), among which γ-tocopherol is the most prevalent in the diet. According to preclinical data, it is suggested that supplementing with vitamin E may be beneficial in AD since it not only reduces oxidative stress caused by Aβ but also improves memory and cognitive deficits. Tocotrienols exhibited promising results in AD animal models, exerting in some cases a more robust action than α-tocopherol, despite the fact that α-tocopherol is the vitamin E family member that has been the subject of most research. It shows synergistic antioxidant and anti-inflammatory activity when combining vitamin E with other compounds, thus which may help to treat AD (Gugliandolo et al. 2017).
Sang et al. designed several distinct chalcone-Vitamin E-donepezil hybrids (Fig. 12.7) multi-target active small molecules by combining vitamin E, donepezil, and chalcone. According to their studies, 17f is a good antioxidant, huMAO-B inhibitor, and a selective metal chelator as it inhibited AChE effectively (eeAChE IC50 1.88 μM and ratAChE IC50 0.41 μM). Also, the docking and kinetic experiments confirmed that 17f was an AChE inhibitor of mixed type. Additionally, it inhibited Cu2+- and self-induced Aβ1–42 aggregation with notable percentage rates of 93.5% and 78.0% at 25 M, respectively, and disassembled self- and Cu2+-induced aggregation of the accumulated Aβ1–42 fibrils with rates of 72.3% and 84.5%, respectively. Especially, 17f demonstrated good BBB permeability in vitro and neuroprotective impact on H2O2-induced PC12 cell damage, which indicates 17f is a potent multi-targeted ligand for treating AD (Sang et al. 2022).
An oxidative metabolite of α-tocopherol Alpha-Tocopherolquinone (α-TQ) (Fig. 12.7) has been shown to decrease Aβ induced cytotoxicity, oxidative stress, and inflammation by blocking Aβ42 fibril formation. It protects cells from oxidative stress by reversible two-electron redox cycling. Furthermore, it shows detox effects by eliminating reactive metabolites, suppressing ROS via quinine redox cycling, and generating the antioxidant hydroquinone (Crisostomo et al. 2007). α-TQ also inhibits Aβ aggregation, attenuated Aβ-induced cytotoxicity in SH-SY5Y neuroblastoma cells, and decreases inflammatory cytokine release as ROS and NO generation in BV-2 microglial cells in vitro (Yang et al. 2010). To investigate the effects and mechanisms of α-TQ on cognition and diseases in vivo, Wang et al. administered α-TQ orally to transgenic mice with AD. Their results demonstrated that α-TQ attenuated memory impairment, decreased Aβ oligomer levels, reduced lipid peroxidation, and restored superoxide dismutase activity in mice with AD. Furthermore, suppressing NF-κB signalling α-TQ decreased microglial activation and cytokine generation. These data imply that α-TQ has therapeutic promise in treating AD (Wang et al. 2016).
Tocotrienols and tocopherols vary structurally, as tocotrienols contain unsaturated isoprenoid side chains, whereas tocopherols comprise saturated side chains. It can address aspects of AD such as mitochondrial dysfunction, oxidative stress, and aberrant cholesterol production. Tocotrienol has been shown in preclinical investigations to lower oxidative stress by activating microbial activity and cellular repair, acting as a free radical scavenger; also, it protects cells from toxicity induced by glutamate. Human epidemiological research revealed a substantial inverse association between tocotrienol levels and AD development (Chin and Tay 2018). Tocotrienol is a potentially neuroprotective compound by lowering oxidative stress and promoting cellular repair, can halt the onset and progression of AD.
Ibrahim, Nor Faeizah, and colleagues studied the effects of vitamin E analogues such as α-tocotrienol (α-T3), γ-tocotrienol (γ-T3), and α-tocopherol (α-TOC) on Aβ oligomerization, aggregation, and disaggregation in vitro. They performed Thioflavin T (ThT) assay, which showed α-T3 reduced Aβ aggregation at 10 μM concentration. α-T3 and γ-T3 showed Aβ disaggregation, as evidenced by a decrease in ThT fluorescence α-TOC, on the other hand, had no impact. ThT assay results were confirmed with scanning electron microscopy imaging. Examination in the photoinduced cross-linking of unmodified protein assay revealed that γ-T3 reduced Aβ oligomerisation. Thus, tocotrienols have the potential role in developing therapeutic agents for AD (Ibrahim et al. 2021).
Trolox (Fig. 12.7) is the water-soluble and cell-permeable derivative of vitamin E that accumulates in the cytoplasm. It appeared to reduce Aβ plaque-induced oxidative stress and structural alterations in neurites and may neutralise free radical species, thus considered to be associated with ageing or AD. It can also prevent hydrogen peroxide and Aβ induced neurotoxicity and suppress GSK-3β (Munoz et al. 2002). As a result, various biological actions strengthen its neuroprotective capacity, making it a good lead for developing multifunctional drugs to treat AD. The increased tau hyperphosphorylation produced by Aβ depends on p38 mitogen-activated protein kinase (MAPK) and can be prevented by inhibiting MAPK. p38 is involved in the linkage of tau and Aβ. Giraldo et al. investigated the role of p38 signalling in AD and the protection provided by Trolox and found that incubation with Trolox inhibits Aβ-induced p38 activation (Giraldo et al. 2014).
Trolox has been used to develop tacrine–trolox hybrids to reduce metal-induced oxidative stress in AD. Teponnou et al. designed and synthesised tacrine-trolox hybrids having different linker chain lengths. Trolox moiety inhibited eqBuChE and TcAChE with IC50 of 3.16–128.82 nM, 17.37–2200 nM, respectively, and had free radical scavenging activities with IC50 in the range of 11.48–49.23 μM. Chains with longer linker lengths hybrids improved ChE inhibitory activity. The docking experiments showed that compound 8d could bind to the PAS and CAS of TcAChE and eqBuChE, implying that it can inhibit ChE-induced Aβ aggregation. Out of all the derivatives, they found compound 8d the most potent and the best lead molecule showing an ability to inhibit AChE and BuChE and acting as a robust antioxidant. With these results, 8d can be used as a multifunctional agent for treating AD (Teponnou et al. 2017).
Nepovimova et al. designed and synthesised 21 tacrine–trolox hybrids (7a–u) as multifunctional candidates against AD which exerts antioxidant and anticholinesterase activities with less in vivo toxicity after intramuscular administration in rats and the possible to cross the BBB. Their results demonstrated that derivative 7u is the key structure (Nepovimova et al. 2015).
2.6 Vitamin K
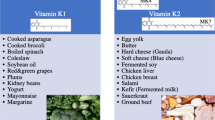
Vitamin K (VK) refers to a class of fat-soluble chemicals known as naphthoquinones, which includes naturally present vitamins K1 and K2 as well as synthetic vitamin K3 (Fig. 12.8). Olive oil and other green vegetables are the main sources of vitamin K1, while vitamin K2 is found in trace amounts in eggs, butter, etc. VK is mainly found as menaquinone-4 in the CNS, which controls the action of proteins taking part in chemotaxis, mitogenesis, cell proliferation, myelination, and neuroprotection (DiNicolantonio et al. 2015; Ferland 2012). VK, long known for its involvement in bone development and blood clotting, has recently emerged as a critical nutrient for brain function. Its deficiency is associated with changes in sphingolipid homeostasis that seem to be detrimental to the mechanisms responsible for producing and absorbing Aβ peptides (Grimm et al. 2016).
Derivatives of vitamin K2 (VK2) by Josey et al. revealed that for neuroprotective effect, particular structural core is important; for example, naphthoquinone and amine substitution at the 2′ carbon considerably increased its protective activity. After adding a benzyl group at 2′ amine, the compound’s safety index increased by eliminating neurotoxicity further; it also improved the compound’s protective potency by chloro-substitution at the meta site of an aromatic ring. They derived a series of VK2 analogues as 1a–g, of which 2j and 2q are more effective even at lesser concentrations. Compounds 2j, 2q, and VK2 are most likely exert their effects through PARL regulatory mechanism (Josey et al. 2013).
Huy, Pham Dinh Quoc, and colleagues developed analogues of vitamin K3 (VK3) that effectively protect neuroblastoma cells from Aβ-induced toxicity and prevent Aβ aggregation. They studied the VK3 analogue’s effects on various Aβ amyloidogenic properties, viz. free radical formation, cell viability, and aggregation, using biological and spectroscopic methods. Using molecular dynamics modelling, they determined the binding mode and affinity of VK3 analogues binding to Aβ and found several VK3 analogues inhibited Aβ aggregation. The computed inhibition constants for VK3–6, VK3–9, and VK3–10 were in the μM range, which is close to the IC50 of curcumin. It also revealed that VK3–9 might efficiently reduce free radicals and protect against Aβ-induced cytotoxicity and inhibit Aβ aggregation. Modified analogues of VK3 can thus be designed as efficient anti-amyloidogenic drugs for treating AD (Huy et al. 2013).
3 Conclusion
In conclusion, vitamin-based derivatives may show to be a promising strategy for the treatment of Alzheimer’s disease. Since it is a multifactorial disease, it needs therapy that can modify multiple cellular pathways. Vitamin-based derivatives exhibit antioxidant action, cholinesterase inhibitory activity, GSK-3β inhibitory activity, metal chelating activity, as well as some other properties that possibly slow the progression of Alzheimer’s disease. This chapter discusses the several vitamin derivatives that are developed and biologically evaluated for their effectiveness on Alzheimer’s disease.
Abbreviations
- AChE:
-
Acetylcholinesterase
- AD:
-
Alzheimer’s disease
- ADAM10:
-
A Disintegrin metalloproteinase 10
- APL:
-
Acute promyelocytic leukaemia
- ApoE:
-
Apolipoprotein E
- APP:
-
Amyloid precursor protein
- ATP:
-
Adenosine triphosphate
- ATRA:
-
All-trans RA
- Aβ:
-
Amyloid-beta
- BACE1:
-
Beta-site APP-cleaving enzyme 1
- BBB:
-
Blood-brain barrier
- BEXA:
-
Bexarotene
- BFT:
-
Benfotiamine
- BHQ:
-
Biotin-8-hydroxyquinoline
- BuChE:
-
Butyrylcholinesterase
- CAS:
-
Catalytic anionic site
- CNS:
-
Central nervous system
- COVID-19:
-
Coronavirus disease 2019
- COX:
-
Cyclooxygenase
- DBT:
-
Dibenzoylthiamine
- DNA:
-
Deoxyribonucleic acid
- FDA:
-
Food and Drug Administration
- GLUT:
-
Glucose transporters
- GSH:
-
Glutathione
- GSK-3:
-
Glycogen synthase kinase 3
- HBHQ:
-
8-Hydroxyquinolyl-biotin hydrazine
- IL-6:
-
Interleukin-6
- LPS:
-
Lipopolysaccharides
- MAO-B:
-
Monoamine oxidase B
- MAPK:
-
Mitogen-activated protein kinase
- MARRS:
-
Membrane-associated, rapid response steroid-binding
- MEM:
-
Memantine
- NAD:
-
Nicotinamide adenine dinucleotide
- NADP:
-
Nicotinamide adenine dinucleotide phosphate
- NEP:
-
Neprilysin
- NMDA:
-
N-Methyl-d-aspartate
- PAS:
-
Peripheral anionic site
- RA:
-
Retinoic acid
- RAR-α:
-
Retinoic acid receptor alpha
- RNA:
-
Ribonucleic acid
- RNS:
-
Reactive nitrogen species
- ROS:
-
Reactive oxygen species
- RXR:
-
Retinoid X receptor
- SVCT1:
-
Sodium-dependent vitamin C transporter-1
- SVCT2:
-
Sodium-dependent vitamin C transporter-2
- ThT:
-
Thioflavin T
- TrkB:
-
Tyrosine kinase receptor B
- VDR:
-
Vitamin D receptor
- VK:
-
Vitamin K
- VK2:
-
Vitamin K2
- VK3:
-
Vitamin K3
- α-T3:
-
Αlpha-tocotrienol
- α-TOC:
-
Αlpha-tocopherol
- α-TQ:
-
Alpha-tocopherolquinone
- γ-T3:
-
Gamma-tocotrienol
References
Abobaker A, Alzwi A, Alraied AHA (2020) Overview of the possible role of vitamin C in management of COVID-19. Pharmacol Rep 72(6):1517–1528
Annweiler C, Beauchet O (2011) Vitamin D-mentia: randomized clinical trials should be the next step. Neuroepidemiology 37(3–4):249–258
Balducci C, Paladini A, Micotti E, Tolomeo D, La Vitola P, Grigoli E, Richardson JC, Forloni G (2015) The continuing failure of bexarotene in Alzheimer’s disease mice. J Alzheimers Dis 46(2):471–482
Bhatti AB, Usman M, Ali F, Satti SA (2016) Vitamin supplementation as an adjuvant treatment for Alzheimer’s disease. J Clin Diagn Res 10(8):OE07–OE11
Bidon-Chanal A, Fuertes A, Alonso D, Perez DI, Martinez A, Luque FJ, Medina M (2013) Evidence for a new binding mode to GSK-3: allosteric regulation by the marine compound palinurin. Eur J Med Chem 60:479–489
Bivona G, Gambino CM, Iacolino G, Ciaccio M (2019) Vitamin D and the nervous system. Neurol Res 41(9):827–835
Chin KY, Tay SS (2018) A review on the relationship between tocotrienol and Alzheimer disease. Nutrients 10(7):881
Collins EG, Langbein WE, Orebaugh C, Bammert C, Hanson K, Reda D, Edwards LC, Littooy FN (2003) PoleStriding exercise and vitamin E for management of peripheral vascular disease. Med Sci Sports Exerc 35(3):384–393
Crisostomo AG, Moreno RB, Navaratnam S, Wilkinson JA, Bisby RH (2007) Generation of superoxide and singlet oxygen from alpha-tocopherolquinone and analogues. Free Radic Res 41(6):730–737
Czernichow S, Hercberg S (2001) Interventional studies concerning the role of antioxidant vitamins in cardiovascular diseases: a review. J Nutr Health Aging 5(3):188–195
Ding Y, Qiao A, Wang Z, Goodwin JS, Lee ES, Block ML, Allsbrook M, McDonald MP, Fan GH (2008) Retinoic acid attenuates beta-amyloid deposition and rescues memory deficits in an Alzheimer’s disease transgenic mouse model. J Neurosci 28(45):11622–11634
DiNicolantonio JJ, Bhutani J, O’Keefe JH (2015) The health benefits of vitamin K. Open Heart 2(1):e000300
Dong R, Wang H, Ye J, Wang M, Bi Y (2019) Publication trends for Alzheimer’s disease worldwide and in China: a 30-year bibliometric analysis. Front Hum Neurosci 13:259
Endres K, Fahrenholz F, Lotz J, Hiemke C, Teipel S, Lieb K, Tuscher O, Fellgiebel A (2014) Increased CSF APPs-alpha levels in patients with Alzheimer disease treated with acitretin. Neurology 83(21):1930–1935
Fahrenholz F, Tippmann F, Endres K (2010) Retinoids as a perspective in treatment of Alzheimer’s disease. Neurodegener Dis 7(1–3):190–192
Fan YG, Guo T, Han XR, Liu JL, Cai YT, Xue H, Huang XS, Li YC, Wang ZY, Guo C (2019) Paricalcitol accelerates BACE1 lysosomal degradation and inhibits calpain-1 dependent neuronal loss in APP/PS1 transgenic mice. EBioMedicine 45:393–407
Ferland G (2012) Vitamin K and the nervous system: an overview of its actions. Adv Nutr 3(2):204–212
Ford AH, Flicker L, Alfonso H, Thomas J, Clarnette R, Martins R, Almeida OP (2010) Vitamins B(12), B(6), and folic acid for cognition in older men. Neurology 75(17):1540–1547
Fukasawa H, Nakagomi M, Yamagata N, Katsuki H, Kawahara K, Kitaoka K, Miki T, Shudo K (2012) Tamibarotene: a candidate retinoid drug for Alzheimer’s disease. Biol Pharm Bull 35(8):1206–1212
Gall Z, Szekely O (2021) Role of vitamin D in cognitive dysfunction: new molecular concepts and discrepancies between animal and human findings. Nutrients 13(11):3672
Giraldo E, Lloret A, Fuchsberger T, Vina J (2014) Abeta and tau toxicities in Alzheimer’s are linked via oxidative stress-induced p38 activation: protective role of vitamin E. Redox Biol 2:873–877
Grimm MO, Mett J, Hartmann T (2016) The impact of vitamin E and other fat-soluble vitamins on Alzheimer’s disease. Int J Mol Sci 17(11):1785
Grimm MOW, Thiel A, Lauer AA, Winkler J, Lehmann J, Regner L, Nelke C, Janitschke D, Benoist C, Streidenberger O, Stotzel H, Endres K, Herr C, Beisswenger C, Grimm HS, Bals R, Lammert F, Hartmann T (2017) Vitamin D and its analogues decrease amyloid-beta (Abeta) formation and increase Abeta-degradation. Int J Mol Sci 18(12):2764
Gugliandolo A, Bramanti P, Mazzon E (2017) Role of vitamin E in the treatment of Alzheimer’s disease: evidence from animal models. Int J Mol Sci 18(12):2504
Harrison FE, May JM (2009) Vitamin C function in the brain: vital role of the ascorbate transporter SVCT2. Free Radic Biol Med 46(6):719–730
Hou N, Ren L, Gong M, Bi Y, Gu Y, Dong Z, Liu Y, Chen J, Li T (2015) Vitamin A deficiency impairs spatial learning and memory: the mechanism of abnormal CBP-dependent histone acetylation regulated by retinoic acid receptor alpha. Mol Neurobiol 51(2):633–647
Huy PD, Yu YC, Ngo ST, Thao TV, Chen CP, Li MS, Chen YC (2013) In silico and in vitro characterization of anti-amyloidogenic activity of vitamin K3 analogues for Alzheimer’s disease. Biochim Biophys Acta 1830(4):2960–2969
Ibrahim NF, Hamezah HS, Yanagisawa D, Tsuji M, Kiuchi Y, Ono K, Tooyama I (2021) The effect of alpha-tocopherol, alpha- and gamma-tocotrienols on amyloid-beta aggregation and disaggregation in vitro. Biochem Biophys Rep 28:101131
Jiaranaikulwanitch J, Pandith H, Tadtong S, Thammarat P, Jiranusornkul S, Chauthong N, Nilkosol S, Vajragupta O (2021) Novel multifunctional ascorbic triazole derivatives for amyloidogenic pathway inhibition, anti-inflammation, and neuroprotection. Molecules 26(6):1562
Joe E, Ringman JM (2019) Cognitive symptoms of Alzheimer’s disease: clinical management and prevention. BMJ 367:l6217
Josey BJ, Inks ES, Wen X, Chou CJ (2013) Structure-activity relationship study of vitamin K derivatives yields highly potent neuroprotective agents. J Med Chem 56(3):1007–1022
Jurutka PW, Whitfield GK, Hsieh JC, Thompson PD, Haussler CA, Haussler MR (2001) Molecular nature of the vitamin D receptor and its role in regulation of gene expression. Rev Endocr Metab Disord 2(2):203–216
Kapoor A, Wang BJ, Hsu WM, Chang MY, Liang SM, Liao YF (2013) Retinoic acid-elicited RARalpha/RXRalpha signaling attenuates Abeta production by directly inhibiting gamma-secretase-mediated cleavage of amyloid precursor protein. ACS Chem Neurosci 4(7):1093–1100
Kennedy DO (2016) B Vitamins and the brain: mechanisms, dose and efficacy—a review. Nutrients 8(2):68
Kocot J, Luchowska-Kocot D, Kielczykowska M, Musik I, Kurzepa J (2017) Does vitamin C influence neurodegenerative diseases and psychiatric disorders? Nutrients 9(7):659
Kumar N, Gahlawat A, Kumar RN, Singh YP, Modi G, Garg P (2022) Drug repurposing for Alzheimer’s disease: in silico and in vitro investigation of FDA-approved drugs as acetylcholinesterase inhibitors. J Biomol Struct Dyn 40(7):2878–2892
Kurutas EB (2016) The importance of antioxidants which play the role in cellular response against oxidative/nitrosative stress: current state. Nutr J 15(1):71
La Fata G, Weber P, Mohajeri MH (2014) Effects of vitamin E on cognitive performance during ageing and in Alzheimer’s disease. Nutrients 6(12):5453–5472
Littlejohns TJ, Henley WE, Lang IA, Annweiler C, Beauchet O, Chaves PH, Fried L, Kestenbaum BR, Kuller LH, Langa KM, Lopez OL, Kos K, Soni M, Llewellyn DJ (2014) Vitamin D and the risk of dementia and Alzheimer disease. Neurology 83(10):920–928
Lu’o’ng K, Nguyen LT (2011) Role of thiamine in Alzheimer’s disease. Am J Alzheimers Dis Other Dement 26(8):588–598
Manfredini S, Pavan B, Vertuani S, Scaglianti M, Compagnone D, Biondi C, Scatturin A, Tanganelli S, Ferraro L, Prasad P, Dalpiaz A (2002) Design, synthesis and activity of ascorbic acid prodrugs of nipecotic, kynurenic and diclophenamic acids, liable to increase neurotropic activity. J Med Chem 45(3):559–562
Mimori Y, Katsuoka H, Nakamura S (1996) Thiamine therapy in Alzheimer’s disease. Metab Brain Dis 11(1):89–94
Munoz FJ, Opazo C, Gil-Gomez G, Tapia G, Fernandez V, Valverde MA, Inestrosa NC (2002) Vitamin E but not 17beta-estradiol protects against vascular toxicity induced by beta-amyloid wild type and the Dutch amyloid variant. J Neurosci 22(8):3081–3089
Nepovimova E, Korabecny J, Dolezal R, Babkova K, Ondrejicek A, Jun D, Sepsova V, Horova A, Hrabinova M, Soukup O, Bukum N, Jost P, Muckova L, Kassa J, Malinak D, Andrs M, Kuca K (2015) Tacrine-trolox hybrids: a novel class of centrally active, nonhepatotoxic multi-target-directed ligands exerting anticholinesterase and antioxidant activities with low in vivo toxicity. J Med Chem 58(22):8985–9003
Osimani A, Berger A, Friedman J, Porat-Katz BS, Abarbanel JM (2005) Neuropsychology of vitamin B12 deficiency in elderly dementia patients and control subjects. J Geriatr Psychiatry Neurol 18(1):33–38
Pal T, Bhimaneni S, Sharma A, Flora SJS (2020) Design, synthesis, biological evaluation and molecular docking study of novel pyridoxine-triazoles as anti-Alzheimer’s agents. RSC Adv 10(44):26006–26021
Pal T, Patil P, Sharma A (2021) Synthesis, molecular docking and spectroscopic studies of pyridoxine carbamates as metal chelator. J Mol Struct 1223:128837
Pan X, Gong N, Zhao J, Yu Z, Gu F, Chen J, Sun X, Zhao L, Yu M, Xu Z, Dong W, Qin Y, Fei G, Zhong C, Xu TL (2010) Powerful beneficial effects of benfotiamine on cognitive impairment and beta-amyloid deposition in amyloid precursor protein/presenilin-1 transgenic mice. Brain 133(Pt 5):1342–1351
Pan X, Chen Z, Fei G, Pan S, Bao W, Ren S, Guan Y, Zhong C (2016) Long-term cognitive improvement after benfotiamine administration in patients with Alzheimer’s disease. Neurosci Bull 32(6):591–596
Rai SN, Singh P, Steinbusch HW, Vamanu E, Ashraf G, Singh MP (2021) The role of vitamins in neurodegenerative disease: an update. Biomedicine 9(10):1284
Reynolds EH (2002) Folic acid, ageing, depression, and dementia. BMJ (Clinical research ed) 324(7352):1512–1515
Reynolds E (2006) Vitamin B12, folic acid, and the nervous system. Lancet Neurol 5(11):949–960
Sambon M, Gorlova A, Demelenne A, Alhama-Riba J, Coumans B, Lakaye B, Wins P, Fillet M, Anthony DC, Strekalova T, Bettendorff L (2020) Dibenzoylthiamine has powerful antioxidant and anti-inflammatory properties in cultured cells and in mouse models of stress and neurodegeneration. Biomedicine 8(9):361
Sambon M, Wins P, Bettendorff L (2021) Neuroprotective effects of thiamine and precursors with higher bioavailability: focus on benfotiamine and dibenzoylthiamine. Int J Mol Sci 22(11):5418
Sang Z, Song Q, Cao Z, Deng Y, Zhang L (2022) Design, synthesis, and evaluation of chalcone-vitamin E-donepezil hybrids as multi-target-directed ligands for the treatment of Alzheimer’s disease. J Enzyme Inhib Med Chem 37(1):69–85
Semba RD (2012) The discovery of the vitamins. Int J Vitam Nutr Res 82(5):310–315
Singh YP, Shankar G, Jahan S, Singh G, Kumar N, Barik A, Upadhyay P, Singh L, Kamble K, Singh GK, Tiwari S, Garg P, Gupta S, Modi G (2021) Further SAR studies on natural template based neuroprotective molecules for the treatment of Alzheimer’s disease. Bioorg Med Chem 46:116385
Singh YP, Kumar N, Priya K, Chauhan BS, Shankar G, Kumar S, Singh GK, Srikrishna S, Garg P, Singh G, Rai G, Modi G (2022) Exploration of neuroprotective properties of a naturally inspired multifunctional molecule (F24) against oxidative stress and amyloid beta induced neurotoxicity in Alzheimer’s disease models. ACS Chem Neurosci 13(1):27–42
Starling-Soares B, Carrera-Bastos P, Bettendorff L (2020) Role of the synthetic B1 vitamin sulbutiamine on health. J Nutr Metab 2020:9349063
Sugimoto K, Yajima H, Hayashi Y, Minato D, Terasaki S, Tohda C, Matsuya Y (2015) Synthesis of denosomin-vitamin D3 hybrids and evaluation of their anti-Alzheimer’s disease activities. Org Lett 17(23):5910–5913
Tapias V, Jainuddin S, Ahuja M, Stack C, Elipenahli C, Vignisse J, Gerges M, Starkova N, Xu H, Starkov AA, Bettendorff L, Hushpulian DM, Smirnova NA, Gazaryan IG, Kaidery NA, Wakade S, Calingasan NY, Thomas B, Gibson GE, Dumont M, Beal MF (2018) Benfotiamine treatment activates the Nrf2/ARE pathway and is neuroprotective in a transgenic mouse model of tauopathy. Hum Mol Genet 27(16):2874–2892
Teponnou GAK, Joubert J, Malan SF (2017) Tacrine, trolox and tryptoline as lead compounds for the design and synthesis of multi-target agents for Alzheimer’s disease therapy. Open Med Chem J 11:24–37
Tippmann F, Hundt J, Schneider A, Endres K, Fahrenholz F (2009) Up-regulation of the alpha-secretase ADAM10 by retinoic acid receptors and acitretin. FASEB J 23(6):1643–1654
Tousi B (2015) The emerging role of bexarotene in the treatment of Alzheimer’s disease: current evidence. Neuropsychiatr Dis Treat 11:311–315
Turnaturi R, Oliveri V, Vecchio G (2016) Biotin-8-hydroxyquinoline conjugates and their metal complexes: exploring the chemical properties and the antioxidant activity. Polyhedron 110:254–260
Wang SW, Yang SG, Liu W, Zhang YX, Xu PX, Wang T, Ling TJ, Liu RT (2016) Alpha-tocopherol quinine ameliorates spatial memory deficits by reducing beta-amyloid oligomers, neuroinflammation and oxidative stress in transgenic mice with Alzheimer’s disease. Behav Brain Res 296:109–117
Xu J, Patassini S, Begley P, Church S, Waldvogel HJ, Faull RLM, Unwin RD, Cooper GJS (2020) Cerebral deficiency of vitamin B5 (d-pantothenic acid; pantothenate) as a potentially-reversible cause of neurodegeneration and dementia in sporadic Alzheimer’s disease. Biochem Biophys Res Commun 527(3):676–681
Yang SG, Wang WY, Ling TJ, Feng Y, Du XT, Zhang X, Sun XX, Zhao M, Xue D, Yang Y, Liu RT (2010) Alpha-tocopherol quinone inhibits beta-amyloid aggregation and cytotoxicity, disaggregates preformed fibrils and decreases the production of reactive oxygen species, NO and inflammatory cytokines. Neurochem Int 57(8):914–922
Yang X, Qiang X, Li Y, Luo L, Xu R, Zheng Y, Cao Z, Tan Z, Deng Y (2017) Pyridoxine-resveratrol hybrids Mannich base derivatives as novel dual inhibitors of AChE and MAO-B with antioxidant and metal-chelating properties for the treatment of Alzheimer’s disease. Bioorg Chem 71:305–314
Zandona A, Lihtar G, Marakovic N, Mis K, Busic V, Gaso-Sokac D, Pirkmajer S, Katalinic M (2020) Vitamin B3-based biologically active compounds as inhibitors of human cholinesterases. Int J Mol Sci 21(21):8088
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
The authors declare no conflict of interest.
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Varma, T., Kamble, P., Kumari, M., Diwakar, V., Garg, P. (2023). Vitamin-Based Derivatives for the Management of Alzheimer’s Disease. In: Sharma, A., Modi, G.P. (eds) Natural Product-based Synthetic Drug Molecules in Alzheimer's Disease. Springer, Singapore. https://doi.org/10.1007/978-981-99-6038-5_12
Download citation
DOI: https://doi.org/10.1007/978-981-99-6038-5_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-6037-8
Online ISBN: 978-981-99-6038-5
eBook Packages: MedicineMedicine (R0)