Abstract
Alzheimer’s disease (AD) is a severe neurodegenerative ailment of the brain, affecting millions of elderly people globally. It has also created a great health concern in the future. Several acquired disease conditions and some other factors enhance the chance of developing AD. No treatment can completely cure AD. Scientific literature has established that vitamins have a number of targets in the aetiology of AD through which they act to prevent the neuronal dysfunction in the disease. Thus, by understanding the role of vitamins, we are able to state that vitamins can be a good choice to overcome the detrimental effects of AD. Antioxidant vitamins play a major role because they act by reducing the degree of oxidative stress in the brain. The categories of vitamins having promising effects in declining the course of AD and its symptoms are reviewed. Low vitamin intake can increase the chances of acquiring AD. Fortunately, these significant vitamins that protect the brain can be acquired through various fruits and vegetables that are discussed here.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
2.1 Introduction
A severe neurodegenerative ailment of the brain known as Alzheimer’s disease (AD) is characterized by extracellular beta-amyloid plaques, intraneuronal tau fibrillary tangles, cell death of cholinergic neurons, vascular pathology, and inflammation (Terry et al. 1994). The chance of developing AD is increased by acquired ailments such cerebrovascular disease, diabetes, hypertension, obesity, and dyslipidemia. Globally, there are approximately 50 million AD patients, and this number is expected to double every 5 years to reach 152 million by 2050 (Vogel et al. 2009). Many factors, including nutritional factors, influence the disease, but its cause has not been established. It is reported that the deficiency of certain vitamins also leads to the progression of AD. Consuming these vitamin supplements plays a crucial role in the decline of AD.
Vitamins are collections of highly complex molecules. They are organic in nature and present in food in small amounts and are necessary for regular metabolism. When these nutrients are lacking, it results in various disorders, but when these nutrients are replenished, they cure those deficiency symptoms. Compared to lipids, carbohydrates, and proteins, vitamins are diverse in nature. The organic nature of vitamins sets them apart from other categories, and their classification is based on their chemical makeup and function. Vitamins are required in extremely minute quantities for development, health, and reproduction (Maqbool et al. 2018). AD is incurable today, although treatments exist to ease its symptoms (Livingston et al. 2020). The use of appropriate supplements and a properly balanced diet can contribute to improving the clinical condition of patients with AD.
2.2 AD and Antioxidant Vitamins
Antioxidant vitamins preserve the body from “free radicals,” which harm cells and can result in cancer, heart disease, and Alzheimer’s disease. Numerous antioxidants exist, including beta-carotene, vitamins C and E, and resveratrol. They can be found in meals that come from plants, such bell peppers, berries, and greens.
Grapes, red wine, peanuts, and certain dark chocolate all contain resveratrol. It may provide antiaging benefits and reduce the chance of developing certain diseases, according to scientific studies. For a while, researchers hypothesized that resveratrol could be able to shield the brain from the symptoms of AD. A recent study found that daily resveratrol dosages did decrease the disease’s progression.
During the aging, free radicals frequently accumulate in the nerve cells. One of the elements causing the development and progression of neurodegenerative processes is increased oxidative stress. According to research on the brains of Alzheimer’s patients, the body has been attempting to prevent free radical damage by showing indicators of oxidative stress (Swaminathan and Jicha 2014).Therefore, consuming more antioxidants would seem to be beneficial. However, there isn’t currently a simple solution. Antioxidants may be better obtained through food than from supplements; however, researchers are unsure if particular antioxidants are superior to others.
A probable connection between dietary antioxidants and AD may be explained by a number of biological processes. Age-related oxidative stress of the brain tissue and lymphocytes, increased free radical buildup, and impaired antioxidant mechanisms are all reported. Antioxidants may, in the first instance, reduce the degree of oxidative stress in the brain. Thus, antioxidants may lessen the quantity of DNA deterioration, neuronal cell death, and amyloid accumulation in the brain (Swaminathan and Jicha 2014; Christen 2000). Second, a large intake of antioxidants may lessen the risk of dementia by lowering the risk of atherosclerosis since AD is linked to both cardiovascular risk factors and atherosclerosis (Hofman et al. 1997; Breteler 2000) and oxidative processes are implicated in atherogenesis (Witztum and Steinberg 1991). The risk of dementia may be decreased by halting the creation of these events, which are all significant neuropathological aspects of AD. Antioxidants’ pleiotropic mechanisms, which include reducing oxidized lipid membranes, preventing nucleic acid damage, and preventing protein carbonylation, impede the discovery of a broken particular route that leads to the development of AD. There are a group of vitamins showing promising effects in AD prevention and management (Fig. 2.1).
2.3 Fat-Soluble Vitamins
2.3.1 Vitamin A
Vitamin A, a fat-soluble micronutrient, plays a crucial role in a number of physiological processes, including the generation of red blood cells, immunology, and reproduction. The early development of brain form and function, neuronal proliferation and differentiation, neurite outgrowth, and synaptogenesis are the crucial functions that vitamin A plays in the central nervous system (CNS) (Ono and Yamada 2012). The amounts of vitamin A and beta-carotene in the CSF and blood of AD patients were found to be significantly lowered. It is observed that the average alpha-tocopherol and retinol serum concentration was lower in AD patients as compared to that of the control participants after screening by age, sex, and cardiovascular comorbidities (Bourdel-Marchasson et al. 2001).Vitamin A and beta-carotene have been demonstrated to impact the onset of neurodegenerative illnesses. In comparison with the control group, patients with dementia had significantly lower plasma levels of antioxidants that break chains, such as vitamins A, C, and E (Foy et al. 1999).
A key process that frequently results in neuronal toxicity in AD is the oligomerization of Aß fibrils. Another action of vitamin A and beta-carotene is the inhibition of the production and instability of Aβ fibrils (Ono and Yamada 2012). The aggregation and oligomerization of Aβ40 and Aβ42 fibrils have been demonstrated to be reduced by vitamin A administration, however. Beta-carotene and vitamin A have also been found to stop the decrease of cognitive function in AD. Additionally, these individuals’ improved memory function and spatial learning have been linked to greater amounts of these vitamins (Takasaki et al. 2011; Rivière et al. 1998). Activation of microglia in the nervous system is one of the characteristics of inflammation of the nervous system. Neuropsychiatric diseases are characterized by inflammation both chronically and acutely. According to credible research, microglia activation is one of the factors that lead to AD (Sodhi and Singh 2014).The local concentrations of retinoic acid may also alter as a result of the microglia malfunctioning. Moreover, through interactions with retinoic acid and retinoid X receptors, vitamin A and its derivatives play a crucial role in the differentiation of nerve cells, as well as in the production of neurotransmitters in the brain and gene expression.
2.3.2 Vitamin D
The significance of vitamin D in preserving strong bones has long been established. Recent findings by scientists show a connection between vitamin D and a number of mental processes, including memory and learning. Neurons in the brain and spine that are involved in the production of neurotransmitters and the formation of new nerves are activated by vitamin D. Inflammation is a prevalent feature of Alzheimer’s; thus, researchers also think that vitamin D protects brain neurons and lowers inflammation (Rogers et al. 1988). Especially for people over 65, vitamin D is one of the most crucial vitamins. The aged people over 65 are thought to be vitamin D deficient for a certain cause that is unique and is covered in the section below. Vitamin D insufficiency is associated with significant health complications.
Because it is increasingly difficult for human bodies to produce vitamin D in the aged people, vitamin D deficiency poses a special concern. In comparison with people in their 20s, individuals over the age of 70 make 70% less vitamin D. Ninety-five percent of seniors are thought to be vitamin D deficient. People having a higher risk of vitamin D insufficiency include those who live in regions with shorter days and those who spend less time outside. It is thought that vitamin D assists in regulating the immune system. Vitamin D supplementation is thought to improve one’s ability to fight off illnesses and reduce the danger of contracting them. Numerous studies have shown an association between cognitive decline, AD, and dementia and vitamin D insufficiency. According to a research from the University of Cambridge, those who have severe vitamin D deficiency are twice as likely to have cognitive impairment (Granic et al. 2015). This is in contrast to people who have optimal vitamin D levels.
2.3.3 Vitamin E
The body utilizes vitamin E for a diverse range of purposes, making it a crucial nutrient. Because of its antioxidative qualities, vitamin E may be able to treat Alzheimer’s, according to researchers. The central nervous system has a place to store vitamin E, which lowers lipid peroxidation and amyloid buildup. Antioxidant-based therapy should be started as soon as the condition may be diagnosed. Cholinesterase levels in the brain are decreased by vitamin E.
Dementia and blood levels of vitamins C and E are associated with AD patients. Because of its capacity to scavenge free radicals, lower amyloid activity, and involvement in the chelation of iron, zincs, and copper, ascorbic acid has a neuroprotective impact. It protects the central nervous system from free radical damage. A pro-oxidative diet has been demonstrated to raise the quantity of amyloid precursor protein in a rat research. In individuals with mild to severe AD, vitamin E alone demonstrated to reduce cognitive impairment. It’s interesting to note that memantine treatment when combined with α-tocopherol had fewer favorable results (Liao et al. 2010). Humans require vitamin E as a micronutrient because it helps keep cell membranes healthy. Depending on age, many nations suggest a daily dietary consumption of between 3 and 15 mg of vitamin E. Tocopherols and tocotrienols are abundant in seeds and edible oils like those made from almond, peanut, olive, palm, canola, corn, and soybean while being sparse in plant foods like fruit and vegetables that have low lipid levels.
Vitamin E is the most significant lipophilic radical scavenger in vivo; its primary function is as an antioxidant. In order to neutralize free radicals, vitamin E primarily uses a hydrogen atom transfer process. This reaction yields a non-radical product and a vitamin E radical, which may then attack lipids or react with a reducing agent like vitamin C or ubiquinol to renew vitamin E. As the predominant form of vitamin E in tissues, α-tocopherol has been the subject of most research. In lipoproteins and cell membranes, α-tocopherol functions as a chain-breaking antioxidant, reducing lipid peroxidation and protecting membrane integrity. Tocotrienols, in contrast to α-tocopherol, may have distinct health-improving effects and a higher antioxidant capacity, according to certain research (Serbinova et al. 1991).
“Oxidative agents” are toxic substances that damage the brain and cause AD. Vitamin E typically guards against the brain’s damage from these oxidative radicals. But studies have revealed that those who have Alzheimer’s have particularly low levels of vitamin E (Persson et al. 2014). According to some scientists, the low levels of vitamin E allow oxidative agents to harm the brain. The brain is also harmed by cholinesterase, which is thought to be a factor in AD. Researchers determine vitamin E slows the growth of Alzheimer’s.
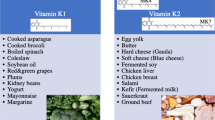
2.3.4 Vitamin K
It is now well acknowledged that vitamin K has strong evidence supporting its crucial functions in the neurological system. One theory is that vitamin K may also contribute to the pathogenesis of AD, a crippling condition for which there is now no treatment. Sphingolipids are a significant group of lipids that are abundantly found in the membranes of brain cells. Alterations in sphingolipid metabolism have been associated with neurodegenerative diseases like AD and age-related cognitive impairment. Numerous studies have demonstrated the function of vitamin K in brain physiology by participating in sphingolipid metabolism and the biological activation of the vitamin K-dependent protein Gas6. Cell development, survival, and apoptosis are just a few of the many cellular activities that Gas6 is functionally engaged with. New evidence also points to the K vitamin menaquinone-4 (MK-4)’s distinct protective effects against oxidative stress and inflammation (Ferland 2012). Overall, the evidence suggests that vitamin K has an impact on cognition and psychomotor behavior.
According to a recent study, people with early-stage AD consumed less vitamin K than control subjects with normal cognitive function. Dietary vitamin K intakes were evaluated using food records from 5 nonconsecutive days gathered from 31 community-dwelling early-stage AD patients and 31 age- and sex-matched cognitively intact control participants. On a person-day basis, the mean vitamin K intake was 63 ± 90 μg/day in patients and 139 ± 233 μg/day in controls. The principal sources of vitamin K are green vegetables. Green vegetables thus contributed 33% and 49%, respectively, to total intakes in patients and control participants. Subjects with AD consumed fewer green vegetables overall, which contributed to their reduced vitamin K intakes (Presse et al. 2008). The main finding of the abovementioned study is that individuals with likely early-stage AD had considerably lower vitamin K intakes than healthy people who were age- and sex-matched. Nevertheless, they are consistent with the most current studies on vitamin K and AD, which contend that inadequate vitamin K intakes may increase the chance of developing AD or hasten its course.
Elderly people and apolipoprotein E4 carriers have an increased risk of developing AD. In older men and women, a relative vitamin K deficit that affects the vitamin’s extrahepatic actions is prevalent. Comparatively to those with other APOE genotypes, APOE4 carriers have decreased levels of vitamin K in their blood circulation. In the brain, vitamin K has crucial functions. According to mounting evidence, vitamin K regulates sulfotransferase activity and the activation of a growth factor/tyrosine kinase receptor (Gas 6/Axl). It is currently believed that vitamin K insufficiency plays a role in the etiology of AD and that taking vitamin K supplements may help with either disease prevention or treatment. Additionally, cardiovascular disease-related neuronal damage may also be lessened by vitamin K (Allison 2001).
Recent research has emphasized the value of vitamin K2 (VK2) for maintaining human health. However, there have been no clinical studies looking into VK2’s potential for treating or preventing AD. An increasing body of data indicating that VK2 has the ability to retard the advancement of AD and contribute to its prevention is found in reviewing basic science research and clinical trials that have linked VK2 to elements implicated in its pathogenesis. Numerous studies have noted VK2’s antiapoptotic and antioxidant activities as well as its impacts on cardiovascular health, mitochondrial dysfunction, cognition, neuroinflammation, and comorbidities in AD (Fig. 2.2). Dysbiosis and VK2 are related in the context of the microbiome’s role in the development of AD (Popescu and German 2021).
2.4 Water Soluble Vitamins
2.4.1 B-Complex
The B vitamins with the most conclusively known links to cognitive deterioration are vitamin B12, niacin, and thiamine. The nerve system and brain of the human play a critical function for B vitamins. Vitamin B6 is required to produce the chemicals that neurons use to communicate with one another, while vitamins B3 and B9 are necessary to generate and repair DNA. The development and repair of vital components of the human neurological system are just a few of the tasks that the B vitamins do, in addition to providing the brain with the energy it needs to function.
B vitamin supplement users had a lower risk of AD than nonusers, according to research from the University of Oxford and the Centers for Disease Control and Prevention (CDC). B vitamins have important functions in several regions of the neurological system and brain.
2.4.1.1 Vitamin B1
Thiamine deficiency in human leads to widespread beriberi, which has a substantial neurological impact. Many researches suggest that neurological issues such as cognitive impairments and encephalopathy are attributed to thiamine inadequacy. The etiology of AD is also related to vitamin B1 (Lu'o'ng and Nguyen 2011; Hazell et al. 2013). Three important enzymes, pyruvate dehydrogenase (PDH), alpha-ketoglutarate dehydrogenase, and alpha-transketolase, are the cofactors for thiamine pyrophosphate. Alpha-ketoglutarate dehydrogenase and alpha-transketolase, enzymes that depend on vitamin B for activity in the brain and peripheral tissues, have been found to have lower plasma levels of vitamin B1 in Alzheimer’s patients (Fessel 2021). The three enzymes decarboxylate their substrates and transfer the resulting acyl groups to coenzymes A (CoA), which results in the regeneration of nicotinamide adenine dinucleotide hydride. A deficiency of these enzymes impairs brain metabolism and decreases synapse metabolism. The submedial thalamic nucleus constitutes the most susceptible portion of the brain with thiamine deficiency and causes selective cell death in the brain. AD patients’ brains have lower levels of thiamine-dependent enzymes, which are required for glucose metabolism and their decrease, and thiamine deficit may be accountable for the deterioration in glucose metabolism (Calingasan et al. 1999). It has been well explored that oxidative stress and inflammation contribute in the preferential neurons that are lost in this zone and the activation of other cell types. For AD patients, increasing thiamine levels in the brain may be therapeutic.
2.4.1.2 Vitamin B2
Animals and vegetables both contain large amounts of vitamin B2, often known as riboflavin. Through a variety of biological oxidation processes, vitamin B6 metabolism, energy production, and cell development, it benefits human health. Moreover, it influences how iron is absorbed, stored, and mobilized by the body (Powers 2003). Additionally, B2 exhibit antioxidant properties. Riboflavin is also significant as an antioxidant in the glutathione redox cycle. Flavin adenine dinucleotide (FAD) and flavin mononucleotide (FMN) are precursors of vitamin B2. Through the reduction of FAD by decreased nicotinamide adenine dinucleotide phosphate (NADPH), glutathione reductase is activated. For the glutathione redox cycle to function continuously, it is necessary to complete this important phase (Saedisomeolia and Ashoori 2018). So it is common to monitor glutathione reductase activity in order to determine the condition of cellular riboflavin. Therefore, riboflavin deficiency may contribute to the development and stabilization of neurodegenerative disorders where oxidative stress is enhanced. There is mounting evidence that oxidative stress plays a significant role in the pathogenesis of neurodegenerative disorders (Mariani et al. 2005). The brain endures excessive oxidative stress as a result of oxidants being released during the advancement of AD (Mangialasche et al. 2009). Reactive oxygen species are remnants of aerobic metabolism, and intracellular enzymes and antioxidants regulate their level (Schaffer and Bronnikova 2012; Apel and Hirt 2004). Reactive oxygen species are transient signaling molecules that are at low levels during normal physiological circumstances. The peroxidation process, which significantly damages proteins, phospholipids, and DNA, is led on by an excessive generation of reactive oxygen species. The oxidase activity of mitochondrial cytochrome C can be reduced by these damages, which can lead to metabolic disruption and cell death (Joodi et al. 2011). In humans, vitamin B2 supplementation may activate conserved signaling pathways that prevent the emergence and progression of neurodegenerative disorders like AD.
2.4.1.3 Vitamin B3
The development of nerve cells, the production of useful energy for the brain, and DNA synthesis and repair are all facilitated by vitamin B3. B3 also acts as a potent antioxidant and aids in brain cell regeneration.
Niacin, commonly known as nicotinic acid, is a kind of vitamin B3 that has subsequently drawn the attention of some scientists. Over the past 20 years, a few epidemiological studies that suggested a link between niacin intake and a lower risk of general cognitive deterioration have raised interest in the vitamin. Recently, scientists have started investigating if the substance benefits people with neurodegenerative illnesses. In mouse models for Parkinson’s, glioblastoma, and multiple sclerosis, recent research findings have revealed that niacin can influence the activity of microglia, crucial immune cells in the brain (Dursun and Gezen-Ak 2019). An AD mouse model has recently demonstrated the first signs of this protective effect.
Researchers are investigating the vitamin B3 niacinamide, also known as nicotinamide, for its potential to reduce tau, a protein that builds up in tangles in the brains of those with AD. A potential approach for the treatment of AD and other dementias is the supplementation of nicotinamide adenine dinucleotide (NAD) to restore the damaged mitochondria. A safe NAD precursor with a high oral bioavailability, nicotinamide ribose slows down the aging process (Bachurin et al. 2018). According to CDC researchers, those who consume fewer vitamin B3 are more likely to acquire AD. Additionally, the study found that vitamin B3 levels above normal reduced the growth of Alzheimer’s.
2.4.1.4 Vitamin B5
Coenzyme A (CoA) and its subsequent derivatives, such as acetyl-CoA, succinyl-CoA, malonyl-CoA, and 3-hydroxy-3-methylglutaryl (HMG)-CoA, are all precursors to pantothenic acid, also known as vitamin B5. In many biological processes, including the metabolism of nucleic acids, carbohydrates, proteins, and lipids, CoA is an essential cofactor. It is involved in the process that creates the vital anti-inflammatory hormone cortisol. It is crucial for myelinization and synthesis of the neurotransmitter acetylcholine. Additionally, vitamin B5 may lessen oxidative stress by encouraging the formation of glutathione. Numerous foods made from plants and animals contain pantothenic acid. Furthermore, this vitamin can be obtained via fermented foods. It has been calculated that human gut bacteria could contribute 0.078% of the recommended daily intake of this vitamin and that 51% of the human gut microbiota genomes include the genes for the pathway that synthesize vitamin B5.
Humans with experimentally induced pantothenic acid shortage had sleeplessness and other health problems. It’s interesting to note that significant vitamin B5 deficiency was found in the brain tissues of AD patients in a recent postmortem investigation. These alterations were particularly noticeable in the hippocampus, entorhinal cortex, and middle temporal gyrus, three brain regions linked to the pathogenesis of AD. The scientists concluded that a vitamin B5 deficiency may be a factor in the development of dementia and neurodegeneration in AD since CoA is involved in the formation of acetylcholine and myelin in the brain. Additionally, a postmortem investigation of patients with Huntington’s disease found that the vitamin B5 levels in their brain tissues had significantly decreased globally. Animal research proved cerebral pantothenate was primarily localized to myelin-containing regions, supporting the aforementioned findings (Rudzki et al. 2021).
2.4.1.5 Vitamin B6
The three chemically different molecules pyridoxal, pyridoxamine, and pyridoxine that make up vitamin B6 are important in the control of mood and cognitive function. A lack of vitamin B6 is linked to an increase in blood homocysteine levels because it is a crucial cofactor in homocysteine re-methylation. Homocysteine may directly damage central nervous system neurons in addition to being a risk factor for cerebrovascular disease. A vitamin B6 deficiency has been associated with neuropsychiatric illnesses such as seizures, migraines, chronic pain, and depression. Older persons frequently have low vitamin B6 levels, according to epidemiological research. A reason or mechanism for the onset of AD and other kinds of dementia has been proposed: hyperhomocysteinaemia. It has been shown that taking supplements of B vitamins, especially vitamin B6, lowers blood homocysteine levels (Malouf and Grimley Evans 2003). In the generation of neurotransmitters, vitamin B6 is utilized. Nerves interact with one another through neurotransmitters, which are chemicals. The digestion of foods to produce energy for the human brain requires B6.
2.4.1.6 Vitamin B9
The water-soluble, naturally occurring form of vitamin B9 is called folate, and it may be found in a variety of foods. Amino acids and DNA are two substances required for the correct operation of practically every system in the human body, and vitamin B9 is crucial for their production. In addition to its role in DNA and RNA synthesis, folate also helps to the metabolism of proteins. Homocysteine, an amino acid that may be harmful to the body in high doses, must be broken down in order for it to function. In addition to being necessary for the production of healthy red blood cells, folate is also crucial during periods of rapid growth, such as during pregnancy and the development of the fetus.
An increasing number of researches suggest that the crucial nutrient folate is essential for the progression of AD (Robinson et al. 2018). Folate concentrations in the plasma and serum should not exceed 45.3 nmol/L. When plasma/serum folate levels are below 6.8 nmol/L and above 13.5 nmol/L, respectively, folate deficiency and probable deficiency are considered to exist (WHO 2015). Previous researches suggested that low folate levels are correlated to all kinds of dementia, including vascular dementia and AD, in addition to particular areas of cognitive performance such as episodic recall and recognition (Wahlin et al. 1996). Additionally, supplementing with folate and folic acid helps to improve cognitive abilities in elderly people and in situations of moderate cognitive impairment (Ma et al. 2019). In addition, a lack of folate causes an increase in tau phosphorylation, which is a key component of neurofibrillary tangles (Chan and Shea 2006). Compared to healthy controls, folate levels were decreased in AD patients. A suspected or actual folate deficit may raise the risk of AD. The chance of developing AD may be lowered by getting enough folate each day. Studies have already revealed that people with moderate cognitive impairment who take folic acid supplements experience a slower rate of brain shrinkage and cognitive loss (Ma et al. 2019). According to these results, getting enough folate can help prevent AD. Randomized controlled studies are required to establish the link between folic acid supplementation or adequate folate consumption and the prevention of AD.
2.4.1.7 Vitamin B12
It is widely known that vitamin B12 functions as a cofactor in the one carbon cycle process where the neurotoxic homocysteine is converted to methionine by the enzyme methionine synthase (Chan and Shea 2006). New aspects of vitamin B12’s role as a gene regulator and an epigenetics modifier impacting brain intellectual abilities have been revealed in the last 10 years (Vogel et al. 2009). The essential function of B12 in the brain is implied by the presence of the cubam receptor, a particular transporter receptor that is identical to that found in the gut (Douaud et al. 2013). Moreover, there is broad agreement that proven AD sufferers have a B12 inadequacy (Dayon et al. 2017), emphasizing the potentially beneficial function of B12 consumption in the treatment of recognized AD. Accordingly, it was shown that older individuals with moderate dementia who received vitamin B supplements saw a sevenfold reduction in brain gray matter shrinkage in AD susceptible areas (Morris 2003). Although research investigating the efficacy of B12 and its mechanistic function in verified AD is few, they seldom relate B12 impact to cholinergic pathways and barely ever link B12 effect to homocysteine, despite seeming clinically beneficial.
Making, maintaining, and repairing the myelin sheath are one of vitamin B12’s most crucial jobs. The layer that shields and surrounds nerve cells is called the myelin sheath. For nerves to communicate with one another, it is essential. Nerve cells are unable to interact when the myelin sheath is destroyed, as it is in Alzheimer’s and dementia (Liao et al. 2010). As a result, a variety of mental issues arise, including the inability to create new memories and communication issues. Vitamin B12 deficiency has a well-known neurologic condition that is defined by cognitive and mental problems, as well as by subacute combined degeneration of the spinal cord and peripheral neuropathy (Goetz and Pappert 1999; Savage and Lindenbaum 1995). Additionally, cognitive problems caused by the neurologic condition can be improved with high-dose vitamin B12 treatment (Allen et al. 1990; Kuzminski et al. 1998). Also, vitamin B12 is required to develop and sustain nerve cells.
2.4.2 Vitamin C
The proper function of the brain is significantly influenced by vitamin C, according to earlier in vivo and in vitro research. The assumption that vitamin C has preventive benefits throughout the spectrum of neurodegenerative illnesses was further supported by decreased plasma levels in patients despite appropriate consumption (Montilla-López et al. 2002). In accordance with a study by Polidori et al. (2015), a certain serum levels of vitamin C may be essential for the prevention of AD and other clinical signs of vascular and cognitive aging. Therefore, it may be established that antioxidant vitamins offer defense against damage caused by oxidative stress in AD. Vitamin C can prevent the progression of AD because of the effects it has on the disease’s pathophysiology in several ways (Fig. 2.3). Numerous investigations, both in vivo and in vitro, came to the conclusion that vitamin C prevents the oligomerization of the Aß peptide, hence assisting in reducing oxidative stress.
Oxidative stress in the tissue is brought on by brain damage, which lowers the amounts of antioxidants like SOD and vitamin C. Supplementing with vitamin C appears to increase SOD levels, which subsequently reduce oxidative stress and stop additional brain damage from occurring (Harrison 2012). Even a typical diet’s consumption of vitamin C may have a neuroprotective impact in AD patients, according to a theory. In addition, it has been shown that Alzheimer’s patients (Fig. 2.3) who consume enough vitamin C experience much less cognitive deterioration (Zandi et al. 2004).
2.5 Conclusion
A serious neurological disorder associated with aging is AD. Since there are more people suffering from AD, it is necessary to find a medication that can stop or slow the disease’s growth. Although there is no known cure for Alzheimer’s, there are therapies that may slow down the disease’s course as well as medication and non-medication approaches that might assist to manage symptoms. In order to manage symptoms and enhance quality of life, people with the condition and those who care for them might benefit from being aware of their alternatives. Understanding available alternatives can aid those suffering with the condition and those who are caring for them in managing symptoms and enhancing quality of life. The risk of AD may be reduced by consuming a diet high in vitamins (Fig. 2.3). Consuming enough fruits and vegetables will make up for vitamin deficiencies, which are typically seen in dementia patients.
References
Allen RH, Stabler SP, Savage DG, Lindenbaum J (1990) Diagnosis of cobalamin deficiency I: usefulness of serum methylmalonic acid and total homocysteine concentrations. Am J Hematol 34(2):90–98
Allison AC (2001) The possible role of vitamin K deficiency in the pathogenesis of Alzheimer’s disease and in augmenting brain damage associated with cardiovascular disease. Med Hypotheses 57(2):151–155
Apel K, Hirt H (2004) Reactive oxygen species: metabolism, oxidative stress, and signal transduction. Annu Rev Plant Biol 55:373–399
Bachurin SO, Gavrilova SI, Samsonova A, Barreto GE, Aliev G (2018) Mild cognitive impairment due to Alzheimer disease: contemporary approaches to diagnostics and pharmacological intervention. Pharmacol Res 129:216–226
Bourdel-Marchasson I, Delmas-Beauvieux MC, Peuchant E, Richard-Harston S, Decamps A, Reignier B, Emeriau JP, Rainfray M (2001) Antioxidant defences and oxidative stress markers in erythrocytes and plasma from normally nourished elderly Alzheimer patients. Age Ageing 30(3):235–241
Breteler MM (2000) Vascular risk factors for Alzheimer's disease: an epidemiologic perspective. Neurobiol Aging 21(2):153–160
Calingasan NY, Uchida K, Gibson GE (1999) Protein-bound acrolein: a novel marker of oxidative stress in Alzheimer's disease. J Neurochem 72(2):751–756
Chan A, Shea TB (2006) Dietary and genetically-induced oxidative stress alter tau phosphorylation: influence of folate and apolipoprotein E deficiency. J Alzheimer's Dis 9(4):399–405
Christen Y (2000) Oxidative stress and Alzheimer disease. Am J Clin Nutr 71(2):621S–629S
Dayon L, Guiraud SP, Corthésy J, Da Silva L, Migliavacca E, Tautvydaitė D, Oikonomidi A, Moullet B, Henry H, Métairon S, Marquis J, Descombes P, Collino S, Martin FJ, Montoliu I, Kussmann M, Wojcik J, Bowman GL, Popp J (2017) One-carbon metabolism, cognitive impairment and CSF measures of Alzheimer pathology: homocysteine and beyond. Alzheimers Res Ther 9(1):43
Douaud G, Refsum H, de Jager CA, Jacoby R, Nichols TE, Smith SM, Smith AD (2013) Preventing Alzheimer's disease-related gray matter atrophy by B-vitamin treatment. Proc Natl Acad Sci U S A 110(23):9523–9528
Dursun E, Gezen-Ak D (2019) Vitamin D basis of Alzheimer's disease: from genetics to biomarkers. Hormones (Athens) 18(1):7–15
Ferland G (2012) Vitamin K, an emerging nutrient in brain function. Biofactors 38(2):151–157
Fessel J (2021) Supplemental thiamine as a practical, potential way to prevent Alzheimer's disease from commencing. Alzheimer's dementia (N. Y.) 7(1):e12199
Foy CJ, Passmore AP, Vahidassr MD, Young IS, Lawson JT (1999) Plasma chain-breaking antioxidants in Alzheimer's disease, vascular dementia and Parkinson's disease. QJM 92(1):39–45
Goetz CG, Pappert EJ (1999) Textbook of clinical neurology. W.B. Saunders, Philladelphia
Granic A, Hill TR, Kirkwood TB, Davies K, Collerton J, Martin-Ruiz C, von Zglinicki T, Saxby BK, Wesnes KA, Collerton D, Mathers JC, Jagger C (2015) Serum 25-hydroxyvitamin D and cognitive decline in the very old: the Newcastle 85+ study. Eur J Neurol 22(1):106–1e7
Harrison FE (2012) A critical review of vitamin C for the prevention of age-related cognitive decline and Alzheimer's disease. J Alzheimers Dis 29(4):711–726
Hazell AS, Faim S, Wertheimer G, Silva VR, Marques CS (2013) The impact of oxidative stress in thiamine deficiency: a multifactorial targeting issue. Neurochem Int 62(5):796–802
Hofman A, Ott A, Breteler MM, Bots ML, Slooter AJ, van Harskamp F, van Duijn CN, Van Broeckhoven C, Grobbee DE (1997) Atherosclerosis, apolipoprotein E, and prevalence of dementia and Alzheimer's disease in the Rotterdam study. Lancet 349(9046):151–154
Joodi G, Ansari N, Khodagholi F (2011) Chitooligosaccharide-mediated neuroprotection is associated with modulation of Hsps expression and reduction of MAPK phosphorylation. Int J Biol Macromol 48(5):726–735
Kuzminski AM, Del Giacco EJ, Allen RH, Stabler SP, Lindenbaum J (1998) Effective treatment of cobalamin deficiency with oral cobalamin. Blood 92(4):1191–1198
Liao WC, Chen JR, Wang YJ, Tseng GF (2010) Methylcobalamin, but not methylprednisolone or pleiotrophin, accelerates the recovery of rat biceps after ulnar to musculocutaneous nerve transfer. Neuroscience 171(3):934–949
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, Mukadam N (2020) Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet 396(10248):413–446
Lu'o'ng KV, Nguyen LT (2011) Role of thiamine in Alzheimer's disease. Am J Alzheimers Dis Other Dement 26(8):588–598
Ma F, Zhou X, Li Q, Zhao J, Song A, An P, Du Y, Xu W, Huang G (2019) Effects of folic acid and vitamin B12, alone and in combination on cognitive function and inflammatory factors in the elderly with mild cognitive impairment: a single-blind experimental design. Curr Alzheimer Res 16(7):622–632
Malouf R, Grimley Evans J (2003) The effect of vitamin B6 on cognition. Cochrane Database Syst Rev 4:CD004393
Mangialasche F, Polidori MC, Monastero R, Ercolani S, Camarda C, Cecchetti R, Mecocci P (2009) Biomarkers of oxidative and nitrosative damage in Alzheimer's disease and mild cognitive impairment. Ageing Res Rev 8(4):285–305
Maqbool MA, Aslam M, Akbar W, Iqbal Z (2018) Biological importance of vitamins for human health: a review. J Agric Basic Sci 2(3):50–58
Mariani E, Polidori MC, Cherubini A, Mecocci P (2005) Oxidative stress in brain aging, neurodegenerative and vascular diseases: an overview. J Chromatogr B Analyt Technol Biomed Life Sci 827(1):65–75
Montilla-López P, Muñoz-Agueda MC, FeijóoLópez M, Muñoz-Castañeda JR, Bujalance-Arenas I, Túnez-Fiñana I (2002) Comparison of melatonin versus vitamin C on oxidative stress and antioxidant enzyme activity in Alzheimer's disease induced by okadaic acid in neuroblastoma cells. Eur J Pharmacol 451(3):237–243
Morris MS (2003) Homocysteine and Alzheimer's disease. Lancet Neurol 2(7):425–428
Ono K, Yamada M (2012) Vitamin a and Alzheimer's disease. Geriatr Gerontol Int 12(2):180–188
Persson T, Popescu BO, Cedazo-Minguez A (2014) Oxidative stress in Alzheimer's disease: why did antioxidant therapy fail? Oxidative Med Cell Longev 2014:1
Polidori MC, Ruggiero C, Croce MF, Raichi T, Mangialasche F, Cecchetti R, Pelini L, Paolacci L, Ercolani S, Mecocci P (2015) Association of increased carotid intima-media thickness and lower plasma levels of vitamin C and vitamin E in old age subjects: implications for Alzheimer's disease. J Neural transm 122(4):523–530
Popescu A, German M (2021) Vitamin K2 holds promise for Alzheimer’s prevention and treatment. Nutrients 13(7):2206
Powers HJ (2003) Riboflavin (vitamin B-2) and health. Am J Clin Nutr 77(6):1352–1360
Presse N, Shatenstein B, Kergoat MJ, Ferland G (2008) Low vitamin K intakes in community-dwelling elders at an early stage of Alzheimer's disease. J Am Diet Assoc 108(12):2095–2099
Rivière S, Birlouez-Aragon I, Nourhashémi F, Vellas B (1998) Low plasma vitamin C in Alzheimer patients despite an adequate diet. Int J Geriatr Psychiatry 13(11):749–754
Robinson N, Grabowski P, Rehman I (2018) Alzheimer's disease pathogenesis: is there a role for folate? Mech Ageing Dev 174:86–94
Rogers J, Luber-Narod J, Styren SD, Civin WH (1988) Expression of immune system-associated antigens by cells of the human central nervous system: relationship to the pathology of Alzheimer's disease. Neurobiol Aging 9(4):339–349
Rudzki L, Stone TW, Maes M, Misiak B, Samochowiec J, Szulc A (2021) Gut microbiota-derived vitamins–underrated powers of a multipotent ally in psychiatric health and disease. Prog Neuro-Psychopharmacol Biol Psychiatry 107:110240
Saedisomeolia A, Ashoori M (2018) Riboflavin in human health: a review of current evidences. Adv Food Nutr Res 83:57–81
Savage DG, Lindenbaum J (1995) 11 neurological complications of acquired cobalamin deficiency: clinical aspects. Baillieres Clin Haematol 8(3):657–678
Schaffer WM, Bronnikova TV (2012) Peroxidase-ROS interactions. Nonlin Dyn 68(3):413–430
Serbinova E, Kagan V, Han D, Packer L (1991) Free radical recycling and intramembrane mobility in the antioxidant properties of alpha-tocopherol and alpha-tocotrienol. Free Radic Biol Med 10(5):263–275
Sodhi RK, Singh N (2014) Retinoids as potential targets for Alzheimer's disease. Pharmacol Biochem Behav 120:117–123
Swaminathan A, Jicha GA (2014) Nutrition and prevention of Alzheimer’s dementia. Front Aging Neurosci 6:282
Takasaki J, Ono K, Yoshiike Y, Hirohata M, Ikeda T, Morinaga A, Takashima A, Yamada M (2011) Vitamin a has anti-oligomerization effects on amyloid-β in vitro. Alzheimer's Dis 27(2):271–280
Terry RD, Masliah E, Hansen LA (1994) Structural basis of the cognitive alterations in Alzheimer disease, Alzheimer Dis 179–196
Vogel T, Dali-Youcef N, Kaltenbach G, Andres E (2009) Homocysteine, vitamin B12, folate and cognitive functions: a systematic and critical review of the literature. Int J Clin Pract 63(7):1061–1067
Wahlin A, Hill RD, Winblad B, Bäckman L (1996) Effects of serum vitamin B12 and folate status on episodic memory performance in very old age: a population-based study. Psychol Aging 11(3):487–496
WHO (2015 Serum and red blood cell folate concentrations for assessing folate status in populations. https://apps.who.int/iris/handle/10665/75584
Witztum JL, Steinberg D (1991) Role of oxidized low density lipoprotein in atherogenesis. J Clin Invest 88(6):1785–1792
Zandi PP, Anthony JC, Khachaturian AS, Stone SV, Gustafson D, Tschanz JT, Norton MC, Welsh-Bohmer KA, Breitner JC, Cache County Study Group (2004) Reduced risk of Alzheimer disease in users of antioxidant vitamin supplements: the Cache County study. Arch Neurol 61(1):82–88
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kiruba, J., Justin Thenmozhi, A., Jayalakshmi, M., Arockia Jeya Yasmi Prabha, E. (2023). Role of Vitamins in Alzheimer’s Disease. In: Thenmozhi, A.J., Manivasagam, T. (eds) Nutraceuticals for Alzheimer's Disease: A Promising Therapeutic Approach. Nutritional Neurosciences. Springer, Singapore. https://doi.org/10.1007/978-981-99-0677-2_2
Download citation
DOI: https://doi.org/10.1007/978-981-99-0677-2_2
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-0676-5
Online ISBN: 978-981-99-0677-2
eBook Packages: MedicineMedicine (R0)