Abstract
The development of Multifunctional Fabric Antennas for Biomedical Applications at 2.36–2.45 GHz ISM Band is proposed here. Using Wireless Body Area Network (WBAN) technology, a low-profile Wearable microstrip patch antenna is built and proposed in this study for continuous detection of patient monitoring, including cardiac output, heartbeat, and respiration. During the course of our work, we developed prototype antennas using a variety of substrate materials, including Teflon, Polyimide, Polytetrafluoroethylene (PTFE), Nylon, and Polystyrene. For metrics like Reflection coefficient, Gain, Directivity, VSWR, Efficiency, and Bandwidth, the built-in antenna was simulated and compared. To achieve better return loss, VSWR, and gain, geometry is modified like S-shaped antenna that operates at 2.5 GHz. At 2.5 GHz, the optimum reflection coefficient values of −45, −38, −25, and −28 dB were obtained against different substrates like polyimide, Teflon, PTFE, and polystyrene, respectively.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
As a result of longer lifespans, which is mostly due to the significant advancements in public health, nutrition, and medicine, the world's aging population has been quickly expanding. By 2035, it is expected that there will be an increasing number of older people; the number of people aged 85 years and over was estimated to be 1.7 million in 2020 (2.5% of the UK population) and this is projected to almost double to 3.1 million by 2045 (4.3% of the UK population) (Office of National Statistics 2022), nearly two times as many people over the age of 65 in the United States (National Institute and on Aging (NIA) 2016), twice as many people over the age of 60 in the People's Republic of China (https://worldpopulationreview.com/countries/china-population, 2022), and by 2050, Japan will have the oldest population in recorded history, with an average age of 52 (https://worldpopulationreview.com/countries/china-population, 2022). In many affluent nations, public healthcare systems are simultaneously dealing with a rise in the number of individuals being diagnosed with chronic conditions like obesity and diabetes. These chronic diseases are caused by improper food, a sedentary lifestyle, and insufficient physical exercise rather than just the aging of the population (U.S. Department of Health and Human Services 2020; World Health Organization, Food and Agriculture Organization of the United Nations 2018). By 2030, diabetes is predicted to overtake heart disease as the seventh greatest cause of death, according to the World Health Organization (WHO) (https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases#:~:text=Key%20facts,%2D%20and%20middle%2Dincome%20countries). Diabetes is a significant condition due to its chronic nature, both for members and for healthcare organizations. These estimates and figures show that the expense of healthcare systems is rising dramatically as a result of the ongoing provision of medical treatment to patients with chronic illnesses and the growing population of older individuals with varied health issues (Switzerland. xxxx; Bodenheimer et al. 2009; Hayes and Gillian 2020). As a result, healthcare systems cannot continue as they are now (Bodenheimer et al. 2009; Bhargava 2021). Early disease identification and diagnosis, in the opinion of scientists (Jazieh and Kozlakidis 2020; Botha et al. 2014; Tossaint-Schoenmakers et al. 2021; Lehnert et al. 2011), is crucial because it both helps to successfully halt the progression of sickness (Lehnert et al. 2011; Yach et al. 2004; Leifer 2003) and greatly lowers the expense of healthcare systems.
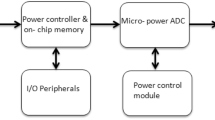
The use of wireless technology in medical devices has increased recently. Implantable and wearable wireless sensors may now include radio transceivers and biological sensor devices due to significant advancements in microelectronics. These gadgets record and keep track of a patient's essential physiological data before sending it to a remote node within, on, or near the body (Levin and Stevens 2011) (Fig. 7.1).
The classification of body-centric wireless communication
Off-body, on-body, or in-body wireless body-centric communication is categorized as part of personal area networks and body-area networks (Alzheimer’s Association Report 2011). The first kind of communication occurs between an off-body system or device and an on-body one. Within on-body networks and wearable devices, the second class serves as the wireless communication interface. The third class is wireless communication to sensor networks and medical implants (Fig. 7.2). In reality, all three types of body-centric communication are used in an integrated system, and clear distinctions between them may not always be made. Even yet, the categorization may be used to show the many difficulties that wearable and implantable antennas must overcome.
IOT-based Wireless Healthcare monitoring system
The IoT-enabled health monitoring system is very different than the conventional health care system. Because of this, IoT makes it harder to get the results and performance that are needed. As all sensors are connected to voltage signals, working with IoT systems is analogous to working in the embedded domain (Pahwa and Lyons 2010). Initially, equipment such as sensors, detectors, monitors, and the microcontroller are connected so that they can operate in accord. The microcontroller performs the analog-to-digital conversion so that data may be read in the proper digital format. The converted data is sent as an input signal to a Microcontroller in an IoT Board, with Raspberry Pi being the most often used microcontroller these days (Fig. 7.3).
System Support during Covid Pandemic
The global spread of the COVID-19 pandemic has significantly altered people's daily lives dramatically. The delayed manufacturing and distribution of vaccinations has put a strain on both developing and wealthy nations’ health systems (Garcia-Pardo et al. 2018). Thus, various governments are quite concerned about the surveillance of COVID-19 infected and recovered patients in the wards (Hall and Hao 2006; Bhardwaj et al. 2022; Momtazmanesh et al. 2020; Iftekhar et al. 2021). As COVID-19 spread can be mitigated by implementing an Internet of things (IoT)-based remote health monitoring system. Biomedical signals can provide information about a person's health; a large amount of data can be collected, and suitable conclusions can be drawn from observation. The Internet of Things has revolutionized the lives of individuals, particularly senior patients, by providing continuous monitoring of health issues. Wearables such as fitness bands and other remotely connected gadgets such as blood pressure and pulse monitors provide patients with access to individualized care. These devices may be customized to send reminders for step count, water consumption, doctor's visits, blood pressure variations, and more. Pulse count, SPO2, temperature, blood pressure, and some other biological data might be detected to identify the COVID-19. Artificial Intelligence techniques might be used to detect COVID-19 patients from a vast quantity of data by monitoring health markers and storing them on the cloud via IoT (Thapliyal et al. 2021). The combination of machine learning with IoT will be beneficial in a variety of ways. IoT technology would assist public health officials in segregating patients who require immediate care from those who might be isolated at home removing the big patient bubble from hospitals and neighborhood health centers (Priesemann et al. 2021).
The smart health monitoring system based on IoT might minimize the need for O2 in hospitals. This device might possibly be equipped with a GPS chip to track the position of the rescued patient. During a lockdown situation, the individuals’ data is shared with the health authorities, and the potentially contaminated individuals are isolated as soon as feasible. An autonomous health monitoring system that reacts or generates an alarm in the event of a patient's severe condition is to be devised (Islam et al. 2020; Kumar and Mukesh 2013). The data is evaluated using the Node MCU microcontroller to deliver notifications to physicians and concerned individuals through emails. It also stores and keeps track of previous diagnostic information about the patient’s health. The patient’s real status is relayed to medical specialists via an Internet portal, and the right medication may be administered to cure the patient.
System Requirements and challenges of WBAN
-
1.
Challenges Presented by E-Textiles
The characterization of the physical layer of the network is an essential phase in the process of developing a WBAN. This step involves making an estimate of the delay spread as well as the path loss between any two nodes located on the body. In order to accomplish this goal, a comprehensive assessment of the electromagnetic wave propagation and antenna behavior close to the human body is required. For both the conductive portions and the substrate, textile materials may be used effectively. Electronic chips and, in general, surface-mounted components (SMCs) must be able to be soldered to the conductive sections using tin solder (Levin and Stevens 2011) (Fig. 7.4).
-
2.
Data Rates
Data rates vary significantly in the healthcare context due to the variety of Wireless Body Area Network applications. Low-data-rate sensors are required for On-Body sensors, while high-data-rate systems are encouraged for multimedia data transmission to the cloud (Khan et al. 2021). Burst transmission uses a lot of energy since it transmits data at a very high speed for a very short period of time. The reliability of wireless monitoring systems in medical applications depends on the data rates used. High data rate devices are best employed in low BER settings, while low data rate devices can survive high Bit Error Rate (BER) situations.
-
3.
Security and Privacy
WBAN systems need security measures to ensure the safety, privacy, reliability, and confidentiality of patient health information. A supporting WBAN infrastructure must apply particular security processes (Khan et al. 2021). WBAN systems provide the security and privacy of patient information. Data is secure while sent, gathered, processed, and stored. A patient may not want his/her information shared with insurance companies, which might deny coverage. Intruders may also modify information by physically grabbing a node, which can lead to a patient's death. Medical records may be used to find a patient’s rivals. This sensitive and vital information should be protected from unwanted access, usage, and alterations (Islam et al. 2020; Srividya and Satyanarayana 2018; Roges and Malik 2021; Rahim and Malik 2021; Malik et al. 2020) (Fig. 7.5).
Antenna Layout
Implantable antennas must be bioavailable in order to guarantee human community safety implant rejection. Moreover, cell lines are sensitive, and if enabled to come into direct touch with the implanted antenna's passivation, they would short-circuit it. The prevention of unwanted short circuits is especially important in the case of antennas intended for long-term implantation. The hypothesized inverse E-shaped microstrip monopole antenna is mathematically constructed using ADS software to operate in the 2.5 GHz ISM band. The antenna is positioned on a different substrate material with a different dielectric constant. The overall dimensions of the antenna are 27 × 15 × 0.16 mm3, highlighting the design's compactness when compared to current antennas. Initially, the proposed antenna was designed without any ground structure and the reflection coefficient was very low. Then defected ground structure was made to improve the reflection coefficient. Even another dielectric layer was added to improve the desired gain. Different substrates were used to obtain the required results.
As shown in Fig. 7.6, the computed and measured reflection coefficients of the antenna in free space, with and without the DGS and dielectric ground structure, are compared. Meanwhile, the suggested EBG-enhanced antenna significantly increased. When the DGS and dielectric substrate is incorporated, both results show good impedance matching with a slight shift in the resonant frequency. The need for excellent dielectric (substrate/superstrate) materials: High-permittivity dielectrics are picked for surgically implanted radiating patch since they truncate the efficacious wavelength as well as lead to reduced resonance frequencies, aiding and abetting in antenna size reduction. Even with such high-permittivity dielectrics, the substrate layer insulates the antenna from the higher-permittivity tissue. Thicker substrates raise the working frequency of the antenna, necessitating larger physical dimensions to refine resonance. Dielectric materials with high permittivity values and thin substrate layers are therefore sought.
Result and Comparison
The return loss at 2.5 GHz seems to be good polyimide, Teflon, PTFE, and polystyrene substrate. The respective return losses are −45, −38, −25, and −28 dB. The comparison graph is given in Figure (Figs. 7.7 and 7.8) (Table 7.1).
a Return loss for the proposed antenna with polyimide substrate, b return loss for the proposed antenna with Teflon substrate, c return loss for the proposed antenna with polytetrafluoroethylene (PTFE) substrate, d return loss for the proposed antenna with nylon substrate, and e return loss for the proposed antenna with polystyrene substrate
Medical implant communication systems (MICS) are made up of an implanted screening tool and an additional surveillance device that is positioned a certain distance (usually 2 m) outward. Preferable connections are being used to alter device parameters, transmit stored information, and transmit effective performance measurement tracking data. Thus, irrespective of resource restrictions, the implanted antenna must pass the message powerful enough for it to be picked up by the external device. It is critical to emphasize that, in addition to patient safety, intervention difficulties restrict the permissible limits intensity incident on the implanted antenna. The field strength of the proposed antenna is shown in Fig. 7.9.
The gain is high for Polyimide which is 7 dB and next to it Polystyrene which is 6 dB and next is Polytetrafluoroethylene (PTFE) which is 5 dB. The comparison of the same is given in Fig. 7.10 and Table 7.2.
Conclusion
In this work, we attempted to provide a quick summary of the issues encountered and remedies proposed for the development, modeling, and constraints of implanted antennas for biomedical applications. The development of implanted antennas is primarily concerned with miniaturization and nontoxicity, despite the fact that electrically tiny antennas have poor transmission efficacy and generally limited bandwidths. Gain improvement is important since it affects the quality of the results. Patch antennas are fundamentally based on two numerical models: Finite-Element and Finite-Difference Time-Domain Methods. Simplified tissue models have been demonstrated to be capable of replacing sophisticated anatomical tissue models, therefore speeding up simulations. A bio-friendly antenna with dimensions of 27 × 15 × 0.16 mm3 was developed and successfully simulated at various substrates with high gain, return loss, and field pattern at 2.5 GHz.
References
Alzheimer’s Association Report (2011) 2011 Alzheimer’s disease facts and figures. Alzheimer’s Demen J Alzheimer’s Assoc 7:208–244
Bhardwaj V, Joshi R, Gaur AM (2022) IoT-based smart health monitoring system for COVID-19. SN Comput Sci 3:137. https://doi.org/10.1007/s42979-022-01015-1
Bhargava B (2021) Wanted a revolution in healthcare system. The Hindu Businessline
Bodenheimer T, Chen E, Bennett HD (2009) Confronting the growing burden of chronic disease: Can the US health care workforce do the job. Health Aff 28:64–74
Botha M et al (2014) The benefits and challenges of e-health applications: a content analysis of the South African context. In: Conference: the international conference on computer science, computer engineering, and social media (CSCESM2014)
Ferdous MdS, Chowdhury F, Moniruzzaman Md (2007) A taxonomy of attack methods on peer-to-peer network. In: Proceedings of the 1st Indian conference on computational intelligence and information security (ICCIIS, 07)
Garcia-Pardo C, Andreu C, Fornes A, Castello-Palacios S, Perez Simbor S, Barbi M, Vallés-Lluch A, Cardona N (2018) Ultra wideband technology for medical in-body sensor networks: an overview of the human body as a propagation medium, phantoms, and approaches for propagation analysis. IEEE Antennas Propag Mag 1–1. https://doi.org/10.1109/MAP.2018.2818458
Hall PS, Hao Y (2006) Antennas and propagation for body centric communications. In: 2006 first European conference on antennas and propagation
Hayes TO, Gillian S (2020) Chronic disease in the United States: a worsening health and economic crisis. 1–19
https://worldpopulationreview.com/countries/china-population (2022)
https://worldpopulationreview.com/countries/japan-population
Iftekhar EN et al (2021) A look into the future of the COVID-19 pandemic in Europe: an expert consultation. Lancet Reg Health Eur 8:100185
Islam MM, Rahaman A, Islam MR (2020) Development of smart healthcare monitoring system in IoT environment. SN Comput Sci 1(3):185
Islam MM, Rahmanand A, Islam MR (2020) Development of smart healthcare monitoring system in IoT environment. SN ComputSci 1(3)
Jazieh AR, Kozlakidis Z (2020) Healthcare transformation in the post-coronavirus pandemic era. Sec. Infectious diseases—surveillance, prevention and treatment
Kargar MJ, Ghasemi S, Rahimi O (2013) Wireless body area network: from electronic health security perspective. Int J Reliab Qual E-Healthc (IJRQEH) 2(4):38–47
Kavitha S, Gokul Anand KR, Poornima T, Sathiya Girija H (2022) IoT centered household security and person’s health care system predominantly aimed at epidemic circumstances. Internet of things and data mining for modern engineering and healthcare applications. ISBN 9781032108544
Khan MM, Mehnaz S, Shaha A, Nayem M, Bourouis S (2021) IoT-based smart health monitoring system for COVID-19 patients. Comput Math Methods Med
Kumar R, Mukesh R (2013) State of the art: security in wireless body area networks. Int J Comput Sci Eng Technol (IJCSET) 4(05):622–630
Lehnert T, Heider D, Leicht H, Heinrich S, Corrieri S, Luppa M, Heller SR, Konig HH (2011) Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev 68:387–420
Leifer BP (2003) Early diagnosis of Alzheimer’s disease: clinical and economic benefits. J Am Geriatr Soc 51:S281–S288
Levin A, Stevens PE (2011) Early detection of CKD: the benefits, limitations and effects on prognosis. Nat Rev Nephrol 7:446–457
Malik PK, Wadhwa DS, Khinda JS (2020) A survey of device to device and cooperative communication for the future cellular networks. Int J Wirel Inf Netw Springer 27:411–432. https://doi.org/10.1007/s10776-020-00482-8
Momtazmanesh S et al (2020) All together to fight COVID-19. Am J Trop Med Hyg 102(6):1181–1183
National Institute on Aging (NIA) (2016) NIH-funded Census Bureau U.S. nih.gov/news-events/news-releases/worlds-older-population-grows-dramatically
Office of National Statistics (2022) Statistical bulletin national population projections: 2020-based interim. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections
Pahwa R, Lyons KE (2010) Early diagnosis of Parkinson’s disease: recommendations from diagnostic clinical guidelines. Am J Manag Care 16:94–99
Priesemann V et al (2021) Towards a European strategy to address the COVID-19 pandemic. Lancet 398(10303):838–839
Rahim A, Malik PK (2021) Analysis and design of fractal antenna for efficient communication network in vehicular model. Sustain Comput Inform Syst 31:100586. Elsevier. https://doi.org/10.1016/j.suscom.2021.100586. ISSN 2210-5379
Roges R, Malik PK (2021) Planar and printed antennas for internet of things-enabled environment: opportunities and challenges. Int J Commun Syst 34(15):e4940. https://doi.org/10.1002/dac.4940ISSN:1099-1131
Srividya, Satyanarayana V (2018) Personal lung function monitoring system for asthma patients using internet of things (IOT). Int J Res Electron Comput Eng 6
Switzerland. http://www.who.int/nmh/publications/ncd_report_full_en.pdf. Accessed 1 May 2016
Thapliyal H et al (2021) Consumer technology-based solutions for COVID-19. IEEE Consum Electron Mag 10(2):64–65
Tossaint-Schoenmakers R et al (2021) The challenge of integrating eHealth into health care: systematic literature review of the Donabedian model of structure, process, and outcome. J Med Internet Res
U.S. Department of Health and Human Services (2020) Physical activity guidelines for Americans, 2nd edn
World Health Organization, Food and Agriculture Organization of the United Nations (2018) The nutrition challenge: food system solutions. WHO/NMH/NHD/18.10
Yach D, Hawkes C, Gould L, Hofman KJ (2004) The global burden of chronic diseases: overcoming impediments to prevention and control. J Am Med Assoc 291:2616–2622
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Sathiyapriya, T., Rajarajeshwari, K.C., Poornima, T., Agarwal, S. (2023). Design of Compact Low-Profile Antenna for Wearable Medical Applications. In: Malik, P.K., Shastry, P.N. (eds) Internet of Things Enabled Antennas for Biomedical Devices and Systems. Springer Tracts in Electrical and Electronics Engineering. Springer, Singapore. https://doi.org/10.1007/978-981-99-0212-5_7
Download citation
DOI: https://doi.org/10.1007/978-981-99-0212-5_7
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-0211-8
Online ISBN: 978-981-99-0212-5
eBook Packages: EngineeringEngineering (R0)