Abstract
Physical activity is an important lifestyle habit in patients with breast cancer. Engaging in high levels of physical activity can help prevent the development of breast cancer and improve life expectancy after the disease. Physical therapists must help their patients acquire these benefits of physical activity. To do so, it is necessary to understand the evidence of physical activity benefits among patients with breast cancer and the different methods and characteristics of assessing physical activity and how to apply them clinically.
In addition, maintaining physical activity is beneficial for breast cancer treatments, such as surgery, chemotherapy, and hormone therapy. Although its development has greatly prolonged life expectancy, breast cancer treatment leads to various adverse events, such as lymphedema, neuropathy, joint pain, and bone loss. It is now known that physical activity plays an important role in reducing these conditions. In addition, research on exercise therapy for cardiotoxicity caused by molecular targeted drugs and myokines produced by muscles is being conducted; these areas are expected to develop in the future.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Physical activity
- Occupational activity
- Leisure-time activity
- Walking
- Sedentary behavior
- Breast cancer patients
- Prevention
1 Introduction
Physical activity is an important lifestyle habit in patients with breast cancer. Engaging in high levels of physical activity can help prevent the development of breast cancer and improve life expectancy. In addition, it has various benefits, such as the reduction of adverse events during treatment. In this chapter, we introduce the impact of physical activity and outline how it can be applied to clinical practice. Each piece of information is accompanied by a bibliography for those who wish to understand the topic in more detail. In addition to the benefits of existing physical activities, this book also introduces the latest findings in areas that are desirable for future development. It is my hope that this information will be meaningful for physical therapists worldwide.
2 Traditional Physical Therapy Regarding Physical Activity in Patients with Breast Cancer
Breast Cancer Epidemiology. An overview of physical activity-related issues that physical therapists caring for patients with breast cancer should be aware of; clinical applications will also be described.
2.1 The Effect of Physical Activity on Patients with Breast Cancer
Many studies have shown that physical activity affects the risk of breast cancer development, prevention of recurrence, and survival. This section outlines the impact of physical activity on each event and introduces the types of physical activity described in previous studies.
2.1.1 Physical Activity and Breast Cancer Risk
Evidence of the association between physical activity and cancer development has been accumulating since the 1990s. NHANES I showed that the risk of developing cancer is increased in groups with low levels of physical activity compared to those with high levels, and site-specific analyses showed that the risk of developing breast and cervical cancers is more associated with physical activity levels in women [1]. Since then, a number of papers have been published focusing on physical activity and the risk of developing breast cancer. The World Cancer Research Fund (WCRF) and American Institute for Cancer Research (AICR) publication “Diet, nutrition physical activity and breast cancer” contains the latest expert report and recommends engaging in physical activity to prevent the development of breast cancer [2]. Several other reviews and meta-analyses have also been published. In a meta-analysis published in 2013, 31 articles demonstrated that a group with a high level of physical activity had a relative risk (RR) of developing breast cancer of 0.88 (95% confidence interval (CI): 0.85–0.91) compared to a group with a low level of physical activity [3]. This meta-analysis concluded that a high level of physical activity, both occupational and nonoccupational, reduced the RR. In addition, a dose-response analysis showed that every 25 metabolic equivalent (MET)-h/week increase in nonoccupational activity was associated with a 2% reduction in the risk of developing breast cancer, every 10 MET-h/week increase in leisure time activity was associated with a 3% reduction in risk, and every 2 h/week increase in moderate- and high-intensity leisure time activities was associated with a 5% reduction in risk. As shown above, the preventive effect varied depending on the type and intensity of physical activity. According to the WCRF expert report, most physical activities are effective in preventing the risk of developing breast cancer in postmenopausal women, whereas only high-intensity physical activities contribute to the prevention of breast cancer risk in premenopausal women [2]. Thus, it is almost certain that physical activity can reduce the risk of developing breast cancer. However, it is important to note that there are differences in the preventive effect depending on the type and intensity of physical activity, and the appropriate type and intensity of physical activity differ according to menopausal status.
The mechanism by which physical activity affects the risk of breast cancer development remains unclear. It is generally believed that the mechanism by which physical activity suppresses the risk of developing all cancers is that physical activity reduces the number of fat cells, which in turn suppresses the production of endogenous hormones and growth factors for tumor cells. Physical activity improves insulin resistance and decreases fasting insulin and C-peptide levels, which are factors in cancer development [2]. The key to breast cancer-specific mechanisms is female hormones. Women who are obese, postmenopausal, or hormone receptor positive (HR+) have been shown to be more sensitive to physical activity [4, 5]. Based on these findings, female hormones have been identified as a factor associated with the relationship between physical activity and risk of developing breast cancer. Factors that contribute to the development of breast cancer include early menarche, late menopause, and first childbirth after the age of 30 years, all of which increase exposure to the female hormone estrogen [2]. In postmenopausal women, high levels of physical activity have been shown to lower female hormone levels. Future research should be conducted on the mediating factors between physical activity and risk of developing breast cancer.
2.1.2 Physical Activity and Recurrence
According to the Breast Cancer Treatment Guidelines published by the Japanese Breast Cancer Society, physical activity has no effect on breast cancer recurrence. A meta-analysis was conducted separately for two periods, before or at diagnosis and after diagnosis of breast cancer, and physical activity did not reduce the risk of breast cancer recurrence in either period (RR before or at diagnosis: 0.93 (95% CI: 0.60–1.45); RR after diagnosis: 0.81 (95% CI 0.64–1.04)) [6]. However, only three studies were included in each period, and there were differences in subject characteristics due to differences in age, menopause information, and postoperative treatment. In addition, the type and intensity of physical activity have not been sufficiently examined, and evidence is insufficient to conclude that physical activity does not affect breast cancer recurrence.
2.1.3 Physical Activity and Survival
Many studies and review articles have evaluated the relationship between physical activity and breast cancer mortality risk [7, 8]. As a result, physical activity is effective for breast cancer death, and a physical therapist, the director of promoting physical activity among breast cancer patients, should be aware of this. In the WCRF/AICR expert report, physical activity before, at, and after the diagnosis of breast cancer was associated with a reduced risk of all-cause mortality [2]. A meta-analysis of physical activity and risk of breast cancer mortality was also conducted in the Japanese Breast Cancer Treatment Guidelines, which reported an RR of 0.86 (95% CI 0.78–0.95) before or at diagnosis and an RR of 0.77 (95% CI 0.72–0.83) for all-cause mortality. Physical activity after diagnosis led to an RR of 0.57 (95% CI 0.46–0.71) for breast cancer mortality and RR of 0.56 (95% CI 0.46–0.69) for all-cause mortality [6]. It is clear from the results of many studies and meta-analyses that physical activity has a protective effect on the risk of death from breast cancer and all-cause mortality.
2.2 Promoting Physical Activity Among Patients
2.2.1 Promote Physical Activity Before Diagnosis of Breast Cancer
The goal is to reduce the risk of developing breast cancer. The target population is not patients with the disease, but people who have not yet developed breast cancer, that is, residents of the community. Physical therapists, who are mainly in charge of post-disability rehabilitation, may not have many opportunities to intervene directly in this population. In addition, while there are various lifestyle-related diseases such as stroke, heart disease, diabetes, and obesity, it is rare for physical therapists to be involved in preventive approaches, specifically for breast cancer. However, in recent years, there have been an increasing number of opportunities for citizens to think about breast cancer through breast cancer awareness events such as the Pink Ribbon Movement and the promotion of cancer screening [9]. If physical therapists can be involved in such situations, it would be meaningful to promote physical activity among citizens with the aim of reducing the risk of developing breast cancer.
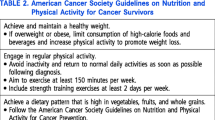
In practice, the main intervention should be to provide information on physical activity that reduces the risk of developing breast cancer through the media and leaflets. The following points should be noted. The assessment of physical activity conducted in previous studies was diverse, and it was difficult to present a uniform amount of physical activity. In addition, the response to the amount of activity changes depends on the presence or absence of factors, such as obesity and menopause. It is advisable to understand the characteristics of the target subject and set the amount of physical activity by referring to studies conducted on similar subjects. The following table presents some guidelines for physical activity (Table 13.1).
All these findings are based on the results of large-scale cohort studies and have a high level of evidence, making them easy to refer to. In addition, the number of times, duration, and intensity of physical activity have been set in concrete terms, making it easy to image. Therefore, it is recommended to refer the abovementioned guidelines for the amount of physical activity needed.
2.2.2 Promoting Physical Activity During and After Breast Cancer Treatment
The goal is to reduce the risk of breast cancer recurrence and improve life expectancy. Current evidence shows that the effect of physical activity on life expectancy is more beneficial than its effect on the risk of recurrence [6]. Therefore, it is appropriate to refer to the physical activity intensity in life prognosis studies when conducting physical therapy. In addition, physical activity during breast cancer treatment has the effect of reducing the adverse events caused by the treatment, and it is also meaningful to perform physical activity to improve these events. The effects of physical activity on adverse events will be discussed in Sect. 13.3.
Physical therapists can provide information about physical activity in patients with breast cancer undergoing rehabilitation during or after surgery, chemotherapy, or radiation therapy. The WCRF/AICR expert report concluded that the impact of physical activity on life expectancy at diagnosis and beyond is beneficial [2]. Some guidelines for physical activity are presented below:
Engage in physical activity more than 10 MET-h/week [12].
-
Moderate intensity exercise for 2.5 h/week or high-intensity exercise for 1.25 h/week
For every 10 MET-h/week increase in physical activity, the RR decreases to 0.8–0.9 [2].
Let us note that whether changes in physical activity levels affect life expectancy. Bertram et al. reported that in a cohort of patients who did not achieve 10 MET-h/week prior to diagnosis, but improved physical activity levels to 10 MET-h/week or more during the first year after diagnosis, subsequent life expectancy did not change compared with the group that did not improve [13]. This article suggests that annual changes in physical activity are not sufficient to reduce the risk of death in patients with breast cancer and that longer exposure to physical activity is needed. We need to pay attention to these points when teaching our patients and provide them with information on how to develop the habit of engaging in physical activity for as long as possible.
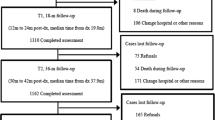
2.3 The Determinants of Physical Activity Among Cancer Patients with Breast Cancer
Promoting physical activity is important for improving life expectancy for patients with breast cancer, and there are many studies around the world that aim to promote physical activity. However, the same approach may result in increased physical activity levels in some individuals but not in others. For an effective approach, it is necessary to understand the determinants of physical activity. A systematic review of exercise adherence in patients with cancer showed that those with a previous exercise habit had better adherence to exercise interventions. However, they found inconsistent results for age, sex, treatment status, physical function, and psychological, social, and environmental factors related to physical activity [14]. Furthermore, few studies have comprehensively analyzed these factors using multivariate analysis, which is a subject for future research. Therefore, we comprehensively evaluated and analyzed these factors to investigate the determinants of habitual physical activity in patients with cancer receiving chemotherapy. Physical activity was assessed using a triaxial accelerometer to measure the number of steps, and potentially determinant variables, such as patient characteristics, medical data about cancer treatment, adverse events according to chemotherapy, physical function (handgrip strength and gait speed), psychological factors (self-efficacy and the decision balance for exercise), social factors (social support scale and lodgers), and environmental factors, were collected. We recruited 37 outpatients receiving chemotherapy. They walked approximately 4200 step counts per day during the treatment. This number was higher than expected. We conducted linear regression analyses and found that positive feelings toward exercise increased habitual physical activity during cancer treatment (Table 13.2) [15]. However, medical data and adverse events, such as fatigue, vomiting, pain, and dyspnea; physical function; social factors; and environmental factors showed no significant association with habitual physical activity. Therefore, we should pay attention to this result. Positive feelings toward exercise is one of the transtheoretical models and a commonly used among community-dwelling elderly people. In recent years, these models have been suggested to be important for patients with cancer [16]. While it is difficult to modify the progression of the disease and the contents of the treatment, as well as its side effects, it is highly possible to change the patient’s own knowledge and motivation for physical activity through our approach. It is important to provide accurate and clear information so that patients can understand the importance of exercise and spontaneously change their behavior.
2.4 Assessment Tools of Physical Activity and Clinical Applications
2.4.1 Assessment of Physical Activity Using Questionnaires
Most large cohort studies have used questionnaires to investigate physical activity [4, 17]. In patients with breast cancer, physical activity has been quantified using METs-h/week and associated with the risk of disease and life expectancy. Although other assessments of activity may be based on subjective judgment of the patient [1], it is more useful to calculate METs-h/week using questionnaires. Each large cohort study used a specific questionnaire: the Japan Public Health Center (JPHC) cohort study used the JPHC prospective study-based physical activity questionnaire (JPHC-PAQ) [18] and the Women’s Healthy Eating and Living (WHEL) study used the Women’s Health Initiative (WHI) [10]. We introduce the JPHC-PAQ to calculate METs-h/day in Fig. 13.1. It is necessary to check each study for specific assessment methods.
2.4.2 Assessment of Physical Activity Using Pedometers and Accelerometers
The questionnaire-based evaluation method was introduced in the previous section. There is a high possibility of recall bias and discrepancy between the actual physical activity and amount of activity in the questionnaire responses. To correct these measurement errors, it is essential to evaluate physical activity using objective indicators. Pedometers and accelerometers are evaluation methods that have been in use for a long time and can objectively assess the amount of physical activity. Particularly for accelerometers, new devices are being developed, which are becoming increasingly accessible to the general public. For some devices, correlation coefficients with actual movements have been calculated [19, 20], and it can be said that they are good tools for accurately assessing physical activity in clinical settings. Recently, the use of smartphones to assess physical activity has been shown to be valid [21].
2.4.3 Clinical Indications
When assessing physical activity among a large group of people, such as in a community-based intervention, a questionnaire-based assessment method such as that introduced in Sect. 13.2.4.1 is appropriate. If one has the opportunity to care for patients in a hospital or clinic-based setting, and they encounter situations that need promoting physical activity in patients, the use of a pedometer or accelerometer is preferable for a more accurate assessment. There are many criteria for using data from an accelerometer [22], such as wearing season, wearing days (including weekend or not), available day (how many hours do they wear the device), and situation (walking time only or all day). The number of seconds required to measure counts varies depending on the type of accelerometer and how the non-wear time is determined varies from study to study (e.g., how long does the zero last). For example, in a study using ActiGraph to assess physical activity, patients were asked to wear the device at the waist on the right side for 21 consecutive days. The non-wear time was defined as 60 consecutive zero counts/min. Sedentary behavior was defined as 0–50 counts/min. Light physical activity was defined as 51–759 counts/min, moderate lifestyle physical activity was defined as 760–1951 counts/min, and moderate- to vigorous-intensity physical activity as ≥1952 counts/min [23]. It is advisable to decide which study to refer to, depending on the method and timing of the study and the accelerometer used. The amount of physical activity calculated using accelerometers is often difficult for patients to interpret. Therefore, it is important to obtain understandable information from the accelerometer, such as step counts/day and the amount of time the patient has been walking. These devices also allow patients to monitor their own activities for easy self-care, as many can check the number of steps taken by looking at device’s monitor.
3 Research Trend for Physical Activity for Patients with Breast Cancer
In this section, we will discuss the research trends in the field of physical activity in patients with breast cancer. As discussed in Sect. 13.2, numerous studies have shown the impact of physical activity on breast cancer incidence and prognosis. With the development of breast cancer treatment, the 5-year survival rate for early stage breast cancer has been improving and the number of breast cancer survivors is increasing [6]. While long-term survival has been achieved through continuous treatment, the number of patients suffering from the side effects of treatment is expected to increase. In recent years, physical activity has been shown to be an effective treatment for these side effects, and we will discuss it, along with our research.
3.1 Lymphedema After Breast Cancer Surgery
Although surgery is one of the major treatments for breast cancer, lymphedema may occur in the upper extremities when the lymph nodes are damaged by axillary lymph node dissection. The incidence of lymphedema is 20%, and the risk factors include axillary lymph node dissection, number of lymph node dissection areas, and mastectomy [24]. Lymphedema can cause pain, heaviness in the arms, limited range of motion and limitation of movement, and decreased quality of life [25]. To prevent lymphedema, surgical treatment and combined physical therapy (such as compression therapy, manual lymphatic drainage, skin care, and exercise therapy) are used, and evidence supporting these is slowly accumulating. These treatments require hospital visits, and it is expected that some patients will not be able to receive the treatments because of the number of facilities, accessibility issues, and financial problems. After surgical treatment, patients are given self-care guidance such as skin care, circumference measurement, and massage. At that time, they should also be provided with guidelines for physical activity. In this subsection, we introduce the effects of physical activity on lymphedema after breast cancer surgery.
Recently, there has been a paradigm shift regarding whether exercise should be administered to patients with lymphedema. In the past, care for lymphedema often involved teaching patients to refrain from the active use of the surgical side of the upper extremity. This tends to lead to a negative cycle of inactivity due to the anxiety of worsening edema, which in turn leads to obesity, a condition that can exacerbate edema. However, it has been shown that resistance training including the surgical side upper extremity is effective in reducing the circumference of the upper limb without worsening edema [26]. Based on the results of these studies, it is now recommended that patients with lymphedema should be actively encouraged to exercise. In addition to these exercise interventions, it is becoming clear that habitual physical activity can also affect lymphedema. Vrieze et al. reported that the lower the level of physical activity, as assessed using the International Physical Activity Questionnaire (IPAQ), the lower the level of lymphedema-related symptoms and life function [27]. Breast cancer patients with lymphedema have been found to have low levels of physical activity [28]; therefore, promoting their activity levels is a necessary issue. In a more practical report, a study investigating risk factors for lymphedema exacerbation showed that postoperative employment and household activities do not lead to lymphedema exacerbation and concluded that there is no need to change the content of work activities before and after surgery [29]. Some studies examined the relationship between physical activity and lymphedema by dividing them into different areas. Although the contribution of physical activity is still unclear due to the small number of studies, the current evidence suggests that it is important to maintain the same level of activity after surgery as before, without becoming inactive.
3.2 Hormone Therapy
3.2.1 Bone-Related Events: Physical Activity
Postoperative hormone therapy is widely used for postmenopausal patients with HR+ breast cancer, and aromatase inhibitors have shown great efficacy in improving overall survival (OS) and disease-free survival (DFS) compared to tamoxifen, a conventional hormone therapy [30]. However, they have also been found to cause skeletal-related events (SRE) such as osteoporosis and fractures as side effects. It has been reported that 5-year administration of Arimidex reduces bone mineral density (BMD) of the lumbar spine and femoral neck by −6% and −7%, respectively [31]. Moreover, fracture events occur in as many as 7% of patients after exemestane treatment [32]. In addition to primary therapies such as bisphosphonates and denosumab, exercise therapy has been regarded as a non-pharmacological treatment [33]. There is scattered evidence of supervised exercise interventions for SRE, and exercise therapy has been recommended in the Joint Position Statement by multiple societies [34]. However, some meta-analyses have shown that exercise has no effect on BMD [35]. Since there are not enough high-quality studies, further accumulation and review of evidence are desirable.
For SRE, the role of habitual physical activity may be more important than that of exercise therapy because hormone therapy lasts for about a year, while exercise interventions last for a month at most, which is much shorter than the duration of therapy. Brooke-Wavell et al. reported that brisk walking can improve bone mineral density for up to 5 years, indicating that the response of bone metabolism to exercise requires a certain period of time. From this perspective, it is important to understand that the response of bone metabolism to exercise requires a certain period of time [36]. It is important to promote habitual physical activity and prevent SRE throughout the treatment period of hormone therapy rather than short-term exercise interventions. However, few studies have examined the relationship between habitual physical activity and SRE. Against this background, we investigated the association between habitual physical activity and bone mineral density, as well as and bone metabolism, in patients with breast cancer receiving postoperative aromatase inhibitor therapy [37]. We found that the level of light physical activity (LPA) and work activities, such as employment and housework, was negatively correlated with the bone metabolism markers P1NP and TRACP-5d. This suggests that even mild physical activity may inhibit the increase in bone metabolism. As patients with breast cancer undergo prolonged treatment, it is difficult for them to engage in high-intensity physical activity and maintain the amount of physical activity; therefore, it is reasonable to conclude that even repetitive walking and occupational activity in daily life can contribute to SRE. However, there are some limitations of the study, such as the fact that it was a cross-sectional study and causality cannot be mentioned, and there was no effect on BMD. It is hoped that more high-quality studies will be conducted in the future.
3.2.2 Joint Pain: Physical Activity
Aromatase inhibitors are widely used in the postoperative period of breast cancer, and SREs have been described in the previous subsection as a side effect. Moreover, aromatase inhibitors induce musculoskeletal symptoms such as joint pain. This is called aromatase inhibitor-induced musculoskeletal symptoms (AIMSS), and it has been reported that arthralgia occurs in as many as 47% of patients and joint stiffness in 44% of patients [38]. It is symmetrically located in the joints of the extremities, and the degree of pain is often severe. It is not caused by joint inflammation, as in orthopedic surgery, but by depletion of the female hormone, estrogen [39]. Therefore, AIMSS occur during hormone therapy. AIMSS not only reduce quality of life but may also cause interruption of hormone therapy [40], affecting the rate of treatment completion. Exercise therapy is important, even for AIMSS. A meta-analysis concluded that exercise therapy can reduce pain and stiffness caused by AIMSS [41]; however, a Cochrane review did not show the effectiveness of exercise [42], and no consensus has been reached. Interventions tend to include high-intensity resistance training and home-based aerobic exercise (>150 min/week), and some studies have reported that interventions increase physical activity levels [33]. At present, no studies have examined the relationship between habitual physical activity and AIMSS, and it is unclear whether physical activity is effective against AIMSS. In contrast, in a cross-sectional study, 60% of patients with AIMSS showed decreased activity after the start of treatment, suggesting a relationship between AIMSS and physical activity [43]. Further studies are needed to confirm this hypothesis.
3.3 Chemotherapy
The use of taxanes, such as paclitaxel, in addition to AC therapy during postoperative chemotherapy improves DFS and OS in patients with breast cancer with positive lymph nodes [44]. Taxanes are plant alkaloids classified as microtubule inhibitors. As such, they can cause peripheral neuropathy. This is known as chemotherapy-induced peripheral neuropathy (CIPN) and includes symptoms such as paresthesia and pain which appear in a symmetrical globe-sock pattern [45]. Taxane-induced peripheral neuropathy (PN) affects the completion rate of chemotherapy in patients with breast cancer. Approximately 17% of patients with breast cancer have their prescription reduced because of taxane-induced PN, particularly paclitaxel [46]. In addition, CIPN has been shown to reduce physical activity and predispose patients to falls [47, 48]. There is no standard treatment for CIPN, and the main approach is to reduce or discontinue drugs that induce PN. Exercise therapy has been shown to contribute to the improvement of balance disorders caused by CIPN, including taxanes. Therefore, exercise therapy may alleviate CIPN symptoms and prevent falls [49]. Exercise includes aerobic exercise and resistance training, which can be performed with self-care. As outpatient chemotherapy has become the mainstream treatment in recent years, it is expected that more research will be conducted to determine whether habitual physical activity and exercise therapy can contribute to the alleviation of CIPN symptoms.
Physical therapists also need to take a preventive perspective on issues such as decreased physical activity and occurrence of falls. With regard to physical inactivity, physical therapists need to understand the risk factors for the development and exacerbation of CIPN, and when working with patients undergoing anticancer therapy, interventions should focus on high-risk patients. Although factors such as age, creatinine clearance, and pack-year have been extracted, the results have been inconsistent across studies [50]. However, in recent years, studies on anemia and CIPN have begun to be published. We also reported that vincristine-induced CIPN, a plant alkaloid system similar to taxanes, was exacerbated by baseline anemia [51]. Similarly, anemia was recently reported to be a risk factor for paclitaxel-induced PN [52]. Therefore, patients with anemia should be carefully monitored for CIPN development and exacerbation. For monitoring, we must assess CIPN, and the evaluation of CIPN is often subjective by medical personnel or is based patient-reported outcomes (PRO). However, these assessments lack an objective. Therefore, we quantitatively assessed CIPN using SWMs (Semmes-Weinstein Monofilament SOT-DM06A, Sakai Med, Tokyo, Japan) and a 128 Hz tuning fork (Luze c128 Hz 01–008, NITI-ON, Chiba, Japan) (Fig. 13.2). We recruited patients with various types of cancers receiving chemotherapy which was inducing peripheral neuropathy. We assessed CIPN at the lower extremity using the SWMs and 128 Hz tuning fork at baseline (first day of treatment regimen in arbitrary course) and follow-up (3 months after baseline). These assessment tools can be used to evaluate the tough detection threshold and vibration sensation, respectively. Both sensations are classified as superficial and are related to balance disorders and falling. We defined patients who had a tough detection threshold, higher than 10 g at any measuring site, or who had no vibration sensation as having an abnormal sensation. The results showed that 37% of the patients had sensory abnormalities associated with fall risk during follow-up [53]. We also found that there was a discrepancy between subjective and quantitative assessments, making it difficult to accurately assess symptoms by interviews alone. To screen for the risk of falls, CIPN should be assessed objectively as well as subjectively. The prevention of physical inactivity and falls is an area in which physical therapists must play a role. Therefore, it is necessary to understand the aggravating factors of CIPN and know how to accurately assess the risk of falling.
3.4 Herceptin for HER2-Positive Molecular Target Drugs
HER2-positive breast cancer accounts for approximately 20% of all breast cancers and has poor prognosis [54]. Recently, trastuzumab, a monoclonal antibody, has been developed. The addition of trastuzumab to anthracycline chemotherapy, which is the standard of care, has led to favorable treatment outcomes [55]. However, cardiotoxicity is a major side effect of trastuzumab. Trastuzumab inhibits the production of HER2 protein by acting on ErbB2, a gene that expresses not only HER2 protein, but also neuglerin, an epidermal growth factor that plays an important role in ventricular formation. Therefore, bilateral heart failure is known to occur in patients treated with trastuzumab [56]. Cardiac decompensation has been reported in 27% of patients treated with anthracycline chemotherapy [57], and 5% of patients treated with trastuzumab give up treatment due to heart failure [58]. For patients with breast cancer, cardiotoxicity is an important side effect that leads to discontinued treatment. The most important risk factor for cardiotoxicity is anthracycline use, and similar risk factors for common cardiac events have been reported, including older age, coronary artery disease, diabetes, hypertension, smoking history, poor cardiac function at baseline, and obesity [56]. Drugs such as ACE inhibitors and B blockers are administered. In recent years, the concept of cardio-oncology has been proposed to address the decline in cardiac function caused by cancer treatments.
Evidence of the effect of exercise therapy on trastuzumab-induced cardiotoxicity has not yet been established. However, regular exercise, smoking cessation, and appropriate dietary habits can reduce the mortality of cardiovascular events; therefore, promoting physical activity could also contribute to the reduction of symptoms due to trastuzumab-induced cardiotoxicity. The ASCO guidelines also emphasize the importance of a healthy lifestyle including physical activity [59]. In addition, the American Heart Association’s Scientific Statement states that cardiac rehabilitation is useful in cardio-oncology and has proposed Cardio-Oncology Rehabilitation (CORE) and presents an algorithm for patients with cancer [60]. Although specific interventions have not yet been developed, cardiac rehabilitation often involves supervised aerobic exercise for at least 40 min, two to three times a week, as in regular cardiac rehabilitation. There is little evidence on the amount of physical activity required; however, considering the contents of cardiac rehabilitation, habitual activity may be useful in reducing the cardiotoxicity of trastuzumab.
4 Further Research
In this section, we will discuss the theme of this chapter and the amount of physical activity in patients with breast cancer. We will also discuss what kind of evidence is expected to further confirm the effects of different levels of physical activity.
4.1 Assessment of Physical Activity
As mentioned in Sect. 13.2, physical activity can be assessed in various ways. The MET is calculated, and LPA, moderate physical activity (MPA), and vigorous physical activity (VPA) are often classified. However, this is insufficient to obtain a more accurate picture of daily physical activity. In recent years, the concept of sedentary behavior, bouts, which indicate the continuity of physical activity; breaks, which indicate the interruption of activity; and domain-specific physical activity, such as leisure activities, transportation, work, and housework; as well as the amount of physical activity have been introduced. The intention is to evaluate the amount of physical activity in greater detail.
Sedentary behavior is defined as “all waking behaviors that consume less than 1.5 METs of energy in the sitting, semi-supine, or supine position [61].” An increase in sedentary behavior results in a high risk of cancer-related death [62]. The key question is how to reduce sedentary behavior, which accounts for approximately 60% of the waking time. The number of papers on this subject has been increasing rapidly in recent years, and it is a field that is attracting much attention. Bouts and breaks have also received attention in recent years. Most conventional studies on the amount of physical activity have assessed the total amount of daily activity. Bouts and breaks, on the other hand, show the continuity and interruption of physical activity and provide clinically important information on how physical activity should be performed. Regarding the amount of physical activity by domain, research has been conducted to provide an indicator of the importance of the amount of physical activity in situations such as leisure activities, transportation, such as commuting to and from work and school, work, and housework.
As described above, there are various concepts or scales regarding the amount of physical activity, apart from intensity and time, and it is becoming possible to grasp physical activity in detail [63].
4.2 Myokine
In recent years, it has become clear that myokines produced from muscles play an important role in the mechanism of regular exercise, which reduces morbidity and improves prognosis in various diseases, including breast cancer. Myokines are hormones expressed, produced, and secreted by skeletal muscles, and are widely known as IL-6 [64]. Evidence for the importance of myokines in patients with breast cancer is beginning to emerge. In vivo studies have shown that oncostatin M and irisin, a type of myokine, inhibit the proliferation of breast cancer cells and induce apoptosis [65, 66]. Although there are no clinical studies so far, it is expected that the impact of these myokines on life expectancy and other outcomes will soon be investigated in clinical studies. We hope that more research on myokines will be conducted in the field of physical therapy. It is necessary to investigate the physical activities that contribute to the production of myokines in detail.
In this section, we described the future perspectives on physical activity in patients with breast cancer. It is important to evaluate physical activity in detail. Myokines can be developed from the in vivo level to the clinical level to show the etiology of physical activity and health outcomes. Through these studies, we will be able to provide evidence-based guidance regarding the amount of activity.
5 Conclusion
This chapter outlines the effects of physical activity on patients with breast cancer. Previous studies have shown that physical activity provides significant benefits to these patients, and physical therapists should take the lead in encouraging the amount of physical activity in patients with breast cancer. We also hope that further research will be conducted on the mechanisms between physical activity and breast cancer development, life expectancy, and the reduction of side effects.
References
Albanes D, Blair A, Taylor PR. Physical activity and risk of cancer in the NHANES I population. Am J Public Health. 1989;79(6):744–50.
World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project. Food, Nutrition, Physical Activity, and the Prevention of Breast Cancer. Diet, nutrition, physical activity, and Breast Cancer Survivors. 2017.
Wu Y, Zhang D, Kang S. Physical activity and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat. 2013;137(3):869–82.
Suzuki R, Iwasaki M, Yamamoto S, Inoue M, Sasazuki S, Sawada N, et al. Leisure-time physical activity and breast cancer risk defined by estrogen and progesterone receptor status—the Japan Public Health Center-based Prospective Study. Prev Med. 2011;52(3–4):227–33.
Enger SM, Ross RK, Paganini-Hill A, Carpenter CL, Bernstein L. Body size, physical activity, and breast cancer hormone receptor status: results from two case-control studies. Cancer Epidemiol Biomark Prev. 2000;9(7):681–7.
Japanese Breast Cancer Society. The Japanese Breast Cancer Society clinical practice guidelines for epidemiology and prevention of breast cancer. 2018 ed. 2018.
Lahart IM, Metsios GS, Nevill AM, Carmichael AR. Physical activity, risk of death and recurrence in breast cancer survivors: a systematic review and meta-analysis of epidemiological studies. Acta Oncol Stockh Swed. 2015;54(5):635–54.
Zhong S, Jiang T, Ma T, Zhang X, Tang J, Chen W, et al. Association between physical activity and mortality in breast cancer: a meta-analysis of cohort studies. Eur J Epidemiol. 2014;29(6):391–404.
Cacciamani GE, Stern MC, Medina LG, Gill K, Sotelo R, Gill IS. Cancer awareness crusades-pink ribbons and growing moustaches. Lancet Oncol. 2019;20(11):1491–2.
McTiernan A, Kooperberg C, White E, Wilcox S, Coates R, Adams-Campbell LL, et al. Recreational physical activity and the risk of breast cancer in postmenopausal women: the Women’s Health Initiative Cohort Study. Obstet Gynecol Surv. 2004;59(3):203–4.
Suzuki S, Kojima M, Tokudome S, Mori M, Sakauchi F, Fujino Y, et al. Effect of physical activity on breast cancer risk: findings of the Japan Collaborative Cohort Study. Cancer Epidemiol Biomark Prev. 2008;17(12):3396–401.
Beasley JM, Kwan ML, Chen WY, Weltzien EK, Kroenke CH, Lu W, et al. Meeting the physical activity guidelines and survival after breast cancer: findings from the after breast cancer pooling project. Breast Cancer Res Treat. 2012;131(2):637–43.
Bertram LAC, Stefanick ML, Saquib N, Natarajan L, Patterson RE, Bardwell W, et al. Physical activity, additional breast cancer events, and mortality among early-stage breast cancer survivors: findings from the WHEL Study. Cancer Causes Control. 2011;22(3):427–35.
Kampshoff CS, Jansen F, van Mechelen W, May AM, Brug J, Chinapaw MJM, et al. Determinants of exercise adherence and maintenance among cancer survivors: a systematic review. Int J Behav Nutr Phys Act. 2014;11:80.
Saito T, Okamura A, Inoue J, Makiura D, Doi H, Yakushijin K, et al. Determinants of physical activity in outpatients with cancer during chemotherapy treatment. Bull Health Sci Kobe. 2018;34:1–11.
Essery R, Geraghty AWA, Kirby S, Yardley L. Predictors of adherence to home-based physical therapies: a systematic review. Disabil Rehabil. 2017;39(6):519–34.
Irwin ML, Smith AW, McTiernan A, Ballard-Barbash R, Cronin K, Gilliland FD, et al. Influence of pre- and postdiagnosis physical activity on mortality in breast cancer survivors: the health, eating, activity, and lifestyle study. J Clin Oncol. 2008;26(24):3958–64.
Inoue M, Yamamoto S, Kurahashi N, Iwasaki M, Sasazuki S, Tsugane S, et al. Daily total physical activity level and total cancer risk in men and women: results from a large-scale population-based cohort study in Japan. Am J Epidemiol. 2008;168(4):391–403.
Floegel TA, Florez-Pregonero A, Hekler EB, Buman MP. Validation of consumer-based hip and wrist activity monitors in older adults with varied ambulatory abilities. J Gerontol A Biol Sci Med Sci. 2017;72(2):229–36.
Crouter SE, Schneider PL, Karabulut M, Bassett DR. Validity of 10 electronic pedometers for measuring steps, distance, and energy cost. Med Sci Sports Exerc. 2003;35(8):1455–60.
Hekler EB, Buman MP, Grieco L, Rosenberger M, Winter SJ, Haskell W, et al. Validation of physical activity tracking via android smartphones compared to ActiGraph accelerometer: laboratory-based and free-living validation studies. JMIR Mhealth Uhealth. 2015;3(2):e36.
Mâsse LC, Fuemmeler BF, Anderson CB, Matthews CE, Trost SG, Catellier DJ, et al. Accelerometer data reduction: a comparison of four reduction algorithms on select outcome variables. Med Sci Sports Exerc. 2005;37(11):S544–54.
Hart TL, Swartz AM, Cashin SE, Strath SJ. How many days of monitoring predict physical activity and sedentary behaviour in older adults? Int J Behav Nutr Phys Act. 2011;8(1):62.
DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14(6):500–15.
Shaitelman SF, Cromwell KD, Rasmussen JC, Stout NL, Armer JM, Lasinski BB, et al. Recent progress in the treatment and prevention of cancer-related lymphedema: lymphedema treatment and prevention. CA Cancer J Clin. 2015;65(1):55–81.
Baumann FT, Reike A, Reimer V, Schumann M, Hallek M, Taaffe DR, et al. Effects of physical exercise on breast cancer-related secondary lymphedema: a systematic review. Breast Cancer Res Treat. 2018;170(1):1–13.
De Vrieze T, Gebruers N, Nevelsteen I, Tjalma WAA, Thomis S, De Groef A, et al. Physical activity level and age contribute to functioning problems in patients with breast cancer-related lymphedema: a multicentre cross-sectional study. Support Care Cancer. 2020;28(12):5717–31.
Yildiz Kabak V, Gursen C, Aytar A, Akbayrak T, Duger T. Physical activity level, exercise behavior, barriers, and preferences of patients with breast cancer–related lymphedema. Support Care Cancer. 2021;29(7):3593–602.
Johansson K, Ingvar C, Albertsson M, Ekdahl C. Factors associated with the development of arm lymphedema following breast cancer treatment: a match pair case-control study. Lymphology. 2002;35(2):59–71.
Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF, et al. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet Lond Engl. 2005;365(9453):60–2.
Eastell R, Adams JE, Coleman RE, Howell A, Hannon RA, Cuzick J, et al. Effect of anastrozole on bone mineral density: 5-year results from the anastrozole, tamoxifen, alone or in combination trial 18233230. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(7):1051–7.
Coleman RE, Banks LM, Girgis SI, Kilburn LS, Vrdoljak E, Fox J, et al. Skeletal effects of exemestane on bone-mineral density, bone biomarkers, and fracture incidence in postmenopausal women with early breast cancer participating in the Intergroup Exemestane Study (IES): a randomised controlled study. Lancet Oncol. 2007;8(2):119–27.
Thomas GA, Cartmel B, Harrigan M, Fiellin M, Capozza S, Zhou Y, et al. The effect of exercise on body composition and bone mineral density in breast cancer survivors taking aromatase inhibitors. Obes Silver Spring Md. 2017;25(2):346–51.
Hadji P, Aapro MS, Body J-J, Gnant M, Brandi ML, Reginster JY, et al. Management of Aromatase Inhibitor-Associated Bone Loss (AIBL) in postmenopausal women with hormone sensitive breast cancer: joint position statement of the IOF, CABS, ECTS, IEG, ESCEO IMS, and SIOG. J Bone Oncol. 2017;7:1–12.
Boing L, Vieira M d CS, Moratelli J, Bergmann A, Guimarães AC d A. Effects of exercise on physical outcomes of breast cancer survivors receiving hormone therapy—a systematic review and meta-analysis. Maturitas. 2020;141:71–81.
Brooke-Wavell K, Jones PR, Hardman AE, Null T, Yamada Y. Commencing, continuing and stopping brisk walking: effects on bone mineral density, quantitative ultrasound of bone and markers of bone metabolism in postmenopausal women. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2001;12(7):581–7.
Saito T, Ono R, Kono S, Asano M, Fukuta A, Tanaka Y, et al. Physical activity among patients with breast cancer receiving aromatase inhibitors is associated with bone health: a cross-sectional observational study. Breast Cancer Res Treat. 2020;182(1):187–93.
Crew KD, Greenlee H, Capodice J, Raptis G, Brafman L, Fuentes D, et al. Prevalence of joint symptoms in postmenopausal women taking aromatase inhibitors for early-stage breast cancer. J Clin Oncol. 2007;25(25):3877–83.
Mao JJ, Stricker C, Bruner D, Xie S, Bowman MA, Farrar JT, et al. Patterns and risk factors associated with aromatase inhibitor-related arthralgia among breast cancer survivors. Cancer. 2009;115(16):3631–9.
Chim K, Xie SX, Stricker CT, Li QS, Gross R, Farrar JT, et al. Joint pain severity predicts premature discontinuation of aromatase inhibitors in breast cancer survivors. BMC Cancer. 2013;13(1):401.
Lu G, Zheng J, Zhang L. The effect of exercise on aromatase inhibitor-induced musculoskeletal symptoms in breast cancer survivors: a systematic review and meta-analysis. Support Care Cancer. 2020;28(4):1587–96.
Roberts KE, Rickett K, Feng S, Vagenas D, Woodward NE. Exercise therapies for preventing or treating aromatase inhibitor-induced musculoskeletal symptoms in early breast cancer. Cochrane Breast Cancer Group, editor. Cochrane Database Syst Rev. 2020. https://doi.wiley.com/10.1002/14651858.CD012988.pub2.
Brown JC, Mao JJ, Stricker C, Hwang W-T, Tan K-S, Schmitz KH. Aromatase inhibitor associated musculoskeletal symptoms are associated with reduced physical activity among breast cancer survivors. Breast J. 2014;20(1):22–8.
De Laurentiis M, Cancello G, D’Agostino D, Giuliano M, Giordano A, Montagna E, et al. Taxane-based combinations as adjuvant chemotherapy of early breast cancer: a meta-analysis of randomized trials. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(1):44–53.
Dougherty PM, Cata JP, Cordella JV, Burton A, Weng H-R. Taxol-induced sensory disturbance is characterized by preferential impairment of myelinated fiber function in cancer patients. Pain. 2004;109(1):132–42.
Bhatnagar B, Gilmore S, Goloubeva O, Pelser C, Medeiros M, Chumsri S, et al. Chemotherapy dose reduction due to chemotherapy induced peripheral neuropathy in breast cancer patients receiving chemotherapy in the neoadjuvant or adjuvant settings: a single-center experience. Springerplus. 2014;3:366.
Mols F, Beijers AJM, Vreugdenhil G, Verhulst A, Schep G, Husson O. Chemotherapy-induced peripheral neuropathy, physical activity and health-related quality of life among colorectal cancer survivors from the PROFILES registry. J Cancer Surviv. 2015;9(3):512–22.
Kolb NA, Smith AG, Singleton JR, Beck SL, Stoddard GJ, Brown S, et al. The association of chemotherapy-induced peripheral neuropathy symptoms and the risk of falling. JAMA Neurol. 2016;73(7):860.
Kanzawa-Lee GA, Larson JL, Resnicow K, Smith EML. Exercise effects on chemotherapy-induced peripheral neuropathy: a comprehensive integrative review. Cancer Nurs. 2020;43(3):E172–85.
Seretny M, Currie GL, Sena ES, Ramnarine S, Grant R, MacLeod MR, et al. Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: a systematic review and meta-analysis. Pain. 2014;155(12):2461–70.
Saito T, Okamura A, Inoue J, Makiura D, Doi H, Yakushijin K, et al. Anemia is a novel predictive factor for the onset of severe chemotherapy-induced peripheral neuropathy in lymphoma patients receiving rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone therapy. Oncol Res. 2019;27(4):469–74.
Mizrahi D, Park SB, Li T, Timmins HC, Trinh T, Au K, et al. Hemoglobin, body mass index, and age as risk factors for paclitaxel- and oxaliplatin-induced peripheral neuropathy. JAMA Netw Open. 2021;4(2):e2036695.
Saito T, Makiura D, Inoue J, Doi H, Yakushijin K, Okamura A, et al. Comparison between quantitative and subjective assessments of chemotherapy-induced peripheral neuropathy in cancer patients: a prospective cohort study. Phys Ther Res. 2020;23(2):166–71.
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235(4785):177–82.
Katzorke N, Rack BK, Haeberle L, Neugebauer JK, Melcher CA, Hagenbeck C, et al. Prognostic value of HER2 on breast cancer survival. J Clin Oncol. 2013;31(15_suppl):640.
Dempsey N, Rosenthal A, Dabas N, Kropotova Y, Lippman M, Bishopric NH. Trastuzumab-induced cardiotoxicity: a review of clinical risk factors, pharmacologic prevention, and cardiotoxicity of other HER2-directed therapies. Breast Cancer Res Treat. 2021;188(1):21–36.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92.
Perez EA, Romond EH, Suman VJ, Jeong J-H, Sledge G, Geyer CE, et al. Trastuzumab plus adjuvant chemotherapy for human epidermal growth factor receptor 2-positive breast cancer: planned joint analysis of overall survival from NSABP B-31 and NCCTG N9831. J Clin Oncol Off J Am Soc Clin Oncol. 2014;32(33):3744–52.
Cardinale D, Colombo A, Torrisi R, Sandri MT, Civelli M, Salvatici M, et al. Trastuzumab-induced cardiotoxicity: clinical and prognostic implications of troponin I evaluation. J Clin Oncol Off J Am Soc Clin Oncol. 2010;28(25):3910–6.
Gilchrist SC, Barac A, Ades PA, Alfano CM, Franklin BA, Jones LW, et al. Cardio-oncology rehabilitation to manage cardiovascular outcomes in cancer patients and survivors: a scientific statement from the American Heart Association. Circulation. 2019;139(21). https://www.ahajournals.org/doi/10.1161/CIR.0000000000000679.
Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary Behavior Research Network (SBRN)—terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):75.
Stamatakis E, Chau JY, Pedisic Z, Bauman A, Macniven R, Coombs N, et al. Are sitting occupations associated with increased all-cause, cancer, and cardiovascular disease mortality risk? A pooled analysis of seven British population cohorts. PLoS One. 2013;8(9):e73753.
Zeiher J, Duch M, Kroll LE, Mensink GBM, Finger JD, Keil T. Domain-specific physical activity patterns and cardiorespiratory fitness among the working population: findings from the cross-sectional German Health Interview and Examination Survey. BMJ Open. 2020;10(4):e034610.
Pedersen BK, Akerström TCA, Nielsen AR, Fischer CP. Role of myokines in exercise and metabolism. J Appl Physiol Bethesda Md 1985. 2007;103(3):1093–98.
Hojman P, Dethlefsen C, Brandt C, Hansen J, Pedersen L, Pedersen BK. Exercise-induced muscle-derived cytokines inhibit mammary cancer cell growth. Am J Physiol Endocrinol Metab. 2011;301(3):E504–10.
Gannon NP, Vaughan RA, Garcia-Smith R, Bisoffi M, Trujillo KA. Effects of the exercise-inducible myokine irisin on malignant and non-malignant breast epithelial cell behavior in vitro. Int J Cancer. 2015;136(4):E197–202.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Saito, T., Ono, R. (2022). Physical Activity in Patients with Breast Cancer. In: Morishita, S., Inoue, J., Nakano, J. (eds) Physical Therapy and Research in Patients with Cancer. Springer, Singapore. https://doi.org/10.1007/978-981-19-6710-8_13
Download citation
DOI: https://doi.org/10.1007/978-981-19-6710-8_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-6709-2
Online ISBN: 978-981-19-6710-8
eBook Packages: MedicineMedicine (R0)