Abstract
With the advent of Videolaryngoscopes and wider availability of Fiberoptic bronchoscopes, some of the unconventional techniques of endotracheal intubation are not very popular in modern anaesthesia. yet, these can be useful techniques in the resource limited settings and with personnel trained in these techniques. Retrograde intubation and blind nasal intubation described in this chapter could prove useful to anesthesiologists or other clinicians when conventional techniques are not feasible or fail. They are characterized by relative simplicity, less dependence on expensive airway devices, minimal patient discomfort, and low incidence of complications.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
-
1.
Unconventional techniques are not included in routine teaching or curriculum but can be lifesaving in certain situations.
-
2.
Retrograde intubation technique is one of them and has been used both as a rescue and elective technique.
-
3.
Cricothyroid membrane identification and puncture, the basic prerequisite for front of neck access, is also applicable to retrograde intubation technique.
-
4.
Unlike cricothyroidotomy, in retrograde intubation, the guidewire is passed cephalad following cricothyroid puncture.
-
5.
Use of flexible endoscope and ultrasound guidance further improves the success and enhances safety.
-
6.
Blind nasal intubation can also be useful in limited clinical situations when resources are limited, or other techniques fail.
-
7.
Continuous monitoring of end tidal carbon dioxide concentration and curve is helpful during blind nasal intubation.
-
8.
Digital intubation technique is rarely performed in modern airway management practice.
1 Introduction
Retrograde intubation and blind nasal intubation described in this chapter could prove useful to anesthesiologists or other clinicians when conventional techniques are not feasible or fail. They are characterized by relative simplicity, less dependence on expensive airway devices, minimal patient discomfort, and low incidence of complications.
2 Retrograde Intubation
Restricted mouth opening severely limits the options for airway management, both in terms of devices and techniques [1, 2]. Worse, failure rate of the chosen technique is also likely to be high. Direct and video laryngoscopy, lighted stylets, or optical stylets are not useful and flexible video endoscopy, though is the best option, may not always be available. Blind nasal intubation has the drawback of requiring multiple airways attempts and high failure rates. Cricothyroidotomy is reserved for “cannot intubate cannot oxygenate” situations. Upfront tracheostomy being more invasive is inherent with its complications such as stenosis, surgical emphysema, and tracheomalacia. Of all these options, retrograde intubation is a technically feasible minimally invasive airway access even in resource limited setup [3]. Though retrograde intubation has been around since the 1960s, it has unfortunately not gained widespread acceptance as a definitive airway access tool despite its successful transformation with modifications in its technique, to stay relevant in the present optic-video-fibreless era [4,5,6,7].
2.1 Historical Perspective
Described first by Butler and Cirillo in 1960, retrograde intubation was used as an alternative to tracheostomy in facilitating unhindered operating field exposure during laryngectomy utilizing a 16F catheter passed as a guide through the tracheostomy site retrieved by oral end which was sutured to an endotracheal tube [4]. Waters in 1963 described retrograde plastic tubing guided through cricothyroid membrane accessed by a Tuohy needle in patients with deformities of jaw secondary to cancrum oris [5].
Powell (1967) reported retrograde intubation as a case series in pediatric difficult airway. Manchester (1972) described emergency pediatric retrograde intubation in children with Pierre-Robin syndrome. Raza (1978) described retrograde intubation as an emergency airway rescue when multiple attempts at direct laryngoscopy had failed. Retrograde intubation was utilized by Pagne (1980) in retropharyngeal abscess, Barland (1981) in micrognathia, Heslet (1985) in epiglottitis, Luhrs (1987) in oral myxoma and in various difficult airway scenarios wherein conventional intubation methods had failed [8, 9].
Despite the initial numerous scientific publications and its inception as an important alternative in ASA difficult airway algorithm, RI did not gain popularity and is often considered outdated, thanks to the advent of advanced and sophisticated airway tools such as videolaryngoscopes and flexible endoscopes [2, 10, 11]. Yet, retrograde intubation finds its definitive place even in the modern airway era in resource limited setups catering to rescue airway challenges in distorted airway anatomy; blood and secretion filled airway and traumatic cervical spine injuries wherein conventional techniques would be impossible or fail or preclude despite the wide array of difficult airway armamentarium in the form of fiberoptic scope, fibreless endoscopes, and video laryngoscopes at disposal [12, 13]. Also being less invasive than the surgical front of neck access techniques, its relevance has been even more justified [14, 15].
Although having a first attempt success rate of 67% across case reports and 69% success rates in cadaver studies, modifications in retrograde techniques have attributed to its success transformation beyond 89–95% in few studies utilizing commercial retrograde intubation kits [16,17,18,19,20,21]. Recently, the combination of the retrograde intubation set used along with ante-grade fiberoptic bronchoscope as guide from above and the addition of ultrasound guidance have rejuvenated interest in the fading art of retrograde intubation [22,23,24,25].
2.2 Definition and Types
Retrograde intubation is minimally invasive, trans-laryngeal guided airway access to facilitate anterograde oro-tracheal or naso-tracheal intubation. It can be performed as an elective technique or when other methods of securing the airway have failed or contraindicated in a given clinical situation. Patients can be awake, sedated or anesthetized, and spontaneously breathing. The technique is employed in both anticipated as well as unanticipated difficult airway scenario [1,2,3].
Multiple techniques of RI have been described and used in different clinical conditions. They vary from blindly performed classical technique to various modifications and combined hybrid techniques. In hybrid techniques, RI is combined with other airway techniques such as flexible endoscopy, video laryngoscopy, and ultrasound.
2.3 Principle
Percutaneous needle puncture of the cricothyroid or cricotracheal membrane is followed by the placement of a retrograde guide (e.g., guidewire) into the nasal or oral cavity traversing the pharynx [2]. Rail roading of endotracheal tube is then carried out either alone or by utilizing an anterograde guide (e.g., airway exchange catheter or antegrade guide catheter available in commercial set) superimposed upon the already secure retrograde guide and directing the endotracheal tube into the larynx either blind or with guidance.
2.4 Advantages of Retrograde Intubation Over Other Intubation Techniques (Table 22.1)
There exist a few clinical scenarios in which retrograde intubation has distinct advantage over the other available intubation techniques especially when the airway is soiled with blood and secretions; in an already complex distorted airway anatomy; limited mouth opening and cervical spine instability [25, 26].
2.5 Indications and Contraindications
Indications include clinical conditions wherein other airway techniques are not suitable or successful. They include (a) limited mouth opening: Oral submucous fibrosis, temporo-mandibular joint ankylosis, maxillo-facial trauma, mandibular trauma, infections in head and neck region [16, 27, 28], (b) upper airway bleed as in potentially hemorrhagic laryngeal and peri-glottic tumors, vascular neck mass, localized trauma, and distorted anatomy in the neck [15, 17, 25, 29], (c) Limited neck movement: Critical cervical spine injuries, ankylosing spondylitis [16, 17, 25], (d) congenital anomalies: Micrognathia, microstomia [2], (e) acquired conditions: Morbid obesity, short neck, obstructive sleep apnea, burns, large airway mass, subglottic stenosis [2], and (f) failed intubation in trauma: Inability to secure airway with conventional direct laryngoscopy, video-laryngoscopy, and fiberoptic devices [13].
Contraindications include (a) unfavorable anatomy in the region of cricothyroid and front of neck: Non-palpable neck landmarks, non-identified cricothyroid membrane, anterior neck mass, large thyroid mass, pre-tracheal mass, and upper airway tumors [3], (b) tumors in the path of access to larynx: Airway polyps, large laryngeal tumors, fragmented airway tumors, and presence of associated laryngo-tracheal stenosis due to tumor spread [3, 29], (c) severe flexion deformity of neck [3, 29, 30], (d) coagulopathy, local soft tissue infection, retropharyngeal abscess [3, 30], and (e) inability to open mouth for guidewire retrieval [9].
2.6 Equipment and Preparation
Minimum sedation to ensure a cooperative and calm patient can be used, in the absence of contraindications, using low dose ketamine (0.5 mg/kg) and/or dexmedetomidine bolus (1 μg/kg) followed by an infusion of 0.5 μg/kg/h. The required equipment and preparation for retrograde intubation are listed in Table 22.2
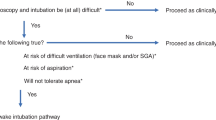
2.7 Classic Technique and Modifications (Fig. 22.1)
-
Step 1: Identification of Cricothyroid to cricotracheal membrane and puncture
-
Puncture is performed using intravenous cannula (16G), or Tuohy needle (16G), with the bevel facing cephalad at 45° angulation, after infiltration of puncture site with 2% lignocaine. Inferior margin of cricothyroid membrane or superior margin of cricotracheal membrane juxtaposed to the cricoid cartilage is the site of entry.
-
The advantage of cricothyroid puncture is the easy identification of the cricothyroid membrane landmark by palpation (laryngeal handshake). One of the reasons for inability to identify cricothyroid membrane is improper position. A sniffing position with extension of the neck will help in identifying the membrane. In obese patients with unidentified landmark, distorted neck anatomy, and anterior neck mass ultrasound guidance would be advantageous for identification of the membrane.
-
Confirmation of needle entry into the trachea can be reassured by continuous aspiration of air bubbles into the saline filled syringe, attached to the cannula or catheter used for puncture. Blind needle puncture should be gentle and controlled to avoid injury to posterior tracheal wall, esophagus, and larynx. Use of ultrasound helps to distinguish between the structures and guide the entry of needle into the trachea, especially in patients in whom identification of puncture site is difficult.
-
Step 2: Insertion of the retrograde guidewire
-
Once the position of the needle is confirmed in the trachea, a guidewire is inserted in the cephalad direction. While inserting the guidewire, patients are often instructed to take deep breaths to achieve abduction of the vocal cords, for smooth passage of the guidewire through larynx. A soft tipped or a J tipped guidewire can be used to reduce the injury to the vocal cords. Various types of guidewires used are vinyl plastic tubing, epidural catheters, vascular catheter guides, angiography catheters, J tipped PTEF coated guidewires, ureteric stents and flexible guidewire provided with nasojejunal feeding tube, guidewire from the Minitrach set, and designated J tipped guidewire from Cook retrograde intubation commercial set.
-
A very rigid or a sharp tip guidewire can lead to injury to vocal cords and pharyngeal mucosa. There may be difficulty in retrieving the guidewire through the oral cavity if it is too soft. Double guidewires have been utilized by some authors to improve the success rate by feeding the wire into the endotracheal tube lumen as well as the side port (Murphy’s eye) simultaneously either by an inside-out or outside-in technique.
-
Step 3: Retrieval of the retrograde guidewire
-
The guidewire inserted is retrieved either nasal or orally. Oral retrieval may be facilitated by finger, forceps, Magill forceps which need at least minimal mouth opening for manipulation (and hence fail in complete trismus). If nasotracheal intubation is required, the guidewire retrieved from the oral cavity needs to be re-directed nasally. A suitable gastric tube is inserted into the patient’s nose and lifted from their pharynx either digitally or by Magill’s forceps, so the tip now exits from the mouth. The guidewire is threaded into the tip of the gastric tube, re-directing the guidewire from mouth to nose, at which time the gastric tube can be removed from the patient. In situations where the length of the guidewire is less, the guidewire can be tied to the suction catheter taken out from oral cavity and then pulled through the nose.
-
Flexible J tipped guidewires have a higher nasal retrieval by design to traverse along the posterior pharyngeal wall. Rarely the guidewire may coil in the pharynx needing assistance for retrieval either by pharyngeal loop or by suction retrieval. The entry point of guidewire is grasped firmly at the entry site using a hemostat or arterial clamp or needle holder. This will not only help in avoiding displacement of the guide wire from the entry site, also will help in to make guide wire taut during advancement of the endotracheal tube.
-
Step 4: Introducing the endotracheal tube
-
The retrieved guidewire from mouth or nose is threaded retrograde into the endotracheal tube, through the Murphy’s eye (providing additional safety while passing the ETT due to the extra length of the tube beyond the glottis). It also avoids the entrapment of the guidewire during removal. Next, the ETT is advanced in antegrade direction gradually while holding the guidewire taught at its proximal end to prevent kinking and to reduce the chances of tube passing into the esophagus TT. During railroading, the endotracheal tube can hitch on to the anterior commissure, epiglottis or vallecula. Corrective maneuvers include 90° anticlockwise rotation of the tube and loosening of the guidewire so that the bevel of the tube slides over the arytenoids. If still not possible, the ETT can be inserted under the guidance of Fiberoptic bronchoscope.
-
Success is indicated by capnography, movement of air across the tube with patients breathing confirming the final position. The successful placement of the endotracheal tube can be confirmed by gush of air while patient breaths, ETCO2 waveform, and tenting of the ETT at the needle entry site.
-
Antegrade guide advancement: If the passing of tube over the guidewire is difficult due to the wide gap between the internal diameter and guidewire, an additional anterograde guide can be passed over the guidewire over which the tube can be railroaded. Various anterograde guides have been utilized and include AEC, flexible endoscope or the custom made anterograde supplied with commercial kits.
-
Step 4: Retrieval of the guidewire
-
Once the position of the tube is confirmed, the clamp applied to the guidewire at the cricothyroid membrane is released and the guidewire can be retrieved either orally or nasally.
Steps of Retrograde intubation. (1) Patient position—neck extended with bolsters placed under shoulder. (2) Puncture of Cricothyroid membrane using 16G intravenous cannula. (3) Confirmation of the cricothyroid membrane by aspiration of air through waterfilled syringe. (4) Insertion of the guidewire in cephalad direction (note different types of guidewire in subpictures). (5) Guidewire is extracted from the nose. Note the end of guidewires. The guidewire in the neck is secured using needle holder (subpicture). (6) Guidewire is passed through Murphy’s eye of endotracheal tube (ETT). (7) The guidewire is taken ouT of circuit end of ETT. Note the straight ETCO2 connector. (8) The ETT is advanced over taut guidewires. The appearance of ETCO2 confirms the correct positioning of the ETT
2.8 Modified Technique Using Commercial Retrograde Intubation Set
Retrograde intubation performed using commercially available kits are user-friendly avoiding assembly of individual components. This saves time during emergency. The Retrograde intubation set is intended to assist in intubation during difficult or emergency airway access procedures in adult and pediatric patients. Cook ™ retrograde intubation set is a commercially available pre-assembled equipment kit to enhance performance with the following readily available components to save time in an emergency:
-
1.
18G introducer needle with needle catheter sheath made of PTFE (polytetrafluorethylene).
-
2.
Flexible J tip guidewire 70 cm long 0.97 mm diameter with graded markings and 11F/14F catheter stylet indexed to guidewire. Total wire guide length is 110 cm. (11F accommodate 4 mm ID and 14F accommodate 5 mm ID endotracheal tubes, respectively.)
-
3.
Tapered tip radio opaque antegrade hollow guide catheter with side ports.
-
4.
Hemostat to stabilize guidewire catheter.
-
5.
Rapi-Fit adapters (15 mm and luer lock connectors) to attach with external oxygen source.
The pediatric retrograde intubation set has 50 cm long 0.97 mm diameter guidewire with 6F catheter stylet accommodating 2.5 mm ID endotracheal tube.
Steps in Using Cook Retrograde Intubation Set
-
1.
Cricothyroid puncture by 18G introducer needle followed by advancement of introducer needle sheath and removal of needle.
-
2.
Confirmation of correct entry by aspiration of continuous air bubbles into the saline filled syringe.
-
3.
Disconnecting the syringe, flexible J tip guidewire is advanced cephalad at 45° angle.
-
4.
The black proximal positioning mark on the guidewire should be visible at the skin access site, to be held by hemostat, ensuring enough length of the guidewire has entered the pharynx.
-
5.
The guidewire is retrieved either by nose or mouth with finger or forceps.
-
6.
The tapered radio opaque guiding catheter is advanced anterograde over the wire, by way of the mouth or nose into the trachea. Advancement of antegrade guide results in tenting at the cricothyroid access site which would be the endpoint of advancement.
-
7.
The endotracheal tube is then railroaded over the wire and guiding catheter into position below the level of the vocal cords.
-
8.
The hemostat unclamped along with the guidewire and antegrade guiding catheter removed from above after securing the endotracheal tube which is advanced to final position.
-
9.
Endotracheal tube cuff inflated and confirmation of tube placement by capnography and auscultation (Ultrasound guidance would be described as a modification) [3, 31].
2.9 Ultrasound Guided Technique
The use of ultrasound for RI has enhanced the safety and success of the technique by providing a real-time guidance in the identification of the structures, point of entry for needle puncture, identification of vessels near the puncture site, and improving the accuracy of airway blocks. Use of ultrasound converts the RI from blind to a guided one [32]. Ultrasound is recommended in time critical cannulation needed for airway management of potentially hemorrhagic laryngeal tumors and distorted airway with unidentifiable neck anatomy [22, 25, 33, 34].
2.10 Fiberoptic Bronchoscope Aided Retrograde Intubation
Two different methods for fiberoptic guided retrograde intubation have been described. In the first technique, the retrograde guidewire is retrieved through the suction port of working channel of flexible endoscope preloaded with endotracheal tube. Alternately, the flexible endoscope can be passed down parallel alongside the retrograde guidewire under vision until railroaded intubation has been achieved [35,36,37,38].
Retrograde and fiberoptic intubation techniques are recommended for patients with difficult airway in patients with laryngeal cancer as sole independent techniques. Retrograde passage of a guidewire through the cricothyroid membrane to guide an antegrade fiberoptic bronchoscope would result in advantageous synergism. Intubation becomes easy over a road map provided by the retrograde guidewire and fiberscope would provide direct visual control of intubation. The fiberoptic bronchoscope also doubles up as a lighted stylet from transillumination on front of neck guiding endotracheal tube advancement. Blind passage of fiberoptic bronchoscope without a retrograde roadmap could lead to trauma, laryngospasm, bleeding, and further worsening of an already compromised airway. The combined method, which can be considered as a hybrid technique, has been extremely successful in patients with obstructive laryngeal tumors [24, 39,40,41,42,43,44]. Failed fiberoptic intubation despite multiple attempts in an airway bleed scenario with anatomical distortion has been secured by retrograde intubation used in combination with ultrasound guidance and passing an antegrade guide in the form of Cook airway exchange catheter for added stability [32].
2.11 Videolaryngoscope Assisted Retrograde Intubation
Most indications for retrograde intubation arise from a limited mouth opening. Videolaryngoscope assisted retrograde intubation has been described sparsely in literature probably owing to the wider mouth opening required to position the blade, where in a retrograde guidewire technique may not be considered. However, in complex airway scenarios of concomitant supraglottic and subglottic narrowing, innovative and out of the box thinking is required where in hybrid techniques combining different airway intubation assist devices and techniques would be beneficial. RI, with other difficult airway techniques may be potentially lifesaving for patients in whom surgical cricothyroidotomy would be primarily undesirable or difficult to perform in the presence of granulomatous vascular neck mass. Successful combination of retrograde intubation with videolaryngoscope (e.g., Glidescope) after a failed fiberoptic intubation attempt has been described. Awake upright fiberoptic intubation and subsequent percutaneous cricothyrotomy were both unsuccessful secondary to obstructive neck mass and retrograde intubation had to be performed with video laryngoscope assistance to deploy a smaller diameter endotracheal tube. The advantage of using video laryngoscope to assist retrograde intubation would be to directly visualize the endotracheal tube entering the laryngeal inlet as well as manipulation of the anterior oropharyngeal structures impeding it otherwise [15].
2.12 Retrograde Intubation with Light Guidance
Light guided trans-illumination from anterior neck has been utilized to guide endotracheal tube into the glottis during retrograde intubation from a light wand or trach light in patients with cervical spine instability. After the retrograde guidewire retrieval by nose or mouth, the light wand mounted on an endotracheal tube has been advanced utilizing the wand as an antegrade guide. The bright glow on the anterior neck has been used as a guide for further advancement of the lighted stylet mounted endotracheal tube under vision improving the success of the technique [9].
2.13 Supraglottic Airway Device Assisted Retrograde Intubation
The initial description reported a modification of retrograde intubation wherein the retrograde guidewire was retrieved through an already positioned laryngeal mask airway. Subsequently, an anterograde guide catheter was advanced over an orally retrieved retrograde guidewire and endotracheal tube railroaded after removal of laryngeal mask retaining the guides [45]. Failed airway management after rapid sequence induction in emergency room led to a combination of intubating laryngeal mask airway (ILMA) used as a ventilating device and retrograde guidewire assisted intubation for procuring definitive airway. Failure of blind passage of endotracheal tube due to repeated resistance led to the retrograde guidewire assistance [46].
Laryngeal mask airway inserted as a rescue airway device after initial failure of conventional intubation with direct laryngoscope has been retained to accommodate a retrograde guide from cook retrograde intubation set and an antegrade fiberoptic bronchoscope advanced to guide intubation in order to obtain a definitive airway for the surgical procedure and replacing the laryngeal mask airway over an exchange stylet [31]. Retrograde intubation has been reported utilizing laryngeal mask airway in syndromic pediatric airway. This method could enable maintaining ventilation until the laryngeal mask gets replaced with an endotracheal tube [47].
2.14 Complications of RI
Generally considered safe in experienced hands, several major and minor complications have been reported in the literature [2, 3, 8, 13, 16, 17, 19, 28, 48,49,50,51,52,53,54,55,56,57]. Cough, sore throat, nose pain, and pain near the needle puncture site are among the reported minor complications. In addition, soft tissue infection, laryngospasm, and bronchospasm have been reported. Lastly, major complications include injury to larynx, posterior tracheal wall, esophagus, hemorrhage during the procedure (from tumor, aberrant vessels, or epistaxis), subcutaneous emphysema, pneumomediastinum, ethmoidal perforation with CSF leak due to guidewire coiling, caudal migration of guidewire, and hypoxemia. Failure to stablish a definitive airway and increased procedural time are technique related drawbacks.
Steps to minimize the complications include the a) use of inferior margin of cricothyroid or superior margin of cricotracheal membrane, use of antegrade guide sheath or AEC over guidewire, and use of hybrid techniques and retrieving the guidewire proximally instead of from the insertion site.
2.15 Pit Falls and Best Practices (Lessons from Past to Present)
Failed retrograde intubation with the use of traditional blind technique, attributed to the narrow confluence of the vestibular folds, laryngeal sinus, and vocal cords, has paved way to modifications of the technique, resulting in improved safety and success (Fig. 22.2). Earlier descriptions of retrograde intubation suggest that the equipment readily available (Tuohy needle, epidural catheter, indigenous guide wire) were often used. Lack of rigidity of the thin guidewire and non-versatility prevented maneuvering. Epidural needles and vascular needles had higher rates of posterior tracheal wall puncture which paved way for sheathed introducer needles [58,59,60].
As part of efforts to modify the classical technique, several guides were tried which included epidural catheters and central venous catheter guidewires among others described previously. An epidural catheter passed through a 16-G Touhy needle with the antegrade addition of a plastic sheath, over the catheter was described first by Waters and has been widely in use historically ever since [2, 5, 21, 60,61,62,63,64]. Similarly, epidural catheter also did not get much popular due to high failure rates. A significant step forward came with the introduction of commercial purpose made kit, increasing the success as well as safety. The J-tipped guidewire used is 70 cm long, kink-resistant and can be kept either lax or torque to facilitate easy navigation in the narrowest available path with least resistance [44, 65, 66]. Recent introduction of the guided techniques like FOB and USG assistance have not only improved the success rate, but also the safety of the procedure [2, 3, 19, 28, 29, 67,68,69,70,71,72].
2.16 Troubleshooting During Retrograde Intubation
Most of the issues related to the techniques have been addressed in detail previously. Following are the few additional concerns in occasional patients.
2.16.1 The Guidewire Is not Going in and not Emerging Inside Oral Cavity?
Guidewire should be directed cephalad at an angulation of 45° to the skin puncture. It may either enter distally into the trachea or become coiled in the pharynx. Hence, it is advisable to take deep breaths to make abduction of the vocal cords, thus facilitation retrograde movement of guidewire. Coiled pharyngeal guidewire may need assistance for retrieval either by pharyngeal loop or by suction retrieval. Further modifications may be needed like use of videolaryngoscope or supraglottic airway device to retrieve. The J tipped guidewires generally exit directly via the nose. Hence, they can be preferred over other guidewires like epidural catheters. Some mouth opening is essential to use these approaches. If absolutely no mouth opening is present, a pharyngeal catheter or fiberoptic bronchoscope may be used.
2.16.2 Which Guidewire Should Be Used for Retrieving by Bronchoscope?
The retrograde guidewire utilized for fiberoptic bronchoscope feed should be sufficiently long, stiff (approximately 100 cm), and easily negotiate the narrow working channel. Otherwise, the guidewire could end up damaging the fiberscope. Antegrade guide catheters such as cardiac catheter, intervention vascular J tip guidewires, cook retrograde intubation set J tip guidewire. Alternatively, an Aintree catheter can be passed over the guidewire, which can accommodate a pediatric fiberoptic bronchoscope. Central venous catheter guidewires are not found suitable as they are not sufficiently long.
2.16.3 Endotracheal Tube Is Passed, but Capnography Trace Is not Obtained?
Failed intubation commonly occurs as inability to pass the endotracheal tube over the guide wire into the trachea or accidental extubation during removal of the guidewire. Endotracheal tube springing into the esophagus after guidewire removal is also common. This can be avoided by threading the guidewire through Murphy’s eye of ETT. Retained guidewire due to slippage of wire further distally into trachea also have been reported for failure.
3 Blind Nasal Intubation
Nasal intubation technique was described first by Kuhn in 1902 [73]. The concept of blind nasal intubation (BNI) was coined by Rowbothom and Magill [74]. The technique became popular during World War I but faded with the advances in airway management subsequently [75,76,77,78]. It has now become limited to medical trainee teaching on intubating mannequins [79]. BNI still remains an useful airway adjunct in resource limited settings, especially among skilled practitioners [80].
Performance of an awake blind nasal intubation has been considered “a dying art” and the impetus shall be on the airway practitioners to preserve it further for the future [81]. Unfortunately blind nasal intubation has been an antiquated technique even in a less resourceful setup and has not been recommended for the re-introduction in the modern era of advanced airway management [82, 83]. BNI although been disregarded, has resurrected its way in airway skill training on intubation mannequins [79, 84]. BNI can still be a lifesaving technique when other airway options have become exhausted [79].
3.1 Technique of BNI
BNI is performed in a spontaneously breathing patient [85]. Pre-operative preparation of the patient dedicatedly improves the success of BNI. Anti-sialagogue, nasopharyngeal decongestion, topicalization (combination of 4% lignocaine, phenylephrine, 10% lignocaine spray, local anesthetic soaked nasal pledgets), and local anesthetic nebulization would result in blunting the airway reflexes [75]. Performance of trans-laryngeal block along with superior laryngeal nerve block either landmark based or utilizing ultrasound, along with sedation would add further to the procedural comfort. Care must be taken not to exceed the total dose of topical and nebulized lignocaine beyond 9 mg/kg.
Well lubricated thin-walled endotracheal tube preferably ivory soft seal cuff made of phthalate (DEHP) directed inferior and posterior to the turbinate, negotiated gently and progressed along the floor of the nose would minimize trauma. Once the tube is in the oral cavity, as indicated by loss of resistance, it is gently pushed forward and tip is positioned close to the laryngeal inlet, as indicated by the feeling air movement across the tube. At this point patient should be asked to take a deep breath and at maximum inspiration, when the glottic opening is maximum, tube can be passed into the trachea.
Various methods have been proposed for improving success during BNI. They include (a) close observation, front of neck palpation and utilizing cuff inflation technique for guiding easy navigation of endotracheal tube [75, 86,87,88], (b) listening to breath sounds originating from the endotracheal tube (poses an infective risk especially in the post-covid era) [75, 89, 90], (c) Mist formation and moisture condensation in the wall of the endotracheal tube during exhalation (not specific to localizing the tube position) [75, 89, 90], (d) attaching a reservoir breathing bag from modified Mapleson breathing circuit. (A technique of blind nasal intubation for anesthesia using the Samson modification of the Mapleson “A” circuit has been described by Veliotes. Adequate depth of anesthesia would be maintained by continuous fresh gas flow insufflation associated with concomitant anesthetic gas scavenging. The movement of the reservoir bag would assist as an intubation guide), (e) adapting a Beck Airway Airflow Monitor (BAAM), whistle or microphone magnifying the breath sounds [89,90,91,92,93], (f) stethoscope attached with an indigenous connector (Binaural or Monaural) [80, 85], (g) mainstream capnography and audio capnometry [82, 85, 89], (h) light guidance using the trans-illumination technique [94,95,96], (i) SCOTI device-Sonomatic Confirmation of Tracheal Intubation (70.8% sensitivity due to its limitation being a static assessment) [97,98,99], and (j) dynamic ultrasound localization. [The visualized glottic structures on real time ultrasound simulate turbulence when the endotracheal tube traverses across the vocal cords]. The linear probe placed over the anterior neck detects an air shadow ripple on translaryngeal window [82, 100]. Blind nasal intubation may often result in esophageal placement of the tube because of reflex swallowing by the patient. Tongue extrusion would result in shifting the supra-laryngeal structures anteriorly, thereby facilitating successful placement of the nasotracheal tube.
3.1.1 Techniques to Minimize Trauma During Blind Nasal Intubation
During nasotracheal intubation, the nasal pathway between the inferior turbinate and the hard palate is chosen to prevent trauma during nasotracheal tube insertion. This has been termed as the “lower pathway.” However, selecting the lower pathway could become challenging especially when BNI is being performed blindly. A cephalad oriented bevel of the endotracheal tube aids in the preferential negotiation into the lower pathway, thereby reducing trauma and epistaxis. The various techniques to reduce trauma during BNI include nasogastric tube guide insertion prior to performance of BNI for better navigation and less manipulation [102, 103], red rubber catheter guide over which endotracheal tube would be trailing [101], nasopharyngeal airway serial dilatation [101], nasopharyngeal airway path finder [104], nasal decongestants, softening of endotracheal tube with warm water/saline at 40 °C [75, 101, 102], use of dexmedetomidine to enable patient to tolerate the endotracheal tube better [105], and maneuvering the endotracheal tube through the lower pathway in the nasal cavity along the nasal floor underneath the inferior turbinate which would minimize trauma (when compared as against passing it through upper pathway between the middle and inferior turbinate) [75]. Furthermore, polyurethane uncuffed tubes, ivory soft seal cuff, and tubes made of phthalate material also minimize nasal bleeding [102].
3.2 Indications and Contraindications
BNI was traditionally being used, in the absence of appropriate alternate devices, in trauma victims with suspected cervical spine injury, wherein basilar skull fracture has been ruled out, presenting for airway control in the emergency room. The common indications are trismus, temporomandibular joint ankylosis, difficult laryngoscopy and intubation, impending airway obstruction, presence of contraindications for front of neck procedures, and postirradiation of head and neck region. In fact, any clinical condition wherein other techniques are contraindicated or failed, or facilities are lacking, BNI can be considered.
Contraindications include acute epiglottitis, basal skull fracture, CSF rhinorrhea, bleeding diathesis, nasal polyps, previous nasal surgery, paranasal abscess, hypertrophic adenoids, apneic patients with impending respiratory arrest supraglottic and laryngeal growth.
3.3 Complications
BNI has a high success rate of 90–92%, even when the operator is relatively inexperienced and is associated with fewer complications (less than 10%) [106, 107]. Reported complications include epistaxis (most common), trauma, bacteremia secondary to mucosal erosion, avulsion of turbinate and septal tear, retropharyngeal dissection leading to perforation, injury to adenoids causing bleeding, fracture of middle turbinate, massive bleeding, olfactory dysfunction, laryngeal trauma, and paranasal sinusitis.
Utility of transnasal humidified rapid insufflation ventilatory exchange (THRIVE) would prevent hypoxemia, if administering sedation becomes inevitable during BNI performance.
4 Digital Tracheal Intubation
The utility of digital tracheal intubation (DTI) assumes utmost importance in an austere environment with limited equipment, when other conventional methods of intubation become impractical, impossible or have failed [108, 109]. The success percentage varies with the skill set reaching up to 89% although often requiring multiple attempts [109]. Just beyond being limited as a historical curiosity, DTI further adds up as an important valuable intubation teaching tool in emergency medicine [109]. With limited equipment and minimal training, an acceptable degree of success could be achieved to secure airway in an unconscious patient. DTI is especially a useful technique among paramedics working in out of hospital scenario with no readily available resources, military medical personnel performing field intubations, clinicians with wilderness skills, disaster management, and emergency medical services [109, 110].
4.1 Historical Perspective
DTI was described initially by Vesalius and later by James Curry in 1792 but was first demonstrated by William MacEwan in 1880 along with chloroform anesthesia performed through a metal tube inserted by blind tactile method [109, 111]. With the discovery of laryngoscope by Chevalier Jackson in 1907, digital intubation became largely out of favor. With further improvements in laryngoscope by Magill in 1920, it almost became an obsolete technique [109].
4.2 Technique
During digital intubation, the epiglottis is palpated digitally, and the endotracheal tube advanced blindly which is guided anteriorly by the fingers providing a navigating landmark [108]. Bougie, internal stylets facilitate intubation and add to the success when performed on airway mannequins.
The index and long fingers of non-dominant hand hold the soft tissues of oral cavity in alignment with the endotracheal tube, which is then passed over the base of the tongue and directed into the trachea. The fingers are extended beyond the base of the tongue, sweeping across to reach the epiglottis. The epiglottis is then lifted by the fingers like a Miller laryngoscope blade and guiding the endotracheal tube between the fingers into the trachea. The endotracheal tube is advanced by the dominant hand, ensuring the distal tip of endotracheal tube brushes across the volar surface of the fingers used for guiding [109, 112,113,114].
4.3 Indications and Contraindications
Indications are out of hospital emergency scenarios (Entrapment in collided vehicle preventing traditional airway management) [109], airway trauma with copious blood and vomitus preventing a laryngoscope/fiberscope view [109], inability to visualize vocal cords with conventional laryngoscope in maxillofacial polytrauma victims needing emergency airway control prior to an attempted surgical airway [109]. Fixed flexion deformity in ankylosing spondylitis with failure to position the patient supine needing assistance (awake video laryngoscope guidance facing the patient along with DTI has been described) [115], and limited extension at atlanto occipital joint (DTI with Bougie guided intubation described) [116]. Neonatal DTI in labor room also has been reported [117].
DTI is contraindicated in patients with intact oro-pharyngeal and gag reflexes [110].
4.4 Complications
The success rate of DTI depends on the familiarity of the procedure and the skill set of the clinician. Complications include soft tissue injury and creation of false passage due to avulsion injury.
5 Complications
Retrograde intubation still finds a definite place in the armamentarium of difficult airway with short learning curve and stays relevant with its modifications even in the present fibreless endoscope era. Difficult airway simulation exercise must include retrograde intubation in its learning domain.
References
King HK, Wang LF, Khan AK, Wooten DJ. Translaryngeal guided intubation for difficult intubation. Crit Care Med. 1987;15:869–71.
Dhara SS. Retrograde tracheal intubation. Anaesthesia. 2009;64:1094–104.
Burbulys D, Kiai K. Retrograde intubation. Emerg Med Clin North Am. 2008;26:1029–41.
Butler FS, Cirillo AA. Retrograde tracheal intubation. Anesth Analg. 1960;39:333–8.
Waters DJ. Guided blind endotracheal intubation: For patients with deformities of the upper airway. Anaesthesia. 1963;18:158–62.
McNamara RM. Retrograde intubation of the trachea. Ann Emerg Med. 1987;16:680–2.
Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiology. 1991;75:1087–110.
Stern Y, Spitzer T. Retrograde intubation of the trachea. J Laryngol Otol. 1991;105(9):746–7.
Hung OR, al-Qatari M. Light-guided retrograde intubation. Can J Anaesth. 1997;44(8):877–82.
Benumof JL. The American Society of Anesthesiologists management of the difficult airway algorithm and explanation-analysis of the algorithm. In: Benumof JL, editor. Airway management: principles and practice. St Louis: C.V. Mosby; 1998. p. 151–3.
Practice guidelines for management of the difficult airway. An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–77.
Ovassapian A, Yelich SJ, Dykes MHM, Brunner EE. Fiberoptic nasotracheal intubation—incidence and cause of failure. Anesth Analg. 1983;62:692–5.
Weksler N, Klein M, Weksler D, et al. Retrograde tracheal intubation: beyond fibreoptic endotracheal intubation. Acta Anaesthesiol Scand. 2004;48(4):412–6.
Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. Anesthesiology. 1995;82:367–76.
Brenman S, Gupta S, Tseeng S. Successful retrograde intubation after failed fiberoptic intubation and percutaneous cricothyrotomy. J Emerg Med. 2017;53(4):550–3.
Barriot P, Riou B. Retrograde technique for tracheal intubation in trauma patients. Crit Care Med. 1988;16(7):712–3.
Gill M, Madden MJ, Green SM. Retrograde endotracheal intubation: an investigation of indications, complications, and patient outcomes. Am J Emerg Med. 2005;23(2):123–6.
Jain G, Singh DK, Yadav G, Gupta SK, Tharwani S. A modification in the tube guide to facilitate retrograde intubation: A prospective, randomised trial. Indian J Anaesth. 2011;55(5):499–503.
Lenfant F, Benkhadra M, Trouilloud P, Freysz M. Comparison of two techniques for retrograde tracheal intubation in human fresh cadavers. Anesthesiology. 2006;104:48–51.
Tüfek A, Uçan MC, Tokgöz O, Çelik F, Ağaçayak S. Evaluation of retrograde intubation in patients with limited mouth opening. J Anesth. 2013;27(4):631–2.
Slots P, Vegger PB, Bettger H, Reinstrup P. Retrograde intubation with a Mini-Trach II kit. Acta Anaesthesiol Scand. 2003;47(3):274–7.
Vieira D, Lages N, Dias J, Maria L, Correia C. Ultrasound-guided retrograde intubation. Anaesthesia. 2013;68:1075–6.
Vieira D, Lages N, Dias J, Maria L, Correia C. Retrograde intubation: An old new technique. Anaesthesia. 2013;68(10):1075–6.
Varshney PG, Kachru N. Fibreoptic-aided retrograde intubation: Is it useful to combine two techniques? Indian J Anaesth. 2011;55:546–7.
Kristensen MS, McGuire B. Managing and securing the bleeding upper airway: a narrative review. Can J Anaesth. 2020;67(1):128–40.
Harris EA, Fischler KE. Does the site of anterior tracheal puncture affect the success rate of retrograde intubation? Br J Anaesth. 2013;110(6):1064–5.
Vithal K, et al. Retrograde intubation in temporomandibular joint ankylosis—a double guide wire technique. Indian J Anaesth. 2008;52(1):90–2.
Vadepally AK, Sinha R, Kumar AVSSS. Retrograde intubation through nasal route in patients with limited mouth opening undergoing oral and maxillofacial surgery. J Oral Biol Craniofac Res. 2018;8(1):30–4.
Ball DR, Stallard M. Retrograde tracheal intubation for bleeding and fragmenting airway tumours. Anaesthesia. 2014;69(2):182.
Ramsey CA, Dhaliwal SS. Retrograde and submental intubation. Atlas Oral Maxillofacial Surg Clin North Am. 2010;18:61–8.
Arndt GA, Topp J, Hannah J, McDowell TS, Lesko A. Intubation via the LMA using a Cook retrograde intubation kit. Can J Anaesth. 1998;45:257–60.
Fichtner A, Vrtny P, Schaarschmidt F. Ultrasound-guided retrograde emergency intubation. Anaesthesist. 2015;64:948–52.
Green JS, Tsui BC. Application of ultrasonography in ENT: Airway assessment and nerve blockade. Anesthesiol Clin. 2010;28:541–53.
Dinsmore J, Heard AM, Green RJ. The use of ultrasound to guide time-critical cannula tracheotomy when anterior neck airway anatomy is unidentifiable. Eur J Anaesthesiol. 2011;28(7):506–10.
Lechman MJ, Donahoo JS, MacVaugh H III. Endotracheal intubation using percutaneous retrograde guidewire insertion followed by antegrade fiberoptic bronchoscopy. Crit Care Med. 1986;14:589–90.
Gupta B, McDonald JS, Brooks JHJ, Mendenhall J. Oral fiberoptic intubation over a retrograde guidewire. Anesth Analg. 1989;68:517–9.
Tobias R. Increased success with retrograde guide for endotracheal intubation. Anesth Analg. 1983;62:366–7.
Roberts KW, Solgonick RM. A modification of retrograde wire–guided fibreoptic assisted endotracheal Intubation in a patient with ankylosing spondylitis. Anesth Analg. 1996;82:1290–1.
Bissinger U, Guggenberger H, Lenz G. Retrograde-guided fiberoptic intubation in patients with laryngeal carcinoma. Anesth Analg. 1995;81:408–10.
Audenaert SM, Montgomery CL, Stone B. Retrograde-assisted fibreoptic tracheal intubation in children with difficult airways. Anesth Analg. 1991;73(5):660–4.
Eidelman LA, Pizov R. A safer approach to retrograde-guided fiberoptic intubation. Anesth Analg. 1996;82(5):1108.
Przybylo HJ, Stevenson GW, Vicari FA. Retrograde fibre optic intubation in a child with Nager’s syndrome. Can J Anaesth. 1996;43:697–9.
Rosenblatt WH, Angood PB, Maranets I. Retrograde fiberoptic intubation. Anesth Analg. 1997;84(5):1142–4.
Dhanyee AS, Pillai R, Sahajanandan R. Wire guided fibreoptic retrograde intubation in a case of glottic mass. Indian J Anaesth. 2016;60(3):219–21.
Harvey SC, Fishman RL, Edwards SM. Retrograde intubation through a laryngeal mask airway. Anesthesiology. 1996;85(6):1503–4.
Miner JR, Rubin J, Clark J, Reardon RF. Retrograde Intubation with an Extraglottic Device in Place. J Emerg Med. 2015;49(6):864–7.
Ciftci T, Erbatur S. Retrograde intubation via laryngeal mask airway in a paediatric patient with fallot-type ventricular septal defect and cleft palate deformity. Middle East J Anaesthesiol. 2016;23(4):479–82.
Parmet J, Metz S. Retrograde endotracheal intubation: an underutilized tool for management of the difficult airway. Contemp Surg. 1996;49(5):300–6.
Wijesinghe H, Gough J. Complications of a retrograde intubation in a trauma patient. Acad Emerg Med. 2000;7(11):1267–71.
Bowes WA, Johnson JO. Pneumomediastinum after planned retrograde fiberoptic intubation. Anesth Analg. 1994;78:795–7.
Beebe DS, Tran P, Belani KG, Adams GL. Pretracheal abscess following retrograde tracheal intubation [Letter]. Anaesthesia. 1995;50(5):470.
Akinyemi O. Complications of guided blind endotracheal intubation. Anesthesia. 1979;34:590–2.
Contrucci RB, Gottlieb JS. A complication of retrograde endotracheal intubation [Letter]. Ear Nose Throat J. 1990;69(11):776–8.
Loh KS, Irish JC. Traumatic complications of intubation and other airway management procedures. Anesthesiol Clin North Am. 2002;20(4):953–69.
Claffey LP, Phelan DM. A complication of cricothyroid ‘minitracheostomy’ ± oesophagal perforation. Intensive Care Med. 1989;15:140–1.
Ratnayake B, Langford RM. A survey of emergency airway management in the United Kingdom. Anaesthesia. 1996;51:908–11.
Van Stralen DW, Rogers M, Perkin RM, Fea S. Retrograde intubation training using a mannequin. Am J Emerg Med. 1995;13(1):50–2.
Powell WF, Ozdil T. A translaryngeal guide for tracheal intubation. Anesth Analg. 1967;46:231–4.
Harmer M, Vaughan RS. Guided blind oral intubation. Anaesthesia. 1980;35:921.
Borland LM, Swan DM, Leff S. Difficult pediatric intubation: a new approach to the retrograde technique. Anesthesiology. 1981;55:577–8.
Mounir N, Madi A, Trop D. Pulling versus guiding: a modification of retrograde guided intubation. Can J Anaesth. 1989;36:336–9.
Mahajan R, Sandhya X, Chari P. An alternative technique for retrograde intubation (correspondence). Anaesthesia. 2001;56:1207–8.
Arya VK, Dutta A, Chari P. Diffcult retrograde endotracheal intubation: the utility of a pharyngeal loop. Anesth Analg. 2002;94:470–3.
Marciniak D, Smith CE. Emergent retrograde tracheal intubation with a gum-elastic Bougie in a trauma patient. Anesth Analg. 2007;105:1720–1.
Sanchez A. Retrograde intubation techniques. In: Hagberg CA, editor. Benumof’s airway management: principles and practice. 3rd ed. Philadelphia: Saunders; 2013. p. 419–26.
Sriramka B, Mallik D, Khetan M, Moda N. Revisiting the awake retrograde nasal intubation technique. J Dent Anesth Pain Med. 2018;18(5):315–7.
Gerenstein RI, Arria-Devoe G. Jwire and translaryngeal guided intubation. Crit Care Med. 1989;17:486.
Gerenstein RI. J-wire facilitates translaryngeal guided intubation. Anesthesiology. 1992;76:1059.
Xue FS, Li QX. Retrograde intubation techniques. In: Xue FS, editor. Modern airway management: a key technique for clinical anesthesia and critical care medicine. Zheng-Zhou: Zheng-Zhou University Publishing House; 2002. p. 474–89.
Bourke D, Levesque PR. Modification of retrograde guide for endotracheal intubation. Anesth Analg. 1974;53:1013–104.
Abou-Madi MN, Trop D. Pulling versus guiding: a modification of retrograde guided intubation. Can J Anaesth. 1989;36:336–9.
Hines MH, Meredith JW. Modified retrograde intubation technique for rapid airway access. Am J Surg. 1990;159:597–9.
Kuhn F. Die pernasale tubage. München Med Wochenschr. 1902;49:1456.
Rowbotham ES, Magill I. Anaesthetics in the plastic surgery of the face and jaws. Proc R Soc Med. 1921;14:17–27.
Chauhan V, Acharya G. Nasal intubation: A comprehensive review. Indian J Crit Care Med. 2016;20(11):662–7.
Rowbotham S. Intratracheal anaesthesia by the nasal route for operations on the mouth and lips. Br Med J. 1920;2:590.
Magill IW. Technique in endotracheal anaesthesia. Br Med J. 1930;2:817.
Magill IW. Endotracheal anaesthesia. Am J Surg. 1936;34:450–5.
Hung O, Zhang J, Lamb A, Hung C, Hung D, Stewart R. Teaching blind nasal intubation in Rwanda. Can J Anaesth. 2015;62(5):553–4.
Harris RD, Gillett MJ, Joseph AP, Vinen JD. An aid to blind nasal intubation. J Emerg Med. 1998;16(1):93–5.
Collins PD, Godkin RA. Awake blind nasal intubation—a dying art? Anaesth Intensive Care. 1992;20(2):225–7.
Dubey PK, Dubey P, Kumar N, Bhardwaj G, Kumar N. Blind nasal intubation revisited: no longer a blind technique? J Emerg Med. 2017;52(2):231–4.
Wilkinson DJ. Providing quality in anesthesia care in low- and middle-income countries. Can J Anaesth. 2014;61:975–8.
Kuduvalli PM, Jervis A, Tighe SQ, Robin NM. Unanticipated difficult airway management in anaesthetised patients: a prospective study of the effect of mannequin training on management strategies and skill retention. Anaesthesia. 2008;63:364–9.
Shapiro H, Unger R. Blind, but not deaf or dirty, intubations. Anesthesiology. 1986;64(2):297.
Kumar R, Gupta E, Kumar S, Rani Sharma K, Rani GN. Cuff inflation-supplemented laryngoscope-guided nasal intubation: a comparison of three endotracheal tubes. Anesth Analg. 2013;116(3):619–24.
Gorback MS. Inflation of the endotracheal tube cuff as an aid to blind nasal endotracheal intubation. Anesth Analg. 1987;66:916–7.
van Elstraete AC, Pennant JH, Gajraj NM, Victory RA. Tracheal tube cuff inflation as an aid to blind nasotracheal intubation. Br J Anaesth. 1993;70:691–3.
Omoigui S, Glass P, Martel DL, Watkins K, Williams KL, Whitefield SM, Wooten LL. Blind nasal intubation with audio-capnometry. Anesth Analg. 1991;72(3):392–3.
Zhang J, Lamb A, Hung O, Hung C, Hung D. Blind nasal intubation: teaching a dying art. Can J Anaesth. 2014;61(11):1055–6.
Dyson A, Saunders PR, Giesecke AH. Awake blind nasal intubation: use of a simple whistle. Anaesthesia. 1990;45:71–2.
Cook RT Jr, Stene JK Jr. The BAAM and endotrol endotracheal tube for blind oral intubation. Beck Airway Air Flow Monitor. J Clin Anesth. 1993;5:431–2.
Hamill M, Toung T. Blind nasotracheal intubations revisited. Anesth Analg. 1994;79:390–1.
Nofal O. Awake light-aided blind nasal intubation: prototype device. Br J Anaesth. 2010;104(2):254–9.
Iseki K, Murakawa M, Tase C, Otsuki M. Use of a modified lightwand for nasal intubation. Anesthesiology. 1999;90:635.
Dong Y, Li G, WuW SR, Shao Y. Lightwand-guided nasotracheal intubation in oromaxillofacial surgery patients with anticipated difficult airways: a comparison with blind nasal intubation. Int J Oral Maxillofac Surg. 2013;42:1049–53.
Trikha A, Singh C, Rewari V, Arora MK. Evaluation of the SCOTI device for confirming blind nasal intubation. Anaesthesia. 1999;54(4):347–9.
Murray D, Ward ME, Sear JW. SCOTI—a new device for identification of tracheal intubation. Anaesthesia. 1995;50:1062–4.
Haridas RP, Chesshire KJ, Rocke DA. An evaluation of SCOTI device. Anaesthesia. 1997;52:453–6.
Dubey PK, Akhileshwar. Ultrasound-guided blind nasal intubation in a patient with massive oral tumor. Paediatr Anaesth. 2018;28(3):300–1.
Elwood T, Stillions DM, Woo DW, Bradford HM, Ramamoorthy C. Nasotracheal intubation: a randomized trial of two methods. Anesthesiology. 2002;96(1):51–3.
Lim CW, Min SW, Kim CS, Chang JE, Park JE, Hwang JY. The use of a nasogastric tube to facilitate nasotracheal intubation: a randomised controlled trial. Anaesthesia. 2014;69(6):591–7.
Sugiura N, Miyake T, Okui K, Hibi G, Oka T, Yamada M, Arai T. Increased success of blind nasotracheal intubation through the use of nasogastric tubes as a guide. Anesth Prog. 1996;43(2):58–60.
Enk D, Palmes AM, Van Aken H, Westphal M. Nasotracheal intubation: a simple and effective technique to reduce nasopharyngeal trauma and tube contamination. Anesth Analg. 2002;95(5):1432–6.
Dhasmana SC. Nasotracheal fiberoptic intubation: patient comfort, intubating conditions and hemodynamic stability during conscious sedation with different doses of dexmedetomidine. J Maxillofac Oral Surg. 2014;13(1):53–8.
Thongrong C, Thaisiam P, Kasemsiri P. Validation of simple methods to select a suitable nostril for nasotracheal intubation. Anesthesiol Res Pract. 2018;2018:4910653.
Dauphinee K. Nasotracheal intubation. Emerg Med Clin North Am. 1988;6(4):715–23.
Juergens AL 2nd, Odom BW, Ren CE, Meyers KE. Success rates with digital intubation: comparing unassisted, stylet, and gum-elastic Bougie techniques. Wilderness Environ Med. 2019;30(1):52–5.
Hardwick WC, Bluhm D. Digital intubation. J Emerg Med. 1984;1(4):317–20.
Shiber JR, Fontane E. Digital tracheal intubation: an effective technique that should not be forgotten. Am J Emerg Med. 2007;25(6):726.
Vesalius A. De Humani Corporis Fabrica. Basil, Switzerland, lS43:658. Located at: History and Special Collection Division, Louise M. Darling Biomedical Library. University of California at Los Angeles; 1543.
Young SE, Miller MA, Crystal CS, Skinner C, Coon TP. Is digital intubation an option for emergency physicians in definitive airway management? Am J Emerg Med. 2006;24(6):729–32.
Cook RT Jr. Digital endotracheal intubation. Am J Emerg Med. 1992;10(4):396.
Stewart RD. Tactile orotracheal intubation. Ann Emerg Med. 1984;13(3):175–8.
Hsieh PS, Ma HP, Wong CS, Ong JR. Emergency tracheal intubation in an ankylosing spondylitis patient in a sitting position using an airway scope combined with face-to-face and digital intubation. J Emerg Med. 2018;54(5):674–7.
Rich JM. Successful blind digital intubation with a Bougie introducer in a patient with an unexpected difficult airway. Proc (Bayl Univ Med Cent). 2008;21(4):397–9.
Moura JH, da Silva GA. Neonatal laryngoscope intubation and the digital method: a randomized controlled trial. J Pediatr. 2006;148(6):840–1.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Ramkiran, S., Bidkar, P.U. (2023). Unconventional Intubation Techniques. In: Ubaradka, R.S., Gupta, N., Bidkar, P.U., Tripathy, D.K., Gupta, A. (eds) The Airway Manual. Springer, Singapore. https://doi.org/10.1007/978-981-19-4747-6_22
Download citation
DOI: https://doi.org/10.1007/978-981-19-4747-6_22
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-4746-9
Online ISBN: 978-981-19-4747-6
eBook Packages: MedicineMedicine (R0)