Abstract
Electromagnetic (EM) navigation is a frameless stereotactic navigation technology, which integrates electromagnetic technology, modern diagnostic radiology technology, stereotactic technology, and minimally invasive surgery. With the assistance of a high-performance computer, it can accurately display the anatomical structure of the spine, the three-dimensional spatial position, and adjacent relationship of lesions. Electromagnetic-based (EM-based) navigated transforaminal endoscopic lumbar discectomy (TELD) has the following advantages: (1) Improving the surgical safety and accuracy of lesion resection. (2) It can determine the positional relationship between intervertebral disc lesion, peripheral blood vessels, and the range of decompression, effectively avoiding damage to normal tissue. (3) It is beneficial for individualized puncture design, which helps in avoiding key structural and functional areas in the spinal canal, and consequently reduces surgical trauma. (4) It can expand surgical indications and effectively avoid trauma and complications caused by routine open surgery. Although electromagnetic navigation can largely reduce the learning curve of TELD to young surgeons, navigation itself has a steep learning curve. It is necessary to be fully familiar with the applicable specifications of navigation and accumulate the experience in order to better combine electromagnetic navigation technology with TELD and improve the overall efficiency of surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Electromagnetic navigation
- Lumbar discectomy
- Transforaminal endoscopic lumbar discectomy
- Minimally invasive spine surgery
-
1.
Transforaminal endoscopic lumbar discectomy (TELD) is one of the most minimally invasive techniques for the treatment of lumbar disc herniation. It is completed under local anesthesia and is attributed with less bleeding and soft tissue trauma. The working channel enters the intervertebral disc through the natural foramen and hardly damages the normal anatomical structure. Thus, the patient can resume normal social activities soon after surgery. However, this minimally invasive technique has a steep learning curve. Especially for beginners, without good intraoperative guidance, serious complications may occur, such as dural sac tear and nerve injury.
-
2.
Electromagnetic (EM) navigation is a frameless stereotactic navigation technology, which integrates electromagnetic technology, modern diagnostic radiology technology, stereotactic technology, and minimally invasive surgery. With the assistance of a high-performance computer, it can accurately display the anatomical structure of the spine, the three-dimensional spatial position, and adjacent relationship of lesions.
-
3.
EM-based navigation-guided TELD has the advantages of good positioning accuracy, real-time monitoring, and great reduction of X-ray perspective. The new technique is especially helpful for inexperienced spinal surgeons. Its application prospect is very broad in the future, and EM-based navigation will further promote the development of percutaneous endoscopic spinal surgery.
1 Introduction
In 1975, Hijikata et al. [1] performed mechanical percutaneous nucleotomy (PN) via posterolateral access to treat lumbar disc herniation for the first time. Under local anesthesia, the working channel was inserted into the intervertebral disc through a small skin incision via posterolateral access for nucleus pulposus resection. However, since the position of the working cannula is determined under C-arm fluoroscopy rather than under microscopic guidance, the cannula cannot enter the spinal canal, so this is an indirect decompression technique without direct vision. Similarly, automated percutaneous lumbar discectomy (APLD) [2] was also applied to remove nuclear material in the following years. Nonetheless, later studies have demonstrated that the success rate of this technique was no more than 65%, which is not different from that of conservative treatment. In addition, the surgical indications of these two methods are relatively narrow and mainly suitable for inclusive lumbar disc herniation, a relatively rare type of lumbar disc herniation. Following Hijikata’s experience, Schreiber [3] improved the original instruments and developed a series of cannulas and a modified arthroscopic technique, which help to remove nucleus pulposus more accurately and effectively, with a reported success rate of 72.5%. One year later, Hausmann et al. [4] also reported that a detailed and risk-free observation of the intervertebral disc space could be performed through improved arthroscopy.
Kambin et al. [5] described the anatomic boundaries of the “safe working zone” of a lumbar intervertebral foramen in the 1990s, which laid the theoretical foundation for the development of percutaneous endoscopic lumbar discectomy (PELD). In 1997, Yeung [6] successfully developed the third-generation spinal endoscope, the Yeung endoscopic spine system (YESS), which emphasized access to the intervertebral disc through the “Kambin’s triangle,” thereby removing the nucleus pulposus tissue from the inside out under direct vision and achieving indirect decompression under vision. Yeung’s technique of “inside out,” carried out with a 2.8 mm surgical channel, is relatively simple and safe for use in cases including inclusive, subligamentous lumbar disc herniation and some discogenic back pain. Yeung and Tsou [7] performed at least a one-year retrospective analysis of 307 patients undergoing PELD. The postoperative satisfaction rate was 90.7%, and the excellent and good rate was 89.3% according to the improved Macnab evaluation criteria, while the incidence of complications was 3.5%. The surgical results were comparable to that of intervertebral fenestration discectomy. However, since this technique warrants decompression inside the disc, its indication is relatively narrow, and it is difficult to work for expelled nucleus and sequestered disc. Furthermore, the nerve root and dural sac cannot be exposed under the microscope, and it is highly vulnerable to damage to the nerve root when entering and exiting through the Kambin’s triangle.
To address the shortcomings of the YESS technique, Hoogland [8] developed the Thomas Hoogland Endoscopic Spine System (THESSYS) in 2003 with a wider range of indications compared to the YESS technique. Hoogland described the “outside-in” approach for transforaminal endoscopic technique by cutting the facet and direct landing into the epidural space so that the ligamentum flavum, dural sac, nerve root, and herniated nucleus pulposus can be seen under a microscope. However, this technique has high technical requirements and a steep learning curve, so beginners are prone to damage spinal nerve roots, blood vessels, and dural sac, which may lead to serious complications. Hoogland et al. [9] reported that 262 patients with recurrent lumbar disc herniation were treated by THESSYS, among which 238 patients (90.84%) completed a 2-year follow-up, with a reported 3.8% complication rate which included 3 cases of nerve root stimulation, 7 cases of early recurrent herniation (<3 months), and no postoperative infection and discitis. Likewise, Schubert et al. [7] performed foraminoplasty by cutting part of the upper facet joint with Hoogland-designed bone reamers to directly insert the c into the spinal canal, and then remove the migrated nucleus pulposus tissue with endoscopic assistance. The postoperative excellent and good rate was 95.3% and the recurrence rate was 3.6%. Furthermore, he believed that the greatest advantage of the THESSYS technique was that the extruded and sequestered nucleus pulposus tissue inside the spinal canal could be directly removed. However, he deemed it relatively difficult to deal with the necrotic and broken nucleus pulposus tissue due to the difficulty of entering the disc, which increased the risk of postoperative recurrence.
Although transforaminal endoscopic lumbar discectomy (TELD) is the most advanced and minimally invasive surgical method for the treatment of lumbar disc herniation, there are still several complications [10,11,12,13,14,15]. These complications include the following: (1) Nerve root injury: the process of puncture, expansion, and working tube insertion without direct vision may result in nerve root injury due to the anatomic variation. (2) Dural sac rupture: It is a rare but serious complication, mainly related to mechanical wear of surgical instruments or radiofrequency thermal injury during operation. (3) Incomplete decompression and postoperative recurrence: Incomplete decompression is often due to incomplete removal of protrusions, stenosis of a nerve root canal, or insufficient foraminoplasty. Postoperative recurrence is mainly related to the incomplete removal of compressive factors, improper postoperative nursing strategy, early stooping, or sneezing. (4) Abdominal and vascular injury: The blood vessels may be damaged during the process of establishing working channels and the puncture needle may enter the abdominal cavity, resulting in viscera (intestinal canal, kidney, and large blood vessel) injury. The occurrence of these complications is mainly related to factors such as poor technical proficiency and inexperience. Moreover, the routine TELD process not only needs to be carried out under the guidance of repeated X-ray fluoroscopy but also needs dynamically detection of the location of the surgical instruments to ensure the safety of patient, which is especially complicated for beginners and may pose additional radiation damage to both doctors and patients.
Electromagnetic (EM) navigation is a frameless stereotactic navigation technology, which integrates electromagnetic technology, modern diagnostic radiology technology, stereotactic technology, and minimally invasive surgery [16,17,18,19,20,21]. It can accurately show the anatomical structure of the spine and the three-dimensional spatial position and adjacent relationship of lesions with the assistance of a high-performance computer [20, 21]. The system is based on powerful computer technology and image processing software, obtaining the relative position of the patient’s vertebral body, articular process, intervertebral disc, and surgical instruments through infrared remote sensing technology and electromagnetic principle, and calculates and displays the relationship between the real-time process of the operation, the accurate location of the lesion, and the surrounding structures. In a word, electromagnetic-based (EM-based) navigation-guided TELD has the advantages of good positioning accuracy and real-time monitoring and is capable of greatly reducing X-ray perspective
2 Components of the Electromagnetic Navigation System
The electromagnetic navigation system (Fiagon GmbH, Germany) for TELD consists of a navigation screen (Fig. 12.1), navigation module, and tracking pointer (Fig. 12.2). There are three windows in the navigation screen, two of which display the position and dynamic changes of surgical tools simulated on anteroposterior and lateral views and the third window displaying the video image of the surgical field as visualized by the endoscope. The navigation module is equipped with a DVD drive, USB port, plug points for navigation sensor, patient localizer, virtual endoscopy planning software, and pointer system. The pointer system is equipped with a connecting plug, pointer, and sensor cable that allows for precise tracking of both position and orientation throughout the electromagnetic field. The special I-See endoscopic spine surgical system (Joimax, IseeU, Germany) (Fig. 12.3) is the instrument dedicated to matching the EM navigation.
3 Indications and Contraindications
3.1 Indications
-
1.
Central, paracentral, extreme-lateral, or prolapsed lumbar disc herniation.
-
2.
Radiation pain in a single lower limb with or without back pain, positive Lasegue sign.
-
3.
Mono-segment of lumbar disc herniation or prolapsed suggested by MRI or CT scans.
-
4.
Failure of strict conservative treatments for at least 3 months.
-
5.
Patients who fail to remit or who relapse after other minimally invasive interventional surgery.
3.2 Contraindications
-
1.
Clinical symptoms or physical examination signs that do not match the radiographic results
-
2.
Cauda equina syndrome
-
3.
Lumbar segmental instability and lumbar spondylolisthesis
-
4.
Lumbar infections, tumors, or deformities
-
5.
Poor local skin condition or wounds at the surgical incision site
-
6.
Patients who are unable to tolerate surgery or cannot cooperate for other reasons
4 Surgical Procedure
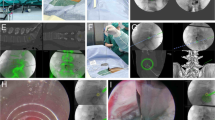
The patient is placed in the prone position on a special, non-metallic, carbon fiber operating (OR) table to prevent electromagnetic interference. The magnetic field generator is fixed on the OR table close to the patient’s hip so that the frame encompasses the entire surgical field. After preparation of the operation site, the k-wire is drilled into the spinous process of the caudal vertebral body adjacent to the operative segment to a depth of 2 cm to make it firmly fixed, and the locator is placed on the skin 5–10 mm away from the k-wire. Thereafter, the tracker is firmly connected with the spinous process, and a mapper bridge is placed next to the locator which is identified by the landmarks in the anteroposterior and lateral X-ray images (Fig. 12.4).
After the perspective image is transmitted to the navigation system via the USB driver, the system automatically performs registration by loading the data. Upon confirmation of registration, intraoperative two-dimensional (2D) images are used to match preoperative computed tomography (CT) image data, and the three-dimensional (3D) data sets enable virtual real-time navigation. The target point (the superior articular process or the herniated disc is usually selected as the target point) of puncture must be set on the EM navigation system at the beginning of the operation (Fig. 12.5).
The operation is performed under local infiltration anesthesia by injecting lidocaine into soft tissue. Firstly, the inner core of the 18-gauge puncture needle is removed, which is replaced by the IseePointer sensor. Consequently, the puncture needle is maintained on the multifunctional board for calibration until the needle symbol appears in the upper right corner of the navigation display. After that, the needle is inserted by a posterolateral approach to the target disc under the guidance of real-time navigation view until it reaches the target. During the process, the changes of the puncture needle angle and depth can be seen in real time (Fig. 12.6).
When the angle is correct, it remains green and only turns red if the puncture angle deviates significantly from the design path. Subsequent surgical procedures are as follows: (1) The needle is replaced with a 0.8-mm guidewire, and (2) then a 1.5 cm skin incision is made along the guidewire. (3) After calibration, a gentle sequential dilatation technique is performed to protect the exiting nerve root and to prevent access pain. (4) The semi-serrated outer working cannula is inserted into a navigation rod consisting of IseePointer and adapters, and (5) then into the calibrated trephine. (6) A rigid, rod-lens endoscope with a working channel is introduced, and selective foraminoplasty and discectomy are performed under continuous normal saline irrigation. (7) The depth of endoscope entry and the position of surgical instruments can be visualized in real time under navigation monitoring. At this time, the lateral border of the ipsilateral ligamentum flavum is resected, the degenerative and protruding intervertebral disc is removed, and the nerve roots are decompressed appropriately. Finally, the end-point is determined with the free mobilization of the exiting nerve root and the dural sac.
Both the preoperative MRI and CT determine and confirm the location of the disc herniation and guide the working channel placement and decompression: (1) for the most common type of LDH, paracentral type, the first task is to find the space between ligamentum flavum and intervertebral disc after foraminoplasty and then to explore the rupture of a disc in the abdominal direction. Remove the protruding nucleus pulposus around the rupture until the ventral side of the nerve root can be seen. If the nerve root can easily fluctuate in water pressure, it indicates that the nerve root has been decompressed successfully and radiofrequency ablation can be used to treat the rupture of annulus fibrosus. (2) For prolapse or sequestration, adequate foraminoplasty is needed to remove part of the bony structure of the superior articular process so that the working channel can enter the target. Generally speaking, after removing the prolapsed nucleus pulposus in the spinal canal, it is necessary to swing the working channel to explore the rupture of the intervertebral disc and remove the degenerative nucleus pulposus in the disc to reduce probability of recurrence. (3) For the extreme-lateral LDH, the working tube is not needed to enter the intervertebral foramen, but it is needed to reach the lateral edge of the articular process in the anterior-posterior view and the posterior edge of the intervertebral disc in the lateral view, simultaneously. After that, the protruding disc and exiting nerve root can be detected. (4) For the completely contained LDH, the working channel can be directly placed into the intervertebral disc without foraminoplasty if the intervertebral foramen is large enough, and the degenerative nucleus pulposus is directly removed. Then, the working channel is gradually withdrawn to the intervertebral foramen area and the nerve root is subsequently explored.
There is no need to place drainage tubes after an operation, and the patient does not need to take antibiotics or painkillers. After 3-h observation postoperatively, the patient is allowed to walk on the ground wearing protective equipment if they have no obvious discomfort. Patients are discharged on the day of surgery or the first day after surgery, but they are informed of precautions in the first 6 weeks, such as reducing strenuous activities, avoiding overwork, or stooping with long hours.
5 Case Study
Male, 54 years old.
Symptoms: Radiation pain from the low back area, down to the left leg and into the left feet for more than 2 years, aggravated in the past 3 months. Activities such as bending, lifting, twisting, and sitting increased the pain. Patient had undergone repeated conservative treatment and steroid blockade with unsuccessful clinical response.
Physical examination: The Lasegue sign was positive on the left side.
The visual analog scale (VAS) was 7/10 (Figs. 12.7, 12.8, 12.9, and 12.10).
6 Discussion
The key prerequisite for a successful TELD is to establish a working channel accurately and safely. The Kambin’s triangle is small because of the occlusion of the superior articular process of the lumbar vertebrae, especially for patients with long and narrow intervertebral foramen, which greatly increases the difficulty of accurate insertion of working cannulas during TELD. For beginners with poor 3D sense and inexperience, the difficulty of performing TELD will be magnified, and the risk of nerve injury will increase as well. In order to ensure operational safety, the working cannulas are inserted under the monitoring of C-arm X-ray fluoroscopy, which virtually increases the radiation exposure of both patients and doctors. Increasing studies have shown that different doses of radiation exposure can induce tumors, cataracts, cardiovascular diseases, etc., posing a serious threat to the health of patients and medical staff [1].
Computer navigation technology is a manifestation of minimally invasive and accurate medical treatment. Navigation technology can accurately locate the lesions, help to select the best surgical approach reasonably, and effectively reduce surgical injury and complications. According to the space position of the instrument, the signals can be divided into optics (infrared ray), magnetism (electromagnetism), and acoustic (ultrasound), and the corresponding navigation is called photoelectric, electromagnetic, and acoustic navigation systems, respectively [21,22,23,24,25,26,27].
The different navigation systems have diverse advantages and disadvantages [2]: (1) Optoelectronic navigation has the highest accuracy, but the signal may be blocked by surgical instruments and operators, and it is expensive. (2) Although ultrasound navigation has the advantages of non-invasive, radiation-free, and real-time tracking, it has not been widely used in clinical practice. (3) Electromagnetic navigation is not restricted by visual field and sightline, especially suitable for minimally invasive spinal surgery, but it is easily affected by environmental ferromagnetic effects. Due to the poor penetrability of ultrasound signals in bone, the guiding performance of the deep spine and spinal canal cannot meet the clinical requirements. The current navigation applications used in spine surgery are mainly optoelectronic navigation and electromagnetic navigation. Optoelectronic navigation is traditional navigation. As a traditional navigation technology, photoelectric navigation has strong anti-interference ability, stable signal, no obvious influence on other equipment in an operating room, and low cost, but there are unfavorable factors such as large size and heavy equipment. In addition, optical navigation may cause navigation interruption through the blocking of light source by surgeons or surgical instruments. Under the guidance of intraoperative imaging (C-arm, O-arm), spinal surgeons perform operations based on their clinical experience and skills.
On the contrary, electromagnetic navigation is a relatively new technology, which has the characteristics of safe and accurate operation under direct vision, ensuring the accurate and real-time reproduction of intraoperative images. It is not susceptible to light occlusion, has no blind area, and can accurately record surgical procedures, improving the accuracy and security of the spinal surgery. Additionally, it is widely used in pedicle screw implantation [20,21,22,23,24,25]. Hahn et al. [3] implanted pedicle screws with the assistance of electromagnetic navigation technology. In their study, there were 37 (77.1%) thoracic pedicle screws with maximum cortical penetration less than 2 mm and only 9 screws with dislocation, indicating that pedicle screws placement under electromagnetic navigation is an ideal method.
Compared with other optoelectronic navigation systems, electromagnetic navigation has the advantages of accurate positioning and no intraoperative occlusion, and the continuity of operation is generally not disturbed. In addition, the advantages of electromagnetic navigation systems are listed as follows: (1) The navigation device is small in size and easy to move. A single person can complete equipment preparation and debugging, reducing the pressure of insufficient operating room space as it is easy to transfer the equipment within the operating room. (2) The entire surgical area is located in the magnetic field, and the objects that do not emit magnetic field signals are not imaged, so it is unchallenging to use during the operation. There is no need to adjust the direction of the instrument repeatedly, improving the operation efficiency and saving operation time. (3) Computer control is not manual control, improving the operation simplicity, accuracy, and stability. (4) It supports hot start, which can be closed or opened at any time, thus avoiding the influence among systems. It has no obvious impact on other equipment in the operating room, and the accuracy of the system is not affected by the various instruments found in the operating room. (5) There is no need for reference to the environment installation and commissioning, no visual field barrier encountered during operation, and is attributed to low infection rate [4].
TELD has the advantages of a bright and clear surgical field, precise discectomy, and fewer complications, albeit still with some limitations, which include as follows: (1) The 2-dimensional (2D) images under percutaneous endoscopy lack depth perception. (2) The anatomical structure under the endoscope is different from that of conventional microanatomy, and lack of experience can easily lead to localization deviation. (3) The narrow operation space and the hand-eye separated operation bring more difficulties to the surgeons. (4) Sometimes, it is difficult to stop bleeding under a microscope, and the position of endoscopy and surgical tools cannot be clearly determined because of the blurred surgical field of vision, which may warrant suspension of the operation. However, the combination of TELD and electromagnetic navigation can reduce the difficulties caused by the above conditions, and can also bring more assistance to doctors who lack surgical experience by aiding in the reduction of the learning curve.
Electromagnetic navigation-assisted percutaneous endoscopic spinal surgery has the following advantages: (1) Improving the surgical safety and accuracy of lesion resection, which are beneficial to the postoperative recovery of patients. (2) It can determine the positional relationship between intervertebral disc lesions and peripheral blood vessels and the range of decompression, effectively avoiding the damage of normal tissue. (3) It is beneficial to individualized puncture design, avoiding the key structural and functional areas in the spinal canal, and reducing surgical trauma. (4) Combined with percutaneous spinal endoscopy, it can expand surgical indications and effectively avoid trauma and complications caused by routine open surgery. However, the electromagnetic field may be affected by iron during the operation, and electromagnetic navigation cannot be used if the patient has iron objects intact. Additionally, the locator must be fixed stable during operation, and the accuracy of navigation will decrease if the locator is unstable or shifted. Therefore, in order to achieve more accurate and occlusion-free stable positioning, further studies are required. However, with the miniaturization of magnetic field transmitters and the improvement of the accuracy of automatic recognition and registration of detectors, electromagnetic navigation is expected to become one of the main gateways of spinal surgical navigation.
There are some points for attention in electromagnetic navigation-assisted TELD: (1) Surgeons and relevant technologists should be professionally trained and familiar with the operation process of a navigation system in order to reduce the operation time of establishing navigation. With the accumulation of experience and familiarity with a navigation system, the time to establish navigation configuration will be gradually shortened, generally within five to ten minutes. (2) The electromagnetic navigation sensor frame and needle positioner must be firmly fixed, generally fixed on the adjacent surgical segment spinous process. On the other hand, the depth of K-wire insertion is required to reach 2 cm, so as to avoid serious errors caused by image drift. (3) Although the direction of puncture needle and reamers and the depth of the insertion and the position of the surgical tools can be monitored in real time during the operation, surgeons should still be familiarized with the anatomical structures under the microscope and should be careful when operating around nerve roots and blood vessels so as to avoid inevitable damage. (4) Although electromagnetic navigation can largely reduce the learning curve of PELD to young surgeons, navigation itself has a steep learning curve. It is necessary to be fully familiar with the applicable specifications of navigation and accumulate the experience of 20–30 cases in order to better combine electromagnetic navigation technology with TELD and improve the efficiency of surgery.
7 Conclusions
EM-based navigation-guided TELD is an effective and safe minimally invasive technology for the treatment of various types of lumbar disc herniation. The TELD assisted by electromagnetic real-time navigation is more accurate and safer, as well as providing a reduction in X-ray radiation damage. The new technique is especially helpful for inexperienced spinal surgeons. Its application prospect for the future is broad-ranging, and EM-based navigation will further promote the development of percutaneous endoscopic spinal surgery.
Abbreviations
- PN:
-
percutaneous nucleotomy
- APLD:
-
automated percutaneous lumbar discetomy
- PELD:
-
percutaneous endoscopic lumbar discectomy
- YESS:
-
Yeung endoscopic spine system
- THESSYS:
-
Thomas Hoogland Endoscopic Spine System
- TELD:
-
transforaminal endoscopic lumbar discectomy
- EM:
-
electromagnetic
- LDH:
-
lumbar disc herniation
- 2D:
-
two-dimensional
- 3D:
-
three-dimensional
- CT:
-
computed tomography
References
Hijikata S. Percutaneous nucleotomy. A new concept technique and 12 years’ experience. Clin Orthop Relat Res. 1989;238(238):9.
Onik G, Helms CA, Ginsberg L, et al. Percutaneous lumbar diskectomy using a new aspiration probe: porcine and cadaver model. Radiology. 1985;155(1):251–2.
Hahn P, Oezdemir S, Komp M, Giannakopoulos A, Kasch R, Merk H, Liermann D, Godolias G, Ruetten S. Navigation of pedicle screws in the thoracic spine with a new electromagnetic navigation system: a human cadaver study. Biomed Res Int. 2015;2015:183586. https://doi.org/10.1155/2015/183586. PMID: 25759814; PMCID: PMC4339821.
Hausmann B, Forst R. Nucleoscope. Instrumentarium for endoscopy of the intervertebral disc space. Arch Orthop Trauma Surg. 1983;102(1):57–9.
Kambin P, NASS. Arthroscopic microdiscectomy. Spine. 2003;3(3 Suppl):60S–4S.
Yeung AT. Minimally invasive disc surgery with the yeung endoscopic spine system (YESS). Surg Technol Int. 1999;8:267–77.
Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976). 2002;27(7):722–31. https://doi.org/10.1097/00007632-200204010-00009. PMID: 11923665.
Hoogland T, Schubert M, Miklitz B, et al. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976). 2006;31(24):E890–7.
Hoogland T, van den Brekel-Dijkstra K, Schubert M, et al. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: a prospective, cohort evaluation of 262 consecutive cases. Spine (Phila Pa 1976). 2008;33(9):973–8.
Pan M, Li Q, Li S, Mao H, et al. Percutaneous endoscopic lumbar discectomy: indications and complications. Pain Physician. 2020;23(1):49–56.
Tacconi L, Baldo S, Merci G, et al. Transforaminal percutaneous endoscopic lumbar discectomy: outcome and complications in 270 cases. J Neurosurg Sci. 2018;26:531–6.
Panagiotopoulos K, Gazzeri R, Bruni A, et al. Pseudoaneurysm of a segmental lumbar artery following a full-endoscopic transforaminal lumbar discectomy: a rare approach-related complication. Acta Neurochir. 2019;161(5):907–10.
Ahn Y. Transforaminal percutaneous endoscopic lumbar discectomy: technical tips to prevent complications. Expert Rev Med Devices. 2012;9(4):361–6.
Kapetanakis S, Gkantsinikoudis N, Chaniotakis C, et al. Percutaneous transforaminal endoscopic discectomy for the treatment of lumbar disc herniation in obese patients: health-related quality of life assessment in a 2-year follow-up. World Neurosurg. 2018;113:e638–49.
Hilbert T, Boehm O, Pflugmacher R, et al. Rare complication after endoscopic discectomy. Anaesthesist. 2014;63(1):41–6.
Hsu PK, Wu YC. Electromagnetic navigation-guided one-stage dual localization of small pulmonary nodules. Chest. 2018;154(6):1462–3.
Arenberg D. Electromagnetic navigation guided bronchoscopy. Cancer Imaging. 2009;9(1):89–95.
Putzer D, Arco D, Schamberger B, et al. Comparison of two electromagnetic navigation systems for ct-guided punctures: a phantom study. Rofo. 2016;188(5):470–8.
Durand P, Moreau-Gaudry A, Silvent AS, et al. Computer assisted electromagnetic navigation improves accuracy in computed tomography guided interventions: a prospective randomized clinical trial. PLoS One. 2019;12(3):e0173751.
von Jako RA, Carrino JA, Yonemura KS, et al. Electromagnetic navigation for percutaneous guide-wire insertion: accuracy and efficiency compared to conventional fluoroscopic guidance. NeuroImage. 2009;47(Suppl 2):T127–32.
von Jako R, Finn MA, Yonemura KS, et al. Minimally invasive percutaneous transpedicular screw fixation: increased accuracy and reduced radiation exposure by means of a novel electromagnetic navigation system. Acta Neurochir. 2011;153(3):589–96.
Allison RR. The electromagnetic spectrum: current and future applications in oncology. uture. Oncologia. 2013;9(5):657–67.
Mehta AC, Hood KL, Schwarz Y, et al. The evolutional history of electromagnetic navigation bronchoscopy: state of the art. Chest. 2018;154(4):935–47.
Komune N, Matsushima K, Matsuo S, et al. The accuracy of an electromagnetic navigation system in lateral skull base approaches. Laryngoscope. 2017;127(2):450–9.
Cai K, Yang R, Lin Q, et al. Near-infrared camera calibration for optical surgical navigation. J Med Syst. 2016;40(3):67.
Diana M, Soler L, Agnus V, et al. Prospective evaluation of precision multimodal gallbladder surgery navigation: virtual reality, near-infrared fluorescence, and X-ray-based intraoperative cholangiography. Ann Surg. 2017;266(5):890–7.
Kapoor R, Ramasamy S, Gardi A, et al. Acoustic sensors for air and surface navigation applications. Sensors (Basel). 2018;18(2):499.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Chen, BL., Lin, YP., Rao, SY. (2022). EM-Based Navigation-Guided Transforaminal Endoscopic Lumbar Discectomy. In: Kim, JS., Härtl, R., Wang, M.Y., Elmi-Terander, A. (eds) Technical Advances in Minimally Invasive Spine Surgery. Springer, Singapore. https://doi.org/10.1007/978-981-19-0175-1_12
Download citation
DOI: https://doi.org/10.1007/978-981-19-0175-1_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-0174-4
Online ISBN: 978-981-19-0175-1
eBook Packages: MedicineMedicine (R0)