Abstract
Full-endoscopic transforaminal lumbar discectomy is based on a puncture technique using a guide needle to reach the target area of the foramen via a percutaneous posterolateral/lateral approach. It may correlate with specific approach-related complications, as exiting nerve root injury. We report the first case of pseudoaneurysm of the lumbar segmental artery secondary to a transforaminal full-endoscopic surgery in the treatment of a lumbar herniated disc. A 39-year-old man underwent left L4-L5 full-endoscopic transforaminal lumbar discectomy for a herniated disc. Three hours after surgery, he experienced acute progressive abdominal pain. An abdomen CT scan showed contrast extravasation in the left paraspinal compartment at L4 vertebral body level. The selective left lumbar angiogram revealed a pseudoaneurysm of a side branch of the left lumbar segmental artery, which was treated by endovascular coiling. The patient made a rapid postoperative recovery without further complications and was discharged 4 days later. This report identifies a rare complication of transforaminal full-endoscopic surgery in the treatment of a herniated lumbar disc. To our knowledge this is the first case of pseudoaneurysm formation of the lumbar artery following a full-endoscopic transforaminal lumbar discectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, the full-endoscopic transforaminal lumbar discectomy (FETD) has been considered as a safe and effective alternative to standard microsurgical procedures for the treatment of lumbar herniated discs and other disorders [3, 11, 14, 20]. FETD differs significantly from traditional microdiscectomy as it is a pure percutaneous posterior-lateral or lateral approach to the foraminal area and it is related to a steep learning curve [9, 16]. The latter mainly correlates with the blind puncture technique which distinguishes the initial phase of the procedure and thus with the specific approach-related complications including exiting nerve root injury or visceral injury [1, 5, 10,11,12].
We report the occurrence of a pseudoaneurysm of a segmental lumbar artery secondary to a full-endoscopic transforaminal L4-L5 discectomy procedure, and we discuss the mechanism of such a rare approach-related complication.
Case report
A 39-year-old man presented with 3-month history of left leg pain, refractory to conservative treatment. Lumbar spine magnetic resonance imaging (MRI) demonstrated a left paramedian extruded herniated disc at L4-L5 level. A left L4-L5 FETD was performed, according to the technique described by Ruetten et al. [15].
The patient was placed in prone position under general anesthesia. The skin incision was placed approximately 10 cm from the midline, on a transverse line bisecting the disc in anterior-posterior fluoroscopic view. A spine needle was inserted posteriorly-laterally and advanced under fluoroscopic guidance until the level of the dorsal annulus, pointing to the left L4-L5 foramen. A guidewire and a cannulated dilator were inserted, entering the foraminal area. Next, a surgical sheath was placed, and through this, the endoscope was inserted and an uneventful full-endoscopic herniectomy was performed under direct visualization.
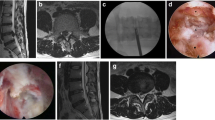
Immediately after surgery, the patient’s radicular symptoms improved, but about 3 h later, he complained of acute progressive left flank abdominal pain. Emergency laboratory examinations and blood pressure were normal, but an abdominal emergency CT scan showed an active circumscribed contrast extravasation in the left paraspinal compartment at L4 vertebral body level (Fig. 1). Thus, an emergency selective left lumbar angiogram was performed revealing a pseudoaneurysm of a side branch of the left lumbar segmental artery (Fig. 2), which was completely embolized by endovascular coiling (Fig. 3). The patient was discharged 4 days later free of complaints.
Discussion
FETD shares several complications with the microdiscectomy procedure, including nerve root injury, incidental durotomy, surgical site infection, cauda equine syndrome, and hematoma [17]. Yet, specific features render FETD a completely different surgical procedure from the standard microdiskectomy. FETD requires a guide needle to reach the target area of the foramen via a percutaneous posterior-lateral or lateral approach [15, 21]. The blind puncture technique needed in this step remains essential for a straight-through procedure and is carried out on a repeated trial-and-error manner under continuous fluoroscopy [1, 8]. As long as puncture targeting remains inaccurate, additional puncture attempts are necessary, increasing the risk of injuring normal tissues [7]. Specific surgery-related complications may occur, including exiting nerve root injury by puncturing, heat transmission by bipolar or mechanical compression from the cannula or surgical tools, and visceral injury [1, 5, 10, 17].
The occurrence of serious vascular injuries in FETD is very rare [17]. Ahn et al. [2] first reported four cases of retroperitoneal hematoma following FETD in a series of 412 patients. As in our patient, in all cases, an initial symptom was a flank/inguinal pain right after a few hours of pain-free interval following surgery. The mechanism of this complication suggested by the authors focused to the initial blind puncture technique toward the foraminal area and its anatomy. In this anatomical area, the segmental lumbar artery and its branches run toward their corresponding foramen. These vessels may be injured during puncturing if the tip of the needle is placed too anteriorly. Among the four cases of retroperitoneal hematomas, two patients presented a diffuse type of hematoma and required open hematoma evacuation. The remaining two patients presented localized type of retroperitoneal hematomas and were managed conservatively. An additional case of a paravertebral hematoma treated conservatively was reported by Chae et al. [4] in a published series of 153 patients treated with FETD, but no further details were given.
We report the first case of pseudoaneurysm of the lumbar segmental artery secondary to a transforaminal full-endoscopic surgery in the treatment of a lumbar herniated disc. In our case, the vascular injury, likely originated by a combination of a needle penetration and direct trauma of the vessel toward the lateral wall of the vertebra, resulted in a lumbar arterial branch pseudoaneurysm, which was treated with endovascular coiling [13]. The clinical manifestations of lumbar artery injury may vary considerably, oscillating from asymptomatic to hemorrhagic shock requiring surgical or endovascular repair [2, 6, 15, 18]. Delayed rupture is also reported with initial formation of pseudoaneurysm complicated by secondary bleeding [19]. Endovascular embolization of lumbar artery pseudoaneurysm may be effective in controlling hemorrhage, and it can be performed in an emergency setting if needed [18].
Adequate technical skill acquisition is mandatory to minimize approach-related complications performing full-endoscopic surgery. Live surgery attendance, hands-on cadaver labs, and strict adherence to well-described step-by-step technical tips outline the ways to handle with the demanding learning curve [12, 16].
Conclusion
We present a unique case of pseudoaneurysm of a segmental lumbar artery secondary to a full-endoscopic transforaminal L4-L5 discectomy procedure. FETD has a steep learning curve that requires caution and experience, especially for those unfamiliar with percutaneous techniques. It may be associated with specific complications related to the blind puncture technique with the guide needle, including exiting nerve root injury and visceral and segmental lumbar artery injury. The latter is extremely rare but potentially risky and spinal endoscopic surgeons should be aware of that.
References
Ahn Y (2012) Transforaminal percutaneous endoscopic lumbar discectomy: technical tips to prevent complications. Expert Rev Med Devices 9:361–366
Ahn Y, Kim JK, Lee BH et al (2009) Postoperative retroperitoneal hematoma following transforaminal percutaneous endoscopic lumbar discectomy. J Neurosurg Spine 10:595–602
Birkenmaier C, Komp M, Leu HF, Wegener B, Ruetten S (2013) The current state of endoscopic disc surgery: review of controlled studies comparing full-endoscopic procedures for disc herniations to standard procedures. Pain Physician 16:335–344
Chae KH, Ju CIJ, Lee SM, Kim BW, Kim SY, Kim HS (2009) Strategies for noncontained lumbar disc herniation by an endoscopic approach: transforaminal suprapedicular approach, semi-rigid flexible curved probe, and 3-dimensional reconstruction CT with discogram. J Korean Neurosurg Soc 46:312–316
Choi I, Ahn J-O, So W-S, Lee S-j, Choi I-J, Kim H (2013) Exiting root injury in transforaminal endoscopic discectomy: preoperative image considerations for safety. Eur Spine J 22:2481–2487
Dausse F, Chevallier P, Motamedi JP, Amoretti N, Cua E, Bruneton JN (2006) Lumbar false aneurysms following image-guided interventive procedures for spondylodiskitic abscesses. Skelet Radiol 35:949–952
Fan G, Guan X, Zhang H et al (2015) Significant improvement of puncture accuracy and fluoroscopy reduction in percutaneous transforaminal endoscopic discectomy with novel lumbar location system. Preliminary report of prospective hello study. Medicine (Baltimore) 94:e2189. https://doi.org/10.1097/MD.0000000000002189
Fan G, Gu X, Liu Y et al (2016) Lower learning difficulty and fluoroscopy reduction of transforaminal percutaneous endoscopic lumbar discectomy with an accurate preoperative location method. Pain Physician 19:E1123–E1134
Hsu H-T, Chang S-J, Yang SS, Chai CL (2013) Learning curve of full-endoscopic lumbar discectomy. Eur Spine J 22:727–733
Kim M-J, Lee S-H, Jung E-S et al (2007) Targeted percutaneous transforaminal endoscopic diskectomy in 295 patients: comparison with results of microscopic diskectomy. Surg Neurol 68:623–631
Lewandrowski K-U (2014) “Outside-in” technique, clinical results, and indications with transforaminal lumbar endoscopic surgery: a retrospective study on 220 patients on applied radiographic classification of foraminal spinal stenosis. Int J Spine Surg 1:8. https://doi.org/10.14444/1026
Nellensteijn J, Ostelo R, Bartels R, Peul W, van Royen B, van Tulder M (2010) Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: a systematic review of the literature. Eur Spine J 19:181–204
Puri AS, Colen RR, Reddy AS et al (2011) Lumbar artery pseudoaneurysm after percutaneous vertebroplasty: a unique vascular complication. Report of 2 cases. J Neurosurg Spine 14:296–299
Ruetten S, Komp M, Godolias G (2005) An extreme lateral access for the surgery of lumbar disc herniation inside the spinal canal using the full-endoscopic uniportal transforaminal approach. Technique and prospective results of 463 patients. Spine 30:2570–2578
Ruetten S, Komp M, Merk H, Godolias G (2007) Use of newly developed instruments and endoscopes: full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine 6:521–530
Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine 33:931–939
Sairyo K, Matsuura T, Higashino K et al (2014) Surgery related complications in percutaneous endoscopic lumbar discectomy under local anesthesia. J Med Investig 61:264–269
Santillan A, Patsalides A, Gobin YP (2010) Endovascular embolization of iatrogenic lumbar artery pseudoaneurysm following extreme lateral interbody fusion (XLIF). Vasc Endovasc Surg 44:601–603
Siablis D, Panagopoulos C, Karamessini M et al (2003) Delayed diagnosis of a false aneurysm after lumbar arterial injury: treatment with endovascular embolization: a case report. Spine 28:E71–E73
Tsou PM, Yeung AT (2002) Transforaminal endoscopic decompression for radiculopathy secondary to intracanal noncontained lumbar disc herniations: outcome and technique. Spine J 2:41–48
Ying J, Huang K, Zhu M et al (2016) The effect and feasibility study of transforaminal percutaneous endoscopic lumbar discectomy via superior border of inferior pedicle approach for down-migrated intracanal disc herniations. Medicine (Baltimore) 95:e2899. https://doi.org/10.1097/MD.0000000000002899
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (San Giovanni Addolorata Ethical Committee) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Patient consent
The patient has consented to the submission of the case report for submission to the journal.
Additional information
Comments
Full-endoscopic procedures are advocated for their minimal invasive nature and most proponents claim complication rates close to zero. While potential advantages like less scaring have not yet been properly evaluated, others have attributed problems like approach-related neuropathic pain to the transforaminal endoscopic route.
This interesting case report adds to the discussion of the pros and cons of full-endoscopic disc surgery in comparison with microscopic procedures reminding us of the difference in possible severe complications of lateral endoscopic procedures with blind access to the site of action.
Claudius Thomé
Innsbruck, Austria
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine degenerative
Rights and permissions
About this article
Cite this article
Panagiotopoulos, K., Gazzeri, R., Bruni, A. et al. Pseudoaneurysm of a segmental lumbar artery following a full-endoscopic transforaminal lumbar discectomy: a rare approach-related complication. Acta Neurochir 161, 907–910 (2019). https://doi.org/10.1007/s00701-019-03876-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-03876-7