Abstract
Flow Diversion is one of the relevant technical improvements of the past decade in the endovascular treatment of cerebral aneurysms. When the efficacy and safety of a recent tool allow treating challenging aneurysms, this adoption in daily practice is fast even if the benefit of use is incompletely shown. We will review studies of these stents called “Flow Diverters” (FD) in animal models and in clinical use, mainly to discuss the technical characteristics inherent to its endovascular prostheses, which determine the choice and the manner in which this medical device can be used. During the chapter we will come back to this choice depending on the type of intracranial aneurysm to be treated, supported by the literature and illustrations of a series of personal cases, also resuming the management of complications in the presence of these devices, antiplatelet treatments as well as retreatment possibilities.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
9.1 Introduction
Endovascular treatment of cerebral aneurysms is the treatment of choice for ruptured intracranial aneurysms [1]. The invention of detachable coils in the early 1990s is largely responsible for the success of endovascular treatment and its adoption by the majority of neuroendovascular operators [2]. However, large, fusiform, or wide-necked aneurysms are more difficult to treat with simple coiling and required, when possible, recourse to a “de-constructive” approach with occlusion of the parent vessel [3]. The more advanced techniques of stent-assisted coiling or balloon remodeling were until recently alternative approaches to simple coiling in the management of some of these aneurysms [4]. However, numerous studies have shown the limitations of coiling approaches, with or without stenting, particularly in large and wide-necked aneurysms, with significant recanalization rates [5].
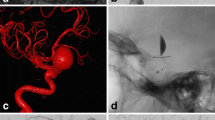
Flow diversion is a unique, innovative endovascular approach. It consists of treating the aneurysm-parent artery, rather than packing the aneurysmal sac with embolization materials. Flow diversion has been used for about 15 years. Initially designed for large side-wall aneurysms, its use by operators has been widely diversified without high-grade recommendations linked to robust scientific evidence on the scope of Flow Diverter (FD) indications. The flow diverter technique (Fig. 9.1) can be used alone or in combination with other endovascular tools such as coils and stents.
The FRED and FRED Jr. flow diversion devices (MicroVention, Aliso Viejo, California, USA) feature a unique dual-layer construction designed to achieve excellent vessel wall apposition, which fosters neointimal growth and long-term aneurysm occlusion. The FRED Jr. device is the first flow diverter that can be delivered using a 0.021″ microcatheter for safe delivery in distal locations. Both devices may be used with or without embolic coils
The Flow Diverter, because of its low porosity, creates intra-aneurysmal hemodynamic changes, with blood stagnation and occlusion of the aneurysm, while most often keeping the arteries whose origins are covered by the FD permeable [6]. At the level of the aneurysm, blood stagnation is followed by thrombosis, inflammation, and thrombus organization, whereas at the level of the treated artery, the FD is covered by a neointimal formation that will eventually lead to healing [7].
Proposing such a tool for aneurysm treatment can only be done responsibly by exploring the chances of success and the expected or potential risks in a variety of preclinical studies; studies of the properties of the tool, flow studies, animal studies, etc., that will lead to a better discernment of this technique: its functioning, its limits, its potential complications, and therefore its indications.
9.2 Study of the FD Characteristics
9.2.1 Flow Diverters: Braided and Low Porosity Stents
FDs differ from previously used stents in their design. Conventional stents were most often constructed by laser cutting a hollow metal tube (hypo tube). FDs are formed by braiding so-called “super elastic” woven wires together, forming a mesh.
The wires forming the FD can slide over each other (Fig. 9.2), which gives it a high conformability, i.e., adaptation to the geometry of the vessel [8]. This braided construction constrains the implant and allows it to pass through the microcatheter before expanding upon exit (Fig. 9.1).
Porosity, FD, and non-FD stents. Stent A is an FD, its porosity is lower. Stent B is also a braided stent but is not an FD. A braided stent is able to deform and open a unit cell in a very important way. Here the FD enters through a unit cell of the non-FD stent without being constrained. Courtesy of J. Raymond – I. Salazkin – A. Makoyeva (Montréal)
There are a growing number of different FDs. Some are approved by the Food and Drugs Administration in the USA (PED, SURPASS). Others have obtained the CE mark (SILK, FRED, P64, DERIVO), and others are used in Asia (TUBRIDGE, FLOW WISE). All these products are grouped under the term “Flow diverters” but they have a large number of technical differences.
In addition to design differences, FDs differ from conventional stents in their porosity. Not all braided stents are considered FDs (LVIS stents and LEO stents are porous braided stents, but have little flow diversion capacity). There is no quantifiable definition that differentiates a braided stent from an FD. However, it is accepted that an FD is a low-porosity stent, unlike non-FD braided stents. For example, it is almost impossible to pass a microcatheter through the mesh of an FD, whereas this strategy is possible (and conventional) when using other stents. The surface area of a unit cell is approximately 1–1.5 mm2 for non-FD braided stents such as LVIS and LEO, whereas this surface area is 0.05 mm2 for FDs.
9.2.2 Porosity
Porosity is calculated by the below Formula (9.1), developed to understand the different technical characteristics influencing the porosity (9.2 and 9.3) with N = Number of wires, d = Wire diameter (section), B = Wire length to make a complete turn (no braiding), α = Angle between the wires in the long axis of the stent.
The porosity value of an implanted FD is different from non-implanted unconstrained ones. Its porosity changes according to the external constraints imposed by the local hemodynamic environment (curvatures of the artery, length of the aneurysmal neck, etc.).
The nominal porosity of stents is partly existent in the literature, but most of the time it is mentioned by the manufacturers without details of the measurement conditions [9]. It varies according to the devices between 45% and 85%; this porosity corresponds to the non-metallic proportion of the surface of the FD deployed at its nominal diameter.
The compaction imposed or not by the operator during deployment, the choice of FD diameter and its relationship with the diameter of the recipient arterial segment are all factors that also modify the porosity of the implant in place.
Pore size (unit cell) is also not a clearly detailed data by the manufacturers. Some give the surface of the unit cell at the nominal diameter. For example, it is 0.02–0.05 mm2 for PED and 0.04–0.05 mm2 for TUBRIDGE.19,20 Others give the major axis of the unit cell, which would be between 110 and 250 μm for SILK or 300–350 μm for DERIVO.17,21 To give an element of comparison, the size of the cells of LEO BABY is 1 mm of major axis and those of LVIS JR is 1.5 mm. Moreover, the data from the literature and those from the industry are not always comparable. There is a perpetual advance in technology in the FD industry. Dandapat et al. recently reviewed current flow diversion technology and clinical use [10].
To understand the adaptation of the FD to its container, an experiment consists in placing an FD in several transparent tubes of increasing size. A change in the shape and orientation of the unit cells is then observed. If the FD is oversized, the unit cell takes on the shape of a rhombus that has its largest diagonal in the axis of the vessel. The unit cell changes its shape to a square when the FD is less oversized relative to its container. Then, when the FD is undersized relative to its container, the unit cell takes the shape of a rhombus with its long axis perpendicular to the long axis of the vessel. The porosity is weaker, the closer the shape of the unit cell is to a square. The more rhombic the unit cell, the greater the porosity, regardless of the direction of the rhombus (Fig. 9.3). The alpha angle is the angle of the unit cell in the axis of the FD. Thus, the closer the alpha angle is to 90°, the lower the porosity, which can reach a minimum of 20%. When the alpha angle is less than 30° (as when the FD is compressed in the microcatheter) or greater than 150°; porosity increases significantly [11,12,13].
The porosity of an FD will always be less at the concavity of the curve than at the convexity (Fig. 9.4). On the other hand, it is relatively constant at the lateral faces [14]. It should be noted that oversizing the FD increases its porosity at the constrained segment but not at the unconstrained segment (aneurysm neck), where it naturally regains its size. This phenomenon gives the appearance of spindle-shaped dilation of the middle portion of the FD [15].
Porosity has been individualized as a parameter influencing flow reduction within the aneurysm [16]. In vitro work comparing the effect on flow reduction of high-porosity stents and DFs unequivocally concludes that there is a stronger effect of the FD, when compared with multiple telescopically nested non-FD stents [17].
Implantation of multiple FDs is sometimes proposed in certain clinical indications in case of ineffectiveness of a first implanted FD (Fig. 9.5). This strategy is also used to treat an aneurysm in cases where anatomic constraints require it. For example, if there is a significant difference in caliber between the distal and proximal anchor zones, different sized FDs can be implanted [18]. However, the porosity resulting from multiple FD assemblies is more difficult to anticipate. For example, a 3.75-mm diameter PED placed in a 3.5-mm tube has an estimated porosity of 78%, but the placement of a second PED of the same size does not necessarily increase porosity significantly [19]. Indeed, layering can be done in a variable manner, thus affecting porosity.
Case of a 50 years-old patient with right P2-P3 junction unruptured aneurysm (a). First treatment was done with a single PED (b). Control angiogram (c) denoted a persistent patency of the aneurysm at 6 months. Second treatment was done with a same-sized PED at 9 months (results in d). Successive control angiograms at 15 months (e) and 21 months (f) showed the progressive interruption of flux within the aneurysm, it also permits to appreciate the stent-in-stent construction
In the case of a stent-in stent, the wires can be placed exactly the same way or they can be placed in the free metal gaps. This arrangement is random, thus the porosity values obtained have wide confidence intervals. As a result, Shapiro et al. advise oversizing the second implanted FD. For example, they suggest placing a second 4.25 mm FD within a first 3.25 mm diameter FD to achieve 60–65% porosity more consistently.
9.2.3 Pore Density
Pore density is a different entity from porosity. It represents the number of pores (unit cells) per unit area (Fig. 9.5). Sadasivan et al. state that pore density is the most important parameter for judging the effectiveness of FDs [20]. Pore density (PD) is calculated by the formula previously shown in [3].
Thus, the greater the number of wires and the shorter the length of wire needed to go around the FD, the greater the pore density. The pore density varies between 12 and 32 pores per mm2. The pore densities of some FDs are as follows; SURPASS 21–32 pores/mm2, SILK 12 pores/mm2, and PED 15–22 pores/mm2. For comparison, a WALL STENT used in the stenting of atheromatous carotid stenosis has a pore density of 0.2 pores/mm2 [21].
9.2.4 Composition
As previously said, considering a perpetual evolution of the FD stents technology, the following details are only given as examples, to image characteristics that can vary and be considered when implanting FD.
The PED is composed of 48 wires with the same gauge for all strands (30 μm) [18]. The SILK has 44 strands of 25 μm gauge and 4 radiopaque wires of 40 μm gauge [14]. The p64 is composed of 64 strands and the TUBRIDGE of 62 strands. The DERIVO has wires of different calibers ranging from 35 (n = 44) to 85 μm (n = 4) [22]. Regarding the SURPASS and TUBRIDGE, the number of wires increases with the diameter of the implant, reaching 96 wires for a 5-mm-diameter implant for the SURPASS and 62 wires if the diameter of the FD is >3.5 mm for the TUBRIDGE. The FRED is a stent-in-stent system with 16 wires on the outer stent and 48 wires on the inner stent [23].
The diameter of the wires and the number of strands influence: friction within the microcatheter, radial force within the artery, and coverage of the perforating arteries. Indeed, the diameter of the ostium of the latter oscillates between 100 μm and 1 mm [20].
The wires used to braid FDs can be made of Nitinol (i.e., SILK, FRED, TUBRIDGE, p64, DERIVO) or cobalt-chromium (PED, SURPASS). Nitinol (Nickel-Titanium) has less radial strength but is easy to handle and has the advantage of excellent shape memory. It is also less radiopaque than cobalt chrome and requires the addition of markers or platinum ‘coils’ for better visibility. Dandapat et al. recall that Cobalt/chromium adds stiffness and radial force while nitinol brings flexibility and easy navigation and deployment, and that Cobalt/chromium implants allow a better answer to ballooning when an incomplete wall apposition is observed [10].
The value of the radial force is difficult to find in the literature but would be more than 1.5 times higher in the case of PED compared to SILK [24]. These data, although rarely reported, may make sense in clinical practice. Indeed, too low a radial force could be the cause of poor opening of the FD in cases where there is an external constraint, such as a pre-aneurysmal stenosis or spasm of the artery.
Alternatively, decreasing porosity by maintaining or increasing pore density increases the amount of metal in the implant. The more metal an FD contains, the more flexible it becomes and the more difficult it is to navigate. The more support the FD needs, the more friction it experiences when navigating the microcatheter, which requires larger diameter microcatheters.
The choice of the FD might govern the microcatheter (diameter) needed for implantation. The latter will obviously define the navigability of the set, and sometimes the feasibility of the procedure (Figs. 9.6 and 9.7).
Patient of 60 years old with a giant unruptured aneurysm of the left carotid siphon (a). Anchoring technic was used to pass through the distal neck of the aneurysm, which was impossible to navigate directly or using two microwires, because of the angioarchitecture and the misfit between the wire and the microcatheter diameters (b, c). A tutor-stent was initially placed (Leo) (d) to perform coiling with jailing technic. A PED was finally placed in the first stent (e). Control angiogram at 6 months showed good results (f)
Flow diverter stent-assisted coiling. The microcatheter is jailed during the deployment of the FD (a–c) and the coiling is done after a partial or total placement. The required set-up to perform this kind of procedure is obviously linked to the microcatheter (the one which will deploy the FD) diameter
These catheters can nowadays have a diameter of 0.017″ (Silk Vista Baby, 48 wires Nitinol stent with platinum DFT technology), 0.021″ (SILK, p48, Fred Jr), 0.027″ (PED, Survpass Evolve, Fred, p64, Derivo 2nd generation), and 0.025″ to 0.040″ (Silk+, Turbridge, Surpass streamline).
Friction problems also increase with stent length but can be improved by surface treatments. An FD that is too rigid can be difficult to navigate, requiring more seating downstream of the aneurysm, and thus taking more risks in the distal delivery area in particular. 48-wire nitinol FDs have the advantage of easy distal placement (e.g., SILK and in particular Silk vista baby, FRED).
The “stent-in-stent” construction of FRED allows for fewer contact points between the FD and the inner wall of the microcatheter, similar to the wooden logs that were used to roll the limestone blocks during the construction of the pyramids.
FDs are self-expanding stents, and their apposition to the vessel walls is done slowly and sequentially by the operator [25]. However, these stents are not all braided in the same way, and the varying braiding “pitch” characterized by different Alpha and Beta angles. The Alpha angle represents the angle of wire crossing in the long axis of the stent, and the Beta angle represents the angle of wire crossing in the short axis of the stent. These angles change depending on the curve made by the FD, as well as its degree of compaction (Fig. 9.6) [14].
Between the constrained zone affixed to the walls of the portal artery and the “free” stent (Free Segment of Stent = FSS) located in front of the aneurysm neck exist two transitional zones (TZ) [26]. These transitional zones, reported in the literature, are described as two incompressible zones, where porosity is higher than at the level of the compaction (central) zone (Fig. 9.8) [27]. Knowledge of these transitional zones is important for the clinician when using an FD to treat a wide-neck aneurysm [28]. The transition zone will be more porous the larger the size of the FD compared with the diameter of the artery [27]. Thus, the tendency is to recommend the use of an FD that is slightly larger than the diameter of the artery in order to ensure the stability of the FD and to decrease the risk of migration.
(a) Photograph of a PED inserted in two hollow tubes. We individualize the free segment of the stent which is the portion of the FD without constraint composed of a compaction area and two transition zones (TZ). (b) Photograph of an FD inserted in a glass tube to emphasize TZ. Courtesy of J. Raymond – I. Salazkin – A. Makoyeva (Montréal)
Some precautions can be considered in order to minimize the importance of transition zones. The first is to avoid oversizing the FD. Another strategy is to first place a non-FD stent at the neck of the aneurysm, and to deploy the DF within this first stent, which then acts as a stent, and allows to avoid fusiform dilation of the FD placed within it (Figs. 9.5 and 9.9). This strategy is sometimes useful in the presence of very large collars or fusiform aneurysms. It should be noted that the FRED device is a stent-in-stent, with a 16-wire braided outer stent and a 48-wire inner stent. Despite this, fusiform dilatation of the entire device remains possible as observed in some works [15]. Other authors, mainly PED users, advise the placement of several FDs to avoid this phenomenon. A first FD, with a smaller diameter, is placed downstream, and then a larger diameter FD is inserted within it and deployed to the proximal anchoring zone [19].
(a). Clinical case illustrating the deployment of a non-FD stent prior to the implantation of 2 FD (SILKS). Courtesy of J. Raymond (Montréal). (b) Photographs showing the importance of a 6–7 mm anchoring zone to avoid stenosis of the FD tip. Courtesy of J. Raymond – I. Salazkin – A. Makoyeva (Montréal)
9.2.5 Choice
Particle velocimetry data show that the closer the nominal diameter of the DF is to that of the artery, the greater the effectiveness [17]. However, the choice of DF diameter depends on multiple factors, including mainly habits, the operator’s deployment technique, and measurements made during the procedure, which are aimed at choosing the right FD to be placed in the right place. The choice of the diameter is an important step in the implantation process and different techniques exist depending on the operator. The most common is to take into account only the proximal diameter (most often the largest), but some operators sum the distal and proximal diameters to make an average. It should be noted that the risk of migration is greater, the smaller the FD compared to the diameter of the artery. Some authors have described cases of migration following the shortening of SILK and PED [29, 30]. For some FDs, the unconstrained diameter (when deployed in the open) is greater than the diameter under which they are labeled (e.g., +0.25 mm for PED, and +0.3 mm for p64) [31].
Proximal misapposition of the FD causes significant changes in flow within the aneurysm after implantation. Indeed, the work of Rayepalli et al. shows that poor proximal apposition leads to a reversal of the direction of flow in the aneurysm, which then enters preferentially through the proximal collar in a direct manner and then exits through the FD [32]. Incomplete apposition may also be a source of thromboembolic events, as shown for some stents [33].
The PED is 2–3 times longer when constrained in the microcatheter compared to its nominal diameter length. This translates into a percentage shortening of 50–66% during deployment. Knowledge of this fact is particularly important in fusiform aneurysms, in which the DF takes on its nominal size because it is not constrained, thus responsible for a significant shortening, which is potentially difficult to predict [24].
9.2.6 Implantation
All of these FDs are available in a wide range of diameters and lengths, and are implanted via microcatheters with internal lumens ranging from 0.017 to 0.040″. The newer FDs can be recaptured after partial implantation [34]. The ability to recapture is a definite addition to the safety of these procedures, as the operator can attempt to avoid unwanted branch coverings, but can also use multiple attempts to anchor the FD, both anteriorly and posteriorly, in order to avoid its tilting in the aneurysm.
Operators use the “Pull and Push” technique to alternately apply pressure to the microcatheter to allow the implant to open and then relax the system to affix the FD in the bends [25]. However, all situations require adaptation. For example, in the case of cavernous aneurysms, because of the absence of major functional arterial branches, maximum compaction is sought. On the other hand, if a functional arterial branch needs to be covered during placement of a DF, the surgeon may decide to increase the porosity of the FD in front of it by decreasing the compaction and/or by oversizing the diameter of the implant used [18] (Fig. 9.10).
65 years old female that presented with chronic headaches and asthenia revealing a giant unruptured partially thrombosed right Sylvian aneurysm (a, b). After a coiling session (c), a PED FD was placed covering the Sylvian bifurcation. From (d–g) the placement of the FD with a low push at the neck. Control angiogram at 6 months showed a full occlusion (h), note the occlusion of the inferior Sylvian branch covered by the stent, the patient was asymptomatic
9.2.7 Surface Treatment
Because of the many links between coagulation pathways, inflammatory reactions, and cell proliferation in the vessel wall, high biocompatibility of FDs is necessary to avoid intra-stent thrombosis [4, 35, 36]. Teams have evaluated the thrombogenicity of Nitinol stents. They have compared bare Nitinol stents with stents that are coated with heparin or albumin and showed that coating these stents with albumin or heparin reduced their thrombogenicity [37]. Most FDs undergo polishing. Others offer a surface treatment that may reduce friction (DERIVO) or increase the biocompatibility of the implant. The developers of the PED FLEX have developed a new surface modification with the “SHIELD” technology. This technology is based on phosphorylated choline (PC), abundant on the surface of red blood cells. This technique, known for more than 10 years, allows the PED FLEX SHIELD to be coated with a layer of less than 3 nm, which mimics the cell membrane. Platelet activation and thrombosis phenomena are decreased by PC-coated stents in animal peripheral arteries [38,39,40]. Girdhar et al. showed that SHIELD FLEX PED was less thrombogenic (in vitro experiment with quantification of thrombin formation) than other FDs [41]. They also show that its “degree of thrombogenicity” was more similar to a SOLITAIRE AB stent, which has only 5–8% metal coverage. Manning et al. reported the use of a simple antiplatelet therapy in settings of hemorrhagic presentations [42]. Even if further prospective investigation is needed, this knowledge may be important in case of hemorrhagic presentations (Fig. 9.11) or following hemorrhagic complications.
A 43 years old patient presented with mFisher IV SAH (a), CTA was considered normal and contrast-enhanced MRI showed a gadolinium uptake within an addition image of the dorsal wall of the right internal carotid artery (b). Angiogram confirmed the presence of a highly suspected blood blister-like aneurysm (c). 2 PED-Shield were placed in a stent-in-stent fashion, to cover the latter abnormality (d). Control angiogram at 6 months showed no more parietal aneurysm (e)
9.2.8 Extremities
Flares are modifications of the distal ends of stents (Fig. 9.12). The flared ends can be related to real Flares of significant size. In these cases, markers (e.g., FRED) are added to these Nitinol arms. The flared ends can be less marked and only represent a continuity of the FD mesh (ex: SILK, DERIVO). Their main role is to facilitate the anchoring of the stent ends. However, true Flares raise concerns about thrombogenicity and distal opening, with a tendency to distal stenosis when placed in smaller caliber arteries, sometimes amplifying the “fish-mouth” phenomenon. These Flares can also complicate secondary catheterization of FDs during retreatment or during placement of a second FD inside the first. The concern then is to ensure that the FD never exits the lumen of the FD during catheterization, to avoid deployment of the second FD between the artery wall and the first [43].
9.2.9 In Vitro Studies
Preclinical in vitro studies are also making progress in the attempt to understand the mechanisms leading to ischemic and hemorrhagic complications. Thus, intra-aneurysmal pressure following FD placement has been studied. To explain delayed ruptures, hypotheses of increased intra-aneurysmal pressure or surface pressure have been put forward. Experiments have shown that the placement of an FD opposite to the aneurysm neck did not modify the pressure in a durable way. In fact, the pressure simply decreased transiently during the placement of the FD to regain a normal pressure shortly afterward. These data initially obtained on bench work were later confirmed by computer-assisted flow studies, but also by data collected on humans [17, 44, 45]. Another concern of the operator is the occlusion of functional arterial branches covered by the FD. Roszelle et al. showed by particle velocimetry study that flow could be decreased by 32.7–46.5% in such a branch covered by a single PED [46].
9.2.10 Computational Fluid Dynamic Studies
It is difficult to talk about flow diversion without mentioning flow studies. In fluid mechanics, the Navier–Stokes equations are nonlinear partial differential equations that are supposed to describe the motion of “Newtonian” fluids (ordinary viscous liquids and gases) in the continuous media approximation. Blood is treated as a Newtonian fluid, with a specified density and viscosity. The blood is assumed to be laminar at the inlet and outlet, with constant and incompressible flow. This flow is calculated from a Doppler or MRI phase-contrast examination, under static and pulsatile conditions, with synchronization to the heart rate. The fluid/structure interaction is thus simulated. These simulations are then generated by a software. Classically, the model generates an inflow and an outflow separated by a helical flow called a vortex [47]. It is worth noting that all the assumptions below have many limitations [48].
Authors have characterized intra-aneurysmal flows using, in particular, the complexity and stability of the flows during the cardiac cycle. The concentration of the inflow and the size of the area receiving the inflow (− or +50% of the area) have also been studied. Cebral et al. showed that in ruptured aneurysms, there was more likely to be angulation of the inflow and numerous recirculation zones [47, 49, 50]. They also reported that complex recirculation flow, concentrated inflow, and a small inflow landing area were risk factors for rupture.
These simulations allow for the quantification of variables of interest; Wall Shear Stress (WSS), pressure, relative residence time (RRT), inflow velocity, inflow volume, oscillatory shear index OSI… The RRT being a reflection of the time of blood contact with the inner surface of the aneurysm. Unfortunately, although flow studies generate a large amount of data, the indexes or variables produced are still subject to speculation.
Therefore, we will focus on the concepts that are most commonly recognized and in particular the WSS. WSS is a shear force that can be described as a tangential friction force between the aneurysm wall and the blood, related to the viscosity of the blood [51]. It can be expressed in terms of maximum or average stress. It is known to play a role in wall remodeling and aneurysm progression [52]. WSS is transformed into biological signals via mechanical receptors on endothelial cells. Thus, a WSS that is too low to maintain endothelial functions may facilitate degeneration of the aneurysmal wall and be responsible for AIC growth and rupture [53, 54]. Abnormal WSS are known to induce inflammatory responses mediated by: endothelial cells, activation of MMP metalloproteases, cell death, degradation of the extracellular matrix, and vascular remodeling [55,56,57,58]. However, and despite the fact that this parameter is cited as the most important, conclusions about its role vary widely [59]. Finally, the authors seem to agree on the role of too high WSS in the initiation phases, and they propose two pathways that can lead to rupture. The first is related to thrombus formation and the inflammatory reaction in the case of low WSS. The second, more direct, is related to matrix degradation secondary to destructive remodeling in the case of high WSS [57].
Two different parameters such as WSS and velocity decrease during FD placement at the aneurysm neck and the appearance of the flow lines changes before and after FD implantation. For example, placement of a NEUROFORM stent decreases the mean inflow velocity by 15%, whereas a PED reduces mean inflow by more than 80% [60]. This link between porosity and inflow reduction has been known since the use of non-DF stents. It is even more important when porosity is low, raising the suspicion that changes in these two variables play an important role in thrombus formation within the aneurysm [61]. A greater relative reduction in WSS and velocity is observed in small or fusiform aneurysms after DF implantation and some authors report that a one-third decrease in velocity is predictive of occlusion at 12 months [62, 63].
9.2.11 Cellular and Tissular Level
If the relationship between the stent and the wall has been extensively studied in cardiology, the particularity of the animal studies that focus on flow diverters is that it is the free segment of the stent (FSS) located at the level of the neck of the aneurysm (where there is no contact between the stent and the wall) that is the major zone of interest.
Indeed, the FSS must undergo biological changes in order to allow the occlusion of the aneurysm. In the first days (D1–3), there is a denudation of the endothelial cells of the artery where the DF is implanted. There are also islands of inflammatory cells at the wire intersections at the level of the FSS. Neonintimal formation at the artery is quite rapid compared with the more delayed formation at the FSS (Fig. 9.13).
(a) Section of the free segment of the FD after extraction which finds a thick neointima. (b) Neointima “bridges” are sometimes found on the luminal side that did not follow the “rule” of a close progression. (c) Photograph of the FSS of an FD 3 months after implantation in a canine model. This image shows the neointimal progression, which starts from the artery and propagates over the FD guides, predominating at the crossings, and proceeding in the direction of flow. (d) Shows the luminal aspect of the FSS of an angiographically occluded aneurysm at 3 months and finds a continuous neointimal layer on the surface of the FD. Courtesy of J. Raymond – I. Salazkin – A. Makoyeva (Montréal)
There are two potential sources of neointimal and neoendothelial cells to overlay the FSS: cells from the adjacent arterial wall (near-to-near migration) and circulating stem cells. For some authors, the neointima spreads over the FSS wires from the artery [13]. In this sense, it is possible that the most perfect possible apposition of the FD is important to allow this layer to form. On the other hand, poor FD apposition could lead to an increase in thrombotic risks. It could also lead to failure to heal because of channels between the DF and the artery that prevent migrating progenitor cells from “sliding” from the artery to the FD [64,65,66]. A complexification of these explanations would be to propose a multifactorial healing process starting from a flow modulation inducing thrombosis notably at the dome, with the concomitant neointimal formation of the FD starting at the portal artery. There may be a link between thrombus formation and endothelialization of the FD that is intertwined in the healing process.
9.2.12 Factors Related to Aneurysm Characteristics
9.2.12.1 The Importance of Aneurysm Size and Volume
It is likely that the size and total aneurysmal volume have an impact on the efficacy of FDs. In a review of the literature, experiments in large animals that resulted in aneurysms with larger volumes had lower efficacy rates than experiments involving smaller aneurysms [67].

9.2.12.2 The Importance of a Curve at the FSS or Covered Branch
FD has been shown to be more effective in lateral aneurysms in straight arteries than in curved arteries, regardless of whether one or more FDs are used [68]. The angle between the FSS and the direction of flow is important as studied by CFD [69]. The more parallel the flow is to the FSS, the better the conditions seem to be for providing support to the neointima. In the case of a curved FSS, which concerns a major part of the clinical situations, the porosity of the implant is of course more important at the convexity of the curve (Fig. 9.14).
(a–d) placement of an FD (PED) for the recanalization of a left carotid-cave unruptured aneurysm. The angioarchitecture permits here to have the FSS in front of a lateral aneurysm, in a quite straight segment, and the stent was placed with push providing a good compaction at the neck (e). Control angiogram at 6 months showed a total occlusion (f)
9.2.12.3 Lateral or Bifurcation Aneurysms and Fusiform Aneurysms
Some authors have studied the efficacy of the FD in bifurcation aneurysm situations and report a low rate of efficacy [70]. Flow diversion in the treatment of bifurcation aneurysms may be less effective because of the presence of a branch covered by the DF. Thus, in some experiments, the presence of a branch from the aneurysmal neck or fundus has been identified as a factor for failure [71]. Some anatomic configurations (lateral aneurysms) facilitate complete ap-positioning of the FSS at the aneurysm neck allowing continuous neointimal coverage along the DF wires (Fig. 9.15). This is more commonly encountered in lateral aneurysms and is not possible in bifurcation aneurysms in which the SSF only partially covers the neck. The size of the neck is also a factor influencing the outcome.
Recurrent aneurysm of previously ruptured Posterior Communicating artery was treated with FD (a). Persistence of a flux within the sac was noted for 12 months after the treatment by FD (b, c) and retreatment was performed using direct access of the sac through the Posterior Communicating artery and simple coiling with the concomitant use of a balloon inside the FD (d, e). Control angiogram at 6 months of the retreatment showed a total occlusion of the aneurysm (f)
9.2.12.4 The Covered or “Jailed” Branch
The presence of a covered, or “jailed” branch arising from the neck or aneurysm is often cited as a cause of ineffective FDs. An FSS can cover both the neck of the aneurysm and a branch. It is desired that this branch remains open, with no or minimal occlusive tissue formation at its ostium. Darsaut et al., in a canine model of a lateral aneurysm with a branch, demonstrated the ability of the FD to occlude the aneurysm while leaving the branch open [72] (Fig. 9.16). To date, in animal models of large bifurcation aneurysms, the FD has failed to occlude these aneurysms, which corroborates some clinical papers that have, for example, shown the ineffectiveness of FDs in bifurcation aneurysms with a jail branch considered hemodynamically significant [68, 73].
Recanalization of a previously ruptured left posteroinferior cerebellar artery initially treated by coils (a). Stenting with an FD in the vertebral artery, covering both aneurysm neck and PICA ostium (b–e). The control angiogram at 6 months showed a preserved patency of the PICA. The aneurysm is still circulating but partially collapsed (f)
9.2.12.5 Factors Related to the Choice of the FD
The effects of the FSS on flow are influenced by the porosity and pore density, which are themselves related to the thickness of the unitary wires and the distance between them [74]. The final porosity of the FSS differs significantly from the nominal porosity, which should be a characteristic given by the manufacturer. The more oversized a DF is in relation to the artery; the longer and more porous its transition zone is, and the greater its deformation is. Conceptually, a high pore density decreases the physiological distance between unitary wires facilitating neointimal coverage from proximal to proximal. Sadisvan et al. showed that pore density was a more important parameter than porosity in terms of effectiveness [20]. It is likely that increasing the number of wires, thus affecting the two cardinal parameters of porosity and pore density, will increase the effectiveness of the implant. Hong et al. showed that the amount of neointima formed was proportional to the amount of metal coverage (MC) of the implant [75]. In clinical practice, the diameter of FD is usually chosen in relation to the proximal diameter (proximal delivery zone), with a degree of oversizing always present to avoid the risk of migration. This oversizing is often greater at the distal anchor zone because of the progressive decrease in vessel caliber. The degrees of expansion are variable and the stent will expand where space is available, either at the aneurysmal neck or in covered branches of significant caliber. This deformation will be even more important if the FD is oversized. The TZs between the areas compressed by the vascular tree and the uncompressed areas are areas of lower porosity.
9.2.12.5.1 Compaction of the Flow Diverter by the Operator
Compaction of the device during deployment will decrease the porosity of the implant to increase its potential to reduce aneurysmal flow and provide better support for neointimal formation. Unfortunately, the transition zones are not accessible to compaction by the operator and their porosity is even more important when the implant is oversized in diameter. Their responsibility in post-FD failures is likely, especially since these zones are often located in the flow entry zones [68, 69].
9.3 Clinical Studies
9.3.1 Efficacy
Numerous series report the efficacy rates (in terms of angiographic occlusion) as well as the morbidity and mortality rates of the use of the flow diversion technique. The differences within these series are numerous and are related to: the characteristics of the treated aneurysms, such as their nonproximal location, or at a bifurcation [76,77,78,79]; the context of their use, ruptured aneurysms [80,81,82], blister dissections [83, 84], surgical wounds [85, 86], aneurysmal recurrences [87]; the FD type [87, 88].
The FDA approval followed the PUFS study, a prospective uncontrolled study that obtained 73.6% complete occlusion at 6 months and a morbidity rate of 5.6% in 107 patients [89]. Similar efficacy and morbidity figures have been found in many prospective registries, such as InterPED [90].
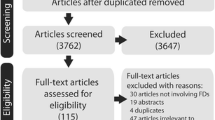
In the meta-analysis of Arrese et al. [91], 15 studies were analyzed for a total of 897 patients with 1018 aneurysms. The mean duration of patient follow-up was 8.5 months. The early mortality rate (1 month) was 2.8% (1.7% hemorrhage and 0.9% ischemia). The early neurological morbidity rate was 7.3%. At more than 1 month, the most frequent complication was ischemia (3.6%), followed by mass effect (1.1%), and rupture (0.9%). The delayed mortality rate was 1.3% (total 4.1%) and the delayed neurological morbidity rate was 2.6%. This represents a total of 14% of morbidity and mortality over the average follow-up period (8.5 months. With regard to the occlusion rate, the average rate was 76.2%. The authors mention that in light of their work the results with FDs are worse than in reported series of coiling, or even clipping [92, 93]. The bias here is obvious, and the conclusion severe if FDs were used after ruling out other treatments (Figs. 9.17 and 9.18). However, the high rate of occlusion at 9 months questions whether this population is predominantly composed of complex aneurysms.
Illustrative case for the use of FDs in complex cases. Case of a 53 years old female that presented with rapidly progressive intracranial hypertension symptoms. MRI revealed a giant partially thrombosed right Sylvian aneurysm (a). Treatment was performed by coiling and flow diverter (Silk Vista Baby) after a craniectomy (b–e). Follow-up images performed at 12 months showed the near-complete occlusion of the aneurysm sac and a significant reduction of the mass effect that permitted to replace the bone flap (f)
Illustrative case for the use of FDs in complex cases. Patient of 25 years old presenting with diplopia. MRI found and fusiform aneurysm with parietal hemorrhagic and thrombotic changes responsible for a brainstem focal ischemia (a–d). After a preventive posterior fossa craniectomy, an occlusion of the post-PICA segment of the right vertebral artery was performed, and 2 FD were placed after the implantation of a tutor stent (Leo) and coiling (control angiogram at 3 months: e, f)
The meta-analysis of Brinjikji et al. [94] included a total of 1451 patients and 1654 aneurysms. The 6-month complete occlusion rate was 76%. Procedure-related morbidity was 5% and mortality was 4%. The postprocedure subarachnoid hemorrhage rate was 3%. The rate of intracerebral hemorrhage was also 3%. The rate of infarction was also 3%, significantly lower in the anterior circulation than in the posterior circulation. The same is true for the rate of ischemic events, which was 6%, and significantly lower in the anterior circulation than in the posterior circulation. This meta-analysis shows that FD treatment is safer in small aneurysms with a lower rate of ischemic events and subarachnoid hemorrhage. These complication rates are in agreement with a systematic review by Briganti et al. who found a mean neurological morbidity of 3.5% and a mean mortality of 3.4% [95]. And also with Lv et al. that analyzed 29 studies or 1524 patients between 2009 and 2014 and reported a morbidity of 14% and a mortality of 6.6%. In this latter study, fusiform, dissecting, circumferentially implanted, posteriorly located, and distal aneurysms were the selected risk factors [96].
Considering flow diversion among MCA, anterior communicating artery, and distal anterior cerebral artery aneurysms, the recent meta-analysis of Cagnazzo et al. [97] included 27 studies (484 aneurysms). The long-term adequate occlusion rate (O’Kelly–Marotta scale, C–D) was 82.7%. Treatment-related complications were 12.5%, with 5.4% morbidity. MCA location was an independent factor associated with lower occlusion (OR = 0.5, P = 0.03) and higher complication rates (OR = 1.8, P = 0.02), compared with anterior communicating artery and distal anterior cerebral artery aneurysms. Large/giant aneurysms were associated with higher odds of complications (OR = 2.2, P = 0.03). The rates of occlusion and narrowing of arteries covered by flow-diverter stents were 6.3% and 23.8%, respectively. Symptoms related to occlusion and narrowing of the jailed arteries were 3.5% and 3%, respectively.
Regarding the posterior circulation, data from previous reviews are in agreement with a meta-analysis that was published in Neuroradiology in 2016, including 14 studies for a total of 225 posterior circulation aneurysms in 220 patients. The procedure-related mortality rate was 15%, with an occlusion rate of 84%. The rate of ischemic events was 11% (7% related to perforators). The post-procedure subarachnoid hemorrhage rate was 3%. The rate of intracerebral hemorrhage was 4% [98].
9.3.2 Classifications
To evaluate our interventions, we have no choice but to reduce the variety and heterogeneity of clinical outcomes [99, 100]. It is best to judge the outcomes of these interventions in a reduced number of categories. The names of these categories must then be determined in order to differentiate successes from failures. Angiographic judgments after coiling of cerebral aneurysms are generally reported using the Roy/Raymond classification which judges occlusion in three categories of aneurysm occlusion (complete occlusion, residual neck, or residual aneurysm). While this scale is easy to use for judging coiled aneurysms, there are limitations in the reproducibility of assigning an angiographic result to a coiled patient by different observers [101]. Similar results have been obtained in magnetic resonance [102]. The same classification has been used to evaluate post-FD results, but its appropriateness is questionable. Indeed, residual aneurysms are common findings after FD placement, and occlusion results have the potential to improve with time. The situation is different with the coiling of cerebral aneurysms where it is desired that the end result persists. A residual neck is often an acceptable outcome in the follow-up of a coiled aneurysm. This may also be the case with FD treatment, but not always, because even slow opacification of an FD-treated aneurysm may be sufficient to sustain a mass effect, aneurysm progression, and in some cases rupture. Several classifications dedicated to post-flow diversion angiographic findings have been proposed. The main are listed below.
9.3.2.1 O’Kelly–Marotta (OKM) Classification [103]
In this classification, a grade is assigned to each aneurysm based on the degree of initial opacification (ABCD) and the degree of stasis [1,2,3] observed during the degree of initial opacification (ABCD) and the degree of stasis [1,2,3] observed during different angiographic phases (arterial = 1, capillary = 2, and venous = 3).
-
A: Total opacification
-
B: Subtotal opacification
-
C: Residual collar
-
D: Complete occlusion
9.3.2.2 Kamran–Byrne (KB) Classification [104]
This classification is proposed for saccular and fusiform aneurysms. For both types of aneurysms, it documents two items: the degree of aneurysmal occlusion using a 5-grade classification for aneurysmal occlusion and a three-point classification for the artery.
Item 1: Degree of occlusion for saccular aneurysms (an equivalent exists for fusiform aneurysms)
-
Grade 0, No change in intra-aneurysmal flow
-
Grade 1, Opacification of more than 50% of initial aneurysm volume
-
Grade 2, Opacification of less than 50% of initial aneurysm volume
-
Grade 3, Opacification limited to the region of the aneurysmal neck
-
Grade 4, Complete occlusion
Item 2: Assessment of the artery.
-
“a”: No change in caliber of the artery
-
“b”: Stenosis of the artery
-
“c”: occlusion of the artery
9.3.2.3 Grunwald Classification (SMART) [105]
This classification includes 5 grades from 0 to 4. This classification is the same for saccular aneurysms and fusiform aneurysms. The SMART classification takes into account the appearance of the inflow, the stasis (a, b, or c), and the location of residual opacification within the aneurysm as well as the degree of stenosis of the artery.
Assessment of the occlusion
-
Grade 0 (arterial time): Early in-jet is found
-
Grade 1 (venous time): The aneurysm is circulating
-
Grade 2 (venous time): The walls and the dome are judged to be unsafe
-
Grade 3 (venous time): The walls and the dome are judged secure
-
Grade 4 (venous time): Complete occlusion
Hemodynamic evaluation
-
“a”: no significant stasis
-
“b”: stasis is visible in the capillary phase
-
“c”: stasis is visible in the venous phase
Carrier axis, intra-stent stenosis (ISS):
-
Grade 0: No stenosis
-
Grade 1: Mild stenosis
-
Grade 2: Moderate stenosis
-
Grade 3: Severe stenosis (>70%)
-
Grade 4: Occlusion
9.4 Complications
They can be neurological or systemic. When they are neurological, they are of two main types, ischemic or hemorrhagic. They may or may not be symptomatic; simply revealed by follow-up examinations. The main difficulty is their definition, because it is obvious that the reported rates will differ according to the definition. In the case of the flow diverter, the implant puts the artery at risk permanently and complications may occur in a delayed fashion. This is important because case series often have a short average follow-up time, which may not reveal these complications at a distance.
9.4.1 Ischemic
Endovascular treatment that requires intra-arterial implantation of a metallic prosthesis raises concerns prosthesis, raises fears of thromboembolic complications (TE) similar to thromboembolic (TE) complications similar to the subacute thrombosis encountered during angioplasty-stenting of stenosing coronary or peripheral arteries [106]. They are largely related to uncontrolled platelet aggregation on the surface of the foreign body that has not yet been incorporated into the wall via neointimal formation. Flow diversion, therefore, requires a priori dual antiplatelet therapy, which will be discussed in the last paragraph.
TE complications can be immediate or delayed, symptomatic or not. They can occur at the level of the stent (Fig. 9.19), but also downstream or at the level of a branch covered by the FD. They represent a wide spectrum of complications: FD thrombosis, FD stenosis, downstream thrombus, ischemia of perforators or covered branches, etc. The heterogeneity of their causes and presentations also makes their report in clinical series very heterogeneous. However, the rate of TE complications is reported to be higher in the posterior circulation, but also in large aneurysms [94, 107]. However, these published data are limited by the short duration of patient follow-up. Skukalek et al. recently published a literature review and meta-analysis of post-FD complications, including TE complications. Nineteen studies were analyzed for a total of 1110 patients [108]. Their results were as follows: Symptomatic and transient TE: 3.67%. Permanent symptomatic TE and mortality: 1.35%. Asymptomatic TE: 1.93%.
Illustrative case of a left Sylvian bifurcation aneurysm, previously ruptured and with multiple sessions of treatment by coils treated by FD (a, b) under dual antiplatelets therapy. Intra-stent thrombosis at hour 3, presented with severe aphasia and right hemiplegia (c). Rescue manoeuvers of mechanical thrombectomy intra-stent with anti-GpIIbIIa infusion (d) yielded to quick reperfusion (e), but a frontal area of necrosis and aphasia persisted
Early or delayed FD thrombosis is always reported in a series of about 100 patients, with an occurrence rate of less than 5% [109]. It is important to keep in mind that the indications in which the first FDs were firstly implanted (proximal carotid aneurysm) were previously treated by occlusion of the (carotid) vessel. In these patients, for whom occlusion was possible, the impact of complete thrombosis of an FD is assumed to be low (unless the DF overlaps the bypass of the polygon of Willis). In this sense Labeyrie et al. report in January 2015 a series of large or fusiform aneurysms treated by occlusion of the supporting axis. The permanent neurological morbidity in this series was also 5% [110]. Thus, evaluation of the polygon or usual or unusual anastomotic support is important to assess before placement of an FD. In other words, if an FD is implanted in a patient tolerant of occlusion, it is important to know this before implant placement.
Another complication associated with the use of FD is delayed stenosis of the bearing artery. Chalouhi et al. report an observation rate of 15.8% of these stenoses, all asymptomatic, in an angiographic study of 139 patients; 73% of these stenoses were detected at 6 months [111].
Finally, as shown in the literature on non-DF intracranial stents, an eventual period of discontinuation of anti P2Y12 is a delicate moment. One of the causes, always raised by the authors, is the role of antiplatelets in ischemic and hemorrhagic complications. Some very late thrombosis (defined in the cardiology literature as occurring more than 1 year after implantation) has been reported [36, 112, 113]. In a series of 86 patients including aneurysms of the anterior or posterior circulation, Guédon et al. report a 3.5% rate of late ischemic complications. The other reported delayed cases are fusiform aneurysms of the basilar trunk treated with multiple PEDs in a telescopic fashion. Certainly, neointimal formation on fusiform aneurysms treated with multiple PEDs takes longer to achieve. It may also never be achieved, and the addition of new FDs as suggested by some may not be the answer. The longer the aneurysm segment, the greater the thrombotic potential of these FDs seems to be. In such cases, the authors advise maintaining double antiplatelets for a longer duration (more than 1 year). These particular cases are difficult in practice, because faced with patients who are clinically worsening, the difficulty is to do nothing.
Ischemic complications related to perforator occlusions after flow diversion are well known and described. Their overall rate is estimated by meta-analyses to be about 6%. The branch covered by the FD may be an artery whose vascularization is terminal, of the perforating artery type, or it may be a branch whose vascularization regime has or may have suppletions (communicating arteries, pial arteries, ophthalmic artery, etc.) (Fig. 9.20). With respect to posterior fossa aneurysms, the number of perforators potentially covered by the FD is very large. The greater number of complications in the treatment of basilar aneurysms could be explained by the delicate and terminal perfusion of the functional structures of the brain stem, and their limited possibility of collateralization. With regard to the anterior circulation, Gawlitza et al. report on 18 aneurysms, 17.6% of symptomatic lacunar lesions rapidly regressed and 29.4% of asymptomatic lacunar lesions [79, 114,115,116,117].
In this context, coverage of the anterior choroidal artery (AchoA) with FDs has been the subject of several publications [116, 118]. Most authors report the absence of clinical complications. However, they report rare cases of asymptomatic occlusions. The AchoA territory can be supplemented by other contributions. Takahashi et al. describe 7 cases of retrograde filling of the AchoA in case of occlusion of the clinoid ICA occlusion. The normal AchoA presents anastomoses with the posterior communicating artery and the PCA. These anastomoses are located at the level of the choroid plexuses, the lateral geniculate body, or at the level of the geniculate body, or at the proximal portion of the PCA [119].
Another artery often covered is the ophthalmic artery. Some authors have reported a 25% occlusion rate of this artery during FD placement [114, 120]. Rouchaud et al. performed ophthalmologic examinations of 28 patients treated with FD for carotid ophthalmic aneurysms; 31% of patients complained of the onset or progression of visual symptoms. In 39.3% of cases, abnormalities were found on ophthalmologic examination, including retinal emboli and optic nerve atrophy [114]. Collateral branches to the ophthalmic artery are numerous, and while proximal occlusion does not appear to be dangerous, it is the emboli to the retina that appear to be of greater concern.
Regarding the coverage of arteries with obvious bypasses (arteries communicating arteries, A1 segment with an effective anterior communicator), these may decrease in caliber or become occluded depending on the hemodynamic regimes, and this without neurological deficit in the vast majority of cases [121] (Fig. 9.21). Another important factor is the actual porosity of the FD located in front of these branches, which is influenced by the placement technique (compression of the implant) and by the choice of its size [122].
Case of a 37 years old female with an Anterior communicating unruptured “fusiform” aneurysm (a). Treatment consisted of the placement of an FD in each A1–A2 segment (Silk Vista Baby) (b–d). Control angiogram showed the exclusion of the aneurysm, and note the modification of flux and caliber within both cerebral anterior circulations (e)
9.4.2 Hemorrhagic
When a flow diverter is used to treat an aneurysm, the rate of hemorrhagic complications is estimated at about 5%, but the figures vary from 0% to 10% depending on the series [80, 123,124,125]. The complications described are subarachnoid and intraparenchymal hemorrhages. These may be near or distant from the aneurysm corresponding to aneurysmal rupture or parenchymal hemorrhage. Hemorrhagic complications have a poor prognosis including major morbidity and mortality. The management of these patients under dual antiplatelets therapy is delicate and the transfusion of platelets, the possible recourse to surgery, and the risk of DF thrombosis create clinical situations that are often complicated [108].
Ruptures following the placement of flow diverters have been widely reported [126,127,128] (Fig. 9.22). Their time of occurrence is not limited to the perioperative period according to reported clinical cases. Rouchaud et al. review the literature and reported that 3/4 of delayed ruptures occurred within the first month, that in 50% of cases, these were giant aneurysms, and that in 20% of cases, these ruptures occurred despite prior coiling. The prognosis of these ruptures is very poor in 80% of cases [129]. There are many hypotheses to explain these ruptures: Related to the thrombus that could cause transient destabilization of the aneurysmal wall [126]. Biological origin related to mural hypoxia, inflammation, and enzymatic degradation. This biological reaction may cause inflammatory secretions in the aneurysm wall via proteases in particular [130]. Hemodynamic origin, such as the presence of residual flow at the inflow zone [131] or the rapid creation of an intra-aneurysmal thrombus that creates an internal force responsible for tearing the aneurysm sac [132].
Patient of 53 years old presented with a SAH (mFisher 4) WFNS 1 (a). Cerebral angiography did not depict a saccular aneurysm, but a late-filling and stagnating millimetric area rising from the right retro-carotidian segment. Conservative management was primarily decided, and control angiography at day 7 showed a slight rebleeding and growth of the aneurysm (b). FD placement under dual antiplatelet therapy was decided and done on day 7 (c). Early control CTA at day 8 was performed following a clinical deterioration, and showed a rebleeding (d), note the absence of opacification of the aneurysm and the patency of the FD
Some authors recommend the use of coils associated with the FD implantation. However, these coils do not provide perfect protection, with Siddiqui et al. reporting two cases of rupture after coiling and FD, and Fischer et al. reported one [133, 134]. Staged techniques, with initial coiling of the aneurysm fundus followed by FD implantation, have been reported in cases of ruptured aneurysms. The goal is twofold: to avoid early aneurysmal rupture and to maximize aneurysmal occlusion. However, there is a lack of strong scientific data to support this strategy except [81, 135].
Intraparenchymal hemorrhages vary in severity depending on the situation and the size of the hematoma. There is no consensus for the management of these hemorrhages, and attitudes obviously depend on the clinical presentation. Depending on the clinical presentation, several options are possible: modification, or not, of the antiplatelet regimen, recourse to surgery [124, 136].
The most common explanation is the hemorrhagic transformation of a silent ischemic lesion, aggravated by double antiplatelet aggregation. However, it is interesting to note that no prior ischemic lesion was observed in the reported cases of hematoma. Yet, these patients frequently have postprocedural control imaging, but MRI series have shown that silent ischemic lesions are common [137]. One could always imagine a hemorrhagic transformation of a small lesion, or of an ischemic lesion that took place remotely from the procedure. Other authors have suggested microscopic embolisms of foreign bodies (PVP, polyvinylpyrrolidone), composed of the internal linings of catheters, which have been found in the brain parenchyma of patients who died of post-FD hemorrhagic complications [138].
Another original explanation is the modification by the flow diverter of the compliance of the vessel in which it is placed. This implantation would change the pressure regime transmitted to the distal vasculature and would result in a hemorrhagic complication [124, 139].
9.5 Antiplatelets Regimen
Antiplatelets are used more and more frequently in daily practice. They are used pre-procedure, intra-procedure, and post-procedure, sometimes for several years following treatment. However, there are actually no recommendations based on strong scientific evidence, and the management of antiplatelets both before and after the procedure remains debated.
The classic preparation, which uses two complementary molecules, Aspirin and Clopidogrel, has its limitations. The variability of response to Clopidogrel has been demonstrated, and its link to ischemic and hemorrhagic complications is strongly suspected [140]. In this context, some learned societies such as SNIS concluded in 2014 that there is insufficient evidence to recommend the routine use of platelet function tests [141]. The life span of platelets is 7–10 days. Approximately 10–15% of the platelet supply is replaced daily. Tests to assess the degree of platelet inhibition are numerous, and the gold standard is LTA (Light Transmission Aggregometry). In the field of INR, the most studied test is the “Verify Now” test, which is the subject of author recommendations [142]. This test estimates the ability of a drug to block the P2Y12 receptor and thus makes it possible to identify hypo- and hyperresponders. Indeed, general and specific reasons make each person’s sensitivity to antiplatelets such as clopidogrel unique (obesity, drug interactions, genetic mutations, pro-coagulant states, smoking, etc.) [102, 143]. The results are reported in P2Y12 reactive units (PRU). If the PRU is high: many platelets are reactive, the risk is thrombotic, If the PRU is low: few platelets are reactive, the risk is hemorrhagic. Delgado et al. proposed acceptable values between 60 and 240 for endovascular stent/DF treatment of cerebral aneurysms [144]. However, other authors such as Tan et al. place the threshold at 208 [140]. In his meta-analysis, Skukalek et al. report the following: a high dose of Aspirin administered for more than 6 months is associated with fewer TE or bleeding events. Less than 6 months of Clopidogrel administration is associated with more TE events. Loading doses of Aspirin and Clopidogrel are associated with fewer bleeding events. Platelet inhibition test results did not correlate with complications [108]. The data from this meta-analysis appear to support the use of high-dose Aspirin and Clopidogrel for at least 6 months in combination with a pre-procedure loading dose.
Aspirin is a COX-1 inhibitor and prevents the synthesis of TXA2, which inhibits platelet function throughout its life. Aspirin is rapidly effective, with maximum activity measurable as early as 30–60 min after administration [145]. Small doses, less than 100 mg, are sufficient to completely block TXA2 synthesis. However, if a period of 4–7 days is required for full normalization of platelet activity, normalization of TS is observed between 48 and 72 h after cessation. Reversal of the therapeutic effect can be achieved by platelet transfusion. Resistance to aspirin is controversial, with reported rates of resistance ranging from 5% to 40%, and resistance can be overcome by increasing the dose [146].
Clopidogrel is a hepatically metabolized pro-drug that induces irreversible ADP blockade at the P2Y12 surface receptor. Clopidogrel has no immediate effect at a maintenance dose of 75 mg but requires 3–7 days to achieve the desired inhibition [147]. A loading dose of Clopidogrel 600 mg achieves platelet inhibition in 2–4 h [148]. The definition of resistance varies between trials and influences the proportion of resistant patients. The rate of resistance to Clopidogrel varies between studies and tests used, reaching over 50% in some series [149]. The most commonly reported interaction is with proton pump inhibitors. This interaction was the subject of an FDA warning in 2009, and one study suggested that the combination of Clopidogrel and pantoprazole should be preferred when these drugs are used together.
Prasugrel and Ticagrelor have already been adopted by many teams despite the lack of evidence of superiority [150] and randomized studies are needed on this topic. While Prasugrel is a pro-drug that requires hepatic hydrolysis and oxidation before binding to the P2Y12 receptor, Ticagrelor does not undergo a transformation in vivo. Prasugrel, for example, shows less inter-patient variability than Clopidogrel. The largest published series is that of Akbari et al., who reported in a non-randomized study a bleeding complication rate of 19.4% in the Aspirin/Prasugrel arm compared with a rate of 3.6% in the Aspirin/Clopidogrel arm [151]. The authors also recommend lowering the daily dose of Prasugrel to 5 mg.
Ticagrelor is not all good. It requires twice-daily dosing, which decreases compliance, and it is difficult to antagonize, with little theoretical efficacy of platelet transfusions in case of bleeding complications. It also has adverse effects such as dyspnea. It is necessary to be wary of its drug interactions; thus, it is recommended to keep the dose of aspirin below 100 mg per day and to avoid doses above 40 mg of the following statins: Simvastatin and Lovastatin.
Anti-GpIIbIIa (Abciximab, Eptifibatide, Tirofiban) molecules cause more rapid platelet inhibition than Clopidogrel. They can be injected intra-arterially or intravenously. They can be used preventively or in the context of clinical or angiographic thromboembolic complications. They can be used during coiling, stenting, or FD implantation [152,153,154]. A bolus type protocol per IV or IA procedure could allow a rapid and constant platelet inhibition, thus avoiding prior preparations and tests. However, the modalities of relaying the treatment which will be continued orally by the patient raise questions. Indeed, the interest of a preparation tested before the procedure is the probable obtaining of a stable regime and a predefined post-procedure treatment. If a per-procedure bolus approach were to be applied, the post-procedure therapy should not suffer from resistance and/or an excessive rate of bleeding complications. In these cases, molecules such as Prasugrel and Ticagrelor may be interesting because of their efficacy, but may also raise concerns about an increase in the bleeding complications described in the cardiology literature [155].
Similar in action mechanism to Ticagrelor, Cangrelor allows intravenous administration and offers the benefit of a very short duration of action (2 min) with a half-life of 3 to 6 min after stopping the infusion. Cangrelor may be a feasible alternative for patients requiring immediate intervention with the use of FD. It allows the possibility for a secure transition to long-term ticagrelor and progression to surgery in the setting of unexpected complications, but the recent introduction of an intravenous P2Y12 inhibitor further adds to the multitude of modalities and contexts in which changes in therapy can occur [156,157,158].
References
Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 26 Oct 2002;360(9342):1267–74.
Guglielmi G, Viñuela F, Sepetka I, Macellari V. Electrothrombosis of saccular aneurysms via endovascular approach. Part 1: Electrochemical basis, technique, and experimental results. J Neurosurg. 1991;75(1):1–7.
Mascitelli JR, Oermann EK, De Leacy RA, Moyle H, Mocco J, Patel AB. Predictors of treatment failure following coil embolization of intracranial aneurysms. J Clin Neurosci. 2015;22(8):1275–81.
Spelle L, Piotin M, Blanc R, Moret J. Remodeling technique in the treatment of intracranial aneurysms: indications, limits and non-indications. Interv Neuroradiol. 2008;14(Suppl 1):52–9.
Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34(6):1398–403.
Augsburger L, Farhat M, Reymond P, Fonck E, Kulcsar Z, Stergiopulos N, et al. Effect of flow diverter porosity on intraaneurysmal blood flow. Klin Neuroradiol. 2009;19(3):204–14.
Kadirvel R, Ding Y-H, Dai D, Rezek I, Lewis DA, Kallmes DF. Cellular mechanisms of aneurysm occlusion after treatment with a flow diverter. Radiology. 2014;270(2):394–9.
Valdivia y Alvarado M, Ebrahimi N, Benndorf G. Study of conformability of the new leo plus stent to a curved vascular model using flat-panel detector computed tomography (DynaCT). Neurosurgery. 2009;64(3 Suppl):ons130-134.
Simgen A, Ley D, Roth C, Yilmaz U, Körner H, Mühl-Benninghaus R, et al. Evaluation of a newly designed flow diverter for the treatment of intracranial aneurysms in an elastase-induced aneurysm model, in New Zealand white rabbits. Neuroradiology. https://doi.org/10.1007/s00234-013-1296-9.
Dandapat S, Mendez-Ruiz A, Martínez-Galdámez M, Macho J, Derakhshani S, Foa Torres G, et al. Review of current intracranial aneurysm flow diversion technology and clinical use. J Neurointerv Surg. 2021;13(1):54–62.
Wang K, Yuan S. Actual metal coverage at the neck is critical for flow-diverting stents in treating intracranial aneurysms. AJNR Am J Neuroradiol. 2013;34(3):E31–2.
Cantón G, Levy DI, Lasheras JC. Hemodynamic changes due to stent placement in bifurcating intracranial aneurysms. J Neurosurg. 2005;103(1):146–55.
Hong B, Wang K, Huang Q, Xu Y, Fang X, Li Z, et al. Effects of metal coverage rate of flow diversion device on neointimal growth at side branch ostium and stented artery: an animal experiment in rabbit abdominal aorta. Neuroradiology. 2012;54(8):849–55.
Aurboonyawat T, Blanc R, Schmidt P, Piotin M, Spelle L, Nakib A, et al. An in vitro study of silk stent morphology. Neuroradiology. 2011;53(9):659–67.
Bing F, Darsaut TE, Salazkin I, Makoyeva A, Gevry G, Raymond J. Stents and flow diverters in the treatment of aneurysms: device deformation in vivo may alter porosity and impact efficacy. Neuroradiology. 2013;55(1):85–92.
Baráth K, Cassot F, Fasel JHD, Ohta M, Rüfenacht DA. Influence of stent properties on the alteration of cerebral intra-aneurysmal haemodynamics: flow quantification in elastic sidewall aneurysm models. Neurol Res. 2005;27(Suppl 1):S120–8.
Dennis KD, Rossman TL, Kallmes DF, Dragomir-Daescu D. Intra-aneurysmal flow rates are reduced by two flow diverters: an experiment using tomographic particle image velocimetry in an aneurysm model. J Neurointerv Surg. 2015;7(12):937–42.
Shapiro M, Raz E, Becske T, Nelson PK. Variable porosity of the pipeline embolization device in straight and curved vessels: a guide for optimal deployment strategy. AJNR Am J Neuroradiol. 2014;35(4):727–33.
Shapiro M, Raz E, Becske T, Nelson PK. Building multidevice pipeline constructs of favorable metal coverage: a practical guide. AJNR Am J Neuroradiol. 2014;35(8):1556–61.
Sadasivan C, Cesar L, Seong J, Rakian A, Hao Q, Tio FO, et al. An original flow diversion device for the treatment of intracranial aneurysms: evaluation in the rabbit elastase-induced model. Stroke. 2009;40(3):952–8.
Ma D, Dargush GF, Natarajan SK, Levy EI, Siddiqui AH, Meng H. Computer modeling of deployment and mechanical expansion of neurovascular flow diverter in patient-specific intracranial aneurysms. J Biomech. 2012;45(13):2256–63.
Ley D, Mühl-Benninghaus R, Yilmaz U, Körner H, Cattaneo GFM, Mailänder W, et al. The Derivo embolization device, a second-generation flow diverter for the treatment of intracranial aneurysms, evaluated in an elastase-induced aneurysm model. Clin Neuroradiol. 2017 Sept;27(3):335–43.
Kocer N, Islak C, Kizilkilic O, Kocak B, Saglam M, Tureci E. Flow re-direction endoluminal device in treatment of cerebral aneurysms: initial experience with short-term follow-up results. J Neurosurg. 2014;120(5):1158–71.
Kim BM, Kim DJ, Kim DI. A new flow-diverter (the FloWise): in-vivo evaluation in an elastase-induced rabbit aneurysm model. Korean J Radiol. 2016;17(1):151–8.
Ma D, Xiang J, Choi H, Dumont TM, Natarajan SK, Siddiqui AH, et al. Enhanced aneurysmal flow diversion using a dynamic push-pull technique: an experimental and modeling study. AJNR Am J Neuroradiol. 2014;35(9):1779–85.
Darsaut TE, Bing F, Makoyeva A, Gevry G, Salazkin I, Raymond J. Flow diversion to treat aneurysms: the free segment of stent. J Neurointerv Surg. 1 Sep 2013;5(5):452–7.
Makoyeva A, Bing F, Darsaut TE, Salazkin I, Raymond J. The varying porosity of braided self-expanding stents and flow diverters: an experimental study. AJNR Am J Neuroradiol. 2013;34(3):596–602.
Darsaut TE, Bing F, Salazkin I, Gevry G, Raymond J. Testing flow diverters in giant fusiform aneurysms: a new experimental model can show leaks responsible for failures. AJNR Am J Neuroradiol. 2011;32(11):2175–9.
Cohen JE, Gomori JM, Moscovici S, Leker RR, Itshayek E. Delayed complications after flow-diverter stenting: reactive in-stent stenosis and creeping stents. J Clin Neurosci. 2014;21(7):1116–22.
Chalouhi N, Tjoumakaris SI, Gonzalez LF, Hasan D, Pema PJ, Gould G, et al. Spontaneous delayed migration/shortening of the pipeline embolization device: report of 5 cases. AJNR Am J Neuroradiol. 2013;34(12):2326–30.
Fischer S, Aguilar-Pérez M, Henkes E, Kurre W, Ganslandt O, Bäzner H, et al. Initial experience with p64: a novel mechanically detachable flow diverter for the treatment of intracranial saccular sidewall aneurysms. AJNR Am J Neuroradiol. 2015;36(11):2082–9.
Rayepalli S, Gupta R, Lum C, Majid A, Koochesfahani M. The impact of stent strut porosity on reducing flow in cerebral aneurysms. J Neuroimaging. 2013;23(4):495–501.
Heller R, Calnan DR, Lanfranchi M, Madan N, Malek AM. Incomplete stent apposition in Enterprise stent-mediated coiling of aneurysms: persistence over time and risk of delayed ischemic events. J Neurosurg. 2013;118(5):1014–22.
Pereira VM, Kelly M, Vega P, Murias E, Yilmaz H, Erceg G, et al. New pipeline Flex device: initial experience and technical nuances. J Neurointerv Surg. 2015;7(12):920–5.
Tulamo R, Frösen J, Hernesniemi J, Niemelä M. Inflammatory changes in the aneurysm wall: a review. J Neurointerv Surg. 2010;2(2):120–30.
Fiorella D, Hsu D, Woo HH, Tarr RW, Nelson PK. Very late thrombosis of a pipeline embolization device construct: case report. Neurosurgery. 2010;67(3 Suppl):onsE313-314.
Krajewski S, Neumann B, Kurz J, Perle N, Avci-Adali M, Cattaneo G, et al. Preclinical evaluation of the thrombogenicity and endothelialization of bare metal and surface-coated neurovascular stents. AJNR Am J Neuroradiol. 2015;36(1):133–9.
Kuiper KK, Robinson KA, Chronos NA, Cui J, Palmer SJ, Nordrehaug JE. Phosphorylcholine-coated metallic stents in rabbit iliac and porcine coronary arteries. Scand Cardiovasc J. 1998;32(5):261–8.
Lewis AL, Stratford PW. A review on phosphorylcholine-coated stents. J Long-Term Eff Med Implants. 2017;27(2–4):233–52.
Whelan DM, van der Giessen WJ, Krabbendam SC, van Vliet EA, Verdouw PD, Serruys PW, et al. Biocompatibility of phosphorylcholine coated stents in normal porcine coronary arteries. Heart. 2000;83(3):338–45.
Girdhar G, Li J, Kostousov L, Wainwright J, Chandler WL. In-vitro thrombogenicity assessment of flow diversion and aneurysm bridging devices. J Thromb Thrombolysis. 2015;40(4):437–43.
Manning NW, Cheung A, Phillips TJ, Wenderoth JD. Pipeline shield with single antiplatelet therapy in aneurysmal subarachnoid haemorrhage: multicentre experience. J Neurointerv Surg. 2019;11(7):694–8.
Gentric J-C, Fahed R, Darsaut TE, Salazkin I, Roy D, Raymond J. Fatal arterial rupture during angioplasty of a flow diverter in a recurrent, previously Y-stented giant MCA bifurcation aneurysm. Interv Neuroradiol. 2016;22(3):278–86.
Schneiders JJ, VanBavel E, Majoie CB, Ferns SP, van den Berg R. A flow-diverting stent is not a pressure-diverting stent. AJNR Am J Neuroradiol. 2013;34(1):E1–4.
Cebral JR, Mut F, Raschi M, Scrivano E, Ceratto R, Lylyk P, et al. Aneurysm rupture following treatment with flow-diverting stents: computational hemodynamics analysis of treatment. AJNR Am J Neuroradiol. 2011;32(1):27–33.
Roszelle BN, Gonzalez LF, Babiker MH, Ryan J, Albuquerque FC, Frakes DH. Flow diverter effect on cerebral aneurysm hemodynamics: an in vitro comparison of telescoping stents and the pipeline. Neuroradiology. 2013;55(6):751–8.
Cebral JR, Mut F, Raschi M, Ding Y-H, Kadirvel R, Kallmes D. Strategy for analysis of flow diverting devices based on multi-modality image-based modeling. Int J Numer Method Biomed Eng. 2014;30(10):951–68.
Xiang J, Tutino VM, Snyder KV, Meng H. CFD: computational fluid dynamics or confounding factor dissemination? The role of hemodynamics in intracranial aneurysm rupture risk assessment. AJNR Am J Neuroradiol. 2014;35(10):1849–57.
Cebral JR, Castro MA, Burgess JE, Pergolizzi RS, Sheridan MJ, Putman CM. Characterization of cerebral aneurysms for assessing risk of rupture by using patient-specific computational hemodynamics models. AJNR Am J Neuroradiol. 2005;26(10):2550–9.
Cebral JR, Mut F, Weir J, Putman CM. Association of hemodynamic characteristics and cerebral aneurysm rupture. AJNR Am J Neuroradiol. 2011;32(2):264–70.
Malek AM, Alper SL, Izumo S. Hemodynamic shear stress and its role in atherosclerosis. JAMA. 1 Dec 1999;282(21):2035–42.
Shojima M, Oshima M, Takagi K, Torii R, Hayakawa M, Katada K, et al. Magnitude and role of wall shear stress on cerebral aneurysm: computational fluid dynamic study of 20 middle cerebral artery aneurysms. Stroke. 2004;35(11):2500–5.
Gibbons GH, Dzau VJ. The emerging concept of vascular remodeling. N Engl J Med. 1994;330(20):1431–8.
Omodaka S, Sugiyama S-I, Inoue T, Funamoto K, Fujimura M, Shimizu H, et al. Local hemodynamics at the rupture point of cerebral aneurysms determined by computational fluid dynamics analysis. Cerebrovasc Dis. 2012;34(2):121–9.
Kang H, Duran CL, Abbey CA, Kaunas RR, Bayless KJ. Fluid shear stress promotes proprotein convertase-dependent activation of MT1-MMP. Biochem Biophys Res Commun. 2015;460(3):596–602.
Kolega J, Gao L, Mandelbaum M, Mocco J, Siddiqui AH, Natarajan SK, et al. Cellular and molecular responses of the basilar terminus to hemodynamics during intracranial aneurysm initiation in a rabbit model. J Vasc Res. 2011;48(5):429–42.
Meng H, Tutino VM, Xiang J, Siddiqui A. High WSS or low WSS? Complex interactions of hemodynamics with intracranial aneurysm initiation, growth, and rupture: toward a unifying hypothesis. AJNR Am J Neuroradiol. 2014;35(7):1254–62.
Xiang J, Natarajan SK, Tremmel M, Ma D, Mocco J, Hopkins LN, et al. Hemodynamic-morphologic discriminants for intracranial aneurysm rupture. Stroke. 2011;42(1):144–52.
Castro MA, Putman CM, Sheridan MJ, Cebral JR. Hemodynamic patterns of anterior communicating artery aneurysms: a possible association with rupture. AJNR Am J Neuroradiol. 2009;30(2):297–302.
Shobayashi Y, Tateshima S, Kakizaki R, Sudo R, Tanishita K, Viñuela F. Intra-aneurysmal hemodynamic alterations by a self-expandable intracranial stent and flow diversion stent: high intra-aneurysmal pressure remains regardless of flow velocity reduction. J Neurointerv Surg. 2013;5(Suppl 3):iii38–42.
Liou T-M, Li Y-C. Effects of stent porosity on hemodynamics in a sidewall aneurysm model. J Biomech. 2008;41(6):1174–83.
Kulcsár Z, Augsburger L, Reymond P, Pereira VM, Hirsch S, Mallik AS, et al. Flow diversion treatment: intra-aneurismal blood flow velocity and WSS reduction are parameters to predict aneurysm thrombosis. Acta Neurochir (Wien). 2012;154(10):1827–34.
Ribeiro de Sousa D, Vallecilla C, Chodzynski K, Corredor Jerez R, Malaspinas O, Eker OF, et al. Determination of a shear rate threshold for thrombus formation in intracranial aneurysms. J Neurointerv Surg. 2016;8(8):853–8.
Chiu AHY, Marotta TR. Pipeline embolization device thrombosis induced peri-construct collateral channels. J Neurointerv Surg. 2016;8(11):e47.
Bavinzski G, Talazoglu V, Killer M, Richling B, Gruber A, Gross CE, et al. Gross and microscopic histopathological findings in aneurysms of the human brain treated with Guglielmi detachable coils. J Neurosurg. 1999;91(2):284–93.
Ozawa T, Tamatani S, Koike T, Abe H, Ito Y, Soga Y, et al. Histological evaluation of endothelial reactions after endovascular coil embolization for intracranial aneurysm. Clinical and experimental studies and review of the literature. Interv Neuroradiol. 2003;9(Suppl 1):69–82.
Fahed R, Raymond J, Ducroux C, Gentric J-C, Salazkin I, Ziegler D, et al. Testing flow diversion in animal models: a systematic review. Neuroradiology. 2016;58(4):375–82.
Darsaut TE, Bing F, Salazkin I, Gevry G, Raymond J. Flow diverters failing to occlude experimental bifurcation or curved sidewall aneurysms: an in vivo study in canines. J Neurosurg. 2012;117(1):37–44.
Darsaut TE, Bing F, Makoyeva A, Gevry G, Salazkin I, Raymond J. Flow diversion of giant curved sidewall and bifurcation experimental aneurysms with very-low-porosity devices. World Neurosurg. 2014;82(6):1120–6.
Raymond J, Darsaut TE, Makoyeva A, Bing F, Salazkin I. Endovascular treatment with flow diverters may fail to occlude experimental bifurcation aneurysms. Neuroradiology. 2013;55(11):1355–63.
Gentric JC, Darsaut TE, Makoyeva A, Salazkin I, Raymond J. The success of flow diversion in large and giant sidewall aneurysms may depend on the size of the defect in the parent artery. AJNR Am J Neuroradiol. 2014;35(11):2119–24.
Darsaut TE, Bing F, Salazkin I, Gevry G, Raymond J. Flow diverters can occlude aneurysms and preserve arterial branches: a new experimental model. AJNR Am J Neuroradiol. 2012;33(10):2004–9.
Tsang ACO, Fung AMY, Tsang FCP, Leung GKK, Lee R, Lui WM. Failure of flow diverter treatment of intracranial aneurysms related to the fetal-type posterior communicating artery. Neurointervention. 2015;10(2):60–6.
Kim M, Taulbee DB, Tremmel M, Meng H. Comparison of two stents in modifying cerebral aneurysm hemodynamics. Ann Biomed Eng. 2008;36(5):726–41.
Wang K, Huang Q, Hong B, Li Z, Fang X, Liu J. Correlation of aneurysm occlusion with actual metal coverage at neck after implantation of flow-diverting stent in rabbit models. Neuroradiology. 2012;54(6):607–13.
Briganti F, Delehaye L, Leone G, Sicignano C, Buono G, Marseglia M, et al. Flow diverter device for the treatment of small middle cerebral artery aneurysms. J Neurointerv Surg. 2016;8(3):287–94.
Caroff J, Neki H, Mihalea C, D’Argento F, Abdel Khalek H, Ikka L, et al. Flow-diverter stents for the treatment of saccular middle cerebral artery bifurcation aneurysms. AJNR Am J Neuroradiol. 2016;37(2):279–84.
Chalouhi N, Tjoumakaris S, Dumont AS, Gonzalez LF, Randazzo C, Starke RM, et al. Treatment of posterior circulation aneurysms with the pipeline embolization device. Neurosurgery. 2013;72(6):883–9.
Gawlitza M, Januel A-C, Tall P, Bonneville F, Cognard C. Flow diversion treatment of complex bifurcation aneurysms beyond the circle of Willis: a single-center series with special emphasis on covered cortical branches and perforating arteries. J Neurointerv Surg. 2016;8(5):481–7.
McAuliffe W, Wycoco V, Rice H, Phatouros C, Singh TJ, Wenderoth J. Immediate and midterm results following treatment of unruptured intracranial aneurysms with the pipeline embolization device. AJNR Am J Neuroradiol. 2012;33(1):164–70.
Brinjikji W, Piano M, Fang S, Pero G, Kallmes DF, Quilici L, et al. Treatment of ruptured complex and large/giant ruptured cerebral aneurysms by acute coiling followed by staged flow diversion. J Neurosurg. 2016;125(1):120–7.
Lin N, Brouillard AM, Keigher KM, Lopes DK, Binning MJ, Liebman KM, et al. Utilization of pipeline embolization device for treatment of ruptured intracranial aneurysms: US multicenter experience. J Neurointerv Surg. 2015;7(11):808–15.
Chalouhi N, Zanaty M, Tjoumakaris S, Gonzalez LF, Hasan D, Kung D, et al. Treatment of blister-like aneurysms with the pipeline embolization device. Neurosurgery. 2014;74(5):527–32.
Kalani MYS, Albuquerque FC, Levitt M, Nakaji P, Spetzler RF, McDougall C. Pipeline embolization for definitive endoluminal reconstruction of blister-type carotid aneurysms after clip wrapping. J Neurointerv Surg. 2016;8(5):495–500.
Iancu D, Lum C, Ahmed ME, Glikstein R, Dos Santos MP, Lesiuk H, et al. Flow diversion in the treatment of carotid injury and carotid-cavernous fistula after transsphenoidal surgery. Interv Neuroradiol. 2015;21(3):346–50.
Nerva JD, Morton RP, Levitt MR, Osbun JW, Ferreira MJ, Ghodke BV, et al. Pipeline embolization device as primary treatment for blister aneurysms and iatrogenic pseudoaneurysms of the internal carotid artery. J Neurointerv Surg. 2015;7(3):210–6.
Chalouhi N, Chitale R, Starke RM, Jabbour P, Tjoumakaris S, Dumont AS, et al. Treatment of recurrent intracranial aneurysms with the pipeline embolization device. J Neurointerv Surg. 2014;6(1):19–23.
Berge J, Biondi A, Machi P, Brunel H, Pierot L, Gabrillargues J, et al. Flow-diverter silk stent for the treatment of intracranial aneurysms: 1-year follow-up in a multicenter study. AJNR Am J Neuroradiol. 2012;33(6):1150–5.
Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 2013;267(3):858–68.
Kallmes DF, Hanel R, Lopes D, Boccardi E, Bonafé A, Cekirge S, et al. International retrospective study of the pipeline embolization device: a multicenter aneurysm treatment study. AJNR Am J Neuroradiol. 2015;36(1):108–15.
Arrese I, Sarabia R, Pintado R, Delgado-Rodriguez M. Flow-diverter devices for intracranial aneurysms: systematic review and meta-analysis. Neurosurgery. 2013;73(2):193–9.
Naggara ON, White PM, Guilbert F, Roy D, Weill A, Raymond J. Endovascular treatment of intracranial unruptured aneurysms: systematic review and meta-analysis of the literature on safety and efficacy. Radiology. 2010;256(3):887–97.
Ogilvy CS, Cheung AC, Mitha AP, Hoh BL, Carter BS. Outcomes for surgical and endovascular management of intracranial aneurysms using a comprehensive grading system. Neurosurgery. 2006;59(5):1037–42.
Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF. Endovascular treatment of intracranial aneurysms with flow diverters: a meta-analysis. Stroke. 2013;44(2):442–7.
Briganti F, Napoli M, Leone G, Marseglia M, Mariniello G, Caranci F, et al. Treatment of intracranial aneurysms by flow diverter devices: long-term results from a single center. Eur J Radiol. 2014;83(9):1683–90.
Lv X, Yang H, Liu P, Li Y. Flow-diverter devices in the treatment of intracranial aneurysms: a meta-analysis and systematic review. Neuroradiol J. 2016;29(1):66–71.
Cagnazzo F, Perrini P, Dargazanli C, Lefevre P-H, Gascou G, Morganti R, et al. Treatment of unruptured distal anterior circulation aneurysms with flow-diverter stents: a meta-analysis. AJNR Am J Neuroradiol. 2019;40(4):687–93.
Wang C-B, Shi W-W, Zhang G-X, Lu H-C, Ma J. Flow diverter treatment of posterior circulation aneurysms. A meta-analysis. Neuroradiology. 2016;58(4):391–400.
Suh SH, Cloft HJ, Lanzino G, Woodward K, Kallmes DF. Interobserver agreement after pipeline embolization device implantation. AJNR Am J Neuroradiol. 2013;34(6):1215–8.
Gaha M, Roy C, Estrade L, Gevry G, Weill A, Roy D, et al. Inter- and intraobserver agreement in scoring angiographic results of intra-arterial stroke therapy. AJNR Am J Neuroradiol. 2014;35(6):1163–9.
Tollard É, Darsaut TE, Bing F, Guilbert F, Gevry G, Raymond J. Outcomes of endovascular treatments of aneurysms: observer variability and implications for interpreting case series and planning randomized trials. AJNR Am J Neuroradiol. 2012;33(4):626–31.
Nakagawa I, Park HS, Yokoyama S, Wada T, Hironaka Y, Motoyama Y, et al. Influence of diabetes mellitus and cigarette smoking on variability of the Clopidogrel-induced antiplatelet effect and efficacy of active management of the target P2Y12 reaction unit range in patients undergoing neurointerventional procedures. J Stroke Cerebrovasc Dis. 2016;25(1):163–71.
O’kelly CJ, Krings T, Fiorella D, Marotta TR. A novel grading scale for the angiographic assessment of intracranial aneurysms treated using flow diverting stents. Interv Neuroradiol. 2010;16(2):133–7.
Kamran M, Yarnold J, Grunwald IQ, Byrne JV. Assessment of angiographic outcomes after flow diversion treatment of intracranial aneurysms: a new grading schema. Neuroradiology. 2011;53(7):501–8.
Grunwald IQ, Kamran M, Corkill RA, Kühn AL, Choi IS, Turnbull S, et al. Simple measurement of aneurysm residual after treatment: the SMART scale for evaluation of intracranial aneurysms treated with flow diverters. Acta Neurochir (Wien). 2012;154(1):21–6.
Saleh A, Hammoudeh A, Tabbalat R, Al-Haddad I, Al-Mousa E, Jarrah M, et al. Incidence and prognosis of stent thrombosis following percutaneous coronary intervention in middle eastern patients: the first Jordanian Percutaneous Coronary Intervention registry (JoPCR1). Ann Saudi Med. 2016;36(1):17–22.
Wong GKC, Kwan MCL, Ng RYT, Yu SCH, Poon WS. Flow diverters for treatment of intracranial aneurysms: current status and ongoing clinical trials. J Clin Neurosci. 2011;18(6):737–40.
Skukalek SL, Winkler AM, Kang J, Dion JE, Cawley CM, Webb A, et al. Effect of antiplatelet therapy and platelet function testing on hemorrhagic and thrombotic complications in patients with cerebral aneurysms treated with the pipeline embolization device: a review and meta-analysis. J Neurointerv Surg. 2016;8(1):58–65.
Szikora I, Berentei Z, Kulcsar Z, Marosfoi M, Vajda ZS, Lee W, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the pipeline embolization device. AJNR Am J Neuroradiol. 2010;31(6):1139–47.
Labeyrie M-A, Lenck S, Bresson D, Desilles J-P, Bisdorff A, Saint-Maurice J-P, et al. Parent artery occlusion in large, giant, or fusiform aneurysms of the carotid siphon: clinical and imaging results. AJNR Am J Neuroradiol. 2015;36(1):140–5.
Chalouhi N, Polifka A, Daou B, Kung D, Barros G, Tjoumakaris S, et al. In-pipeline stenosis: incidence, predictors, and clinical outcomes. Neurosurgery. 2015;77(6):875–9.
Guédon A, Clarençon F, Di Maria F, Rosso C, Biondi A, Gabrieli J, et al. Very late ischemic complications in flow-diverter stents: a retrospective analysis of a single-center series. J Neurosurg. 2016;125(4):929–35.
Klisch J, Turk A, Turner R, Woo HH, Fiorella D. Very late thrombosis of flow-diverting constructs after the treatment of large fusiform posterior circulation aneurysms. AJNR Am J Neuroradiol. 2011;32(4):627–32.
Rouchaud A, Leclerc O, Benayoun Y, Saleme S, Camilleri Y, D’Argento F, et al. Visual outcomes with flow-diverter stents covering the ophthalmic artery for treatment of internal carotid artery aneurysms. AJNR Am J Neuroradiol. 2015;36(2):330–6.
Kulcsár Z, Ernemann U, Wetzel SG, Bock A, Goericke S, Panagiotopoulos V, et al. High-profile flow diverter (silk) implantation in the basilar artery: efficacy in the treatment of aneurysms and the role of the perforators. Stroke. 2010;41(8):1690–6.
Brinjikji W, Kallmes DF, Cloft HJ, Lanzino G. Patency of the anterior choroidal artery after flow-diversion treatment of internal carotid artery aneurysms. AJNR Am J Neuroradiol. 2015;36(3):537–41.
van Rooij WJ, Sluzewski M. Perforator infarction after placement of a pipeline flow-diverting stent for an unruptured A1 aneurysm. AJNR Am J Neuroradiol. 2010;31(4):E43–4.
Raz E, Shapiro M, Becske T, Zumofen DW, Tanweer O, Potts MB, et al. Anterior choroidal artery patency and clinical follow-up after coverage with the pipeline embolization device. AJNR Am J Neuroradiol. 2015;36(5):937–42.
Takahashi S, Suga T, Kawata Y, Sakamoto K. Anterior choroidal artery: angiographic analysis of variations and anomalies. AJNR Am J Neuroradiol. 1990;11(4):719–29.
Puffer RC, Kallmes DF, Cloft HJ, Lanzino G. Patency of the ophthalmic artery after flow diversion treatment of paraclinoid aneurysms. J Neurosurg. 2012;116(4):892–6.
Brinjikji W, Lanzino G, Cloft HJ, Kallmes DF. Patency of the posterior communicating artery after flow diversion treatment of internal carotid artery aneurysms. Clin Neurol Neurosurg. 2014;120:84–8.
Berg P, Iosif C, Ponsonnard S, Yardin C, Janiga G, Mounayer C. Endothelialization of over- and undersized flow-diverter stents at covered vessel side branches: An in vivo and in silico study. J Biomech. 2016;49(1):4–12.
Byrne JV, Beltechi R, Yarnold JA, Birks J, Kamran M. Early experience in the treatment of intra-cranial aneurysms by endovascular flow diversion: a multicentre prospective study. PLoS One. 2 Sep 2010;5(9):e12492.
Cruz JP, Chow M, O’Kelly C, Marotta B, Spears J, Montanera W, et al. Delayed ipsilateral parenchymal hemorrhage following flow diversion for the treatment of anterior circulation aneurysms. AJNR Am J Neuroradiol. 2012;33(4):603–8.
Leung GKK, Tsang ACO, Lui WM. Pipeline embolization device for intracranial aneurysm: a systematic review. Clin Neuroradiol. 2012;22(4):295–303.
Chow M, McDougall C, O’Kelly C, Ashforth R, Johnson E, Fiorella D. Delayed spontaneous rupture of a posterior inferior cerebellar artery aneurysm following treatment with flow diversion: a clinicopathologic study. AJNR Am J Neuroradiol. 2012;33(4):E46–51.
Hampton T, Walsh D, Tolias C, Fiorella D. Mural destabilization after aneurysm treatment with a flow-diverting device: a report of two cases. J Neurointerv Surg. 2011;3(2):167–71.
Kacar E, Fatih Nas O, Erdogan C, Hakyemez B. Intracranial aneurysm rupture during flow diverter stent placement: successful treatment with stent-in-stent combination. Diagn Interv Imaging. 2015;96(4):411–3.
Rouchaud A, Brinjikji W, Lanzino G, Cloft HJ, Kadirvel R, Kallmes DF. Delayed hemorrhagic complications after flow diversion for intracranial aneurysms: a literature overview. Neuroradiology. 2016;58(2):171–7.
Hasan DM, Chalouhi N, Jabbour P, Magnotta VA, Kung DK, Young WL. Imaging aspirin effect on macrophages in the wall of human cerebral aneurysms using ferumoxytol-enhanced MRI: preliminary results. J Neuroradiol. 2013;40(3):187–91.
Ikeda H, Ishii A, Kikuchi T, Ando M, Chihara H, Arai D, et al. Delayed aneurysm rupture due to residual blood flow at the inflow zone of the intracranial paraclinoid internal carotid aneurysm treated with the pipeline embolization device: histopathological investigation. Interv Neuroradiol. 2015;21(6):674–83.
Fox B, Humphries WE, Doss VT, Hoit D, Elijovich L, Arthur AS. Rupture of giant vertebrobasilar aneurysm following flow diversion: mechanical stretch as a potential mechanism for early aneurysm rupture. J Neurointerv Surg. 2015;7(11):e37.
Fischer S, Vajda Z, Aguilar Perez M, Schmid E, Hopf N, Bäzner H, et al. Pipeline embolization device (PED) for neurovascular reconstruction: initial experience in the treatment of 101 intracranial aneurysms and dissections. Neuroradiology. 2012;54(4):369–82.
Siddiqui AH, Kan P, Abla AA, Hopkins LN, Levy EI. Complications after treatment with pipeline embolization for giant distal intracranial aneurysms with or without coil embolization. Neurosurgery. 2012;71(2):E509–13.
Princiotta C, Dall’olio M, Cirillo L, Leonardi M. Staged treatment of a blood blister-like aneurysm with stent-assisted coiling followed by flow diverter in-stent insertion. A case report. Interv Neuroradiol. Sep 2011;17(3):365–70.
Clarençon F, Di Maria F, Biondi A, Chiras J, Sourour N-A. Distant and delayed (>7 days) hemorrhage after treatment by flow-diverter stents in intracranial aneurysms: a rare but potentially serious complication. AJNR Am J Neuroradiol. 2013;34(7):E81–2.
Grunwald IQ, Papanagiotou P, Politi M, Struffert T, Roth C, Reith W. Endovascular treatment of unruptured intracranial aneurysms: occurrence of thromboembolic events. Neurosurgery. 2006;58(4):612–8.
Hu YC, Deshmukh VR, Albuquerque FC, Fiorella D, Nixon RR, Heck DV, et al. Histopathological assessment of fatal ipsilateral intraparenchymal hemorrhages after the treatment of supraclinoid aneurysms with the pipeline embolization device. J Neurosurg. 2014;120(2):365–74.
Mitha AP, Mynard JP, Storwick JA, Shivji ZI, Wong JH, Morrish W. Can the Windkessel hypothesis explain delayed Intraparenchymal Haemorrhage after flow diversion? A case report and model-based analysis of possible mechanisms. Heart Lung Circ. 2015;24(8):824–30.
Tan LA, Keigher KM, Munich SA, Moftakhar R, Lopes DK. Thromboembolic complications with pipeline embolization device placement: impact of procedure time, number of stents and pre-procedure P2Y12 reaction unit (PRU) value. J Neurointerv Surg. 2015;7(3):217–21.
Gandhi CD, Bulsara KR, Fifi J, Kass-Hout T, Grant RA, Delgado Almandoz JE, et al. Platelet function inhibitors and platelet function testing in neurointerventional procedures. J Neurointerv Surg. 2014;6(8):567–77.
Delgado Almandoz JE, Kadkhodayan Y, Crandall BM, Scholz JM, Fease JL, Tubman DE. Variability in initial response to standard clopidogrel therapy, delayed conversion to clopidogrel hyper-response, and associated thromboembolic and hemorrhagic complications in patients undergoing endovascular treatment of unruptured cerebral aneurysms. J Neurointerv Surg. 2014;6(10):767–73.
Luinstra M, Naunton M, Peterson GM, Bereznicki L. PPI use in patients commenced on clopidogrel: a retrospective cross-sectional evaluation. J Clin Pharm Ther. 2010;35(2):213–7.
Delgado Almandoz JE, Crandall BM, Scholz JM, Fease JL, Anderson RE, Kadkhodayan Y, et al. Pre-procedure P2Y12 reaction units value predicts perioperative thromboembolic and hemorrhagic complications in patients with cerebral aneurysms treated with the pipeline embolization device. J Neurointerv Surg. Nov 2013;5(Suppl 3):iii3–iii10.
Dabaghi SF, Kamat SG, Payne J, Marks GF, Roberts R, Schafer AI, et al. Effects of low-dose aspirin on in vitro platelet aggregation in the early minutes after ingestion in normal subjects. Am J Cardiol. 1 Oct 1994;74(7):720–3.
McKee SA, Sane DC, Deliargyris EN. Aspirin resistance in cardiovascular disease: a review of prevalence, mechanisms, and clinical significance. Thromb Haemost. 2002;88(5):711–5.
Savcic M, Hauert J, Bachmann F, Wyld PJ, Geudelin B, Cariou R. Clopidogrel loading dose regimens: kinetic profile of pharmacodynamic response in healthy subjects. Semin Thromb Hemost. 1999;25(Suppl 2):15–9.
Steinhubl SR, Berger PB, Mann JT, Fry ETA, DeLago A, Wilmer C, et al. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA. 20 Nov 2002;288(19):2411–20.
Guo LZ, Kim MH, Jin CD, Lee JY, Yi SJ, Park MK, et al. Comparison of pharmacodynamics between low dose ticagrelor and clopidogrel after loading and maintenance doses in healthy Korean subjects. Platelets. 2015;26(6):563–9.
Jones GM, Twilla JD, Hoit DA, Arthur AS. Prevention of stent thrombosis with reduced dose of prasugrel in two patients undergoing treatment of cerebral aneurysms with pipeline embolisation devices. J Neurointerv Surg. 1 Sep 2013;5(5):e38.
Akbari SH, Reynolds MR, Kadkhodayan Y, Cross DT, Moran CJ. Hemorrhagic complications after prasugrel (Effient) therapy for vascular neurointerventional procedures. J Neurointerv Surg. 2013;5(4):337–43.
Gentric J-C, Brisson J, Batista AL, Ghostine J, Raymond J, Roy D, et al. Safety of Abciximab injection during endovascular treatment of ruptured aneurysms. Interv Neuroradiol. 2015;21(3):332–6.
Sedat J, Chau Y, Gaudard J, Suissa L, Lachaud S, Lonjon M. Administration of eptifibatide during endovascular treatment of ruptured cerebral aneurysms reduces the rate of thromboembolic events. Neuroradiology. 2015;57(2):197–203.
Chalouhi N, Jabbour P, Daou B, Starke RM, Shields B, Hasan DM. A new protocol for anticoagulation with Tirofiban during flow diversion. Neurosurgery. 2016;78(5):670–4.
Valgimigli M, Tebaldi M, Campo G, Gambetti S, Bristot L, Monti M, et al. Prasugrel versus tirofiban bolus with or without short post-bolus infusion with or without concomitant prasugrel administration in patients with myocardial infarction undergoing coronary stenting: the FABOLUS PRO (Facilitation through Aggrastat By drOpping or shortening Infusion Line in patients with ST-segment elevation myocardial infarction compared to or on top of PRasugrel given at loading dOse) trial. JACC Cardiovasc Interv. 2012;5(3):268–77.
Linfante I, Ravipati K, Starosciak AK, Reyes D, Dabus G. Intravenous cangrelor and oral ticagrelor as an alternative to clopidogrel in acute intervention. J Neurointerv Surg. 2021;13(1):30–2.
Aguilar-Salinas P, Agnoletto GJ, Brasiliense LBC, Santos R, Granja MF, Gonsales D, et al. Safety and efficacy of cangrelor in acute stenting for the treatment of cerebrovascular pathology: preliminary experience in a single-center pilot study. J Neurointerv Surg. 2019;11(4):347–51.
Cortez GM, Monteiro A, Sourour N, Clarençon F, Elhorany M, Grigoryan M, et al. The use of cangrelor in neurovascular interventions: a multicenter experience. Neuroradiology. 2020;63(6):925–34.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Ognard, J., Abdelrady, M., Gentric, JC. (2022). Flow Diverter Stents. In: Lv, X. (eds) Endovascular Surgery of Cerebral Aneurysms. Springer, Singapore. https://doi.org/10.1007/978-981-16-7102-9_9
Download citation
DOI: https://doi.org/10.1007/978-981-16-7102-9_9
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-7101-2
Online ISBN: 978-981-16-7102-9
eBook Packages: MedicineMedicine (R0)