Abstract
Within the metaorganisms, cross-communication between commensal organisms and the host is crucial for the maintenance of physiological homeostasis. At times, microbiota becomes accountable for breaching homeostasis by creating a microenvironment favoring uncontrolled cell growth. Chronic infection and inflammation act as inciting factors for reactive oxygen species generation promoting damage to DNA, proteins, and lipids. Oxidative stress activates a variety of transcription factors that in turn control the expression of several inflammatory cytokines and chemokines. Consecutive changes including altered cell growth, genetic instability, and inhibition of apoptosis create a proper carcinogenic milieu. Apart from the complicated side effects associated with prevailing anticancer therapies, their safety, stability, and affordability are in question. At present, significant immunomodulating properties of probiotic bacteria are being considered as a promising tool in cancer treatment. In addition, to boost the innate defense mechanisms of hosts, probiotics can act as antigenotoxic, anticarcinogenic, and antioxidative agents. In this chapter, the role of pathogenic microbes in oxidative stress-induced cancer and the effectiveness of probiotics as a future therapeutic strategy in preventing cancer onset and progression through manipulating intestinal microflora are highlighted.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
Introduction
Cancer is a cumulative name of a group of diseases that can start with an uncontrollable abnormal type of cell growth in almost any organ or tissue of the body. Later, the cells metastasize to invade adjoining parts of the body and/or spread to various organs, being the major cause of death from cancer. According to WHO (www.who.int/health-topics/cancer), cancer is the second leading cause of death in the world with an estimated 9.6 million deaths. Cancer develops in three subsequent stages, namely, initiation, promotion, and progression. In the initiation stage, genotoxic carcinogen or exposure to irritation or inflammation induces an irreversible DNA mutation. In the promotion stage, proneoplastic cells undergo stimulated expansion of clonal growth, and in the progression stage, a clone of an early neoplastic cell is transformed into a fully malignant type, resulting in uncontrolled growth. In bacteria and protozoa-induced cancers, the presence of pathogens or their secreted products induces chronic inflammation and oxidative stress and thus modifies the cellular pathways of the host. To eliminate the pathogen, free radicals are produced by the inflammatory cells including macrophages and eosinophils. These free radicals can oxidize and damage DNA and may initiate DNA mutation in host cells leading to malignant transformation. The pathogenic organisms produce and secrete virulence factors like bacterial toxins, which disrupt and manipulate the homeostasis of host cells affecting cytoskeleton organization, trafficking of vesicles, intracellular signaling pathways, and protein synthesis. The bacterial defensive factors show adverse effects such as DNA damage, genomic instability, resistance to cell death, and signaling pathway alterations. These may cumulatively lead to carcinogenesis (Candela et al. 2014).
Several types of cancers can be induced by pathogenic microorganisms such as Helicobacter pylori in gastric cancer and MALT lymphomas, Chlamydia trachomatis in cervical cancer, Salmonella typhi in gallbladder cancer, and Fusobacterium nucleatum and Bacteroides fragilis in colon cancer (Kostic et al. 2012). Normal oral microflora maintains homeostatic condition in the oral cavity, but dysbiosis in the oral cavity may favor the growth of acidogenic and aciduric species, namely, Streptococci, Lactobacilli, and Bifidobacteria (Takahashi and Nyvad 2011), to cause dental caries. The growth of Tannerella forsythia, Porphyromonas gingivalis, Treponema denticola, oral Synergistetes, and Saccharibacteria (TM7) has also been found to be responsible for periodontal infections (Al-hebshi et al. 2015). In several studies, periodontitis, being the long-term chronic inflammation of gums, is associated with oral squamous cell carcinoma (OSCC). Porphyromonas spp. and Fusobacterium spp. are significantly higher in OSCC tissue compared to the healthy mucosa. P. gingivalis is associated with pancreatic cancer and gingival squamous carcinoma. F. nucleatum is associated with colorectal cancer (CRC) (Kostic et al. 2012).
Chronic inflammatory diseases increase the risk of carcinogenesis in digestive organs, such as inflammatory bowel disease (IBD) for colitic cancer, chronic atrophic gastritis for gastric cancer, chronic hepatitis for hepatocellular carcinoma (HCC) and cholangiocellular carcinoma, and chronic pancreatitis for pancreatic cancer. Inflammation can produce reactive oxygen species (ROS) via neutrophils, macrophage activation, peroxisomes, microsomes, and activation of the mitochondrial energy metabolism pathway. Endogenous production of ROS comes from the mitochondrial respiratory pathway and the NOX enzyme pathway (Block and Gorin 2012). Chronic exposure to high levels of ROS induces tissue remodeling, changes in gene expression, and DNA damage, resulting in the production of 8-oxo-dG. Lipid peroxidation produces 4-HNE and MDA that can induce angiogenesis. This may activate Wnt/β-catenin and PI3K/Akt signaling pathway and inactivate the tumor suppressor gene PTEN in a time and concentration-dependent manner (Lee et al. 2015). Treatment of cancer patients by using chemotherapy and radiation therapy is a painful process. Moreover, it exerts tremendous physical, emotional, and financial strains on individuals, families, communities, and health systems. In this context, the recent data on probiotic research using cancer cell lines and animal models strongly support its unprecedented ability in cancer prevention and improvement from early stages of cancer. The host having an adequate amount of live probiotic microorganisms gets additional beneficial effects. Many species and strains of Lactobacillus, Lactococcus, Pediococcus, Enterococcus, Streptococcus, Leuconostoc, Bacillus, Escherichia coli, Bifidobacterium, and Saccharomyces are predominantly used as probiotics (Fijan 2014). They can protect the intestinal mucosal barrier from toxic substances and pathogens. Therefore, it is able to modulate the immune system and prevent oxidative stress. Probiotic microorganisms create a physiologically restrictive environment by reducing intestinal pH through producing organic acids – lactic acid, acetic acid, bacteriocins, and defensins. These can prevent the colonization of pathogenic bacteria in the gut flora (Ng et al. 2009).
Bacteria-Induced Oxidative Stress Promotes Cancer Development
Oxidative DNA damage is regarded as one of the etiological factors in cancer promotion and progression. Bacterial infections play an important role in carcinogenesis through secretion of pro-inflammatory cytokines and ROS generation. Bacterial infections may also act as a cofactor in metastasis of cancer. In this context, few mechanisms of pathogen-induced carcinogenesis in different physiological systems of humans are discussed below.
Oxidative Stress in the Digestive System
Oral Carcinogenesis
P. gingivalis regulates intrinsic mitochondrial apoptosis pathways by JAK1/STAT3 and PI3K/Akt signaling. The suppression of proapoptotic BAD activity elevates BCL-2 (antiapoptotic): BAX (proapoptotic) ratio that decreases the release of the apoptosis effector cytochrome c. In another different mechanism, P. gingivalis inhibits apoptosis through a cascade of events that begins with the upregulation of miRNA-203 in gingival epithelial cells (GECs). Furthermore, nucleoside diphosphate kinase (NDK) secreted by P. gingivalis prohibits ATP-dependent apoptosis in GECs. It also interferes with an anticancer immune response mediated by ATP activation of P2X7 receptors on dendritic cells. The activation of IL6/STAT3 by chronic coinfection with P. gingivalis and F. nucleatum increases the advancement of chemically caused oral cancer (Binder Gallimidi et al. 2015).
FimA adhesion protein of P. gingivalis accelerates the cell cycle progression in S and G2 phases by upregulating cyclins, activating cyclin-dependent kinases (CDKs) by phosphorylation, and decreasing the level of p53 tumor suppressor protein (Pan et al. 2014). The lipopolysaccharide (LPS) of P. gingivalis is responsible for dysregulation of p53. P. gingivalis may promote GEC proliferation by activating β-catenin via gingipain-dependent proteolysis (Zhou et al. 2015). P. gingivalis and F. nucleatum has been reported to promote cellular invasion in OSCC. P. gingivalis infection activates the ERK1/2-ETS1, p38/HSP27, and PAR/NF-κβ pathways and upregulates pro-MMP-9 expression. Gingipains convert the proenzyme pro-MMP-9 into active MMP-9, which enhances cellular invasion (Inaba et al. 2015). Repeated exposure to P. gingivalis can also increase the invasiveness of OSCC cells by inducing epithelial to mesenchymal transition, stemness, and increased production of MMP-1 and MMP-10 (Ha et al. 2015). Infection of human epithelial cells by F. nucleatum enhances MMP-13 (collagenase 3) synthesis through activation of mitogen-activated protein kinase p38 and boosts cellular motility, reportedly through stimulation of Etk/BMX, S6 kinase p70, and RhoA kinase (Uitto et al. 2005).
Persistence of infection for a long time generates chronic inflammation, which gradually promotes different stages of carcinogenesis including induction, progression, invasion, and metastasis. ROS, reactive nitrogen intermediates (RNI), and cytokines produced by inflammatory cells contribute to the initiation of cancer by inducing mutations, genomic instability, and epigenetic alterations. Inflammatory cytokines then activate key transcription factors such as STAT3 and NF-κβ within the premalignant cells. This in turn supports the pro-malignant processes including proliferation, angiogenesis, invasion, and metastasis that may later result in a suitable tumor microenvironment (Landskron et al. 2014).
Acetaldehyde, hydroxyethyl radicals, and hydroxyl radicals are carcinogenic metabolites that are capable of forming DNA adducts. The ADH enzyme in certain oral bacteria such as Streptococcus salivarius, S. intermedius, S. mitis (Kurkivuori et al. 2007), nonpathogenic Neisseria spp., and Candida spp. catalyzes acetaldehyde production at mutagenic amounts under aerobic or microaerophilic conditions.
Oxidative Stress in the Gastrointestinal Tract
Clinical case studies, in vivo experiments in mice, and in vitro assays demonstrate positive correlation between microbe-induced chronic inflammatory disease and progression of carcinogenesis (Takaki and Yamamoto 2015). Colonization of H. pylori induces oxidative stress in the infected gastric mucosa and develops chronic atrophic gastritis and gastric cancer.
CagA protein of H. pylori induces oxidative stress that leads to chronic inflammation and carcinogenesis. CagA is delivered into gastric epithelial cells via T4SS, after which the pathophysiological actions take place in mitochondria where CagA suppresses tumor suppressor sirtuins (SIRT3). Subsequently, ROS and the hypoxia-related transcription factor HIF-1α get increased. Hypoxia and HIF-1α control a putative HRE positioned at the promoter of a carcinogenesis-related protein AQP3. The ROS-HIF-1α-AQP3-ROS loop not only causes DNA damage but also prevents DNA repair mechanisms, subsequently causing increased apoptosis. In addition, H. pylori infection induces the production of pro-inflammatory cytokines, such as IL-6, IL-8, and TNF, depending on the level of AQP3. CagA protein upregulates Wnt/β-catenin signaling and induces the proliferation of cancer stem cells (Yong et al. 2016).
Oxidative Stress in the Colon
Oxidative stress is an important progenitor and is related to genetic and epigenetic changes in the development of CRC. IBD including Crohn’s disease and ulcerative colitis (UC) is a risk factor for colitis-associated CRC. An individual’s environment might play an important role in inducing oxidative stress, as the gastrointestinal (GI) tract is constantly exposed to ingested materials and pathogens, including bacteria (Bhattacharyya et al. 2014). ROS-induced oxidized DNA such as 8-OHdG in CpG dinucleotide prevents carcinogenesis-related genes from being methylated. The accumulation of epigenetic alterations in the colon epithelium, such as DNA methylation of tumor suppressor genes, contributes to the development of cancer. IBD is a typical chronic inflammatory disease of the GI tract. Inflammatory cells, such as lymphocytes and neutrophils, are known to infiltrate the active mucosal lesions of UC patients. These cells can even induce active mucosal lesions. Single-nucleotide polymorphisms (SNPs) in the antioxidant gene GPX1 have been linked to UC, and SOD2 is linked to Crohn’s disease (CD). This implies that these diseases are genetically linked to oxidative stress (Costa Pereira et al. 2017). Analysis of mitochondrial DNA mutations has revealed that they are prevalent in UC and colon cancer tissue. The higher level of oxidative stress-related 8-OHdG in UC colon tissue indicates that mitochondrial DNA accumulation and oxidative stress are powerful contributors of carcinogenesis.
Streptococcus bovis is a normal gastrointestinal bacterium of ruminants. It increases the expression of some proliferative markers and induces IL-8 production in normal colonic mucosa. Antigens of S. bovis are capable of adhering to GI-epithelial, endothelial blood cells as well as to extracellular matrix and can induce IL-8 synthesis. This cytokine promotes oxidative/nitrosative stress and overexpression of COX-2. COX-2 induces cell proliferation mediated by prostaglandin synthesis and local immunosuppression. The synergistic effect of COX-2 is observed with other enzymes, which may promote CRC. In addition, S. bovis can induce MMP-2 and MMP-9 and form carcinogenic nitroso compounds that play a crucial role in CRC growth and progression (Tjalsma et al. 2012).
Oxidative Stress in the Reproductive System
Cervical cancer is the fourth most frequent cancer in women as reported in 2018 (WHO). Although the oncogenic human papillomavirus is known to be the major causative agent, recent reports suggest that Chlamydia is also responsible for cervical cancer. The infection with C. trachomatis induces ROS production via NOX and NLRX1 pathways (Abdul-Sater et al. 2010) leading to oxidative damage. Intracellular Chlamydia first induces NOX-dependent production of ROS, gets diffused into the mitochondrial matrix, interacts with NLRX1, and starts another round of ROS production. C. trachomatis can disrupt DNA damage responses (DDR) through alteration of histone modifications and activation of repair inhibitory mechanisms. The organism is also capable of downregulating polymerase beta through miR-499a upregulation, therefore impairing the BER (base excision repair) pathway (Gulve et al. 2019) and leading to single-strand and double-strand breakages in DNA. BER deficiency promotes genetic instability and is closely associated with the development of precancerous conditions. Downregulation of the tumor suppressor protein p53 prevents Chlamydia-infected cells from undergoing apoptosis. C. trachomatis causes telomere shortening (Prusty et al. 2013), which in turn helps to acquire tumorigenic properties.
Prostatic tissue invasion and intracellular deposition of Propionibacterium acne in the glandular epithelial cell are considered to be concomitantly involved in benign prostate hyperplasia and prostate cancer. Prostatic inflammation can be caused by Propionibacterium acne, as P. acne is the most frequent among all other bacteria that have been isolated from patients with prostate cancer (Davidsson et al. 2016). Oxidative free radicals caused by inflammation are one of those multiple factors that can initiate prostate cancer.
Oxidative Stress in the Respiratory System
Human lungs are exposed to the external environment and contain a specific pattern of microbiota. Among various environmental risk factors, microbes play an important part in maintaining microecological balance in the human lungs. There are certain microbial species in the lung tissues that are involved in regulating the pathogenesis of lung microenvironment. Chlamydia pneumoniae, a Gram-negative respiratory pathogen, is a common cause of chronic lung infection and prolonged inflammation (Khan et al. 2016). Epidemiological evidences have shown that C. pneumoniae is likely to be related to the growth and development of lung cell carcinoma. ROS generated during inflammation contributes to DNA damage and promotes carcinogenesis. Significant increase of C. pneumoniae IgA antibody is considered as a risk factor of adenocarcinoma and small cell carcinoma of the lungs. Chlamydial heat shock protein-60 (CHSP-60) antibodies are thus used as serological markers of prospective lung cancer (Chaturvedi et al. 2010). Healthy individuals’ alveolar macrophages emit TNF-α, IL-1, IL-8, as well as superoxide oxygen radicals that have been proven to cause lung tissue and DNA damage. C. pneumoniae acts as an effective inducer of TNF-α, IL-1, and IL-6 in host monocytic cells, playing a significant a role in carcinogenesis.
Bacterial Toxins Induced Cancer Development
Manipulation of host inflammatory response is emerging as an important mechanism for bacteria-induced cancer. Bacterial toxins modulate the host’s immune system in different manners such as specific immune cell activation and production of cytokines and metabolites to trigger a continuous inflammatory state that subsequently drives cells toward cancer development. Several factors are described below.
DNA-Damaging Toxins
After successful colonization in the GI tract, pathogenic microorganisms secrete several bacterial protein toxins that damage DNA, resulting in DNA mutation, oncogene activation, and cancer development.
Colibactin
The genome of some E. coli strains from the phylogenetic group B2 contains polyketide synthase (pks) island that produces the genotoxin colibactin. This colibactin can induce double-strand breaks (DSBs) in DNA of eukaryotic cells (Arthur et al. 2012). This may cause incomplete DNA repair, G2/M cell cycle arrest, chromosomal instability, and anchorage-independent colony formation. Again, the inflammation of GI tract may induce the growth of microbes, modulate pks island for more colibactin production, and alter the expression of microbial genes that are crucial for tumor development in host cells (Arthur et al. 2012).
Cytolethal Distending Toxin
Gram-negative bacterial pathogens like Campylobacter jejuni and E. coli strains are reported to produce cytolethal distending toxin (CDT). CDT holotoxin contains three different subunits, namely, CdtA, CdtB, and CdtC. CdtB is responsible for enzymatic activity, while CdtA binds to the host cell membrane. The nuclear transport signal of CdtB N-terminal region helps in nuclear localization and executes its cytotoxicity. In the context of structural and functional aspects, enzymatically active subunit CdtB is homologous to the mammalian DNase I. DNA damage and activation of DDR by CDT intoxication exhibit cytotoxic effects like G1 and/or G2 phase arrest and activation of DNA repair mechanisms. The cells that are unable to repair the damage eventually undergo senescence or apoptosis (Guerra et al. 2011). Frequent exposure to DNA damaging agents of endogenous (ROS) and exogenous (ionizing radiation) sources stimulates tumor initiation by altering gene expression of key proteins involved in DDR, cell cycle regulation, or DNA repair pathways. Prolong exposure of sublethal doses of CDT increases frequency of mutations, chromosomal aberrations, and impairment of the DDR. The B subunit of CDT is also present in typhoid toxin produced by Salmonella enterica serovar Typhi. CdtB-encoding Salmonella induces cell cycle arrest in the G2/M phase (Rodriguez-Rivera et al. 2015).
Cell-Signaling-Disrupting Toxins
Bacterial protein toxins can act on immune cells through interfering with cell proliferation pathways. These deregulated inflammatory responses further stimulate cells towards cancer progression. Some of the cell signal disrupting toxins and their roles in promoting carcinogenesis are described below.
Cytotoxin-Associated Gene A (CagA) and Vacuolating Cytotoxin A (VacA)
Helicobacter pylori is a microaerophilic Gram-negative bacterium that selectively colonizes in the acid-rich gastric epithelium and gastric mucosa of the human stomach (Moodley et al. 2012). H. pylori is classified as class I carcinogen by the International Agency for Research on Cancer (IARC), as it is responsible for several gastric diseases such as chronic gastritis and ulceration to neoplastic changes in stomach tissues (Cid et al. 2013). A complex process involving numerous factors including host genetic susceptibility factors, environmental factors, and the virulence factors of H. pylori helps to establish a proper carcinogenic milieu for gastric cancer (Ferreira et al. 2014). In H. pylori, these virulence factors are encoded from CagA and SabA gene present in the pathogenicity island, whereas peptidoglycan (PGN) and LPS help in immune evasion for which persistence of infection elicits chronic inflammation-mediated carcinogenesis.
Cytotoxic Necrotizing Factor 1
Some pathogenic E. coli strains produce the CNF1 protein toxin that can permanently activates Rho GTPase family proteins. Three groups of GTPases, Rho, Rac, and Cdc42, are activated by CNF1 through the deamidation of a pivotal glutamine residue, glutamine 63 in Rho or 61 in Cdc42. As a master regulator of the actin cytoskeleton, CNF1-activated Rho GTPase generates several actin-dependent events in cells. These include multi-nucleation, nuclear constriction, budding, multipolar metaphases, increase in cellular motility, and activation of NF-κβ via the stimulation of the Akt/Iκβ kinase pathway (Boyer et al. 2004). Apoptosis can be prevented by increasing the number of antiapoptotic proteins and promoting Rho-dependent cell spreading through CNF1.
Bacteroides fragilis Toxin
Bacteroides fragilis is an opportunistic pathogen and present as normal colonic microbiota due to its adherent nature with the mucosal layer in the colon (Dejea et al. 2013). B. fragilis toxin (BFT), a metalloprotease protein toxin from ETBF strain, is responsible for its pathogenicity in diarrheal disease, IBD, and CRC. BFT binds to the intestinal epithelial cell receptor, stimulates the cleavage of the tumor suppressor protein E-cadherin, and activates Wnt and NF-κβ signaling pathways (Dai et al. 2019). ETBF can increase tumorigenesis due to boosted STAT3 expression and promotes the recruitment of the highly pro-inflammatory subset of T helper type 17 lymphocytes. The pro-carcinogenic role of BFT is to develop a deregulated inflammatory response.
Staphylococcal Enterotoxins
Staphylococcal enterotoxins (SEs) of Staphylococcus aureus stimulate the large population of T cells leading to the production of a cytokine array (Pinchuk et al. 2010). SE may play an influential role in the malignant expansion and the evolution of immune dysregulation in patients with cutaneous T-cell lymphoma (CTCL), and thus, CTCL patients are frequently colonized with Staphylococcus aureus. Recent evidences demonstrate that SEs generate crosstalk between benign and malignant T cells causing a STAT3-mediated IL-10 production by the malignant T cells. The SEs subsequently alter the interactions between malignant and benign immune cells, resulting in greater cellular immunity suppression and disease activity in the patient. This leads to further deterioration of the skin barrier (Krejsgaard et al. 2014). The weakened host defense leads to the colonization of S. aureus and propagation, and these eventually increase the susceptibility of hosts to secondary infections.
Avirulence Protein A
Salmonella typhimurium is a major cause of human gastroenteritis. Chronic infections are often associated with hepatobiliary cancers. Salmonella typhi secreted protein toxin AvrA is associated with hepatobiliary cancers and colon cancer. It modulates inflammation, apoptosis, and proliferation of epithelial cells by changing the ubiquitination and acetylation of target proteins. AvrA enhances colonic tumorigenesis through activation of Wnt/β-catenin signaling pathway (Lu et al. 2014). AvrA plays an important role in several other pathways including oxidative phosphorylation, mTOR, and MAPK (Liu et al. 2010). AvrA-expressing bacteria can activate the STAT3 pathway leading to enhanced proliferation, thereby promoting tumorigenesis (Liu et al. 2010). It has been reported to enhance ROS production and c-Myc expression and thus considered as a key factor promoting CRC (Satuman et al. 2021).
FadA
Fusobacterium nucleatum, a Gram-negative anaerobic normal microflora of the oral cavity, has become one of the most prevalent species found in extraoral sites under diseased conditions (Han 2015). The abundant presence of F. nucleatum in CRC patients makes it a potential candidate for CRC susceptibility. In patients with adenomas and adenocarcinomas, F. nucleatum levels are ten to 100 times higher than in healthy people, promoting an upsurge in the expression of inflammatory and carcinogenic genes. The FadA adhesion with host E-cadherin generates carcinogenic effect by activating β-catenin signaling and increasing the expression of transcription factors, oncogenes, Wnt genes, and inflammatory genes. These cumulative events stimulate the growth of CRC cells (Rubinstein et al. 2013).
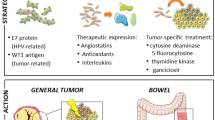
The mechanisms of oxidative stress-induced carcinogenesis by pathogenic bacteria are shown in Fig. 1.
The mechanism of oxidative stress-induced carcinogenesis by pathogenic bacteria. (1) Enterotoxigenic Bacteroides fragilis (ETBF) synthesizes BFT that binds to specific CEC receptor. BFT targets epithelial cell tight junctions, resulting in E-cadherin cleavage and activation of β-catenin that stimulates cellular proliferation through Wnt/β-catenin pathway. Simultaneously, it increases the expression of SMO gene via c-Myc, which in turn promotes SMO-dependent ROS production and DNA damage, increasing the risk of colon carcinogenesis. ETBF up-regulates STAT3 expression. This results in upregulation of IL-17 secretion and thus activates NF-κβ pathway and secretion of some specific chemokines (CXCL1, CXCL2, and CXCL5). This recruits myeloid-derived suppressor cells (MDSCs) and induces carcinogenesis. (2) Enterococcus faecalis generates extracellular superoxide and hydrogen peroxide, which further induces NF-κβ signaling through DNA damage and inflammation. E. faecalis can also express TGF-β in the intestinal epithelial cells, thereby activating the Smad signaling pathway. The superoxide produced by the microbiota can cause chromosome instability by enhancing the expression of COX-2 through the release of TNF-α from macrophages and thus initiates colorectal cancer. (3) Helicobacter pylori expresses a virulent microbial oncoprotein, i.e., CagA, that enters into gastric epithelial cells through T4SS. This induces gastric carcinogenesis through increased SMO level, thereby causing DNA damage. CagA induces NF-κβ pathway, which further increases the expression of cytokines (IL-1β and IL-8) and inducible nitric oxide synthase. A mediator of inflammation, nitric oxide is generated from iNOS. Furthermore, activation of NF-κβ upregulates the expression of miR-155, a microRNA associated with gastric inflammation. Another virulence factor, VacA, induces chemokine expression through Ca2+ influx as well as mitochondrial generation of reactive oxygen intermediates (ROIs) from human eosinophils, leading to chronic inflammation of the gastric mucosa. (4) Fusobacterium nucleatum invades colorectal epithelium with the help of FadA adhesin, which binds to E-cadherin, thereby activating β-catenin signaling. This increases the expression of oncogenes such as c-Myc and cyclin D1 and microRNA-21. Upon infection with F. nucleatum, the production of pro-inflammatory cytokines (IL-6 and IL-8) gets enhanced from immune cells
The Role of Protozoa in Cancer Development
Toxoplasma gondii
Toxoplasma gondii, the causative agent of toxoplasmosis, is found to be associated with various diseases, such as central nervous system neoplasia, meningioma, pituitary adenoma, primary intraocular B-cell lymphoma, nasopharyngeal carcinoma, embryonal carcinoma, gynecological benign tumors, cervical cancer, primary intraocular lymphoma, and primary intraocular B-cell lymphoma. Due to encystation, they can survive in the brain for a long time where elevated inflammation and inhibition of apoptosis increase the risk of brain cancer. T. gondii-infected host cells show resistance to multiple inducers of apoptosis, including Fas-dependent and Fas-independent cytotoxic T lymphocyte (CTL)-mediated cytotoxicity. Over-stimulation of the pituitary gland to fight the parasitic infection may lead to adenoma formation. Toxoplasma spp. have been reported to promote brain carcinogenesis through alteration of the host miRNAome (Thirugnanam et al. 2013).
Cryptosporidium parvum
Cryptosporidium parvum, the causative agent of cryptosporidiosis, has been correlated with digestive carcinogenesis, mainly colorectal cancer (Sulzyc-Bielicka et al. 2018). Coproantigens of this parasite can be found in the feces of patients with tumors located in the sigmoid and descending colon. C. parvum is found to be associated with cystic hyperplasia of the colonic mucosa, aural-pharyngeal polyps, gastrointestinal neoplastic changes, invasive adenocarcinoma, invasive gastrointestinal and biliary adenocarcinoma, glandular cystic polyps, and intramucosal adenocarcinoma. Altered gene expression of BCL-2, c-Myc, APC, and β-catenin during C. parvum infection is potentially involved in the development of C. parvum-induced ileocecal oncogenesis and neoplasia (Benamrouz et al. 2014).
Trichomonas vaginalis
Trichomoniasis caused by the protozoan Trichomonas vaginalis has become an emerging risk factor of cervical neoplasia and prostate cancer. Virulent isolates of T. vaginalis from patients with cervical neoplasia condition show the presence of a large number of hydrogenosomes and vacuoles that can aggravate cervical neoplasia (Yusof and Kumar 2012).
Plasmodium falciparum and Burkitt Lymphoma
In 1982, malaria and Epstein-Barr virus (EBV) were identified as cofactors in the pathogenesis of endemic Burkitt lymphoma. The main risk factor for endemic Burkitt lymphoma is coinfection with P. falciparum and EBV. Erythrocytes infected with P. falciparum adhere to B cells with the help of the CIDR1α domain of PfEMP1 and induce B cell activation, proliferation, and differentiation into plasma cells (Simone et al. 2011). Increased proliferation of polyclonal B cell population intensifies the risk of expansion and transition of EBV-infected B cells and might be a potential threat to the emergence of a malignant B cell clone. P. falciparum inhibits EBV-specific T cell immunity and increases the risk of Burkitt lymphoma through the growth and aberrant proliferation of EBV-infected B cells. P. falciparum-induced elevated viral load intensifies the oncogenic effects with the development of lymphoma. Activation-induced cytidine deaminase (AID) plays a key role in regulating chronic malaria and promoting malaria-induced lymphomagenesis. Malaria is not a direct cause of cancer itself, but P. falciparum infection changes the lymphoma phenotype that favors mature B cell lymphomas by encouraging extended AID expression in germinal B cells (Robbiani et al. 2015).
Entamoeba histolytica
Entamoeba histolytica, the causative agent of amoebiasis, adheres to the mucus layer of the intestine followed by colonization and destruction of the host’s extracellular matrix. Host immune response against amoebae includes secretion of abundant IgA to prevent pathogens from adhering and penetrating the mucus layer, recognition of the pathogens via Toll-like receptor surrounded by intestinal epithelial cells to activate NF-κβ, and further production of inflammatory cytokines. Neutrophils and macrophages activated by IFN-γ can be attracted to the site of infection and produce ROS and NO to kill the trophozoites. In the chronic stage of infection, the amount of ROS and reactive nitrogen species (RNS) are highly elevated in the microenvironment of the intestinal tract. This increases the oxidative stress in host cells and eventually causes the damage of DNA. E. histolytica contains its own defense mechanism to survive against the oxidative stress (Biswas et al. 2021; Dam et al. 2019b). The trophozoites of E. histolytica are found to coexist with malignancies, including lung adenocarcinoma, cervical squamous carcinoma, perineal carcinoma, and sigmoid and colonic adenocarcinoma (Varet et al. 2018). Chronic intestinal amoebiasis sometimes manifests into a tumorous, inflammatory mass, called ameboma. Ameboma can be formed in patients with invasive amoebiasis (Jaiswal et al. 2015).
Blastocystis hominis
Blastocystis hominis is an enteric protozoan parasite having a controversial pathogenic potential and reported to be associated with CRC. Stimulation with Blastocystis spp. antigen results in increased proliferation of HCT116 cells. Colon cancer cells produce higher levels of IL-6 and IL-8. IL-6 helps in the proliferation of human colon and colorectal carcinoma cells. Peripheral blood mononuclear cells (PBMCs) and HCT116 cells treated with Blastocystis spp. antigen show differential patterns of IL-6, IL-8, TNF-α, IFN-γ, proapoptotic p53, and cathepsin B. The Blastocystis ST7-produced cysteine protease cathepsin B has been associated with enhanced Caco-2 cell monolayer permeability. Cathepsin B in high concentrations may intensify colon cancer cells by diminishing the cellular immune response. Blastocystis spp. isolated from symptomatic patients causes oxidative damage in the animal model, suggesting the role of oxidative stress in developing the pathophysiology of cancer (Kumarasamy et al. 2013).
Giardia lamblia
Giardia lamblia, the causative agent of giardiasis, has been found to coexist with tumor masses in the pancreas and gallbladder in some sporadic cases. In adenocarcinoma, the presence of Giardia parasite may be speculated for having a potential relationship between giardiasis and carcinogenesis (Hurnik et al. 2019).
Therapeutic Roles of Probiotics in Cancer Treatment and Prevention
Probiotics play an important and protective role against cancer development. They are now being used as an alternative drug for the treatment of various cancers. This is because they may possess several factors compared to other bacteria. The role of various probiotic strains for the prevention and treatment of cancer is listed in Table 1 and Fig. 2.
Role of probiotics in the prevention of cancer. (1) Probiotic microorganisms produce antimicrobial substances such as bacteriocins that inhibit the growth of various pathogens. They also produce some organic acids that lower intestinal pH, thereby preventing pathogenic adhesion in the intestinal epithelium. Lacticin 3147, a bacteriocin produced by Lactococcus lactis, inhibits C. difficile-associated diarrhea. (2) Mucins are the glycoproteins that are the major constituents of the epithelial mucus layer. Several probiotics promote mucous secretion to improve epithelial barrier function. Adhesion of enteropathogenic E. coli (EPEC) is inhibited by L. plantarum 299v, and this probiotic strain induces mucin secretion. (3) Pediococcus acidilactici K15 (PA) plays a role in the production of IgA in PBMCs. The secretion of IgA in the intestinal mucosa is important to improve host defense against pathogens. Blimp-1, BAFF, and APRIL are involved in the innate pathway of IgA production from B cells. LAB contains several kinds of TLR ligands and activates DCs to secrete many kinds of cytokines such as IL-5, IL-6, and IL-10. These cytokines promote the differentiation of plasma cells that are involved in IgA production. (4) Lactobacillus suntoryeus HY7801 (LS) inhibits TLR-4 mediated NF-κβ activation. This decreases the expression of pro-inflammatory cytokines such as IL-1β, IL-6, COX-2, and TNF-α. The activity of harmful bacterial enzymes such as β-glucuronidase and hyaluronidase is significantly reduced by HY7801. (5) Antioxidative role of probiotics. (a) VSL#3, a probiotic mixture containing Streptococcus salivarius subsp. thermophilus, Lactobacillus casei, L. plantarum, L acidophilus, L. delbrueckii subsp. bulgaricus, Bifidobacterium longum, B infantis, and B. breve, produces a soluble factor that inhibits the activity of proteasome after an early exposure of the probiotic-conditioned media. VSL#3 treatment reduces the release of MCP-1 in response to NF-κβ activation by TNF-α. The expression of anti-inflammatory and cytoprotective HSPs such as HSP 25 and HSP 72 is increased, and oxidative stress is reduced in colonic epithelial cells after probiotic treatment. (b) Lactobacillus rhamnosus GG (LGG) produces soluble proteins p40 and p75 that alleviate H2O2-induced disruption of tight junctions and TER. Pretreatment with p40 or p75 blocks the selective inhibitors such as U0126 (MAP kinase inhibitor) and Ro-32-0432 (PKC inhibitor) that results in the activation of extracellular signal-regulated kinases 1 and 2 (ERK1/2, a subfamily of MAPK) and PKC isoforms PKCβ1 and PKCɛ. The activation of ERK1/2 and PKC isoforms protects junction proteins such as ZO-1, occludin, E-cadherin, and β-catenin from oxidative stress-induced redistribution. (6) Antiproliferative and apoptotic role of probiotics and short-chain fatty acids. (a) Lactococcus lactis ssp. lactis (L. lactis) exerts antiproliferative effects on the SNU-1 human stomach cancer cells by arresting G0/G1 phase, increasing the expression of p53 and p21, and reducing the level of cyclin D1. (b) SCFAs such as butyrate and propionate play an important role in the induction of apoptosis. Butyrate increases the expression of p21 and induces HDAC inhibition, causing cell cycle arrest at G1 phase. Propionate induces apoptosis in cancer cells by activating p21 and caspases. (7) Probiotic Enterococcus faecium M74 can detoxify the carcinogens, aflatoxin B1 and patulin. (8) β-Glucuronidase and hyaluronidase are the harmful enzymes, produced by intestinal bacteria such as Clostridium perfringens, Bacteroides fragilis, Clostridium paraputrificum, Bacteroides vulgatus, Bacteroides uniformis, Ruminococcus gnavus, Staphylococcus, Peptostreptococcus, and Eubacterium. This enzyme produces carcinogenic aglycones by hydrolyzing β-glucuronides. Elevated levels of β-glucuronidase enzyme in plasma increases the risk of developing cancer such as CRC, breast cancer, and prostate cancer. Probiotics, such as B. longum SPM1207, L. paracasei 0908, L. paracasei 0919, and Lactobacillus acidophilus can inhibit the activity of harmful bacterial enzymes that can convert pro-carcinogens (ProC) to active carcinogens (ActiveC)
Production of Antimicrobial Substances
Inappropriate use of antibiotics has created the worldwide emergence of resistant microorganisms. Nowadays, the biomedical importance of antimicrobial peptides is being explored as novel therapeutics for several diseases. Antimicrobial peptides (AMPs) are the small biologically active molecules, produced by organisms through their innate immune system. Bacteriocins are small AMPs produced by bacteria including probiotics. A few reports have suggested that AMPs including bacteriocins have cytotoxic effects against cancer cells. Probiotic E. coli Nissle 1917 induces the mucosal epithelium to produce human β-defensin 2, an AMP having an ability to control adherence and invasion (Schlee et al. 2007). Lactobacillus brevis strain 925A produces a bacteriocin, brevicin 925A, which shows an effective role against dental caries and food poisoning pathogens like Streptococcus mutans and Listeria monocytogenes. Lactococcus lactis produces lacticin 3147, a bacteriocin that inhibits C. difficile-associated diarrhea. B. bifidum NCFB 1454 produces bifidocin B that shows bacteriocin activity against Gram-positive bacteria. Lactococcus lactis produces two naturally occurring variants of bacteriocins, Nisin Z and A, having an antitumor potential against head and neck squamous cell carcinoma. Moreover, it shows antimicrobial activity against periodontal pathogens including Porphyromonas gingivalis, Treponema denticola, and Fusobacterium nucleatum, which are responsible for oral cancer (Kamarajan et al. 2020).
Improvement of Intestinal Barrier
Diffusion of potential detrimental factors from the intestinal lumen into the tissue is prevented by the intestinal epithelial junctional complex. Disruption of epithelial junctional complex leads to the loss of mucosal integrity and barrier function that eventually increases the permeability to allergens, pathogens, and toxic substances (Rao and Samak 2013). Some of the proteins such as scaffold protein (ZO) and transmembrane proteins (occludin and claudin) are localized and involved in the formation of tight junctions. Probiotic L. rhamnosus GG prevents changes in occludin, ZO-1, E-cadherin, and β-catenin due to oxidative stress by the activation of ERK1/2 (a subfamily of MAPK) and PKC isoforms PKCβ1 and PKCε. Bifidobacterium bifidum OLB6378 exerts protective effects against necrotizing enterocolitis injury by lowering the inflammation in the ileum and improving intestinal integrity. Lactobacillus fructosus C2 can exert a therapeutic effect against enterotoxigenic E. coli or S. typhimurium infection (Yu et al. 2015). Butyrate-producing probiotic Clostridium butyricum MIYAIRI 588 improves the expression of tight junction proteins and reduces inflammatory indexes and serum endotoxin levels (Endo et al. 2013).
Modulation of the Immune System
Probiotic microorganisms produce molecules with immune-regulatory and anti-inflammatory functions that can modulate the host immune system by stimulating dendritic cells (DCs) and natural killer (NK) cells of the innate immune system. The primary immune response is triggered by different pattern recognition receptors like Toll-like receptors (TLRs) and C-type lectin receptors (CLRs) expressed on various immune cells like DCs, NKs, and non-immune cells such as epithelial cells, endothelial cells, and fibroblast cells (Bermudez-Brito et al. 2012). TNF-α stimulates NF-κβ, which initiates the transcription of a series of genes including IL-8, IL-6, IL-1β, COX-2, and p-65. Lactobacillus rhamnosus GG enhances the expression of TLR-9 that attenuates TNF-α-enhanced NF-κβ activity (Ghadimi et al. 2010). Lactobacillus suntoryeus HY7801 inhibits TLR-4-linked NF-κβ activation and decreases the expression of pro-inflammatory cytokines such as IL-1β, IL-6, and TNF-α. Thus, it can lower the activities of harmful intestinal bacterial enzymes such as β-glucuronidase.
Antioxidant Properties of Probiotics
Oxidative stress can be generated in host cells by various endogenous and exogenous factors. Probiotic microorganisms exert antioxidant activity in different ways such as production of antioxidant enzymes (Fe-SOD and Mn-SOD), secretion of antioxidant metabolites (butyrate and folate), and modulation of molecular signaling pathway (Dam et al. 2019a).
Superoxide, a reactive oxygen species, is abundantly produced by the mitochondria and catalyzed by SOD into hydrogen peroxide and water. Lactobacillus fermentum E-3 and E-18, L. casei BL23, and L. lactis are few examples of probiotic strains that produce antioxidative enzymes such as catalase and SOD that can prevent oxidative stress (LeBlanc et al. 2011).
Probiotic Clostridium butyricum MIYAIRI 588 strain produces butyrate that suppresses hepatic oxidative stress, improves oxidative stress-induced damages, and reduces nonalcoholic fatty liver disease (Endo et al. 2013). Probiotic bacteria of the genera Lactobacillus and Bifidobacterium can produce folate, and Lactobacillus helveticus can produce 5-methyltetrahydrofolate, a folic acid derivative. The intracellular cell-free extract of Lactobacillus helveticus CD6 can scavenge DPPH radical and chelate Fe2+ and inhibits the rate of ascorbate autoxidation (Ahire et al. 2013). Folate availability affects the efficiency of DNA methylation and gene expression, whereas folate deficiency leads to DNA hypomethylation that results in overexpression of oncogenes and inactivation of tumor suppressor genes. Even low folate intake may enhance the chance of breast cancer among postmenopausal women (Sellers et al. 2001).
The extracellular polysaccharide secreted from Bacillus sp. strain LBP32 prevents inflammation induced by lipopolysaccharide from Escherichia coli 0111:B4 in RAW 264.7 cells. It also inhibits the release of pro-inflammatory cytokines, activation of NF-κβ, and ROS production (Diao et al. 2014). Several enzymes (COX, CYP, and NOX) are involved in producing ROS. Mucosal expression of COX-2 is downregulated in H. pylori-infected Mongolian gerbils upon the treatment of Lacidofil, a mixture of probiotic Lactobacillus rhamnosus and Lactobacillus acidophilus (Brzozowski et al. 2006).
Antiproliferative Activity of Probiotics
Uncontrolled cell proliferation if unchecked by apoptosis can lead to cancer progression. Probiotic microorganisms inhibit growth and proliferation of cancerous cells. Probiotic bacteria are the focus of research in recent days because of their anticancer properties. However, they can do it through a combination of versatile processes that includes the suppression of the microbial growth accountable for the production of mutagens and carcinogens, the protection of DNA from oxidative damage, the alteration of carcinogen metabolism, and the regulation of expression of various genes involved in cell death and apoptosis. Short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate are produced from complex carbohydrates by the intestinal microbiota and play an essential role in suppressing carcinogenesis (Adom and Nie 2013). Several probiotic strains modulate the gut microbiota composition by increasing SCFAs producing bacterial count. SCFAs can bind with various G-protein-coupled receptors (GPRs) such as GPR41, GPR43, and GPR109. GPR43 plays an effective role in the induction of apoptosis and regulation of cell proliferation. Propionate exerts an anti-tumor effect in colon cancer cells via GPR43. GPR43/propionate treatment reduces the level of proliferating cell nuclear antigen and enhances apoptotic cell death. GPR43 with propionate acts as an apoptosis inducer and a tumor suppressor in colon cancer (Tang et al. 2011). Application of B. lactis significantly enhances the production of SCFA, and that can give protection from the development of CRC (Le Leu et al. 2010). Butyrate effectively regulates cell proliferation by inhibiting histone deacetylase (HDAC), which in turn leads to the overexpression of p21. This eventually leads to the cell cycle arrest at G1 phase in cancer cells and thus inhibits colon carcinogenesis (Adom and Nie 2013). Probiotic microorganisms reduce the activity of harmful enzymes β-glucuronidase and β-glucosidase. β-Glucuronidase hydrolyzes β-glucuronides and produces carcinogenic aglycones. The elevated level of β-glucuronidase enzyme in plasma increases the risk of developing colorectal cancer, breast cancer, and prostate cancer (Mroczynska et al. 2013). Probiotic bacteria B. longum SPM1207 and Lactobacillus acidophilus play an important role in inhibiting the activity of such harmful enzymes (Lee et al. 2009).
Future Perspective
Extensive epidemiological evidences indicate the role of microbes in inducing 20% of all cancers. The use of probiotic bacteria is becoming a promising tool in cancer therapy. The world market for probiotics is growing at an estimated yearly rate of 7%. Although probiotic treatment has emerged as an effective alternative to combat the severity of cancer, lack of clinical and preclinical studies and some unwanted side effects demand caution during its application on humans. It is rarely used in routine clinical practice as there are very few commercially available strains. The exact bioactive component of the probiotics that provides beneficial effects should be addressed in order to step up the basic studies into clinical trials. Although the scenario of probiotics in cancer therapy seems alluring, the advancement is not linear. Safety assessment of probiotics seems to be the biggest issue at this point. Identification of the most beneficial strains for cancer prevention in humans necessitates a large database as a starting point. Novel engineered probiotic microorganisms may offer new insights into therapeutic usage for the prevention and treatment of cancer. More clinical and preclinical studies are needed to gain the most effective outcome from probiotic therapy in regulating a targeted human flora that may aid in the development of personalized medicine in the future.
Abbreviations
- 4-HNE:
-
4-Hydroxynonenal
- 8-OHdG:
-
8-Hydroxydeoxyguanosine
- 8-oxo-dG:
-
8-Oxo-2′-deoxyguanosine
- ADH:
-
Alcohol dehydrogenase
- AID:
-
Activation-induced cytidine deaminase
- AMPK:
-
Adenosine monophosphate-activated protein kinase
- AMPs:
-
Antimicrobial peptides
- APC:
-
Anaphase promoting complex
- APRIL:
-
A proliferation-inducing ligand
- AQP3:
-
Aquaporin 3
- ATP:
-
Adenosine triphosphate
- AvrA:
-
Avirulence protein A
- BAD:
-
BCL-2-associated death promoter
- BAFF:
-
B cell-activating factor
- BAX:
-
BCL-2 associated X
- BCL-2:
-
B-cell lymphoma 2
- BER:
-
Base excision repair
- BFT:
-
B. fragilis toxin
- BLIMP:
-
B lymphocyte-induced maturation protein 1
- cagA:
-
Cytotoxin-associated gene A
- CD:
-
Crohn’s disease
- CDKs:
-
Cyclin-dependent kinases
- CDT:
-
Cytolethal distending toxin
- CIDR:
-
Succeeding cysteine-rich interdomain region
- CLRs:
-
C-type lectin receptors
- CNF1:
-
Cytotoxic necrotizing factor 1
- COX:
-
Cyclooxygenase
- CRC:
-
Colorectal cancer
- CTCL:
-
Cutaneous T-cell lymphoma
- CTL:
-
Cytotoxic T lymphocytes
- CXCL:
-
C-X-C motif chemokine ligand
- CYP:
-
Cytochrome P450
- DC:
-
Dendritic cell
- DDR:
-
DNA damage responses
- DNA:
-
Deoxyribonucleic acid
- DNase I:
-
Deoxyribonuclease I
- DPPH:
-
2,2-Diphenyl-1-picrylhydrazyl
- DSBs:
-
Double-strand breaks
- EBV:
-
Epstein-Barr virus
- ERK:
-
Extracellular regulated kinase
- ETBF:
-
Enterotoxigenic B. fragilis
- Etk/BMX:
-
Epithelial and endothelial tyrosine kinase/bone marrow X
- FOXO3a:
-
Forkhead box O3a
- GEC:
-
Gingival epithelial cell
- GI:
-
Gastrointestinal
- GPRs:
-
G-protein-coupled receptors
- GPX1:
-
Glutathione peroxidase 1
- HCC:
-
Hepatocellular carcinoma
- HDAC:
-
Histone deacetylase
- HIF-1α:
-
Hypoxia-inducible factor 1α
- HNE:
-
4-Hydroxy-2-nonenal
- HRE:
-
Hypoxia response element
- HSP:
-
Heat shock protein
- IARC:
-
International Agency for Research on Cancer
- IBD:
-
Inflammatory bowel disease
- IFN-γ:
-
Interferon-γ
- IgA:
-
Immunoglobulin A
- IL:
-
Interleukin
- JAK1/STAT3:
-
Janus kinase 1/signal transducer and activator of transcription 3
- JNK:
-
c-Jun N-terminal kinases
- LPS:
-
Lipopolysaccharide
- MALT:
-
Mucosa-associated lymphoid tissue
- MDA:
-
Malondialdehyde
- MDSC:
-
Myeloid-derived suppressor cells
- miRNA:
-
MicroRNA
- NDK:
-
Nucleoside diphosphate kinase
- NF-κβ:
-
Nuclear factor κ light-chain enhancer of activated B cells
- NK:
-
Natural killer
- NLRX1:
-
NOD-like receptor family member X1
- NO:
-
Nitric oxide
- NOX:
-
NADPH oxidase
- Nrf2:
-
Nuclear factor erythroid 2-related factor 2
- OSCC:
-
Oral squamous cell carcinoma
- PBMC:
-
Peripheral blood mononuclear cells
- PfEMP1:
-
P. falciparum erythrocyte membrane protein 1
- PGN:
-
Peptidoglycan
- PI3K/Akt:
-
Phosphatidylinositol 3-kinase/protein kinase B
- PKC:
-
Protein kinase C
- pro-MMP-9:
-
Pro-matrix metalloproteinase-9
- PTEN:
-
Phosphatase and tensin homolog deleted on chromosome 10
- RNI:
-
Reactive nitrogen intermediates
- RNS:
-
Reactive nitrogen species
- ROI:
-
Reactive oxygen intermediate
- ROS:
-
Reactive oxygen species
- SabA:
-
Sialic acid–binding adhesin
- SCFA:
-
Short-chain fatty acid
- SE:
-
Staphylococcal enterotoxin
- Sir2:
-
Silent information regulator 2
- SMO:
-
Spermine oxidase
- SNP:
-
Single-nucleotide polymorphism
- SOD2:
-
Superoxide dismutase 2
- T4SS:
-
Type IV secretion systems
- TER:
-
Transepithelial resistance
- TGF-β:
-
Tumor growth factor β
- TLR:
-
Toll-like receptor
- TNF-α:
-
Tumor necrosis factor α
- UC:
-
Ulcerative colitis
- VacA:
-
Vacuolating cytotoxin A
- WHO:
-
World Health Organization
- Wnt:
-
Wingless-related integration site
- ZO:
-
Zonula occludens
References
Abdul-Sater AA et al (2010) Enhancement of reactive oxygen species production and chlamydial infection by the mitochondrial Nod-like family member NLRX1. J Biol Chem 285:41637–41645. https://doi.org/10.1074/jbc.M110.137885
Adom D, Nie D (2013) Regulation of autophagy by short chain fatty acids in colon cancer cells. In: Bailly Y (ed) Autophagy - a double-edged sword. IntechOpen, Rijeka. https://doi.org/10.5772/54999
Ahire JJ, Mokashe NU, Patil HJ, Chaudhari BL (2013) Antioxidative potential of folate producing probiotic Lactobacillus helveticus CD6. J Food Sci Technol 50:26–34. https://doi.org/10.1007/s13197-011-0244-0
Al-hebshi NN, Al-Alimi A, Taiyeb-Ali T, Jaafar N (2015) Quantitative analysis of classical and new putative periodontal pathogens in subgingival biofilm: a case-control study. J Periodontal Res 50:320–329. https://doi.org/10.1111/jre.12210
Arthur JC et al (2012) Intestinal inflammation targets cancer-inducing activity of the microbiota. Science 338:120–123. https://doi.org/10.1126/science.1224820
Benamrouz S et al (2014) Cryptosporidium parvum-induced ileo-caecal adenocarcinoma and Wnt signaling in a mouse model. Dis Model Mech 7:693–700. https://doi.org/10.1242/dmm.013292
Bermudez-Brito M, Plaza-Diaz J, Munoz-Quezada S, Gomez-Llorente C, Gil A (2012) Probiotic mechanisms of action. Ann Nutr Metab 61:160–174. https://doi.org/10.1159/000342079
Bhattacharyya A, Chattopadhyay R, Mitra S, Crowe SE (2014) Oxidative stress: an essential factor in the pathogenesis of gastrointestinal mucosal diseases. Physiol Rev 94:329–354. https://doi.org/10.1152/physrev.00040.2012
Binder Gallimidi A et al (2015) Periodontal pathogens Porphyromonas gingivalis and Fusobacterium nucleatum promote tumor progression in an oral-specific chemical carcinogenesis model. Oncotarget 6:22613–22623. https://doi.org/10.18632/oncotarget.4209
Biswas P, Ghosh R, Das M, Pal S, Dam S (2021) Molecular characterization of EhAK6, an endonuclease V domain-containing aurora kinase protein from Entamoeba histolytica: protein-protein interaction, docking and functional aspect. Curr Res Biotechnol 3:225–234. https://doi.org/10.1016/j.crbiot.2021.07.003
Block K, Gorin Y (2012) Aiding and abetting roles of NOX oxidases in cellular transformation. Nat Rev Cancer 12:627–637. https://doi.org/10.1038/nrc3339
Boyer L et al (2004) Rac GTPase instructs nuclear factor-kappaB activation by conveying the SCF complex and IkBalpha to the ruffling membranes. Mol Biol Cell 15:1124–1133. https://doi.org/10.1091/mbc.e03-05-0301
Brzozowski T et al (2006) Effect of probiotics and triple eradication therapy on the cyclooxygenase (COX)-2 expression, apoptosis, and functional gastric mucosal impairment in Helicobacter pylori-infected Mongolian gerbils. Helicobacter 11:10–20. https://doi.org/10.1111/j.0083-8703.2006.00373.x
Candela M, Turroni S, Biagi E, Carbonero F, Rampelli S, Fiorentini C, Brigidi P (2014) Inflammation and colorectal cancer, when microbiota-host mutualism breaks. World J Gastroenterol 20:908–922. https://doi.org/10.3748/wjg.v20.i4.908
Chaturvedi AK et al (2010) Chlamydia pneumoniae infection and risk for lung cancer. Cancer Epidemiol Biomark Prev 19:1498–1505. https://doi.org/10.1158/1055-9965.EPI-09-1261
Cid TP, Fernandez MC, Benito Martinez S, Jones NL (2013) Pathogenesis of Helicobacter pylori infection. Helicobacter 18(Suppl 1):12–17. https://doi.org/10.1111/hel.12076
Costa Pereira C et al (2017) Association between polymorphisms in antioxidant genes and inflammatory bowel disease. PLoS One 12:e0169102. https://doi.org/10.1371/journal.pone.0169102
Dai Z et al (2019) The role of microbiota in the development of colorectal cancer. Int J Cancer 145:2032–2041. https://doi.org/10.1002/ijc.32017
Dam B, Misra A, Banerjee S (2019a) Role of gut microbiota in combating oxidative stress. In: Oxidative stress in microbial diseases, pp 43–82. https://doi.org/10.1007/978-981-13-8763-0_4
Dam S, Biswas P, Ghosh R (2019b) Oxidative stress in Entamoeba histolytica. In: Oxidative stress in microbial diseases, pp 257–280. https://doi.org/10.1007/978-981-13-8763-0_14
Davidsson S et al (2016) Frequency and typing of Propionibacterium acnes in prostate tissue obtained from men with and without prostate cancer. Infect Agent Cancer 11:26. https://doi.org/10.1186/s13027-016-0074-9
Dejea C, Wick E, Sears CL (2013) Bacterial oncogenesis in the colon. Future Microbiol 8:445–460. https://doi.org/10.2217/fmb.13.17
Diao Y et al (2014) Extracellular polysaccharide from Bacillus sp. strain LBP32 prevents LPS-induced inflammation in RAW 264.7 macrophages by inhibiting NF-kappaB and MAPKs activation and ROS production. Int Immunopharmacol 18:12–19. https://doi.org/10.1016/j.intimp.2013.10.021
Endo H, Niioka M, Kobayashi N, Tanaka M, Watanabe T (2013) Butyrate-producing probiotics reduce nonalcoholic fatty liver disease progression in rats: new insight into the probiotics for the gut-liver axis. PLoS One 8:e63388. https://doi.org/10.1371/journal.pone.0063388
Ferreira RM, Machado JC, Figueiredo C (2014) Clinical relevance of Helicobacter pylori vacA and cagA genotypes in gastric carcinoma. Best Pract Res Clin Gastroenterol 28:1003–1015. https://doi.org/10.1016/j.bpg.2014.09.004
Fijan S (2014) Microorganisms with claimed probiotic properties: an overview of recent literature. Int J Environ Res Public Health 11:4745–4767. https://doi.org/10.3390/ijerph110504745
Ghadimi D, Vrese M, Heller KJ, Schrezenmeir J (2010) Effect of natural commensal-origin DNA on toll-like receptor 9 (TLR9) signaling cascade, chemokine IL-8 expression, and barrier integritiy of polarized intestinal epithelial cells. Inflamm Bowel Dis 16:410–427. https://doi.org/10.1002/ibd.21057
Guerra L, Cortes-Bratti X, Guidi R, Frisan T (2011) The biology of the cytolethal distending toxins. Toxins (Basel) 3:172–190. https://doi.org/10.3390/toxins3030172
Gulve N, Prusty BK, Rudel T (2019) Chlamydia trachomatis impairs host base excision repair by downregulating polymerase beta. Cell Microbiol 21:e12986. https://doi.org/10.1111/cmi.12986
Ha NH et al (2015) Prolonged and repetitive exposure to Porphyromonas gingivalis increases aggressiveness of oral cancer cells by promoting acquisition of cancer stem cell properties. Tumour Biol 36:9947–9960. https://doi.org/10.1007/s13277-015-3764-9
Han YW (2015) Fusobacterium nucleatum: a commensal-turned pathogen. Curr Opin Microbiol 23:141–147. https://doi.org/10.1016/j.mib.2014.11.013
Hurnik P et al (2019) Another case of coincidental Giardia infection and pancreatic cancer. Parasitol Int 71:160–162. https://doi.org/10.1016/j.parint.2019.04.013
Inaba H, Amano A, Lamont RJ, Murakami Y (2015) Involvement of protease-activated receptor 4 in over-expression of matrix metalloproteinase 9 induced by Porphyromonas gingivalis. Med Microbiol Immunol 204:605–612. https://doi.org/10.1007/s00430-015-0389-y
Jaiswal SS, Mehra R, Pattnaik MR (2015) Amoeboma-lest we forget!!! Indian J Surg 77:190–192. https://doi.org/10.1007/s12262-015-1267-y
Kamarajan P et al (2020) Periodontal pathogens promote cancer aggressivity via TLR/MyD88 triggered activation of integrin/FAK signaling that is therapeutically reversible by a probiotic bacteriocin. PLoS Pathog 16:e1008881. https://doi.org/10.1371/journal.ppat.1008881
Khan S, Imran A, Khan AA, Abul Kalam M, Alshamsan A (2016) Systems biology approaches for the prediction of possible role of Chlamydia pneumoniae proteins in the etiology of lung cancer. PLoS One 11:e0148530. https://doi.org/10.1371/journal.pone.0148530
Kostic AD et al (2012) Genomic analysis identifies association of Fusobacterium with colorectal carcinoma. Genome Res 22:292–298. https://doi.org/10.1101/gr.126573.111
Krejsgaard T et al (2014) Staphylococcal enterotoxins stimulate lymphoma-associated immune dysregulation. Blood 124:761–770. https://doi.org/10.1182/blood-2014-01-551184
Kumarasamy V, Kuppusamy UR, Samudi C, Kumar S (2013) Blastocystis sp. subtype 3 triggers higher proliferation of human colorectal cancer cells, HCT116. Parasitol Res 112:3551–3555. https://doi.org/10.1007/s00436-013-3538-5
Kurkivuori J et al (2007) Acetaldehyde production from ethanol by oral streptococci. Oral Oncol 43:181–186. https://doi.org/10.1016/j.oraloncology.2006.02.005
Landskron G, De la Fuente M, Thuwajit P, Thuwajit C, Hermoso MA (2014) Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res 2014:149185. https://doi.org/10.1155/2014/149185
Le Leu RK, Hu Y, Brown IL, Woodman RJ, Young GP (2010) Synbiotic intervention of Bifidobacterium lactis and resistant starch protects against colorectal cancer development in rats. Carcinogenesis 31:246–251. https://doi.org/10.1093/carcin/bgp197
LeBlanc JG et al (2011) Use of superoxide dismutase and catalase producing lactic acid bacteria in TNBS induced Crohn’s disease in mice. J Biotechnol 151:287–293. https://doi.org/10.1016/j.jbiotec.2010.11.008
Lee DK et al (2009) Lactic acid bacteria affect serum cholesterol levels, harmful fecal enzyme activity, and fecal water content. Lipids Health Dis 8:21. https://doi.org/10.1186/1476-511X-8-21
Lee CU et al (2015) Redox modulation of PTEN phosphatase activity by hydrogen peroxide and bisperoxidovanadium complexes. Angew Chem Int Ed Eng 54:13796–13800. https://doi.org/10.1002/anie.201506338
Liu X, Lu R, Xia Y, Wu S, Sun J (2010) Eukaryotic signaling pathways targeted by Salmonella effector protein AvrA in intestinal infection in vivo. BMC Microbiol 10:326. https://doi.org/10.1186/1471-2180-10-326
Lu R et al (2014) Enteric bacterial protein AvrA promotes colonic tumorigenesis and activates colonic beta-catenin signaling pathway. Oncogene 3:e105. https://doi.org/10.1038/oncsis.2014.20
Moodley Y et al (2012) Age of the association between Helicobacter pylori and man. PLoS Pathog 8:e1002693. https://doi.org/10.1371/journal.ppat.1002693
Mroczynska M, Galecka M, Szachta P, Kamoda D, Libudzisz Z, Roszak D (2013) Beta-glucuronidase and Beta-glucosidase activity in stool specimens of children with inflammatory bowel disease. Pol J Microbiol 62:319–325
Ng SC, Hart AL, Kamm MA, Stagg AJ, Knight SC (2009) Mechanisms of action of probiotics: recent advances. Inflamm Bowel Dis 15:300–310. https://doi.org/10.1002/ibd.20602
Pan C, Xu X, Tan L, Lin L, Pan Y (2014) The effects of Porphyromonas gingivalis on the cell cycle progression of human gingival epithelial cells. Oral Dis 20:100–108. https://doi.org/10.1111/odi.12081
Pinchuk IV, Beswick EJ, Reyes VE (2010) Staphylococcal enterotoxins. Toxins (Basel) 2:2177–2197. https://doi.org/10.3390/toxins2082177
Prusty BK, Krohne G, Rudel T (2013) Reactivation of chromosomally integrated human herpesvirus-6 by telomeric circle formation. PLoS Genet 9:e1004033. https://doi.org/10.1371/journal.pgen.1004033
Rao RK, Samak G (2013) Protection and restitution of gut barrier by probiotics: nutritional and clinical implications. Curr Nutr Food Sci 9:99–107. https://doi.org/10.2174/1573401311309020004
Robbiani DF et al.,. (2015). Plasmodium infection promotes genomic instability and AID-dependent B cell lymphoma. Cell 162:727–737. https://doi.org/10.1016/j.cell.2015.07.019
Rodriguez-Rivera LD, Bowen BM, den Bakker HC, Duhamel GE, Wiedmann M (2015) Characterization of the cytolethal distending toxin (typhoid toxin) in non-typhoidal Salmonella serovars. Gut Pathogens 7:19. https://doi.org/10.1186/s13099-015-0065-1
Rubinstein MR, Wang X, Liu W, Hao Y, Cai G, Han YW (2013) Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/beta-catenin signaling via its FadA adhesin. Cell Host Microbe 14:195–206. https://doi.org/10.1016/j.chom.2013.07.012
Satuman S et al (2021) The effect of acute and chronic infection-induced by AvrA protein of salmonella typhimurium on radical oxygen species, phosphatase and tensin homolog, and cellular homolog expression during the development of colon cancer. Open Access Macedonian J Med Sci 9:343–351. https://doi.org/10.3889/oamjms.2021.4945
Schlee M, Wehkamp J, Altenhoefer A, Oelschlaeger TA, Stange EF, Fellermann K (2007) Induction of human beta-defensin 2 by the probiotic Escherichia coli Nissle 1917 is mediated through flagellin. Infect Immun 75:2399–2407. https://doi.org/10.1128/IAI.01563-06
Sellers TA et al (2001) Dietary folate intake, alcohol, and risk of breast cancer in a prospective study of postmenopausal women. Epidemiology 12:420–428. https://doi.org/10.1097/00001648-200107000-00012
Simone O, Bejarano MT, Pierce SK, Antonaci S, Wahlgren M, Troye-Blomberg M, Donati D (2011) TLRs innate immunereceptors and Plasmodium falciparum erythrocyte membrane protein 1 (PfEMP1) CIDR1alpha-driven human polyclonal B-cell activation. Acta Trop 119:144–150. https://doi.org/10.1016/j.actatropica.2011.05.005
Sulzyc-Bielicka V et al (2018) Colorectal cancer and Cryptosporidium spp. infection. PLoS One 13:e0195834. https://doi.org/10.1371/journal.pone.0195834
Takahashi N, Nyvad B (2011) The role of bacteria in the caries process: ecological perspectives. J Dent Res 90:294–303. https://doi.org/10.1177/0022034510379602
Takaki A, Yamamoto K (2015) Control of oxidative stress in hepatocellular carcinoma: helpful or harmful? World J Hepatol 7:968–979. https://doi.org/10.4254/wjh.v7.i7.968
Tang Y, Chen Y, Jiang H, Robbins GT, Nie D (2011) G-protein-coupled receptor for short-chain fatty acids suppresses colon cancer. Int J Cancer 128:847–856. https://doi.org/10.1002/ijc.25638
Thirugnanam S, Rout N, Gnanasekar M (2013) Possible role of Toxoplasma gondii in brain cancer through modulation of host microRNAs. Infect Agent Cancer 8:8. https://doi.org/10.1186/1750-9378-8-8
Tjalsma H, Boleij A, Kato I (2012) Streptococcus bovis and colorectal cancer. In: Bacteria and cancer, pp 61–78. https://doi.org/10.1007/978-94-007-2585-0_3
Uitto VJ et al (2005) Fusobacterium nucleatum increases collagenase 3 production and migration of epithelial cells. Infect Immun 73:1171–1179. https://doi.org/10.1128/IAI.73.2.1171-1179.2005
Varet H et al (2018) Enteric bacteria boost defences against oxidative stress in Entamoeba histolytica. Sci Rep 8:9042. https://doi.org/10.1038/s41598-018-27086-w
Yong X et al (2016) Helicobacter pylori upregulates Nanog and Oct4 via Wnt/beta-catenin signaling pathway to promote cancer stem cell-like properties in human gastric cancer. Cancer Lett 374:292–303. https://doi.org/10.1016/j.canlet.2016.02.032
Yu Q, Yuan L, Deng J, Yang Q (2015) Lactobacillus protects the integrity of intestinal epithelial barrier damaged by pathogenic bacteria. Front Cell Infect Microbiol 5:26. https://doi.org/10.3389/fcimb.2015.00026
Yusof AM, Kumar S (2012) Phenotypic ‘variant’ forms of Trichomonas vaginalis trophozoites from cervical neoplasia patients. Exp Parasitol 131:267–273. https://doi.org/10.1016/j.exppara.2012.03.015
Zhou Y et al (2015) Noncanonical activation of beta-catenin by Porphyromonas gingivalis. Infect Immun 83:3195–3203. https://doi.org/10.1128/IAI.00302-15
Acknowledgments
The financial assistance from DAE-BRNS, Government of India (Project No. 37 (1)/20/15/2014-BRNS), and CSIR, Government of India (Project No. 27(0322)/17/EMR-II) is thankfully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Section Editor information
Rights and permissions
Copyright information
© 2022 Springer Nature Singapore Pte Ltd.
About this entry
Cite this entry
Biswas, P., Pal, S., Das, M., Dam, S. (2022). Microbe-Induced Oxidative Stress in Cancer Development and Efficacy of Probiotics as Therapeutics in Preventing Its Onset and Progression. In: Chakraborti, S. (eds) Handbook of Oxidative Stress in Cancer: Therapeutic Aspects. Springer, Singapore. https://doi.org/10.1007/978-981-16-5422-0_159
Download citation
DOI: https://doi.org/10.1007/978-981-16-5422-0_159
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-5421-3
Online ISBN: 978-981-16-5422-0
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences