Abstract
Transdermal administration is of high interest for drug delivery due to its non-invasiveness and easy dosing. However, this route of drug delivery faces the challenges of low drug permeability across the skin. This chapter reviews the role of ionic liquids (ILs) for transdermal delivery of active pharmaceutical ingredients (APIs). In particular, it focuses on the case of the Choline Geranate (CAGE), including its synthesis, structural features, physical properties, and enhanced permeation across epithelial barriers as a transdermal drug carrier. Its scale-up and medical applications are also discussed. This system has potential to become a powerful excipient to improve the pharmacokinetic profiles of many pharmaceutical products in transdermal applications.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
3.1 Introduction
Ionic liquids (ILs, loosely defined as salts with melting points below 100 °C (Welton 1999)) have attracted considerable attention in the field of pharmaceutical research due to their intrinsic tunable properties. In 1997, Chemical & Engineering News published their piece about ILs as “Designer Solvents” (Freemantle 1998) and effectively launched a renaissance in scientific and engineering interest in the field. In 2007, the concept of Active Pharmaceutical Ingredients ILs (API-ILs) was introduced (Hough et al. 2007), and soon thereafter IL-based systems have been proposed as solubilizers of poorly water-soluble active pharmaceutical ingredients (Jaitely et al. 2008; Mizuuchi et al. 2008), skin penetration enhancers (Sidat et al. 2019), and stabilizers for large molecules (Harada et al. 2018; Reslan and Kayser 2018).
Transdermal drug delivery is a non-parenteral administration technique that eliminates drug exposure to the gastrointestinal (GI) tract and first-pass metabolism. Instead, it delivers drugs locally to the skin to achieve systemic drug distribution and ensures the sustained and controlled release of drugs (Kalluri and Banga 2011). Although transdermal delivery offers advantages such as non-invasiveness and easy applicability, the properties of the skin barrier allow the permeation of only small (<500 Da) lipophilic molecules under normal conditions (Prausnitz and Langer 2008; Yang et al. 2017).
The rate-limiting barrier of the epidermis resides in the stratum corneum (SC). In other words, for the percutaneous absorption to occur, i.e., the penetration of substances into various layers of skin and permeation across the skin into the systemic circulation (Prausnitz et al. 2017; Brisson 1974) to take place, the drug must penetrate through the SC, the most superficial layer of the epidermis (Fig. 3.1). In general, once drug molecules cross the stratum corneal barrier, passage into deeper dermal layers and systemic uptake occurs relatively quickly and easily (Mehta 2004). Thus, permeability constant of water for SC is 1.1 × 10–7 cm/sec, while for dermis is 1.0 × 10–4 cm/sec, a 1000-fold faster (Brisson 1974). The SC has a thickness of 10–20 µm, composed of dead keratinocytes that are connected by glycoprotein, and produce the protein keratin which, together with the ceramide lipid component, form a dense structure (Prausnitz et al. 2017). Therefore, effective delivery of macromolecules across the skin, especially biologics which are becoming the major focus of pharmaceutical research, requires the use of perturbation methods to reduce skin barrier function.
Detailed representation of the epidermis layers of human skin. Reprinted with permission from Ramadon et al. Drug Delivery Transl Research, 2021 (Ramadon et al. 2021)
Several formulation-based approaches, comprising primarily of chemical permeation enhancers (CPEs) have also been developed (Karande et al. 2005,2004; Karande and Mitragotri 2009; Chen et al. 2014; Kim et al. 2008). The most common transdermal enhancers are ethanol, dimethylsulfoxide, Azone, terpenoids, and menthol ester derivatives. However, few of them are used clinically owing to their acute skin toxicity or irritation, as well as other safety issues that have not been clarified. Recently, ILs and deep eutectic solvents (DESs) have been introduced as a novel class of formulation-based approaches to enhance transdermal drug delivery for a wide range of molecules. The high tunability of these types of compounds allows achieving the desired physical, chemical, and biological properties of the CPE systems. This has generated immense research interests since the conventional CPEs have reached a plateau in terms of their discovery and efficacy.
The tunability of either ILs and/or DESs allows exploring different strategies, including their use as carriers (i.e., as solvents) solubilizing both hydrophilic and hydrophobic APIs of diverse classes, directly dissolving the API or in combination with oil, forming ionic liquid-in-oil microemulsion (Shamshina et al. 2018). A third option is the incorporation of the API into the IL composition, thus, changing the properties of the API itself (Shamshina et al. 2018). In this book chapter, we will review the latest attempts and strategies to use these systems as transdermal carriers, i.e., as potential replacements of CPEs.
3.2 Are These Systems ILs or DESs?
Here, we will not focus on ILs as a drug carrier vs. API-ILs, but the penetration of these systems through the skin. Usually, for APIs in the form of ILs (API-ILs), as well as for the IL as a drug carrier used in transdermal penetration, melting points below body temperature are targeted (Shamshina et al. 2018). The proper design with appropriate choice of counterions allows targeting the specific (<37 °C) melting point, and other targeted properties; here, we are interested mainly in dissolution capacity, permeability, and stability.
At the molecular level, the continuum of proton transfer vs. hydrogen bonding exists, and led to design rules for the “liquefaction” of higher melting salt forms, particularly through modulating ionicity of the ILs. As a result, liquefaction is achieved due to either complete proton transfer (classic IL systems) or due to the appearance of hydrogen bonding between two actives (“liquid co-crystals” or deep eutectics, classic DES systems) (Rebelo et al. 2007; Fei et al. 2006). One more strategy that results in liquefaction is an intentional change in the stoichiometry or complexity of the ions and/or complexes. Thus, ILs are defined as salts which melt below 100 °C, and DESs are eutectic mixtures of two or more distinct components which typically interact via strong hydrogen bonding, exist as mixtures of charged and neutral species, either in equimolar or non-stoichiometric ratios, and have a much lower melting point than the individual components (Zakrewsky et al. 2014a).
The first transdermally delivered IL was, indeed, one of the first API-ILs reported. It was reported by Rogers and coworkers (Hough et al. 2007) in 2007, and obtained by pairing lidocaine with sodium docusate, resulting in lidocaine docusate ([Lid][Doc]) IL, which was liquid at room temperature. The antinociceptive effect of this IL was superior to that of lidocaine as was evidenced by the improved and more extended therapeutic impact in a mouse model. Considering that fully ionized salts (e.g., metal salts, with each ion being solvated individually) normally diffuse poorly through lipid membranes, the result of the antinociceptive test was quite surprising. The next set of studies was reported by MacFarlane et al. (Stoimenovski and MacFarlane 2011). The study reported another example of transport of the pharmaceutically active ILs (protic ammonium salicylates) through a silicone membrane.
After a thorough spectroscopic investigation, it was found that even though it was initially suggested that API-ILs were composed entirely of dissociated ions, there is a wide range in the degree of ionicity in these liquid forms. ILs prepared by MacFarlane were even more permeable than corresponding inorganic salts, due to the formation of an ion-pair complex, and not separate solvated ions. Wang et al. expanded this approach showing that dual-active deep eutectics can form strong hydrogen-bonded complexes (i.e., DESs) without formal charges (Wang et al. 2014) in Lid·Ibu DES. When Lid·Ibu was dissolved in ethanol, the two actives were held together via strong hydrogen bond interactions, and simultaneously transported through a model silicone membrane, with almost identical transport rates of both. Park et al. hypothesized that such strongly hydrogen-bonded complexes might facilitate the transport of drugs through the skin, compared to commercial analogs (Park and Prauznitz 2010). These initial studies followed by extensive research and various degrees of ionicity were shown to exist in these systems, including deep eutectics, oligomeric ILs, etc., altogether termed liquid cocrystals (Bica and Rogers 2010; Kelley et al. 2013; Bica et al. 2011).
Indeed, it has been previously shown that by adding an excess of the neutral parent acid or base, it is possible to form materials that were termed “confused ionic liquids” (Bica and Rogers 2010). This included tetrabutylphosphonium salicylate ([P4444][Sal])/salicylic acid (HSal) salts [P4444][Hx(Sal)1+x] with no melting point, lidocainium salicylate salts ([HLid][Hx(Sal)1+x]), etc. With all these findings, Rogers has recently raised concern about the definition of the transdermally penetrating compound, CAGE (Choline And GEranate), that was presented in the literature as both an ionic liquid (IL) and deep eutectic solvent (DES), in a single phrase as “ionic liquid deep eutectic,” and pointed out the inappropriateness of the use of both mutually exclusive definitions simultaneously (Rogers and Gurau 2018). In reply to Rogers’ concern, the developers of CAGE, noted that the current definitions of either ILs or DESs are based on extreme behaviors and the reality is somewhere in the middle, and stated that “Our choline and geranate (CAGE) compound fits the definition of an IL since it comprises largely ionic species, cholinium and geranate, and has a melting point below 100 °C. At the same time, CAGE is not a classical IL since it also contains neutral geranic acid (Banerjee et al. 2018a).”
In our opinion, GAGE represents such an example of the formation of neither purely ionic nor neutral hydrogen-bonded oligomeric ions of parent acid and conjugate base, where the excess of geranic acid becomes tightly bound into the complex between choline and geranate, and the compound is still retaining the favorable properties of an IL; and suggest its proper structural formula would be [Cho][H(Ger)2] rather than commonly used [Cho][Ger]2, but we will use the ratio of the starting components to indicate the composition of the systems, to not confuse a reader even more.
The discussion of the nature of the components in solution is complex and sometimes not easy to elucidate. It is not limited to a discussion about proper nomenclature, but a critical and needed characterization, since it will determine the chemical and physical properties of the system and their potential applications (Kelley et al. 2013). As an example, the triethylammonium acetate system, although could be seen as a simple, protic ionic liquid, required extensive experimental studies to be classified as a complex system with oligomeric ions (Berton et al. 2018).
In the next sections, we will only focus on the effect of systems reported as transdermal carriers for active pharmaceutical ingredients, irrespective of the names assigned to the systems by the authors. For those systems still under discussion, such as CAGE, we will use the structural formula to avoid incorrect terminologies.
3.3 Using ILs as Transdermal Carriers
Recently, ILs and DESs (the definitions and differences between ILs and DESs were given and discussed above, but henceforth we will use structural formula or ratio in “tricky” cases) have demonstrated an excellent ability to enhance the permeation of macromolecules, acting as both enhancers and solvents in transdermal transport. An example of that is the study of Qi et al. who compared the performance of the 31 ammonium-based ILs with 44 conventional CPE systems for transdermal drug delivery, through examining the Attenuated Total Reflectance Fourier Transform Infrared (ATR-FTIR) spectra of skin SC exposed to both types of systems (Qi et al. 2020). Indeed, the ATR-FTIR allows to measure heterogeneity of SC and identifying lipid-rich and lipid-poor regions. The technique also allows determining the permeation and distribution of a drug (as well as solvents) into the SC.
When this analysis was conducted, a clear distinction was noted in the ATR-FTIR spectra after ILs and CPEs treatment, despite variations among each class: The former systems induced greater reductions in lipid peak areas but smaller reductions in the peaks of α-helixes of proteins (Qi et al. 2020). Karande et al. indicated that these two types of peaks have clear implications for transdermal drug delivery using CPEs, namely, that the extent of lipid extraction and fluidization was related to the potency of permeation enhancement, and the reduction in stable protein secondary structure correlated with the irritation potential (Karande et al. 2005). Based on the design principles that an ideal topical formulation should have strong permeation enhancement but low irritation potential, ILs exhibited a better performance than conventional CPEs.
Not only ammonium but choline ([Cho])-based systems were extensively studied. These systems were synthesized and tested to enhance skin penetration using mannitol as a model drug, chosen because of its hydrophobicity and thus low permeability into the skin (Zakrewsky et al. 2014b). The systems that were tested included choline urea (1:2 choline:urea ratio, Cho:Urea (1:2)), choline hexanoate (1:2 choline:hexanoic acid ratio, Cho:Hexanoic acid (1:2)), choline oleate (1:2 choline:oleic acid, Cho:Oleic acid (1:2)), choline geranate (1:2 choline:geranic acid, Cho:Geranic Acid (1:2), also abbreviated as CAGE), trihexyltetradecylphosphonium oleate ([P66614][Oleate]), trihexyltetradecylphosphonium hexanoate ([P66614][Hexanoate]), and trihexyltetradecylphosphonium geranate ([P66614][Ger]).
The systems Cho:Urea (1:2) and Cho:Hexanoic Acid (1:2), reduced the permeation of mannitol, in comparison to the saline control, while Cho:Oleic Acid (1:2) and [P66614][Oleate] showed no enhancement in skin permeation comparing with saline control. However, [P66614][Oleate] enhanced transport of mannitol into deep skin as much as fivefold, indicating potential topic applications. The systems [P66614][Hexanoate], Cho:Geranic Acid (1:2), and [P66614][Ger] showed a significant transdermal enhancement. The highest enhancement was observed using Cho:Geranic Acid (1:2), with nearly fivefold enhancement of total delivery and more than 10 times more drug penetrating deep tissue layers. These findings showed that the depth of penetration could be controlled by the proper design of the systems: [P66614][Oleate] resulted in enhanced delivery to the superficial layer of the skin, while [P66614][Hexanoate] and Cho:Geranic Acid (1:2) exhibited delivery primarily in the deep tissue layers, i.e., [P66614][Hexanoate] showing a preference for the epidermis and Cho:Geranic Acid (1:2) for the dermis.
The systems that showed enhancement of mannitol delivery were also tested for transdermal delivery of a model antibiotic, cefadroxil. All the tested systems delivered 15–20% of the applied dose, which translates to approximately fivefold enhancement of cefadroxil delivery into the skin. Again, Cho:Geranic Acid (1:2) led to the highest enhancement of cefadoxil delivery into the dermis (∼16-fold compared with the aqueous solution), while other similar systems led to various degrees of enhanced transport (Zakrewsky et al. 2014b).
Since this initial publication in 2014 about its exceptional properties as a transdermal carrier (Zakrewsky et al. 2014b), Cho:Geranic Acid (1:2) arose as a leading solubilizing agent, with optimal antibacterial, cytotoxic, and skin-permeating properties, and has recently been patented (Zakrewsky et al. 2019). It is such an interesting case with huge potential that there is a company formed based on the platform this drug provides—CAGE Bio Inc., that uses structural heterogeneity of cations and anions to enhance membrane permeation (The ionic liquid platform 2020). It is worth spending a bit more time discussing these systems.
3.4 Choline:Geranic Acid Systems as Case Study
Synthesis
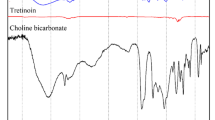
CAGE is typically synthesized by a salt metathesis reaction between choline bicarbonate and geranic acid (Fig. 3.2). The completion of the reaction is monitored through the evolution of CO2 gas. The CAGE is a clear, colorless to yellow colored liquid, with a pH ~ 8.5, conductivity ~1.3 mS/cm, and a characteristic odor.
Toxicity
The starting components of Cho:Geranic Acid (1:2), i.e., choline and geranic acid, belong to the Generally Recognized as Safe (GRAS) list (Choline chloride 2020; Cohen et al. 2020). In vitro tests using normal human bronchial epithelial (NHBE) cells as a model nonskin cell to assess potential toxicity in the event of systemic absorption, showed no toxicity for Cho:Geranic Acid (1:2) (Zakrewsky et al. 2014b). ATR-FTIR (i.e., changes to α-helix content in the SC) and reconstructed human epidermal cultures (EpiDerm) were used to assess its irritation potential: It was found that while geranic acid and choline showed significant irritation potential, Cho:Geranic Acid (1:2) showed no significant changes with respect to the control (Zakrewsky et al. 2014b).
GLP dermal toxicity of CAGE was also studied in minipigs (Ko et al. 2020a), considered to be an excellent model to study the toxicity of topical skin formulations. Studies were conducted using Göttingen minipigs, by applying the Cho:Geranic Acid (1:2) as a 40 wt% gel formulated in common pharmaceutical excipients; 1 ml of this gel was applied over 10% of the pig body area once a day for 91 consecutive days. CAGE showed no signs of toxicity—clinical (ocular, electrocardiography, hematology, coagulation, clinical chemistry, urine analysis, and organ weights parameters) or non-clinical (body weight changes, food consumption).
Biological Activity
Besides mannitol and cefadroxil, Cho:Geranic Acid (1:2) has shown to induce an excellent solubility (450 times, from 0.016 mg/mL in water to 7.2 mg/mL in Cho:Geranic Acid (1:2)) of Nobiletin (NOB), a poorly water-soluble flavonoid of low oral bioavailability (Hattori et al. 2019). In vitro transdermal tests showed that Cho:Geranic Acid (1:2) was effective in enhancing transdermal absorption of NOB, compared to other penetration enhancers, such as ethanol-phosphate buffered saline (EtOH:PBS), and glycol monoethyl ether (DGME, Transcutol), following the order Cho:Geranic Acid (1:2) > EtOH:PBS > PBS > DGME. Subsequent in vivo tests were performed applying the NOB/Cho:Geranic Acid (1:2) to the shaved back of Sprague–Dawley rats. The NOB/Cho:Geranic Acid (1:2) transdermal formulation was 20-times more bioavailable than the oral solid form of NOB. Furthermore, NOB/Cho:Geranic Acid (1:2) drug formulation showed significant drops of the blood glucose level due to the hypoglycemic activity of NOB in the rats. These results indicated that NOB/Cho:Geranic Acid (1:2) formulation was able to penetrate the SC layer while PBS can only deliver NOB to the skin surface.
The use of Cho:Geranic Acid (1:2) was not limited to the solubilization of hydrophobic molecules of small size but was extended to transdermal delivery of macromolecules. An increase of permeation of dextran of different molecular weights (Mw 4, 20, 40, 70, and 150 kDa) was reported using Cho:Geranic Acid (1:2), with >40-fold increase observed for intermediate-size dextran (Mw 20 kDa) over control (PBS) (Qi and Mitragotri 2019), opening the possibility of delivering proteins, peptides, and even antibodies. Thus, without the use of any additional physical/chemical penetration enhancement techniques, Cho:Geranic Acid (1:2) was able to deliver proteins such as bovine serum albumin (BSA, Mw ~66 kDa), ovalbumin (OVA, Mw ~45 kDa), and insulin (Mw ~5.8 kDa) across porcine skin and significantly reduce blood glucose levels in rats when insulin-CAGE was topically administered (Banerjee et al. 2017).
The penetration of BSA, OVA, and insulin from Cho:Geranic Acid (1:2) was also compared with the commonly used CPEs such as DGME and ethanol. In all cases, penetration of BSA, OVA, and insulin was significantly higher in the presence of Cho:Geranic Acid (1:2) than in the presence of common CPEs. A significant 40% drop in blood glucose levels was observed 4 h after insulin–Cho:Geranic Acid (1:2) was administered to rat skin, compared to other formulation controls. The pharmacokinetic performance of the delivered insulin was studied, and interestingly, unlike efficacy of injected insulin that drops over time, the efficacy of insulin Cho:Geranic Acid (1:2) formulation indicated a sustained profile as serum insulin levels plateaued, suggesting that Cho:Geranic Acid (1:2) can be used to achieve long-term glycemic control, thereby eliminating the need for frequent insulin injections, and notably improving compliance among diabetic patients. The safety and efficacy of the system using insulin as a model drug hold significant promise as a platform technology to deliver injectables through the buccal route. In addition, insulin dispersed in Cho:Geranic Acid (1:2) was also tested for oral delivery, and was efficiently absorbed by the gastrointestinal tract after being orally administered as capsules to rats, indicating that Cho:Geranic Acid (1:2) was applicable as an oral delivery vehicle of insulin as well (Banerjee et al. 2018b).
Little is known about the exact role of the system components in the transdermal transport of drugs. Existing studies have been limited, only reporting changes in the SC lipid content using FTIR, and led to the hypothesis that Cho:Geranic Acid (1:2) acts as a lipid extractor of SC components, improving the permeability of drugs across the skin (Qi and Mitragotri 2019; Banerjee et al. 2017).
Influence of Water
Considering transdermal delivery applications, the water present in the epidermis and the dermis might interact with Cho:Geranic Acid (1:2) and influence its structure. Assuming that the SC depth is 20 μm, the epidermis depth is 200 μm, and the water content is 70% by mass (Bielfeldt et al. 2009; Warner et al. 1988), then the amount of water was calculated as 1.1 vol% water in the SC and 10.2 vol% water in the epidermis, in the case of the application of 500 μL of Cho:Geranic Acid (1:2) to 4 cm2 skin (Takeda et al. 2021). Using Small-angle X-ray scattering (SAXS) and Nuclear Magnetic Resonance (NMR) analyses, it was shown that the addition of water up to 17% did not disturb the nanostructure of the CAGE substantially, that is, the structure of Cho:Geranic Acid (1:2) would be maintained within the skin when transdermally administered. When the amount of water exceeded 25 vol%, the viscosity of Cho:Geranic Acid (1:2) increased, and the IL exhibited low fluidity and formed micelles with an excess of water. This indicated that, even if the skin is highly hydrated, Cho:Geranic Acid (1:2) would form various structures such as lamellar and micellar phases. However, in a recent report, the authors indicated that with dilution, CAGE will gradually dissociate into its individual components (Ko et al. 2020b).
Structural Information
The important question that arises relates to ionic interactions that brought about such activity. To elucidate this, the ratio of Cho:Geranic Acid was explored by preparing not only the 1:2 Cho:Geranic Acid ratio, but also 1:1, 1:4, and 2:1 (Tanner et al. 2018). The new formulations were characterized using 1H NMR spectroscopy, which suggested that the degree of hydrogen bonding in these systems is increased with the ratio of geranic acid to choline. The degree of hydrogen bonding influenced the physical and chemical properties of the system and its interactions with the skin and the dissolved drug. Properties such as viscosity, conductivity, and water miscibility were determined. Both the viscosity, conductivity, and miscibility in water decreased with the concentration of geranic acid. The 1:1 variant did not follow the linear trend, with the conductivity being lower and the viscosity being higher than expected, indicating an ion-pairing between choline and geranate. As the hydrophobicity increases with the geranic acid, those compositions with higher concentrations of this component showed higher lipid removal from the SC and enabled the dissolution of hydrophobic molecules, whilst a higher choline content increases the hydrophilicity of the IL, dissolving more hydrophilic molecules.
The degree to which the ions in each variant interact with each other will also influence their interactions with both drugs and skin. The 1:2 system was shown to be composed of choline, geranic acid, and the geranate anion in a 1:1:1 ratio ([Cho][H(Ger)2]) which has been described as oligomeric (or confused) IL. 1H NMR spectra of CAGE indicated a chemical shift of the protons compared to the position of these in starting materials, more so for the protons localized adjacent to the quaternary nitrogen in choline (Ko et al. 2020a). Analysis of the FTIR spectrum showed the carbonyl peak in the geranic acid to be located at 1645 cm−1, while in CAGE an additional peak at 1549 cm−1 appears, not present in either precursor, indicating the formation of geranate. Magic-angle spinning (MAS) NMR, polarizing optical microscopy, small-angle X-ray scattering (SAXS), and mass spectrometry were used for the analysis of the closest analog of CAGE, GAGE-oct, where one equivalent of geranic acid was replaced with octanoic acid (Mann et al. 2020). Mass spectrometry and the 1H NMR chemical shift of CAGE-oct indicated a dynamic system, with H-exchange occurring between hydrogen-bonded/ionic complexes in [Cho][H(Ger)(Oct)], and this provides an insight into the [Cho][H(Ger)2] structural arrangement as well.
When the different systems were tested for in vitro delivery of insulin through the skin, it was observed that the systems containing 1:2 or 1:4 were effective in transporting the insulin through the SC, while neither the 2:1 nor the 1:1 samples—nor the starting materials—were able to transport the insulin into the skin (Tanner et al. 2018). These same systems were also tested for the transdermal delivery of the lipophilic drug ruxolitinib and the hydrophilic drug acarbose. In both cases, the delivery efficacy increased by approximately fourfold as the geranic acid content increased from 2:1 to 1:2 ratio, after which it plateaued, confirming that Cho:Geranic Acid (1:2) exhibited the highest delivery efficacy for hydrophilic as well as lipophilic drugs (Tanner et al. 2019).
The same model drugs, i.e., ruxolitinib and acarbose were used to compare the performance of Cho:Geranic Acid (1:2) with variants by replacing geranic acid with other organic acids in a 1:2 Cho:Organic Acid ratio, including citronellic acid, hexenoic acid, octanoic acid, octanoic acid, glutaric acid, decanoic acid, salicylic acid, and glycolic acid. As expected, the amount of drug delivered was dependent on the composition: In both cases, geranic acid outperformed other anions, followed by its close analog citronellic acid. Interestingly, octanoic acid, which possesses the same number of carbons as those in geranic acid backbone, performed well, ranked behind geranic acid and citronellic acid. Decanoic acid, on the other hand, which possesses an identical number of carbons as geranic acid, ranked very low and was poorly effective for both drugs. Octenoic acid ranked just below octanoic acid, like citronellic acid ranking below geranic acid, thus indicating that the enhancement is not simply a function of lipophilicity and that a single unsaturated bond makes an impact on delivery efficacy. Small anions including salicylic acid and glutaric acid were on the lower end of the ranking spectrum (Tanner et al. 2019). This is consistent with the expected mechanisms of action of ILs. Specifically, hydrophobic tails of anions and/or cations play a key role in the fluidization of the SC lipids. Since choline is highly hydrophilic and lacks long, aliphatic chains, the anions provide the primary mode of lipid disruption. Systematic modifications of the anion revealed that the ILs with the fewest interionic interactions were most successful at transdermal transport. Modifications of cations to further reduce the interionic interactions also improved delivery efficacy. The combination of the most effective cations and anions led to the selection of (2-hydroxyethyl)tributylammonium:citronellic acid (1:2 ratio) as the best delivery system, with 117.1 ± 12.7 µg cm−2 ruxolitinib measured in the dermis and acceptor after 24 h (Tanner et al. 2019).
Using the Cho:Geranic Acid (1:2) platform, similar ILs were synthesized at a stoichiometric ratio of 1:2 (cation:anion), and investigated to simultaneously stabilize small interfering RNAi (siRNA) and enhance its penetration into the skin following topical application (Mandal et al. 2020). The siRNA structure was found to be altered in the presence of Cho:Geranic Acid (1:2), Cho:Dimethylacrylic Acid (1:2), and Cho:Biphenyl-3-carboxylic Acid (1:2). On the other hand, Cho:Isovaleric Acid (1:2) and Cho:Phenylpropanoic Acid (1:2) retained the secondary structure of siRNA. The improved stability of siRNA in the presence of Cho:Phenylpropanoic Acid (1:2) suggested the possibility of synergistic effects between the ILs prepared from two structurally different anions. Consequently, the effect of IL mixtures on siRNA stability was assessed, to determine whether the compatibility of Cho:Phenylpropanoic Acid (1:2) with siRNA might offer additional protection against the adverse effects of Cho:Geranic Acid (1:2) and Cho:Biphenyl-3-carboxylic acid (1:2) on the siRNA structure. The combination of Cho:Geranic Acid (1:2) (25 vol%) and Cho:Phenylpropanoic Acid (1:2) (25 vol%) led to a prominent band indicative of retention of siRNA structure and generated the highest epidermal accumulation of siRNA, notably higher than any other individual ILs and/or combination. This formulation was then used in an imiquimod-induced psoriasis-like skin inflammation model that resembles plaque-type psoriasis in humans. Topical application of IL-siRNA for 4 consecutive days generated a substantial reduction in the levels of inflammatory cytokines and an array of psoriasis-related gene products (Mandal et al. 2020). Future work should focus on IL moiety optimization for improved cell internalization and biocompatibility, as well as applying this platform for the treatment of other skin diseases such as psoriasis, atopic dermatitis, and melasma (Zakrewsky and Mitragotri 2016).
Incorporating the Cho:Geranic Acid (1:2) Formulation to Solid Supports
These systems can also be used to dissolve drugs, and the mixture was incorporated into transdermal patches or devices as delivery systems. For example, Cho:Geranic Acid (with 1:1 or 1:2 molar ratio) were compared with Cho:Oleic Acid (with 1:1 or 1:2 molar ratio) to dissolve insulin, and the mixtures were incorporated into biofilms composed of xanthan gum and bacterial nanocellulose (Jorge et al. 2020). The films containing Cho:Geranic Acid (1:1) or (1:2) exhibited positive antimicrobial activity against Escherichia coli and Staphylococcus aureus but did not affect Pseudomonas aeruginosa. On the contrary, none of the Cho:Oleic Acid systems showed an effect upon E. coli and only a mild antimicrobial activity against S. aureus. On P. aeruginosa, only Cho:Oleic Acid (1:1) showed a positive mild antimicrobial activity. The Cho:Geranic Acid (1:2) that performed best in terms of lack of cytotoxicity, genotoxicity, and permeation enhancement was used to dissolve insulin and integrated into the biofilm, allowing an average permeated protein per skin area of 1.05 µg protein mm−2 skin.
In a recent publication, Silva and coworkers isolated lytic bacteriophages for Staphylococcus intermedius as a new antimicrobial treatment for pyoderma via cutaneous permeation of bacteriophage particles and used Cho:Geranic Acid (1:1) and (1:2) as permeation enhancers (Silva et al. 2021). The isolated phage particles, identified as Caudovirales, most likely belonging to the family Myoviridae, had particle sizes in the order of the nanometers (<100 nm). The phage particles were mixed with Cho:Geranic Acid (1:1) or (1:2), and the mixtures were integrated into hydroxyethyl cellulose (HEC) gel. When tested for transdermal delivery, the presence of Cho:Geranic Acid (1:2) led to increased average of permeated phage particles, as opposed to the permeation assays with Cho:Geranic Acid (1:1) or the absence of either Cho:Geranic Acid (1:1) or (1:2) in the HEC matrix. Combining phage particles and Cho:Geranic Acid (1:2) allowed the transdermal permeation of phage particles and will potentially allow the treatment of pyodermal infection. The same research group has developed a sodium alginate-based hydrogel integrating choline oleate as a carrier for a cocktail of lytic phage particles aiming at the treatment of deep skin infections in humans caused by Acinetobacter baumannii (Campos et al. 2020). Combining phage particles with choline-based ILs as carriers may be an excellent alternative to antibiotics to combat dermal infections.
Commercial Deployment
Scaling up the synthesis of CAGE and its medical applications are one of the greatest challenges for the translation of this compound into practice. The first report scaling up the synthesis of Cho:Geranic Acid (1:2), kg scale, was recently published in Ko et al. 2020a, where 40 wt% Cho:Geranic Acid (1:2) was incorporated as a gel using hydroxypropyl cellulose as a gelling agent; gel vehicle consisted of ~90% water along with some propylene glycol (cosolvent), a fragrance, and a gelling agent. This formulation, referred to as CGB400, was used for in vitro and in vivo tests. The resulting gel showed promising results, usingthe antimicrobial properties of Cho:Geranic Acid (1:2) for rosacea treatment. After proving for low toxicity and high antimicrobial effects, a 12-week open-label cosmetic study for rosacea was performed on humans. A marked improvement in symptoms was observed, with ~70% of the subjects reporting a greater reduction in lesions after treatment. Although this study did not include a drug and only explored the properties of Cho:Geranic Acid (1:2) previously shown in vitro and in mice as a broad-spectrum antimicrobial agent (Zakrewsky et al. 2016), it sets a precedent for the scaling up and low toxicity of the CAGE, now tested in humans.
Conclusions
Currently, CAGE Bio, Inc., a clinical-stage startup based in San Carlos, Calif. exploits CAGE and similar systems, to develop novel pharmaceutical products for dermatology, inflammation, immunology, etc. The startup has recently secured $7.2M in funding (CAGE Bio Inc 2021).
This is however not the first example of ILs and/or DESs with transdermal properties proposed for commercialization. The Lidocaine–Etodolac Patch (DES, containing the NSAID etodolac and the pain-reliever lidocaine) has shown to be effective in the treatment of postherpetic neuropathic (PHN) pain in placebo- and active-controlled comparisons and has been incorporated into a topical transdermal delivery system, Etodolac–Lidocaine Topical Patch (RX-7EAT or “Etoreat”) (ClinicalTrials.gov 2018 ; Miwa et al. 2016). The etodolac products developed by a research and development Japanese company, MedRx, exhibited increased transdermal absorbability and improved efficacy of this IL. The new venture, IL Pharma Inc. (MEDRx, Kagawa, Japan), owned 51% by Kaneka and 49% by MedRx, took over programs that MedRx was developing on its own. This patch was the first API-IL that has reached clinical trials for the treatment of ankle sprains, low back pain, and muscle soreness. MedRx Co. Ltd. has received approval to conduct human trials in the US and completed Phase I trials for acute pain in the USA (NCT02695381). Even though in vitro studies showed that this system significantly increased the skin permeation of etodolac (9.3-fold) compared to “free” etodolac (Miwa et al. 2016), due to the lack of statistically significant differences between Etoreat and placebo in humans, its development has been suspended.
Another system includes GSK2838232, the HIV-1 maturation inhibitor (MI) that is being developed for the treatment of HIV-1 infection in combination with other antiretroviral therapy, derived from the triterpene betulin natural product (Shamshina and Rogers 2020). It is currently in Phase IIa clinical studies, to evaluate its safety, pharmacokinetics, and antiviral activity in participants with HIV-1 virus (DeJesus et al. 2020).
Indeed, drug development is a long and expensive process, taking on average, 10–15 years, with ~14% of all drugs in clinical trials eventually getting approval from the FDA (Hale 2018). Based on this situation, IL (or DES)-based technology of producing transdermally active drugs, by selectively combining ionizable compounds from GRAS-list into a single IL (or DES) form, could take a shorter time to market. Owing to their easy tunability, ILs and DESs constitute a vast number of formulation candidates. The number of combinations is almost endless, by modifying functional groups, carbon-chain lengths, and ion ratios. However, ILs and DESs would require further characterization, and way more additional testing that is available now, and here, federal funding could play an important role by widening opportunities and providing more incentives to those investors who are willing to take risks.
References
Banerjee A, Ibsen K, Iwao Y, Zakrewsky M, Mitragotri S (2017) Transdermal protein delivery using choline and geranate (CAGE) deep eutectic solvent. Adv Healthcare Mater 6:1601411
Banerjee A, Ibsen K, Brown T, Chen R, Agatemor C, Mitragotri S (2018a) Reply to Rogers and Gurau: definitions of ionic liquids and deep eutectic solvents. Proc Natl Acad Sci USA 115:E11000–E11001
Banerjee A, Ibsen K, Brown T, Chen R, Agatemor C, Mitragotri S (2018b) Ionic liquids for oral insulin delivery. Proc Natl Acad Sci USA 115:7296–7301
Berton P, Kelley SP, Wang H, Rogers RD (2018) Elucidating the triethylammonium acetate system: Is it molecular or is it ionic? J Mol Liq 269:126–131
Bica K, Rogers RD (2010) Confused ionic liquid ions − A “liquification” and dosage strategy for pharmaceutically active salts. Chem Commun 46:1215–1217
Bica K, Shamshina JL, Hough WL, MacFarlane DR, Rogers RD (2011) Liquid forms of pharmaceutical co-crystals: exploring the boundaries of salt formation. Chem Commun 47:2267–2269
Bielfeldt S, Schoder V, Ely U, Van Der Pol A, De Sterke J, Wilhelm K-P (2009) Assessment of human stratum corneum thickness and its barrier properties by in-vivo confocal Raman spectroscopy. Int J Cosmet Sci 31:479–480
Brisson P (1974) Percutaneous absorption. Can Med Assoc J 110:1182–1185
CAGE Bio Inc (2021) CAGE Bio closes $7.2 Million round of series A funding. https://www.prnewswire.com/news-releases/cage-bio-closes-7-2-million-round-of-series-a-funding-301229156.html. Last accessed 04–19–21
Campos WF, Silva EC, Oliveira TJ, Oliveira JM, Tubino M, Pereira C, Vila MMDC, Balcão VM (2020) Transdermal permeation of bacteriophage particles by choline oleate: potential for treatment of soft-tissue infections. Future Microbiol 15:881–896. https://doi.org/10.2217/fmb-2019-0290
Chen Y, Quan P, Liu X, Wang M, Fang L (2014) Novel chemical permeation enhancers for transdermal drug delivery. Asian J Pharm Sci 9:51–64
Choline chloride (April 1, 2020). FDA U.S. Food & Drug. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=582.5252. Last accessed 04–19–21
ClinicalTrials.gov (2018) Identifier: NCT01198834, MRX-7EAT Etodolac-Lidocaine Topical Patch in the Treatment of Ankle Sprains. https://clinicaltrials.gov/ct2/show/NCT01198834. Last accessed 04–19–21.
Cohen SM, Eisenbrand G, Fukushima S, Gooderham NJ, Guengerich FP, Hecht SS, Rietjens IMCM, Harman C, Taylor SV (April 1, 2020) GRAS 28 Flavoring Substances. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=582.5252. Last accessed 04–19–21
DeJesus E, Harward S, Jewell RC, Johnson M, Dumont E, Wilches V, Halliday F, Talarico CL, Jeffrey J, Gan J, Xu J, Felizarta F, Scribner A, Ramgopal M, Benson P, Johns BA (2020) A phase IIa study evaluating safety, pharmacokinetics, and antiviral activity of GSK2838232, a novel, second-generation maturation inhibitor, in participants with human immunodeficiency virus type 1 infection. Clin Infect Dis 71:1255–1262
Fei Z, Geldbach TJ, Zhao D, Dyson PJ (2006) From dysfunction to bis-function: on the design and applications of functionalised ionic liquids. Chem Eur J 12:2122–2128
Freemantle M (1998) Designer Solvents. Ionic liquids may boost clean technology development. Chem Eng News 76:32–37
Hale C (2018) New MIT study puts clinical research success rate at 14 percent. https://www.centerwatch.com/articles/12702-new-mit-study-puts-clinical-research-success-rate-at-14-percent#:~:text=Nearly%2014%20percent%20of%20all,MIT%20Sloan%20School%20of%20Management. Last accessed 04–19–21
Harada LK, Pereira JFB, Campos WF, Silva EC, Moutinho CG, Vila MMDC, Oliveira JM Jr, Teixeira JA, Balcão VM, Tubino M (2018) Insights into protein-ionic liquid interactions aiming at macromolecule delivery systems. J Braz Chem Soc 29:1983–1998
Hattori T, Tagawa H, Inai M, Kan T, Kimura S-I, Itai S, Mitragotri S, Iwao Y (2019) Transdermal delivery of nobiletin using ionic liquids. Sci Rep 9:20191. https://doi.org/10.1038/s41598-019-56731-1
Hough WL, Smiglak M, Rodríguez H, Swatloski RP, Spear SK, Daly DT, Pernak J, Grisel JE, Carliss RD, Soutullo MD, Davis JD Jr, Rogers RD (2007) The third evolution of ionic liquids: Active pharmaceutical ingredients. New J Chem 31:1429–1436
Jaitely V, Karatas A, Florence AT (2008) Water immiscible room temperature ionic liquids: some properties relevant to their pharmaceutical use. Int J Pharm 354:168–173
Jorge LR, Harada LK, Silva EC, Campos WF, Moreli FC, Shimamoto G, Pereira JFB, Oliveira Jr. JM, Tubino M, Vila MMDC, Balcão VM (2020) Non-invasive transdermal delivery of human insulin using ionic liquids: In vitro studies. Front Pharmacol 11, Article 243. https://doi.org/10.3389/fphar.2020.00243
Kalluri H, Banga AK (2011) Transdermal delivery of proteins. AAPS PharmSciTech 12:431–441
Karande P, Mitragotri S (2009) Enhancement of transdermal drug delivery via synergistic action of chemicals. BBA-Biomem 1788:2362–2373
Karande P, Jain A, Mitragotri S (2004) Discovery of transdermal penetration enhancers by high-throughput screening. Nat Biotech 22:192–197
Karande P, Jain A, Ergun K, Kispersky V, Mitragotri S (2005) Design principles of chemical penetration enhancers for transdermal drug delivery. Proc Natl Acad Sci USA 102:4688–4693
Kelley SP, Narita A, Holbrey JD, Green KD, Reichert WM, Rogers RD (2013) Understanding the effects of ionicity in salts, solvates, co-crystals, ionic co-crystals, and ionic liquids, rather than nomenclature, is critical to understanding their behavior. Cryst Growth Des 13:965–975
Kim M-J, Doh H-J, Choi M-K, Chung S-J, Shim C-K, Kim D-D, Kim JS, Yong C-S, Choi H-G (2008) Skin permeation enhancement of diclofenac by fatty acids. Drug Delivery 15:373–379
Ko J, Mandal A, Dhawan S, Shevachman M, Mitragotri S, Joshi N (2020) Clinical translation of choline and geranic acid deep eutectic solvent. Bioeng Transl Med e10191. https://doi.org/10.1002/btm2.10191
Ko J, Mandal A, Dhawan S, Shevachman M, Mitragotri S, Joshi N (2020) Clinical translation of choline and geranic acid deep eutectic solvent. Bioeng Transl Med e10191. Prepublication Peer Review and Author Responses. https://publons.com/publon/https://doi.org/10.1002/btm2.10191. Last accessed 04–19–21
Mandal A, Kumbhojkar N, Reilly C, Dharamdasani V, Ukidve A, Ingber DE, Mitragotri S (2020) Treatment of psoriasis with NFKBIZ siRNA using topical ionic liquid formulations. Sci Adv 6:eabb6049
Mann SK, Devgan MK, Franks WT, Huband S, Chan CL, Griffith J, Pugh D, Brooks NJ, Welton T, Pham TN, McQueen LL, Lewandowski JR, Brown SP (2020) MAS NMR Investigation of molecular order in ionic liquid crystal. J Phys Chem B 4975–4988
Mehta R (2004) Topical and transdermal drug delivery: what a pharmacist needs to know. InetCE. 1st, Arizona, 1–10
Miwa Y, Hamamoto H, Ishida T (2016) Lidocaine self-sacrificially improves the skin permeation of the acidic and poorly water-soluble drug etodolac via its transformation into an ionic liquid. Eur J Pharm Biopharm 102:92–100
Mizuuchi H, Jaitely V, Murdan S, Florence AT (2008) Room temperature ionic liquids and their mixtures: potential pharmaceutical solvents. Eur J Pharm Sci 33:326–331
Park HJ, Prauznitz MR (2010) Lidocaine-ibuprofen ionic liquid for dermal anesthesia. AIChE J 61:2732–2738
Prausnitz M, Langer R (2008) Transdermal drug delivery. Nat Biotechnol 26:1261–1268
Prausnitz MR, Elias PM, Franz TJ, Schmuth M, Tsai J-C, Menon GK, Holleran WM, Feingold KR (2017) Skin barrier and transdermal drug delivery. Chapter 124. In Bolognia J, Schaffer J, Cerroni L (eds) Dermatology: 2-volume set, 4th edn. Elsevier
Qi QM, Mitragotri S (2019) Mechanistic study of transdermal delivery of macromolecules assisted by ionic liquids. J Controlled Release 311–312:162–169
Qi QM, Duffy M, Curreri AM, Balkaran JPR, Tanner EEL, Mitragotri S (2020) Comparison of ionic liquids and chemical permeation enhancers for transdermal drug delivery. Adv Funct Mater 30:2004257
Ramadon D, McCrudden MTC, Courtenay AJ, Donnelly RF (2021) Enhancement strategies for transdermal drug delivery systems: current trends and applications. Drug Delivery Transl Res 1–34. https://doi.org/10.1007/s13346-021-00909-6
Rebelo LPN, Lopes JNC, Esperança JMSS, Guedes HJR, Lachwa J, Najdanovic-Visak V, Visak ZP (2007) Accounting for the unique, doubly dual nature of ionic liquids from a molecular thermodynamic and modeling standpoint. Acc Chem Res 40:1114–1121
Reslan M, Kayser V (2018) Ionic liquids as biocompatible stabilizers of proteins. Biophys Rev 10:781–793
Rogers RD, Gurau G (2018) Is “choline and geranate” an ionic liquid or deep eutectic solvent system? Proc Natl Acad Sci USA 115:E10999
Shamshina JL, Rogers RD (2020) Are myths and preconceptions preventing us from applying ionic liquid forms of antiviral medicines to the current health crisis? Int J Mol Sci 21:6002–6018
Shamshina JL, Berton P, Wang H, Zhou X, Gurau G, Rogers RD (2018) Ionic liquids in the pharmaceutical industry. In Zhang W, Cue B (eds) Green techniques for organic synthesis and medicinal chemistry, 2nd edn, Wiley, pp 541–577
Sidat Z, Marimuthu T, Kumar P, du Toit LC, Kondiah P, Choonara YE, Pillay V (2019) Ionic liquids as potential and synergistic permeation enhancers for transdermal drug delivery. Pharmaceutics 11:1–21
Silva EC, Oliveira TJ, Moreli FC, Harada LK, Vila MMDC, Balcão VM (2021) Newly isolated lytic bacteriophages for Staphylococcus intermedius, structurally and functionally stabilized in a hydroxyethylcellulose gel containing choline geranate: potential for transdermal permeation in veterinary phage therapy. Res Vet Sci 135:42–58
Stoimenovski J, MacFarlane DR (2011) Enhanced membrane transport of pharmaceutically active protic ionic liquids. Chem Commun 47:11429–11431
Takeda J, Iwao Y, Karashima M, Yamamoto K, Ikeda Y (2021) Structural evaluation of the choline and geranic acid/water complex by SAXS and NMR analyses. ACS Biomater Sci Eng 7:595–604
Tanner EEL, Ibsen KN, Mitragotri S (2018) Transdermal insulin delivery using choline-based ionic liquids (CAGE). J Control Release 286:137–144
Tanner E, Curreri A, Balkaran J, Selig-Wober N, Yang A, Kendig C, Fluhr M, Kim N, Mitragotri S (2019) Design principles of ionic liquids for transdermal drug delivery. Adv Mater 31:1901103
The ionic liquid platform (2020) https://cagebio.com/our-technology. Last accessed 04–19–21
Wang H, Gurau G, Shamshina J, Cojocaru OA, Janikowski J, MacFarlane DR, Davis JH Jr, Rogers RD (2014) Simultaneous membrane transport of two active pharmaceutical ingredients by charge assisted hydrogen bond complex formation. Chem Sci 5:3449–3456
Warner RR, Myers MC, Taylor DA (1988) Electron probe analysis of human skin: determination of the water concentration profile. J Invest Dermatol 90:218–224
Welton T (1999) Room-temperature ionic liquids. Solvents for synthesis and catalysis. Chem Rev 99:2071–2084
Yang R, Wei T, Goldberg H, Wang W, Cullion K, Kohane D (2017) Getting drugs across biological barriers. Adv Mater 29:1606596
Zakrewsky M, Mitragotri S (2016) Therapeutic RNAi robed with ionic liquid moieties as a simple, scalable prodrug platform for treating skin disease. J Controlled Release 242:80–88
Zakrewsky M, Lovejoy KS, Kern TL, Miller TE, Le V, Nagy A, Goumas AM, Iyer RS, Del Sesto RE, Koppisch AT, Fox DT, Mitragotri S (2014a) Biological applications of ionic liquids. Proc Natl Acad Sci USA 111:13313–13318
Zakrewsky M, Lovejoy KS, Kern TL, Miller TE, Le V, Nagy A, Goumas AM, Iyer RS, Del Sesto RE, Koppisch AT, Fox DT, Mitragotri S (2014b) Ionic liquids as a class of materials for transdermal delivery and pathogen neutralization. Proc Natl Acad Sci USA 111:13313–13318
Zakrewsky M, Banerjee A, Apte S, Kern TL, Jones MR, Del Sesto RE, Koppisch AT, Fox DT, Mitragotri S (2016) Choline and geranate deep eutectic solvent as a broad-spectrum antiseptic agent for preventive and therapeutic applications. Adv Healthcare Mater 5:1282–1289
Zakrewsky M, Mitragotri S, Fox DT, Koppisch A, Del Sesto RE, Lovejoy K (2019) Ionic liquids for transdermal drug delivery. US 10,449,254 B2, 22 October 2019
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Berton, P., Shamshina, J.L. (2021). Ionic Liquids for Transdermal Drug Delivery: Choline Geranate System as a Case Study. In: Goto, M., Moniruzzaman, M. (eds) Application of Ionic Liquids in Drug Delivery. Springer, Singapore. https://doi.org/10.1007/978-981-16-4365-1_3
Download citation
DOI: https://doi.org/10.1007/978-981-16-4365-1_3
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-4364-4
Online ISBN: 978-981-16-4365-1
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)