Abstract
Immunohistochemistry (IHC) is an indispensable tool in the diagnosis of sarcomas. Sarcomas are a vast, diverse and complex group of neoplasms arising from mesenchymal origin. They present a diagnostic challenge as they are rare and have many overlapping appearances under the microscope. Accurate diagnosis of sarcomas is necessary for deciding management and prognostication of the disease. Historically, the categorisation of sarcomas has been based on their presumed line of differentiation [1, 2]. In some cases, the histomorphology is straightforward and distinct; however, in other cases, the histogenesis can be ambiguous, and further investigation is required to assist with the diagnosis [3]. To compound this, benign mesenchymal lesions and non-sarcomatous tumours are frequently encountered as differential diagnoses to sarcomas and thus present an additional diagnostic challenge [4]. The use of ancillary pathological techniques, therefore, is essential in the evaluation of mesenchymal tumour samples. IHC is a microscopy-based method that utilises immunological and biochemical principles to detect protein expression in tumour cells. Since its discovery in 1942, IHC has progressively improved through development of new antibodies. Nowadays, it has established itself as a valuable adjunctive step in the pathological diagnosis of surgical specimens of bone and soft tissue tumours.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
8.1 Introduction
Immunohistochemistry (IHC) is an indispensable tool in the diagnosis of sarcomas. Sarcomas are a vast, diverse and complex group of neoplasms arising from mesenchymal origin. They present a diagnostic challenge as they are rare and have many overlapping appearances under the microscope. Accurate diagnosis of sarcomas is necessary for deciding management and prognostication of the disease. Historically, the categorisation of sarcomas has been based on their presumed line of differentiation [1, 2]. In some cases, the histomorphology is straightforward and distinct; however, in other cases, the histogenesis can be ambiguous, and further investigation is required to assist with the diagnosis [3]. To compound this, benign mesenchymal lesions and non-sarcomatous tumours are frequently encountered as differential diagnoses to sarcomas and thus present an additional diagnostic challenge [4]. The use of ancillary pathological techniques, therefore, is essential in the evaluation of mesenchymal tumour samples. IHC is a microscopy-based method that utilises immunological and biochemical principles to detect protein expression in tumour cells. Since its discovery in 1942, IHC has progressively improved through development of new antibodies. Nowadays, it has established itself as a valuable adjunctive step in the pathological diagnosis of surgical specimens of bone and soft tissue tumours.
8.2 History of IHC: “Putting Tail Lights on Antibodies”
While IHC was discovered by Dr. Albert Coons in 1942, the story of its development is vast and involves the contribution of many scientists. Its inception can be traced back to the late 1800s, when Dr. Emil von Behring first described antibodies in the context of passive immunisation against diphtheria and tetanus and successfully treated his first patient [5]. It was through this work that earned him the first Nobel Prize in physiology and medicine in 1901 [6]. Following this, many other scientists contributed to research into antigen-antibody interactions, including Professor Paul Ehrlich, who further characterised the antigen-antibody interaction [7]; Dr. Kraus, who developed the precipitin test, a technique for detecting antigen-antibody complexes in solution [8]; and Dr. John Marrack, who attached dye to antibodies in order to visualise these complexes [9].
One important catalyst in the development of IHC occurred in the early 1920s, when Michael Heidelberger and Oswald Avery produced coloured antigen-antibody complexes to demonstrate that antigens were polysaccharides [10]. Then, by attaching a purple azo dye to antigens, Heidelberger and another associate, Forrest Kendall, were able to produce coloured antigen-antibody complex precipitates [11].
In 1942, Dr. Albert Coons developed fluorescein-labelled antibodies that could be detected by light microscopy and, thus, discovered the technique of IHC [12]. Immunofluorescence, however, was unable to be detected by electron microscopy, so subsequent developments aimed to address this limitation. In 1959, Dr. S. J. Singer detected antigens by electron microscopy by using ferritin-antibody [13]. Later, Graham and Karnovsky pioneered a new immunoenzyme labelling method by tagging antibodies with enzymes [14]. Through this work, Elizabeth Leduc, Stratis Avrameas and, separately, Paul Nakane, developed new immunoperoxidase techniques, which allowed detection of antigens and both light and electron microscopy levels [15, 16]. This technique was further modified by Ludwig Sternberger with the peroxidase-antiperoxidase (PAP) technique, thus improving sensitivity and efficacy [17]. In 1971, W. Page Faulk and G. Malcolm Taylor used colloidal gold as a label to detect antigens by electron microscopy [18]. Jurgen Roth, Moise Bendayan and Lelio Orci contributed further improvements to this protocol over the next decade through introduction of protein A-coated colloidal gold and thus developed the technique that is widely used today [19].
8.3 Procedure, Technical Considerations and Possible Limitations
The general concept of IHC involves using antibodies attached with a chromogenic enzyme to highlight and visualise a specific antigen of interest. The process of IHC is heavily protocolised to ensure strict standardisation and reproducibility of results [20]. The process of IHC is lengthy and complex, with each step contributing to its overall accuracy. The quality assurance of IHC is comprised on many critical components, including tissue handling, fixation, processing, sectioning, testing and interpretation of results [21].
The IHC protocol can be broadly simplified to three main players: (1) the tissue sample in question, (2) the antibodies to be used for testing and (3) the method of detection and analysis. The careful consideration of each of these main components determines the reliability of the IHC test. Each factor, their technical considerations and possible limitations will be discussed in further detail below.
8.3.1 Preparing the Tissue Sample
The first critical task is ensuring that enough viable tumour tissue is obtained in order to perform all necessary histology and ancillary tests. It is essential that the surgeon captures sufficient cells representative of the tumour to make an accurate diagnosis. This can be challenging when performing a biopsy. It has been shown that open biopsy has the greatest diagnostic accuracy when compared with fine needle aspiration and core biopsy [22]. Open biopsy, however, is more invasive, has higher risk of contamination and carries higher costs, so core biopsy is most often preferred as the next most accurate technique [23].
The pre-analytical phase of IHC is critical for accurate analysis. This includes tissue handling, fixation, paraffinisation, sectioning, storage and antigen retrieval, and each of these steps influences the quality of the result later. Firstly, the time from resection to fixation of a tissue sample can affect the detection of proteins by IHC due to the length of ischaemic time that the tissue undergoes [24]. During this period of time, the tissue undergoes ‘cold ischaemia’, in which proteins, RNA and DNA are degraded as a result of anoxic damage [25]. Studies of various cancer types have shown differences in IHC results when there is a delay in fixation [26,27,28]. Fixation itself is another area of potential variability or error. Factors including the duration, formula of the formalin solution and the tissue to fixative ratio all influence the quality of IHC [24, 29]. The tissue, once fixed, then undergoes further processing that includes washing and removal of excess fixative, dehydration and clearing and paraffin impregnation. These paraffin blocks are sectioned into thin slices and stored. Thickness of the sections may also influence IHC results and increase intensity of immunostaining. Tears sustained during the cutting process may cause artefact or loss of protein staining [25]. Storage of these sections also has impact on IHC, with studies demonstrating a loss of p53 staining with prolonged storage of sections [30, 31].
8.3.2 Selecting Useful Antibodies
In order to perform IHC, pathologists firstly need to select a panel of suitable antibodies that will help guide the diagnosis. The selection, application and interpretation of useful antibodies are discussed in further detail in this chapter. There are also some antibodies that have been shown to be non-specific and, as a result, do not provide diagnostic relevance. Vimentin, for example, is a marker that is widely expressed in almost all tumour types, mesenchymal and non-mesenchymal and therefore not recommended for use [3, 32, 33]. Similarly, histiocytic markers alpha-1-antitrypsin and alpha-1-antichymotrypsin demonstrate widespread expression and have been replaced by the more specific CD68 [4, 33]. Myoglobin was previously used for detection of rhabdomyosarcoma, however is only expressed in approximately 60% of cases [34, 35]. Nowadays, myogenin is used in its place as a marker in rhabdomyosarcoma.
At the manufacturer level, it is necessary to enforce strict protocols for quality control in order to ensure standardisation of all reagents. There are also various technical considerations regarding storage of antibody reagents. Improper storage, for example, can be responsible for greater than 50% of IHC failures [36].
8.3.3 Detecting and Analysing the Reaction
Once the antigen-antibody reaction has taken place, there needs to be an adequate system to visualise and analyse the IHC results in a reproducible and reliable fashion. This part of the process can be broadly broken up into two broad steps: (1) detection of immunoreactivity and (2) clinical interpretation of results.
Detection systems are necessary to visualise whether an antigen-antibody reaction has taken place, since antibodies alone cannot be seen under light or electron microscopy. In order to do this, labels are attached to the antibodies. Common detection systems include direct-conjugate-labelled antibody method, indirect procedure, avidin-biotin complex method, streptavidin-biotin systems, phosphatase anti-phosphatase label system, polymer-based detection and tyramine amplification system [37]. These are all various techniques used to attach a chromogenic label to the antibodies. Polymeric- and tyramine-based amplification methods are beneficial in that they greatly improve sensitivity; however, they are also associated with more complex protocols that result in worse standardisation and reproducibility [21]. In order to better highlight the immunoreaction, counter staining can also be performed to provide further contrast to the antibody labels. Haematoxylin is the most common counterstain used for IHC, although eosin, methylene blue, methylene green and toluidine blue can also be used [21, 37].
In order to accurately interpret the results, pathologists also need to understand the relative sensitivities and specificities of the reagents. It must be emphasised that, while IHC is a powerful diagnostic tool, there is no single antibody or antibody combination that is completely unique to tumour type [38]. The interpretation of these markers in the context of bone and soft tissue tumours will be discussed in detail in this chapter.
8.4 Immunohistochemical Markers
8.4.1 Broad-Spectrum Markers
In sarcoma diagnosis, a panel of antibodies is routinely used in the initial instance to analyse a tissue sample. These markers can either confirm a diagnosis or characterise cell phenotypes to further guide immunohistochemical or molecular testing. Frequently used cell-typic markers include cytokeratins, epithelial membrane antigen (EMA), S100 protein, desmin, smooth muscle actin (SMA) and CD34. These antibodies are largely non-specific, which means that they are expressed in multiple sarcoma subtypes. The interpretation of these markers, therefore, is most useful in combination with the wider clinical, radiological and histopathological picture.
8.4.1.1 Cytokeratins
Keratins are a family of proteins expressed in normal epithelial tissue. As such, the detection of keratins, in particular low-molecular-weight keratins, may indicate epithelial differentiation of soft tissue tumours [33]. There are 20 described keratin protein types, of which 8 have basic or higher isoelectric points (Type I; KRT 1–8) and the remainder has acidic or lower isoelectric points (Type II; KRT 9–20) [39]. AE1/AE3 are broad-spectrum immunohistochemical antibodies that are most commonly used to detect keratins in surgical pathology. AE1 contains antibodies to Type I keratins (KRT 10, 14–16 and 19), while AE3 recognises Type II keratins (1–8) [40]. This antibody cocktail is used as a first-line immunohistochemical investigation for spindle cell, pleomorphic, round cell and epithelioid tumours. They are also extremely useful in the differentiation between sarcoma and its carcinoma mimics [41].
8.4.1.2 Epithelial Membrane Antigen
EMA is a transmembrane glycoprotein that is widely expressed in normal epithelial tissue and their neoplastic counterparts. In addition to carcinomas, some soft tissue tumours demonstrate recurrent EMA expression. These tumours typically include epithelioid sarcoma [42], synovial sarcoma [43,44,45,46] and myoepithelioma [47, 48] but are widely absent in many other soft tissue tumours [49].
8.4.1.3 S100 Protein
The S100 protein describes a multigene family of 21 proteins that demonstrate close structural similarity but widely varying function that includes participation in proliferation, migration, inflammation and differentiation [50,51,52]. It is commonly positive in a range of soft tissue tumours, including melanomas, benign peripheral nerve sheath tumours (PNST), clear cell sarcoma and myoepitheliomas.
8.4.1.4 Desmin
Desmin, a muscular marker, is an intermediate filament that is normally expressed in skeletal muscle and smooth muscle cells [53, 54]. In surgical pathology, its main utility resides in the identification of rhabdomyosarcomas and leiomyosarcomas, as well as their benign counterparts [53, 55]. Desmin is, however, positive in a number of other sarcomas, including desmoplastic small round tumours [56, 57], myofibroblastic tumours [53, 54, 58] and tenosynovial giant cell tumours [59]. Its interpretation is best made alongside other myogenic markers, including SMA and more specific markers myogenin and MyoD1, in the differentiation and diagnosis of muscular tumours.
8.4.1.5 Smooth Muscle Actin
SMA is another muscular marker that is expressed in normal smooth muscle cells. It is a useful marker in diagnosis of smooth muscle tumours and myofibroblastic tumours. It is also expressed in normal myofibroblasts, myoepithelial cells and smooth muscle-related pericytes and glomus cells and, therefore, positive in the tumours of the respective lineages [60].
8.4.1.6 CD34
CD34 is a transmembrane glycoprotein that is widely expressed in many soft tissue tumours, particularly spindle cell and epithelioid cell tumours [4]. Its expression is encountered consistently in malignant vascular tumours [61, 62], solitary fibrous tumour (SFT), dermatofibrosarcoma protuberans and spindle cell lipomas. Variable expression is seen in GISTs, epithelioid sarcoma and MPNST.
8.4.1.7 CD99
CD99, also known as MIC2, is a transmembrane glycoprotein normally expressed on the cell surface of T lymphocytes [63]. In surgical pathology, it is a non-specific marker that is useful in the classification of round cell tumours. It is particularly useful in the identification of Ewing’s sarcoma/PNET, in which it demonstrates strong membranous staining [64,65,66].
8.4.2 Novel Markers
The advent of molecular techniques has allowed the genetic characterisation of soft tissue tumours and discovery of recurrent mutations including reciprocal translocations, amplifications and point mutations. An understanding of these genetic aberrations and their respective protein products have allowed pathologists to develop targeted immunohistochemical surrogates for the identification of genetic mutations in tumours samples that can aid in its diagnosis.
8.4.2.1 FLI-1
In translocations, these surrogate markers do not detect the fusion itself but rather identifies the resultant overexpression of specific proteins [67].
Ewing’s sarcoma/primitive neuroectodermal tumours (PNET) are a class of small, blue, round cell tumours that share a similar histomorphology with tumours such as neuroblastoma, rhabdomyosarcoma and poorly differentiated synovial sarcomas [68]. A specific t(11;22) translocation is found in approximately 90% of all Ewing’s sarcoma/PNET, resulting in an EWSR1-FLI-1 fusion product [69,70,71]. The sc-356 immunohistochemical stain is a polyclonal antibody to the carboxy-terminal of FLI that has demonstrated 71% sensitivity and 92% specificity for Ewing’s sarcoma/PNET in previous studies [68, 72].
8.4.2.2 MDM2 and CDK4
Atypical lipomatous tumours/well-differentiated liposarcomas (ALT/WDLPS) and dedifferentiated liposarcomas (DDLPS) are two separate types of fatty tumours that are both characterised by complex genomes, resulting in supernumerary ring and giant marker chromosomes and the amplification of 12q13–15 gene locus [73, 74]. MDM2 and CDK4 are two genes within this locus, and their amplified protein products can be detected by IHC [75, 76].
8.5 Application and Interpretation of IHC
IHC has a well-established role in the diagnosis of bone and soft tissue tumours. The frequent overlapping histological features of sarcomas require the use of ancillary techniques, such as IHC, to help further distinguish tissue characteristics. As described in Fig. 8.1, IHC plays three key roles in the differential diagnosis of bone and soft tissue tumours: (a) in establishing any rare or atypical benign mesenchymal lesions that may resemble malignant tumours; (b) the identification of malignant lesions of non-mesenchymal origin; and (c) the characterisation of specific sarcoma subtypes, in particularly distinguishing one sarcoma type from histologic mimics. Ultimately, accurate diagnosis of mesenchymal neoplasms is essential in providing prognostic information for patients and guiding appropriate therapeutic care.
8.5.1 Identification of Benign Tumours
While IHC alone cannot definitively differentiate all benign and malignant tumours [38], it can be extremely useful in identifying atypical benign lesions that share similar histological appearances with a malignancy. Clarification of whether a tumour is benign or malignant may influence the course of treatment, for example, the type of excision (marginal vs wide local excision) or the addition of neoadjuvant therapy. Tumours that may mimic malignancies include SFT and benign PNST.
8.5.1.1 Solitary Fibrous Tumour
SFT is a benign soft tissue tumour of spindle cell morphology. Its histologic features can be difficult to distinguish from various other soft tissue tumours, including mesothelioma or other spindle cell tumours [4, 77]. IHC reveals CD34 and Bcl-2 positivity in most cases, and these markers are therefore highly sensitive for SFT [78, 79]. Negative staining for both markers would strongly suggest an alternative diagnosis [80]. IHC for STAT6 can be used as a surrogate marker of the NAB2-STAT6 fusion product highly characteristic for SFT [81]. STAT6 is therefore a highly specific marker for SFT and is useful in distinguishing from histologic mimics [82, 83]. Other valuable markers in the diagnosis of SFT include CD99 and beta-catenin [78, 84].
8.5.1.2 Nodular Fasciitis
Nodular fasciitis (NF) typically presents as a rapidly growing, poorly circumscribed mass that reveals dense cellularity and high mitotic activity on pathological examination. It is not uncommon for NF to be misdiagnosed as sarcoma, such as dermatofibrosarcoma protuberans, low-grade myofibroblastic sarcoma or malignant peripheral nerve sheath tumour (MPNST), thus warranting IHC for definitive diagnosis [85,86,87]. IHC demonstrates positive staining for SMA in almost all cases with consistent negativity for desmin, h-caldesmon, S100 and beta-catenin [88, 89].
8.5.2 Exclusion of Non-mesenchymal/Non-sarcomatous Tumours
Once a benign lesion has been ruled out and the tumour has been classified as malignant, the pathologist must exclude the diagnosis of a non-mesenchymal tumour. There are various non-sarcomatous lesions that may resemble sarcomas due to their overlapping histological features. Common examples include sarcomatoid carcinoma, melanoma, lymphoma and mesothelioma.
8.5.2.1 Sarcomatoid Carcinoma
Histologically, sarcomatoid carcinomas may be confused with undifferentiated spindle cell or pleomorphic sarcomas [60]. It is most often associated with primary breast carcinoma, renal cell carcinoma and mucosal or cutaneous squamous cell carcinoma, although it can present at any site [41]. In these cases, it is important to use IHC to identify areas of epithelial differentiation, which will support a diagnosis of carcinoma [90]. Broad-spectrum keratins, such as AE1/AE3 and pan-cytokeratin and EMA, are expressed in almost all sarcomatoid carcinoma, allowing distinction from histologically similar sarcomas [91,92,93,94].
8.5.2.2 Malignant Melanoma
Malignant melanoma can prove a diagnostic challenge for pathologists as they often mimic sarcomas, even in their immunohistochemical profile. Primary malignant melanoma, for example, can appear histologically like MPNST and clear cell sarcomas. Both MPNST and malignant melanoma have been shown to express S100 [95,96,97,98,99], as has clear cell sarcoma [100,101,102]. In this situation, the pattern of staining carries significance in delineating these entities. S100 expression is more commonly diffuse in melanoma, compared with MPNST, in which it is usually focal or multifocal. In clear cell sarcoma, staining for HMB45 is generally more intense or diffuse than S100, which is not the case in melanoma [41].
8.5.3 For Diagnosis of Mesenchymal Tumours
In some sarcomas, IHC forms a crucial part of diagnosis, where the immunohistochemical profile of a tissue sample may be diagnostic or highly suggestive of a sarcoma subtype. Examples discussed further below are rhabdomyosarcoma, gastrointestinal stromal tumours (GIST) and malignant vascular tumours.
8.5.3.1 Rhabdomyosarcomas
Rhabdomyosarcomas encompass multiple subtypes, of which embryonal rhabdomyosarcoma (ERMS) and alveolar rhabdomyosarcoma (ARMS) are the most common. Desmin, alongside more lineage-specific markers MyoD1 and myogenin, is useful for diagnosis [103, 104]. These markers are positive in almost 100% of ERMS and ARMS and up to 90% of all rhabdomyosarcomas [53, 103, 105, 106]. The expression pattern of myogenin is also of significance in these tumours. For instance, myogenin staining is often stronger and more uniform in ARMS than ERMS [107]. A diffuse expression of myogenin has also been correlated with poor survival in paediatric patients with rhabdomyosarcoma [108].
8.5.3.2 Gastrointestinal Stromal Tumours
Identification and diagnosis of gastrointestinal stromal tumours (GIST) is crucial for patient outcomes as there is a highly effective treatment available [109]. KIT (CD117) is a receptor tyrosine kinase that is activated in 85–90% of GISTs through a gain-of-function mutation [110,111,112,113]. This results in the constitutive activation of KIT receptor tyrosine kinase in a ligand-independent manner [114]. Immunohistochemical detection of CD117, therefore, is highly supportive of a GIST diagnosis. This finding is particularly significant given the availability of targeted therapies such as imatinib, an inhibitor of KIT-tyrosine kinase [115, 116]. It is important to note, however, that CD117 can be positive in other tumours including Ewing sarcoma [117,118,119] and angiosarcoma [120,121,122], so the immunohistochemical results must be interpreted in the context of clinical and radiological findings. The small subset of GISTs that are KIT-negative is often positive for DOG1, also called anoctamin-1 (Ano-1). DOG1/Ano-1 is considered the antibody of choice in addition to CD117 in the immunohistochemical testing for GISTs [123], with similar sensitivities and specificities between DOG1/Ano-1 and CD117 [124].
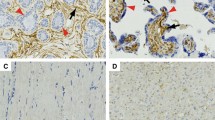
8.5.3.3 Malignant Vascular Tumours
Malignant vascular tumours encompass a broad class of tumours including angiosarcoma, epithelioid and spindle vascular tumours and Kaposi sarcoma. IHC plays a valuable role in diagnosing malignant vascular tumours because due to their wide spectrum of histopathological patterns that are not easily identifiable on histology alone. In assessing these tumours, CD31, CD34 and Fli-1 are useful immunohistochemical markers. CD31 is considered the gold-standard marker in the diagnosis of malignant vascular tumours, as it demonstrates positivity in angiosarcomas, Kaposi sarcomas and epithelioid haemangioepitheliomas [61, 125, 126]. ERG is also a highly sensitive vascular marker in the diagnosis of angiosarcoma [126]. CD34 is often positive in angiosarcoma and Kaposi sarcoma but variably expressed in epithelioid vascular tumours [61, 127]. A more recent marker, Fli-1, also demonstrates good sensitivity for spindle and epithelioid tumours [128]. Additionally, Kaposi sarcoma is an atypical vascular lesion that is uniquely defined by the presence of human herpes virus-8 (HHV-8), which can be detected by IHC [129, 130].
References
Fletcher CD. The evolving classification of soft tissue tumours—an update based on the new 2013 WHO classification. Histopathology. 2014;64(1):2–11.
Jo VY, Fletcher CD. WHO classification of soft tissue tumours: an update based on the 2013 (4th) edition. Pathology. 2014;46(2):95–104.
Wei S, Henderson-Jackson E, Qian X, Bui MM. Soft tissue tumor immunohistochemistry update: illustrative examples of diagnostic pearls to avoid pitfalls. Arch Pathol Lab Med. 2017;141(8):1072–91.
Coindre JM. Immunohistochemistry in the diagnosis of soft tissue tumours. Histopathology. 2003;43(1):1–16.
Behring Ev. Über das zustandekommen der diphtherie-immunität und der tetanus-immunität bei thieren; 1890.
Kaufmann SH. Remembering Emil von Behring: from tetanus treatment to antibody cooperation with phagocytes. MBio. 2017;8(1):e00117-17.
Kasten FH. Paul Ehrlich: pathfinder in cell biology. 1. Chronicle of his life and accomplishments in immunology, cancer research, and chemotherapy. Biotech Histochem. 1996;71(1):2–37.
Kraus R. Uber spezifische Reaktionen in keimfreien Filtraten aus Cholera, Typhus and Pestbouillonkulturen, erzeugt durch homologues Serum. Wien Klin Wochschr. 1897;10:736–8.
Marrack JR. Derived antigens as a means of studying the relation of specific combination to chemical structure: (section of therapeutics and pharmacology). Proc R Soc Med. 1934;27(8):1063–5.
Heidelberger M, Avery OT. The soluble specific substance of pneumococcus. J Exp Med. 1923;38(1):73–9.
Heidelberger M, Kendall FE. A quantitative study of the precipitin reaction between type III pneumococcus polysaccharide and purified homologous antibody. J Exp Med. 1929;50(6):809–23.
Coons AH, Creech HJ, Jones RN. Immunological properties of an antibody containing a fluorescent group. Proc Soc Exp Biol Med. 1941;47(2):200–2.
Singer SJ. Preparation of an electron-dense antibody conjugate. Nature. 1959;183(4674):1523–4.
Graham RC Jr, Karnovsky MJ. The early stages of absorption of injected horseradish peroxidase in the proximal tubules of mouse kidney: ultrastructural cytochemistry by a new technique. J Histochem Cytochem. 1966;14(4):291–302.
Leduc EH, Avrameas S, Bouteille M. Ultrastructural localization of antibody in differentiating plasma cells. J Exp Med. 1968;127(1):109–18.
Nakane PK, Pierce GB Jr. Enzyme-labeled antibodies for the light and electron microscopic localization of tissue antigens. J Cell Biol. 1967;33(2):307–18.
Sternberger LA, Hardy PH Jr, Cuculis JJ, Meyer HG. The unlabeled antibody enzyme method of immunohistochemistry: preparation and properties of soluble antigen-antibody complex (horseradish peroxidase-antihorseradish peroxidase) and its use in identification of spirochetes. J Histochem Cytochem. 1970;18(5):315–33.
Faulk WP, Taylor GM. An immunocolloid method for the electron microscope. Immunochemistry. 1971;8(11):1081–3.
Roth J, Bendayan M, Orci L. Ultrastructural localization of intracellular antigens by the use of protein A-gold complex. J Histochem Cytochem. 1978;26(12):1074–81.
Hewitt S, Robinowitz M, Bogen S, Gown A, Kalra K, Otis C, et al. Quality assurance for design control and implementation of immunohistochemistry assays: approved guideline. Wayne: Clinical Lab Standards Institute; 2011.
Dabbs DJ. Diagnostic Immunohistochemistry E-Book: theranostic and genomic applications, expert consult: online and print. Amsterdam: Elsevier Health Sciences; 2013.
Layfield LJ, Schmidt RL, Sangle N, Crim JR. Diagnostic accuracy and clinical utility of biopsy in musculoskeletal lesions: a comparison of fine-needle aspiration, core, and open biopsy techniques. Diagn Cytopathol. 2014;42(6):476–86.
Traina F, Errani C, Toscano A, Pungetti C, Fabbri D, Mazzotti A, et al. Current concepts in the biopsy of musculoskeletal tumors: AAOS exhibit selection. J Bone Joint Surg Am. 2015;97(2):e7.
Engel KB, Moore HM. Effects of preanalytical variables on the detection of proteins by immunohistochemistry in formalin-fixed, paraffin-embedded tissue. Arch Pathol Lab Med. 2011;135(5):537–43.
Taylor CR, Shi S-R, Barr N, Wu N. Techniques of immunohistochemistry: principles, pitfalls, and standardization. Diagn immunohistochem. 2013;2:1–42.
Khoury T, Sait S, Hwang H, Chandrasekhar R, Wilding G, Tan D, et al. Delay to formalin fixation effect on breast biomarkers. Mod Pathol. 2009;22(11):1457–67.
Di Tommaso L, Kapucuoglu N, Losi L, Trere D, Eusebi V. Impact of delayed fixation on evaluation of cell proliferation in intracranial malignant tumors. Appl Immunohistochem Mol Morphol. 1999;7(3):209.
Qiu J, Kulkarni S, Chandrasekhar R, Rees M, Hyde K, Wilding G, et al. Effect of delayed formalin fixation on estrogen and progesterone receptors in breast cancer: a study of three different clones. Am J Clin Pathol. 2010;134(5):813–9.
Grizzle WE. Special symposium: fixation and tissue processing models. Biotech Histochem. 2009;84(5):185–93.
Prioleau J, Schnitt SJ. p53 antigen loss in stored paraffin slides. N Engl J Med. 1995;332(22):1521–2.
Wester K, Wahlund E, Sundstrom C, Ranefall P, Bengtsson E, Russell PJ, et al. Paraffin section storage and immunohistochemistry. Effects of time, temperature, fixation, and retrieval protocol with emphasis on p53 protein and MIB1 antigen. Appl Immunohistochem Mol Morphol. 2000;8(1):61–70.
Chan JK. Advances in immunohistochemistry: impact on surgical pathology practice. Semin Diagn Pathol. 2000;17(3):170–7.
Miettinen M. Immunohistochemistry of soft tissue tumours—review with emphasis on 10 markers. Histopathology. 2014;64(1):101–18.
Kodet R. Rhabdomyosarcoma in childhood. An immunohistological analysis with myoglobin, desmin and vimentin. Pathol Res Pract. 1989;185(2):207–13.
Leader M, Patel J, Collins M, Henry K. Myoglobin: an evaluation of its role as a marker of rhabdomyosarcomas. Br J Cancer. 1989;59(1):106–9.
Johnson CW. Issues in immunohistochemistry. Toxicol Pathol. 1999;27(2):246–8.
Kim SW, Roh J, Park CS. Immunohistochemistry for pathologists: protocols, pitfalls, and tips. J Pathol Transl Med. 2016;50(6):411–8.
Goldblum JR, Weiss SW, Folpe AL. Enzinger and Weiss’s soft tissue tumors E-book: expert consult: online and print. Amsterdam: Elsevier Health Sciences; 2013.
Moll R, Franke WW, Schiller DL, Geiger B, Krepler R. The catalog of human cytokeratins: patterns of expression in normal epithelia, tumors and cultured cells. Cell. 1982;31(1):11–24.
Cooper D, Schermer A, Sun TT. Classification of human epithelia and their neoplasms using monoclonal antibodies to keratins: strategies, applications, and limitations. Lab Investig. 1985;52(3):243–56.
Doyle LA. Non-mesenchymal mimics of sarcoma. Surg Pathol Clin. 2015;8(3):493–513.
Miettinen M, Fanburg-Smith JC, Virolainen M, Shmookler BM, Fetsch JF. Epithelioid sarcoma: an immunohistochemical analysis of 112 classical and variant cases and a discussion of the differential diagnosis. Hum Pathol. 1999;30(8):934–42.
Wrba F, Fertl H, Amann G, Tell E, Krepler R. Epithelial markers in synovial sarcoma. An immunohistochemical study on paraffin embedded tissues. Virchows Arch A Pathol Anat Histopathol. 1989;415(3):253–8.
Ordonez NG, Mahfouz SM, Mackay B. Synovial sarcoma: an immunohistochemical and ultrastructural study. Hum Pathol. 1990;21(7):733–49.
Lopes JM, Bjerkehagen B, Holm R, Bruland O, Sobrinho-Simoes M, Nesland JM. Immunohistochemical profile of synovial sarcoma with emphasis on the epithelial-type differentiation. A study of 49 primary tumours, recurrences and metastases. Pathol Res Pract. 1994;190(2):168–77.
van de Rijn M, Barr FG, Xiong QB, Hedges M, Shipley J, Fisher C. Poorly differentiated synovial sarcoma: an analysis of clinical, pathologic, and molecular genetic features. Am J Surg Pathol. 1999;23(1):106–12.
Kilpatrick SE, Hitchcock MG, Kraus MD, Calonje E, Fletcher CD. Mixed tumors and myoepitheliomas of soft tissue: a clinicopathologic study of 19 cases with a unifying concept. Am J Surg Pathol. 1997;21(1):13–22.
Michal M, Miettinen M. Myoepitheliomas of the skin and soft tissues. Report of 12 cases. Virchows Arch. 1999;434(5):393–400.
Pinkus GS, Kurtin PJ. Epithelial membrane antigen—a diagnostic discriminant in surgical pathology: immunohistochemical profile in epithelial, mesenchymal, and hematopoietic neoplasms using paraffin sections and monoclonal antibodies. Hum Pathol. 1985;16(9):929–40.
Bresnick AR, Weber DJ, Zimmer DB. S100 proteins in cancer. Nat Rev Cancer. 2015;15(2):96–109.
Hermann A, Donato R, Weiger TM, Chazin WJ. S100 calcium binding proteins and ion channels. Front Pharmacol. 2012;3:67.
Donato R, Cannon BR, Sorci G, Riuzzi F, Hsu K, Weber DJ, et al. Functions of S100 proteins. Curr Mol Med. 2013;13(1):24–57.
Truong LD, Rangdaeng S, Cagle P, Ro JY, Hawkins H, Font RL. The diagnostic utility of desmin. A study of 584 cases and review of the literature. Am J Clin Pathol. 1990;93(3):305–14.
Rangdaeng S, Truong LD. Comparative immunohistochemical staining for desmin and muscle-specific actin. A study of 576 cases. Am J Clin Pathol. 1991;96(1):32–45.
Machado I, Mayordomo-Aranda E, Giner F, Llombart-Bosch A. The role of immunohistochemistry in rhabdomyosarcoma diagnosis using tissue microarray technology and a xenograft model. Fetal Pediatr Pathol. 2015;34(5):271–81.
Gerald WL, Miller HK, Battifora H, Miettinen M, Silva EG, Rosai J. Intra-abdominal desmoplastic small round-cell tumor. Report of 19 cases of a distinctive type of high-grade polyphenotypic malignancy affecting young individuals. Am J Surg Pathol. 1991;15(6):499–513.
Ordonez NG. Desmoplastic small round cell tumor: II: an ultrastructural and immunohistochemical study with emphasis on new immunohistochemical markers. Am J Surg Pathol. 1998;22(11):1314–27.
Qiu X, Montgomery E, Sun B. Inflammatory myofibroblastic tumor and low-grade myofibroblastic sarcoma: a comparative study of clinicopathologic features and further observations on the immunohistochemical profile of myofibroblasts. Hum Pathol. 2008;39(6):846–56.
Folpe AL, Weiss SW, Fletcher CD, Gown AM. Tenosynovial giant cell tumors: evidence for a desmin-positive dendritic cell subpopulation. Mod Pathol. 1998;11(10):939–44.
Hornick JL. Practical soft tissue pathology: a diagnostic approach E-Book: a volume in the pattern recognition series. Amsterdam: Elsevier Health Sciences; 2017.
Miettinen M, Lindenmayer AE, Chaubal A. Endothelial cell markers CD31, CD34, and BNH9 antibody to H- and Y-antigens—evaluation of their specificity and sensitivity in the diagnosis of vascular tumors and comparison with von Willebrand factor. Mod Pathol. 1994;7(1):82–90.
Kanitakis J, Narvaez D, Claudy A. Expression of the CD34 antigen distinguishes Kaposi’s sarcoma from pseudo-Kaposi’s sarcoma (acroangiodermatitis). Br J Dermatol. 1996;134(1):44–6.
Fellinger EJ, Garin-Chesa P, Su SL, DeAngelis P, Lane JM, Rettig WJ. Biochemical and genetic characterization of the HBA71 Ewing’s sarcoma cell surface antigen. Cancer Res. 1991;51(1):336–40.
Ambros IM, Ambros PF, Strehl S, Kovar H, Gadner H, Salzer-Kuntschik M. MIC2 is a specific marker for Ewing’s sarcoma and peripheral primitive neuroectodermal tumors. Evidence for a common histogenesis of Ewing’s sarcoma and peripheral primitive neuroectodermal tumors from MIC2 expression and specific chromosome aberration. Cancer. 1991;67(7):1886–93.
Fellinger EJ, Garin-Chesa P, Triche TJ, Huvos AG, Rettig WJ. Immunohistochemical analysis of Ewing’s sarcoma cell surface antigen p30/32MIC2. Am J Pathol. 1991;139(2):317–25.
Folpe AL, Goldblum JR, Rubin BP, Shehata BM, Liu W, Dei Tos AP, et al. Morphologic and immunophenotypic diversity in Ewing family tumors: a study of 66 genetically confirmed cases. Am J Surg Pathol. 2005;29(8):1025–33.
Parham DM. Immunohistochemical markers of soft tissue tumors: pathologic diagnosis, genetic contributions, and therapeutic options. Anal Chem Insights. 2015;10(Suppl 1):1–10.
Folpe AL, Hill CE, Parham DM, O’Shea PA, Weiss SW. Immunohistochemical detection of FLI-1 protein expression: a study of 132 round cell tumors with emphasis on CD99-positive mimics of Ewing’s sarcoma/primitive neuroectodermal tumor. Am J Surg Pathol. 2000;24(12):1657–62.
Turc-Carel C, Aurias A, Mugneret F, Lizard S, Sidaner I, Volk C, et al. Chromosomes in Ewing’s sarcoma. I. An evaluation of 85 cases of remarkable consistency of t(11;22)(q24;q12). Cancer Genet Cytogenet. 1988;32(2):229–38.
Zucman J, Delattre O, Desmaze C, Plougastel B, Joubert I, Melot T, et al. Cloning and characterization of the Ewing’s sarcoma and peripheral neuroepithelioma t(11;22) translocation breakpoints. Genes Chromosomes Cancer. 1992;5(4):271–7.
Delattre O, Zucman J, Plougastel B, Desmaze C, Melot T, Peter M, et al. Gene fusion with an ETS DNA-binding domain caused by chromosome translocation in human tumours. Nature. 1992;359(6391):162–5.
Nilsson G, Wang M, Wejde J, Kreicbergs A, Larsson O. Detection of EWS/FLI-1 by immunostaining. an adjunctive tool in diagnosis of Ewing’s sarcoma and primitive neuroectodermal tumour on cytological samples and paraffin-embedded archival material. Sarcoma. 1999;3(1):25–32.
Mandahl N, Akerman M, Aman P, Dal Cin P, De Wever I, Fletcher CD, et al. Duplication of chromosome segment 12q15-24 is associated with atypical lipomatous tumors: a report of the CHAMP collaborative study group. CHromosomes And MorPhology. Int J Cancer. 1996;67(5):632–5.
Rosai J, Akerman M, Dal Cin P, DeWever I, Fletcher CD, Mandahl N, et al. Combined morphologic and karyotypic study of 59 atypical lipomatous tumors. Evaluation of their relationship and differential diagnosis with other adipose tissue tumors (a report of the CHAMP Study Group). Am J Surg Pathol. 1996;20(10):1182–9.
Binh MB, Sastre-Garau X, Guillou L, de Pinieux G, Terrier P, Lagace R, et al. MDM2 and CDK4 immunostainings are useful adjuncts in diagnosing well-differentiated and dedifferentiated liposarcoma subtypes: a comparative analysis of 559 soft tissue neoplasms with genetic data. Am J Surg Pathol. 2005;29(10):1340–7.
Binh MB, Garau XS, Guillou L, Aurias A, Coindre JM. Reproducibility of MDM2 and CDK4 staining in soft tissue tumors. Am J Clin Pathol. 2006;125(5):693–7.
Davanzo B, Emerson RE, Lisy M, Koniaris LG, Kays JK. Solitary fibrous tumor. Transl Gastroenterol Hepatol. 2018;3:94.
Rakheja D, Molberg KH, Roberts CA, Jaiswal VR. Immunohistochemical expression of beta-catenin in solitary fibrous tumors. Arch Pathol Lab Med. 2005;129(6):776–9.
Vogels RJ, Vlenterie M, Versleijen-Jonkers YM, Ruijter E, Bekers EM, Verdijk MA, et al. Solitary fibrous tumor—clinicopathologic, immunohistochemical and molecular analysis of 28 cases. Diagn Pathol. 2014;9:224.
Akaike K, Kurisaki-Arakawa A, Hara K, Suehara Y, Takagi T, Mitani K, et al. Distinct clinicopathological features of NAB2-STAT6 fusion gene variants in solitary fibrous tumor with emphasis on the acquisition of highly malignant potential. Hum Pathol. 2015;46(3):347–56.
Koelsche C, Schweizer L, Renner M, Warth A, Jones DT, Sahm F, et al. Nuclear relocation of STAT6 reliably predicts NAB2-STAT6 fusion for the diagnosis of solitary fibrous tumour. Histopathology. 2014;65(5):613–22.
Mohajeri A, Tayebwa J, Collin A, Nilsson J, Magnusson L, von Steyern FV, et al. Comprehensive genetic analysis identifies a pathognomonic NAB2/STAT6 fusion gene, nonrandom secondary genomic imbalances, and a characteristic gene expression profile in solitary fibrous tumor. Genes Chromosomes Cancer. 2013;52(10):873–86.
Yoshida A, Tsuta K, Ohno M, Yoshida M, Narita Y, Kawai A, et al. STAT6 immunohistochemistry is helpful in the diagnosis of solitary fibrous tumors. Am J Surg Pathol. 2014;38(4):552–9.
Rao N, Colby TV, Falconieri G, Cohen H, Moran CA, Suster S. Intrapulmonary solitary fibrous tumors: clinicopathologic and immunohistochemical study of 24 cases. Am J Surg Pathol. 2013;37(2):155–66.
Plaza JA, Mayerson J, Wakely PE Jr. Nodular fasciitis of the hand: a potential diagnostic pitfall in fine-needle aspiration cytopathology. Am J Clin Pathol. 2005;123(3):388–93.
Luna A, Molinari L, Bollea Garlatti LA, Ferrario D, Volonteri V, Roitman P, et al. Nodular fasciitis, a forgotten entity. Int J Dermatol. 2019;58(2):190–3.
Khanna V, Rajan M, Reddy T, Alexander N, Surendran P. Nodular fasciitis mimicking a soft tissue sarcoma—a case report. Int J Surg Case Rep. 2018;44:29–32.
Lu L, Lao IW, Liu X, Yu L, Wang J. Nodular fasciitis: a retrospective study of 272 cases from China with clinicopathologic and radiologic correlation. Ann Diagn Pathol. 2015;19(3):180–5.
Magro G. Differential diagnosis of benign spindle cell lesions. Surg Pathol Clin. 2018;11(1):91–121.
Wick MR, Ritter JH, Humphrey PA. Sarcomatoid carcinomas of the lung: a clinicopathologic review. Am J Clin Pathol. 1997;108(1):40–53.
Guarino M, Tricomi P, Giordano F, Cristofori E. Sarcomatoid carcinomas: pathological and histopathogenetic considerations. Pathology. 1996;28(4):298–305.
Lewis JE, Olsen KD, Sebo TJ. Spindle cell carcinoma of the larynx: review of 26 cases including DNA content and immunohistochemistry. Hum Pathol. 1997;28(6):664–73.
Nishihara K, Tsuneyoshi M. Undifferentiated spindle cell carcinoma of the gallbladder: a clinicopathologic, immunohistochemical, and flow cytometric study of 11 cases. Hum Pathol. 1993;24(12):1298–305.
Taskin OC, Akkas G, Memis B, Seven IE, Basturk O, Jang KT, et al. Sarcomatoid carcinomas of the gallbladder: clinicopathologic characteristics. Virchows Arch. 2019;475(1):59–66.
Wick MR, Swanson PE, Scheithauer BW, Manivel JC. Malignant peripheral nerve sheath tumor. An immunohistochemical study of 62 cases. Am J Clin Pathol. 1987;87(4):425–33.
Giangaspero F, Fratamico FC, Ceccarelli C, Brisigotti M. Malignant peripheral nerve sheath tumors and spindle cell sarcomas: an immunohistochemical analysis of multiple markers. Appl Pathol. 1989;7(2):134–44.
Romano RC, Carter JM, Folpe AL. Aberrant intermediate filament and synaptophysin expression is a frequent event in malignant melanoma: an immunohistochemical study of 73 cases. Mod Pathol. 2015;28(8):1033–42.
Bolander A, Agnarsdottir M, Wagenius G, Stromberg S, Ponten F, Ekman S, et al. Serological and immunohistochemical analysis of S100 and new derivatives as markers for prognosis in patients with malignant melanoma. Melanoma Res. 2008;18(6):412–9.
Prieto VG, Shea CR. Use of immunohistochemistry in melanocytic lesions. J Cutan Pathol. 2008;35(Suppl 2):1–10.
Dim DC, Cooley LD, Miranda RN. Clear cell sarcoma of tendons and aponeuroses: a review. Arch Pathol Lab Med. 2007;131(1):152–6.
Hisaoka M, Ishida T, Kuo TT, Matsuyama A, Imamura T, Nishida K, et al. Clear cell sarcoma of soft tissue: a clinicopathologic, immunohistochemical, and molecular analysis of 33 cases. Am J Surg Pathol. 2008;32(3):452–60.
Hantschke M, Mentzel T, Rutten A, Palmedo G, Calonje E, Lazar AJ, et al. Cutaneous clear cell sarcoma: a clinicopathologic, immunohistochemical, and molecular analysis of 12 cases emphasizing its distinction from dermal melanoma. Am J Surg Pathol. 2010;34(2):216–22.
Wang NP, Marx J, McNutt MA, Rutledge JC, Gown AM. Expression of myogenic regulatory proteins (myogenin and MyoD1) in small blue round cell tumors of childhood. Am J Pathol. 1995;147(6):1799–810.
Cui S, Hano H, Harada T, Takai S, Masui F, Ushigome S. Evaluation of new monoclonal anti-MyoD1 and anti-myogenin antibodies for the diagnosis of rhabdomyosarcoma. Pathol Int. 1999;49(1):62–8.
Kumar S, Perlman E, Harris CA, Raffeld M, Tsokos M. Myogenin is a specific marker for rhabdomyosarcoma: an immunohistochemical study in paraffin-embedded tissues. Mod Pathol. 2000;13(9):988–93.
Wijnaendts LC, van der Linden JC, van Unnik AJ, Delemarre JF, Voute PA, Meijer CJ. The expression pattern of contractile and intermediate filament proteins in developing skeletal muscle and rhabdomyosarcoma of childhood: diagnostic and prognostic utility. J Pathol. 1994;174(4):283–92.
Dias P, Chen B, Dilday B, Palmer H, Hosoi H, Singh S, et al. Strong immunostaining for myogenin in rhabdomyosarcoma is significantly associated with tumors of the alveolar subclass. Am J Pathol. 2000;156(2):399–408.
Heerema-McKenney A, Wijnaendts LC, Pulliam JF, Lopez-Terrada D, McKenney JK, Zhu S, et al. Diffuse myogenin expression by immunohistochemistry is an independent marker of poor survival in pediatric rhabdomyosarcoma: a tissue microarray study of 71 primary tumors including correlation with molecular phenotype. Am J Surg Pathol. 2008;32(10):1513–22.
Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Int J Surg Pathol. 2002;10(2):81–9.
Lux ML, Rubin BP, Biase TL, Chen CJ, Maclure T, Demetri G, et al. KIT extracellular and kinase domain mutations in gastrointestinal stromal tumors. Am J Pathol. 2000;156(3):791–5.
Rubin BP, Singer S, Tsao C, Duensing A, Lux ML, Ruiz R, et al. KIT activation is a ubiquitous feature of gastrointestinal stromal tumors. Cancer Res. 2001;61(22):8118–21.
Corless CL, McGreevey L, Haley A, Town A, Heinrich MC. KIT mutations are common in incidental gastrointestinal stromal tumors one centimeter or less in size. Am J Pathol. 2002;160(5):1567–72.
Yarden Y, Kuang WJ, Yang-Feng T, Coussens L, Munemitsu S, Dull TJ, et al. Human proto-oncogene c-kit: a new cell surface receptor tyrosine kinase for an unidentified ligand. EMBO J. 1987;6(11):3341–51.
Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279(5350):577–80.
van Oosterom AT, Judson I, Verweij J, Stroobants S, Donato di Paola E, Dimitrijevic S, et al. Safety and efficacy of imatinib (STI571) in metastatic gastrointestinal stromal tumours: a phase I study. Lancet. 2001;358(9291):1421–3.
Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD, Eisenberg B, Roberts PJ, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002;347(7):472–80.
Scotlandi K, Manara MC, Strammiello R, Landuzzi L, Benini S, Perdichizzi S, et al. C-kit receptor expression in Ewing’s sarcoma: lack of prognostic value but therapeutic targeting opportunities in appropriate conditions. J Clin Oncol. 2003;21(10):1952–60.
Ahmed A, Gilbert-Barness E, Lacson A. Expression of c-kit in Ewing family of tumors: a comparison of different immunohistochemical protocols. Pediatr Dev Pathol. 2004;7(4):342–7.
Gonzalez I, Andreu EJ, Panizo A, Inoges S, Fontalba A, Fernandez-Luna JL, et al. Imatinib inhibits proliferation of Ewing tumor cells mediated by the stem cell factor/KIT receptor pathway, and sensitizes cells to vincristine and doxorubicin-induced apoptosis. Clin Cancer Res. 2004;10(2):751–61.
Miettinen M, Sarlomo-Rikala M, Lasota J. KIT expression in angiosarcomas and fetal endothelial cells: lack of mutations of exon 11 and exon 17 of C-kit. Mod Pathol. 2000;13(5):536–41.
Hornick JL, Fletcher CD. Immunohistochemical staining for KIT (CD117) in soft tissue sarcomas is very limited in distribution. Am J Clin Pathol. 2002;117(2):188–93.
Komdeur R, Hoekstra HJ, Molenaar WM, Van Den Berg E, Zwart N, Pras E, et al. Clinicopathologic assessment of postradiation sarcomas: KIT as a potential treatment target. Clin Cancer Res. 2003;9(8):2926–32.
Novelli M, Rossi S, Rodriguez-Justo M, Taniere P, Seddon B, Toffolatti L, et al. DOG1 and CD117 are the antibodies of choice in the diagnosis of gastrointestinal stromal tumours. Histopathology. 2010;57(2):259–70.
Miettinen M, Wang ZF, Lasota J. DOG1 antibody in the differential diagnosis of gastrointestinal stromal tumors: a study of 1840 cases. Am J Surg Pathol. 2009;33(9):1401–8.
De Young BR, Frierson HF Jr, Ly MN, Smith D, Swanson PE. CD31 immunoreactivity in carcinomas and mesotheliomas. Am J Clin Pathol. 1998;110(3):374–7.
Sullivan HC, Edgar MA, Cohen C, Kovach CK, HooKim K, Reid MD. The utility of ERG, CD31 and CD34 in the cytological diagnosis of angiosarcoma: an analysis of 25 cases. J Clin Pathol. 2015;68(1):44–50.
Suster S, Fisher C. Immunoreactivity for the human hematopoietic progenitor cell antigen (CD34) in lipomatous tumors. Am J Surg Pathol. 1997;21(2):195–200.
Folpe AL, Chand EM, Goldblum JR, Weiss SW. Expression of Fli-1, a nuclear transcription factor, distinguishes vascular neoplasms from potential mimics. Am J Surg Pathol. 2001;25(8):1061–6.
Cheuk W, Wong KO, Wong CS, Dinkel JE, Ben-Dor D, Chan JK. Immunostaining for human herpesvirus 8 latent nuclear antigen-1 helps distinguish Kaposi sarcoma from its mimickers. Am J Clin Pathol. 2004;121(3):335–42.
Patel RM, Goldblum JR, Hsi ED. Immunohistochemical detection of human herpes virus-8 latent nuclear antigen-1 is useful in the diagnosis of Kaposi sarcoma. Mod Pathol. 2004;17(4):456–60.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Tran, V., Slavin, J. (2021). Immunohistochemistry in Bone and Soft Tissue Tumours. In: Choong, P.F.M. (eds) Sarcoma . Springer, Singapore. https://doi.org/10.1007/978-981-15-9414-4_8
Download citation
DOI: https://doi.org/10.1007/978-981-15-9414-4_8
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-9413-7
Online ISBN: 978-981-15-9414-4
eBook Packages: MedicineMedicine (R0)