Abstract
Atrophy is a classical hallmark of an array of disorders that affect skeletal muscle, ranging from inherited dystrophies, acquired inflammatory myopathies, ageing (sarcopenia) and critical illness (sepsis). The loss of muscle mass and function in these instances is associated with disability, poor quality of life and in some cases mortality. The mechanisms which underpin muscle atrophy are complex; however, significant research has demonstrated an important role for inflammatory cytokines such as tumour necrosis factor-alpha (TNF-α), mediated by the generation of reactive oxygen species (ROS) in muscle wasting. Moreover, activation of the transcription factor nuclear factor kappa B (NF-κB) is a key lynchpin in the overall processes that mediate muscle atrophy. The significance of NF-κB as a key regulator of muscle atrophy has been emphasised by several in vivo studies, which have demonstrated that NF-κB-targeted therapies can abrogate muscle atrophy. In this chapter, we will summarise current knowledge on the role of cytokines (TNF-α) and NF-κB in the loss of muscle mass and function and highlight perspectives towards future research and potential therapies to combat muscle atrophy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Skeletal muscle is a robust and plastic organ; accounting for approximately 40% total body weight and 50% total protein and is responsible for ambulation, postural support, metabolic homeostasis and thermogenesis. Skeletal muscle is plastic in the sense of its capability of rapidly responding to load, in terms of training or disuse; and these features undoubtedly underpinned the success of our species in hunter-gather times [1]. However, in response to an array of pathological stimuli, it is dysregulation in mechanisms of plasticity which gives rise to atrophy of muscle. Skeletal muscle atrophy is defined as loss of muscle mass, derived from imbalance between rates of protein synthesis and degradation [2]. We observe muscle atrophy in an array of pathogenic states, ranging from inherited (DMD) and acquired (myositis) myopathies to sepsis (hyper-inflammation and disuse) and age-related loss of muscle mass (sarcopenia) [2]. In these instances, we observe a reduction in muscle fibre cross-sectional area and thus a reduction in force output – which manifests as muscle weakness and reduced capacity to exercise – collectively resulting in impaired quality of life. The cellular mechanisms, which are responsible for muscle atrophy, are indeed complex. However, significant research of the last ~20 years has indicated that nuclear factor kappa B (NF-κB) pathway activation and inflammatory cytokines such as TNF-α are key players in muscle atrophy. In this chapter, we discuss the basic biology of NF-κB signalling, the evidence demonstrating the role of NF-κB as a lynchpin in muscle atrophy – intertwined with the role of cytokines in atrophy – and how pharmacologically targeting NF-κB may be an avenue for therapy.
2 NF-kB and Muscle Atrophy
2.1 The NF-kB Signalling Pathway
NF-κB is a pleiotropic, redox-sensitive, nuclear transcription factor, which regulates the expression of a vast array of genes, associated with a diverse range of biological processes – ranging from innate and adaptive immune responses to cell growth, maturation and survival [3]. NF-κB plays a crucial role in allowing cells to adapt to a diverse array of environmental stimuli. In mammalian species NF-κB is comprised of the subunits p50, p52 p65 (RelA), c-Rel and RelB [4]. The individual protein subunits of NF-κB bind together to form heterodimers that are defined as the NF-κB complex. Dimerisation occurs at a region termed the rel-homology domain (RHD). The RHD is located on the N-terminus of each NF-κB unit and is approximately 300 amino acid bases in length [5]. There are 15 known dimers that have been identified to form NF-κB units. There is relative homology between the subunits, however key differences in p50 and p52 are apparent, whereby they lack a transactivational domain at their C-terminus; p50/52 homodimers do not activate transcription upon migration to the nucleus. One of the most characteristic dimers, which do activate transcription, is the p65/50 dimer [3].
NF-κB resides in the cytosol of cells in an inactive state, tightly bound to IκB, comprised of several subunits: IκBα, IκBβ, IκBγ and IκBε [3]. IκB forms covalent bonds with NF-κB that maintains it in a state of inactivity. Although inactive NF-κB is described as cytosolic, the NF-κB-IκB complex is constantly migrating in a cyclical fashion to and from the nucleus [6]. IκB prevents any significant binding of NF-κB to DNA, and the net export from the nucleus is greater than that of the import – implying NF-κB to be cytosolic in origin [6]. NF-κB activation occurs by severing of covalent bonds with IκB via the action of the IκB kinase (IKK). IKK is a kinase, which phosphorylates IκB and initiates IκB degradation via the ubiquitin-proteasome pathway – leaving NF-κB free and active, which then translocates to the nucleus and binds to requisite promoter sequences at the κB domains [4].
NF-κB activation can occur in response to a variety of stimuli from viral and bacterial components to pro-inflammatory cytokines – however, one of the most well-characterised activators is TNF-α [6]. The canonical activation of NF-κB due to degradation of the inhibitor of kappa B alpha/beta (IKBα/β) by IκB kinase (IKK) is TNF-dependent [3]. The activation of IKKβ by TNF-α occurs due to translocation of IKKβ to the membrane by the chaperones CDC37 and HSP90; the activation of IKKβ is RIP-dependent. IKKβ phosphorylates the IKBα and IKBβ subunits which bind to and stabilise NF-κB in an inactivate state in the cytoplasm. TNF-α is produced by a variety of cell types, such as monocytes, macrophages, NK cells, endothelial cells, smooth muscle cells [7] in skeletal muscle [8] and adipocytes [9].
2.2 NF-κB in Muscle Disease
There is an overwhelming body of evidence delineating the important role for NF-κB in muscle wasting – in part, derived from a pivotal study in 2000. Authors demonstrated a key role for NF-κB in the loss of MyoD in cachexia – mediated via TNF-α/IFN-γ gamma signalling [10]. Research in more recent years has expanded our understanding in this context, with in vitro, in vivo, and now strong clinical evidence – reporting NF-κB as a key lynchpin in muscle atrophy.
Sarcopenia is the age-related loss of muscle mass – which typically occurs from the fifth decade of life onwards – with upwards of 50% loss of muscle mass observed in the eighth decade [11]. Loss of muscle mass and function in ageing is associated with frailty and impaired quality of life – and is an overall significant socioeconomic burden. During ageing we observed a loss of overall muscle fibre number and a reduction in cross-sectional area of those remaining fibres. Studies examining the role of NF-κB in the context of ageing have demonstrated elevated NF-κB content was fourfold higher in the medial vastus lateralis of elderly men (70 ± 1 years) when compared with young men (28 ± 1 years) [12]. In murine studies, anterior tibialis muscle of aged mice showed an aberrant persistent activation of NF-κB DNA binding activity [13]. Collectively, these studies illustrate a constitutive activation of NF-κB in aged muscle; however, the precise mechanism of action in the context of sarcopenia is poorly understood.
The idiopathic inflammatory myopathies, collectively termed myositis, are a group of heterogeneous acquired autoimmune disease, which primarily target skeletal muscle. Myositis can be subcategorised into polymyositis (PM), dermatomyositis (DM) and inclusion body myositis (IBM) characterised by profound muscle wasting, weakness and disability. Elevated circulating and muscle levels of cytokines, such as TNF-α and IFN-γ alongside deposition of CD4/CD8 T-cells in muscle, are all hallmarks of disease [14]. The NF-κB pathway has been investigated in the context of myositis, with both PM and DM biopsies showing NF-κB activation [15]. Moreover, immunohistochemical investigations of biopsies from IBM patients showed increased deposition of p50 and p65 subunits in diseased muscle fibres [16]. An intriguing hallmark of myositis is the overexpression of major histocompatibility complex (MHC) I on the muscle fibre surface [17]. Mechanistic in vitro and in vivo studies have demonstrated that MHC I overexpression can drive NF-κB activation in muscle [18].
In terms of inherited myopathies, the X-linked recessive disorder Duchenne muscular dystrophy (DMD) has received significant attention in the context of NF-κB. DMD is a chronic degenerative neuromuscular disease, characterised by muscle lacking functional dystrophin protein [19]. Consequently, profound damage to the muscle fibre membrane occurs, which is a key driver of the degeneration of muscle in DMD. The muscle of DMD patients undergoes cyclical bouts of damage (degeneration) and regeneration – with invasion of immune cells, a secondary feature of the disease. Analysis of biopsy tissue from patients with DMD showed enhanced NF-κB DNA binding activity, determined by electrophoretic mobility shift assay (EMSA) [15]. Furthermore, studies in the mdx model of DMD have further highlighted NF-κB pathway activation in muscle using EMSA [20]. There is a prevailing theory that dysregulation of NF-κB signalling in DMD contributes the muscle inflammation and degradation. Thus, there is interest in pursuing novel NF-κB-targeted therapies to combat this process. Collectively, there is significant evidence to demonstrate a potential role for NF-κB in mediating the pathogenesis in a range of acquired and inherited myopathies.
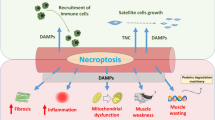
2.3 Mechanisms of NF-κB-Mediated Muscle Atrophy
Here we highlight mechanisms researchers have identified, which muscle atrophy and wasting are mediated through, in the context of NF-κB pathway activation (Fig. 12.1). As a pleiotropic transcription factor, NF-κB regulates a plethora of genes, of which a proportion encode an array of cytokines and chemokines. Given the aforementioned myopathies in this chapter harbour significant inflammatory cell components (either as a primary in IIM or secondary pathogenic feature in DMD) to their pathogenesis, it is not surprising to see NF-κB as a lynchpin to some of those effects. Moreover, the notion that skeletal muscle is now considered an endocrine organ, capable of releasing an array of proteins and peptides – such as certain cytokines and chemokines – offers an interesting perspective. Studies have shown that treatment of C2C12 myotubes with TNF-α induces the upregulation of inflammatory cytokine gene expression and release [21, 22]. Moreover, cytokine and chemokine release is regulated by NF-κB activation, mediated by free radical generation by the mitochondria [22]. The release of catabolic cytokines such as IL-6 may have paracrine signalling effects on neighbouring fibres and may self-perpetuate atrophy. The perspective of muscle-derived cytokines (myokines) rather than solely derived from immune cells is an additional facet to disease pathogenesis in myopathologies.
In muscle atrophy, we typically observe an imbalance in protein synthetic and degradative pathways. Specifically, we see activation of the ubiquitin-proteasome network – which regulates protein degradation. Poly-ubiquitination of proteins by the E3 ubiquitin ligases muscle RING finger protein 1 (MuRF1) and atrogin-1 targets proteins for degradation via the proteasome [23, 24]. There is now elegant evidence which describes how NF-κB signalling and the ubiquitin-proteasome pathway are intertwined in the context of atrophy. Overexpression of IKKβ in a murine model was elevated MuRF1 expression – which was ablated in MuRF1-knockout cross strain [25]. Moreover, a study using a muscle-specific knockout of IKKβ in a mouse model, prevented NF-κB activation, and subsequent muscle wasting in response to denervation [26]. Thus, there is elegant evidence which shows the interplay between protein degradation pathways and NF-κB activation in terms of muscle atrophy. Mechanistically, this evidence provides a strong justification in the pursuit of NF-κB-modifying therapies and agents in an effort to combat muscle-wasting disorders.
2.4 Therapeutic Targeting of NF-κB Activation
There is now a bourgeoning array of both synthetic and natural compounds, which have been characterised to target different aspects of NF-κB signalling. Given the strong association with NF-κB and muscle atrophy, it is perhaps logical to pursue interventions in this context. Some focus has been on targeting in the activators of NF-κB activation, with the focus on TNF-α. There is an array of biologics, comprising either monoclonal antibodies to TNF-α (e.g. infliximab) or decoy TNF receptors (e.g. etanercept) – which have been put to great use in the rheumatic diseases [27]. Both of these drugs have been tested and shown some beneficial effects in the mdx model of DMD – reducing myonecrosis and suppressing overall inflammation [28, 29]. In contrast, in patients with myositis, who often have elevated expression of TNF-α in muscle, the effectiveness of anti-TNF therapies is not convincing [30]. If indeed NF-κB signalling has a role to play in muscle atrophy in myositis, then perhaps more NF-κB-centric therapies may be worthy of pursuit. In terms of more NF-κB-centric/selective therapies, the NEMO-binding domain (NBD) peptide offers that opportunity. The NBD peptide disrupts the correct assembly of the IKK complex – which prevents canonical NF-κB pathway activation. Utilisation of NBD peptide in the mdx model of DMD significantly reduced macrophage invasion into muscle and reduced overall membrane damage/lysis [20] . The salicylates have also been shown to have the capacity to inhibit NF-κB activation [31]. Administration of sodium salicylate in aged mice results in downregulation in inflammatory gene expression and improved repair of muscle [32]. In terms of natural compounds to target NF-κB signalling, curcumin (the primary curcumoid component of turmeric) harbours anti-NF-κB properties [33]. Treatment of mdx mice with curcumin resulted in improved muscle strength, increased sarcolemmal integrity and a downregulation of inflammatory markers [34].
3 Cytokines in Muscle Atrophy
3.1 Tumour Necrosis Factor-Alpha
TNF-α is a 157-amino-acid-long peptide encoded on the short arm of chromosome 6 in humans [35] and exists in both soluble and membrane-bound forms. TNF-α is initially produced as 26 kDa membrane-spanning protein, anchored in place due to a 79-amino acid precursor sequence. Subsequent proteolytic cleavage frees TNF-α from the membrane into a 17 kDa soluble form [36]. TNF-α exists in circulation as a homotrimer, approximately 52 kDa in size [37], which binds to approximately 25 different receptors [7]; however, the most prevalent and well characterised are TNF receptors 1 and 2 (TNFR-1/2) [38]. TNFR-1 is fairly ubiquitously expressed across a range of cell types, whereas TNFR-2 seems to be more confined to cells of a haematopoietic origin [39]. Moreover, the vast majority of biological functions of TNF-α occur via TNFR-1 [40]. The signalling cascade initiated via TNF-α binding of TNFR-1 is very well characterised (Fig. 12.1). The TNF-α homotrimer binds the TNFR-1 forming the TNF-TNFR-1 complex, where the intracellular domain is recognised and recruits TNF-receptor-associated death domain (TRADD) to the complex. Additional adaptor proteins are recruited to the complex, namely, receptor-interacting protein (RIP) and TNF-R-associated factor 2 (TRAF-2). The function of TRAF-2 is to recruit the protein cellular inhibitor of apoptosis 1 (cIAP-1) which also activates the mitogen-associated protein kinase pathway (MAPK) [40]. However, RIP is a key component of TNF-α signalling by the activation of nuclear factor kappa B (NF-κB).
3.2 TNF-α and Skeletal Muscle Wasting
The biological importance of TNF-α was demonstrated in several key studies throughout the 1970s and 1980s. TNF-α was originally discovered over 30 years ago as a serum soluble molecule, released by macrophages, which suppressed tumour growth significantly in mice [41]. TNF-α was characterised to be the hormone termed cachectin, which induced profound cachexia in mice [42]. Treatment of rats with recombinant TNF-α was found to induce a state of septic shock [43]. Administration of anti-TNF-α antibodies during endotoxin-induced insult provided protection against septic shock-induced cachexia and reduced overall morbidity [44]. These important studies provided a key insight into the deleterious role of TNF-α during instances of profound bacterial infection and that TNF-α is likely to be a key mediator of cachexia (muscle atrophy). Sepsis patients characteristically present with profound elevations in circulating levels of TNF-α [45]. Elevated circulating TNF-α is a key driver in the significant loss of total protein ~16%, which occurs over a 3-week period in patients with severe sepsis [46]. Moreover, experimental rodent models of sepsis have shown that reduced protein synthesis is associated with disrupted ribosomal s6 kinase phosphorylation in a TNF-α-dependent manner [47].
The exposure of muscle to TNF-α results in a loss of total muscle protein, a process that is reported to be regulated by NF-κB; additionally the loss of muscle protein demonstrated in this study was correlated with elevated ubiquitin conjugation and augmented by endogenous production of ROS [48]. Overexpression of the IκBα protein (which holds NF-κB in its inactive state) in muscle results in resistance to TNF-α-induced protein loss [49]. Studies examining the inhibition of NF-κB activation in vivo demonstrated improved skeletal muscle regeneration following trauma [50]. Thus, there is a clear association between TNF-α, NF-κB activation and muscle atrophy.
Although the loss of muscle protein as a consequence of TNF-α exposure is profound, it has been reported that the loss of muscle protein is superseded by a significant fall in specific force generation by muscle [51]. Studies into muscle contractility in the diaphragm consistently report a fall in specific force generation in response to elevated levels of TNF-α [52]. Moreover this occurrence has been reported in the absence of muscle wasting [53]. Further studies have demonstrated loss of muscle function in the absence of atrophy, via TNF-α-induced activation of caspase-3, which may be due to the loss of the actin and myosin contractile filaments [54]. Studies have reported that TNF-α-induced loss of muscle protein occurs via the ubiquitin-proteasome pathway [55]. The ubiquitin-proteasome controls cellular proteolytic degradation of ubiquitinated proteins [56]. TNF-α administration induces elevation in ubiquitin expression and upregulation of markers associated with proteolytic degradation [55]. Upregulation of ubiquitin-conjugating activity in skeletal muscle has been reported to occur in a TNF-α/NF-κB-dependent manner [57].
The loss of muscle mass and significant reduction in muscle force as a result of TNF-α exposure have been widely described to be associated with elevated production of ROS [48]. Using a rodent model of TNF-α-induced cachexia, muscle loss was found to be ablated following pre-treatment with nitro-L-arginine, a known nitric oxide synthase (NOS) inhibitor [58]. The upregulation of NF-κB by TNF-α in skeletal muscle is reported to be controlled, in part, by the glutathione pathway; suppression of glutathione reductase activity reduced TNF-α-induced NF-κB activation [59]. More recently, treatment of muscle fibres with the antioxidant trolox (a vitamin E derivative) resulted in attenuation in the TNF-α-induced fall in specific force generation by muscle [51]. Moreover, the specific effect of ROS on muscle wasting has been investigated widely. Treatment of C2C12 myotubes with hydrogen peroxide (H2O2) resulted in the upregulation of the expression of ubiquitin ligases responsible for controlling protein degradation via the proteasome [60]. ROS-mediated muscle proteolysis has also been associated with Ca2+ calpain activity. Elevated formation of reactive aldehyde complexes by ROS causes accumulation of Ca2+ in the cytosol, due to disruption of Ca2+ transport across the plasma membrane [61], thus, inducing calpain-mediated cleavage of key proteins such as titin and nebulin, which are components of the contractile architecture [62]. Although the effect of ROS on skeletal muscle is profound, it is still unclear whether elevated ROS forms part of a downstream signalling cascade that mediates muscle atrophy.
3.3 Role of Other Cytokines in Muscle Atrophy
Although TNF-α is arguably one of the most well-studied cytokines in the context of muscle atrophy, there are other cytokines/chemokines which have an important role to play. Interleukin-6 (IL-6) is a classical pro-inflammatory cytokine, which harbours ancillary function in terms of influencing metabolism [63, 64]. A seminal study in the mid-1990s, whereby treatment of transgenic IL-6 overexpressor mice with an IL-6 receptor antibody, ameliorated muscle atrophy in this model [65]. Similarly, more recent evidence in the Apc (Min/+) murine model exhibit IL-6-dependent muscle atrophy – mediated through activation of atrogin-1 [66]. In a further rodent study, IL-6 was reported to induce atrophy via downregulation of ribosomal S6 kinase phosphorylation – favouring a more catabolic state [67]. Moreover, in vitro studies in murine C2C12 cells have demonstrated IL-6 to inhibit myogenic differentiation [68]. There is also clinically relevant evidence for an important role for IL-6 in muscle atrophy. Patients with polymyositis and dermatomyositis present with elevated circulating levels of Il-6, which correlate with disease severity [69]. Moreover, use of an anti-IL-6R monoclonal antibody ameliorated disease progression in a murine C-reactive protein-induced model of myositis [70]. In addition a small cohort of treatment refractory polymyositis patients treated with the commercial anti-IL-6R tocilizumab has showed beneficial clinical outcomes – evidenced by reduced circulating creatine kinase levels and suppressed myo-oedema [71]. Interestingly, there has been an observation of acquired inflammatory myopathy developing in a patient treated with tocilizumab – however, this is an exceptionally rare occurrence [30]. Overall, there is strong mechanistic evidence for the role of IL-6 in muscle atrophy – with significant interest from global pharma in pursuing trials of anti-IL-6 therapies in a range of myopathies.
4 Future Perspectives
Our understanding of the basic biology, which mediates the impact of NF-κB and inflammatory cytokines on muscle, has developed exponentially over the last decade. The potential to target NF-κB signalling to target muscle wasting in a range of myopathologies is an attractive proposition. Currently, however the vast majority of success has been in animal models – with limited evidence in humans. Thus, there is still a crucial need to better understand the precise impact and potential long-term effects of NF-κB-modulating therapies.
References
Lightfoot A, McArdle A, Griffiths RD (2009) Muscle in defense. Crit Care Med 37(10 Suppl):S384–S390. https://doi.org/10.1097/CCM.0b013e3181b6f8a500003246-200910001-00013 [pii]
Fanzani A, Conraads VM, Penna F, Martinet W (2012) Molecular and cellular mechanisms of skeletal muscle atrophy: an update. J Cachexia Sarcopenia Muscle 3(3):163–179. https://doi.org/10.1007/s13539-012-0074-6
Ghosh S, Karin M (2002) Missing pieces in the NF-kappaB puzzle. Cell 109(Suppl):S81–S96
Hayden MS, Ghosh S (2011) NF-kappaB in immunobiology. Cell Res 21(2):223–244. doi:cr201113 [pii]. https://doi.org/10.1038/cr.2011.13
Carmody RJ, Ruan Q, Liou HC, Chen YH (2007) Essential roles of c-Rel in TLR-induced IL-23 p19 gene expression in dendritic cells. J Immunol 178(1):186–191 doi:178/1/186 [pii]
Ashall L, Horton CA, Nelson DE, Paszek P, Harper CV, Sillitoe K, Ryan S, Spiller DG, Unitt JF, Broomhead DS, Kell DB, Rand DA, See V, White MR (2009) Pulsatile stimulation determines timing and specificity of NF-kappaB-dependent transcription. Science 324(5924):242–246. doi:324/5924/242 [pii]. https://doi.org/10.1126/science.1164860
Idriss HT, Naismith JH (2000) TNF alpha and the TNF receptor superfamily: structure-function relationship(s). Microsc Res Tech 50(3):184–195
Plomgaard P, Penkowa M, Pedersen BK (2005) Fiber type specific expression of TNF-alpha, IL-6 and IL-18 in human skeletal muscles. Exerc Immunol Rev 11:53–63
Hotamisligil GS, Shargill NS, Spiegelman BM (1993) Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 259(5091):87–91
Guttridge DC, Mayo MW, Madrid LV, Wang CY, Baldwin AS Jr (2000) NF-kappaB-induced loss of MyoD messenger RNA: possible role in muscle decay and cachexia. Science 289(5488):2363–2366
Lexell J (1993) Ageing and human muscle: observations from Sweden. Can J Appl Physiol 18(1):2–18
Cuthbertson D, Smith K, Babraj J, Leese G, Waddell T, Atherton P, Wackerhage H, Taylor PM, Rennie MJ (2005) Anabolic signaling deficits underlie amino acid resistance of wasting, aging muscle. FASEB J 19(3):422–424. https://doi.org/10.1096/fj.04-2640fje
Vasilaki A, McArdle F, Iwanejko LM, McArdle A (2006) Adaptive responses of mouse skeletal muscle to contractile activity: The effect of age. Mech Ageing Dev 127(11):830–839. https://doi.org/10.1016/j.mad.2006.08.004
Lightfoot AP, Cooper RG (2016) The role of myokines in muscle health and disease. Curr Opin Rheumatol 28(6):661–666. https://doi.org/10.1097/BOR.0000000000000337
Monici MC, Aguennouz M, Mazzeo A, Messina C, Vita G (2003) Activation of nuclear factor-kappaB in inflammatory myopathies and Duchenne muscular dystrophy. Neurology 60(6):993–997
Yang CC, Askanas V, Engel WK, Alvarez RB (1998) Immunolocalization of transcription factor NF-kappaB in inclusion-body myositis muscle and at normal human neuromuscular junctions. Neurosci Lett 254(2):77–80
Schneider C, Gold R, Dalakas MC, Schmied M, Lassmann H, Toyka KV, Hartung HP (1996) MHC class I-mediated cytotoxicity does not induce apoptosis in muscle fibers nor in inflammatory T cells: studies in patients with polymyositis, dermatomyositis, and inclusion body myositis. J Neuropathol Exp Neurol 55(12):1205–1209
Nagaraju K, Casciola-Rosen L, Lundberg I, Rawat R, Cutting S, Thapliyal R, Chang J, Dwivedi S, Mitsak M, Chen YW, Plotz P, Rosen A, Hoffman E, Raben N (2005) Activation of the endoplasmic reticulum stress response in autoimmune myositis: potential role in muscle fiber damage and dysfunction. Arthritis Rheum 52(6):1824–1835. https://doi.org/10.1002/art.21103
Nowak KJ, Davies KE (2004) Duchenne muscular dystrophy and dystrophin: pathogenesis and opportunities for treatment. EMBO Rep 5(9):872–876. https://doi.org/10.1038/sj.embor.7400221
Acharyya S, Villalta SA, Bakkar N, Bupha-Intr T, Janssen PM, Carathers M, Li ZW, Beg AA, Ghosh S, Sahenk Z, Weinstein M, Gardner KL, Rafael-Fortney JA, Karin M, Tidball JG, Baldwin AS, Guttridge DC (2007) Interplay of IKK/NF-kappaB signaling in macrophages and myofibers promotes muscle degeneration in Duchenne muscular dystrophy. J Clin Invest 117(4):889–901. https://doi.org/10.1172/JCI30556
Bhatnagar S, Panguluri SK, Gupta SK, Dahiya S, Lundy RF, Kumar A (2010) Tumor necrosis factor-alpha regulates distinct molecular pathways and gene networks in cultured skeletal muscle cells. PLoS One 5(10):e13262. https://doi.org/10.1371/journal.pone.0013262
Lightfoot AP, Sakellariou GK, Nye GA, McArdle F, Jackson MJ, Griffiths RD, McArdle A (2015) SS-31 attenuates TNF-alpha induced cytokine release from C2C12 myotubes. Redox Biol 6:253–259. https://doi.org/10.1016/j.redox.2015.08.007
Sandri M, Sandri C, Gilbert A, Skurk C, Calabria E, Picard A, Walsh K, Schiaffino S, Lecker SH, Goldberg AL (2004) Foxo transcription factors induce the atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy. Cell 117(3):399–412
Bodine SC, Baehr LM (2014) Skeletal muscle atrophy and the E3 ubiquitin ligases MuRF1 and MAFbx/atrogin-1. Am J Physiol Endocrinol Metab 307(6):E469–E484. https://doi.org/10.1152/ajpendo.00204.2014
Cai D, Frantz JD, Tawa NE Jr, Melendez PA, Oh BC, Lidov HG, Hasselgren PO, Frontera WR, Lee J, Glass DJ, Shoelson SE (2004) IKKbeta/NF-kappaB activation causes severe muscle wasting in mice. Cell 119(2):285–298. https://doi.org/10.1016/j.cell.2004.09.027
Mourkioti F, Kratsios P, Luedde T, Song YH, Delafontaine P, Adami R, Parente V, Bottinelli R, Pasparakis M, Rosenthal N (2006) Targeted ablation of IKK2 improves skeletal muscle strength, maintains mass, and promotes regeneration. J Clin Invest 116(11):2945–2954. https://doi.org/10.1172/JCI28721
Conti F, Ceccarelli F, Massaro L, Cipriano E, Di Franco M, Alessandri C, Spinelli FR, Scrivo R (2013) Biological therapies in rheumatic diseases. Clin Ter 164(5):e413–e428. https://doi.org/10.7417/CT.2013.1622
Grounds MD, Torrisi J (2004) Anti-TNFalpha (Remicade) therapy protects dystrophic skeletal muscle from necrosis. FASEB J 18(6):676–682. https://doi.org/10.1096/fj.03-1024com
Grounds MD, Davies M, Torrisi J, Shavlakadze T, White J, Hodgetts S (2005) Silencing TNFalpha activity by using Remicade or Enbrel blocks inflammation in whole muscle grafts: an in vivo bioassay to assess the efficacy of anti-cytokine drugs in mice. Cell Tissue Res 320(3):509–515. https://doi.org/10.1007/s00441-005-1102-z
Lundberg IE, Vencovsky J, Alexanderson H (2014) Therapy of myositis: biological and physical. Curr Opin Rheumatol 26(6):704–711. https://doi.org/10.1097/BOR.0000000000000109
Kopp E, Ghosh S (1994) Inhibition of NF-kappa B by sodium salicylate and aspirin. Science 265(5174):956–959
Oh J, Sinha I, Tan KY, Rosner B, Dreyfuss JM, Gjata O, Tran P, Shoelson SE, Wagers AJ (2016) Age-associated NF-kappaB signaling in myofibers alters the satellite cell niche and re-strains muscle stem cell function. Aging (Albany NY) 8(11):2871–2896. https://doi.org/10.18632/aging.101098
Buhrmann C, Mobasheri A, Busch F, Aldinger C, Stahlmann R, Montaseri A, Shakibaei M (2011) Curcumin modulates nuclear factor kappaB (NF-kappaB)-mediated inflammation in human tenocytes in vitro: role of the phosphatidylinositol 3-kinase/Akt pathway. J Biol Chem 286(32):28556–28566. https://doi.org/10.1074/jbc.M111.256180
Pan Y, Chen C, Shen Y, Zhu CH, Wang G, Wang XC, Chen HQ, Zhu MS (2008) Curcumin alleviates dystrophic muscle pathology in mdx mice. Mol Cells 25(4):531–537
Spriggs DR, Deutsch S, Kufe DW (1992) Genomic structure, induction, and production of TNF-alpha. Immunol Ser 56:3–34
Vilcek J, Lee TH (1991) Tumor necrosis factor. New insights into the molecular mechanisms of its multiple actions. J Biol Chem 266(12):7313–7316
Smith RA, Baglioni C (1987) The active form of tumor necrosis factor is a trimer. J Biol Chem 262(15):6951–6954
Loetscher H, Pan YC, Lahm HW, Gentz R, Brockhaus M, Tabuchi H, Lesslauer W (1990) Molecular cloning and expression of the human 55 kd tumor necrosis factor receptor. Cell 61(2):351–359 doi:0092-8674(90)90815-V [pii]
Ryffel B, Mihatsch MJ (1993) TNF receptor distribution in human tissues. Int Rev Exp Pathol 34 Pt B:149–156
Chen G, Goeddel DV (2002) TNF-R1 signaling: a beautiful pathway. Science 296(5573):1634–1635. https://doi.org/10.1126/science.1071924 296/5573/1634 [pii]
Carswell EA, Old LJ, Kassel RL, Green S, Fiore N, Williamson B (1975) An endotoxin-induced serum factor that causes necrosis of tumors. Proc Natl Acad Sci U S A 72(9):3666–3670
Beutler B, Greenwald D, Hulmes JD, Chang M, Pan YC, Mathison J, Ulevitch R, Cerami A (1985) Identity of tumour necrosis factor and the macrophage-secreted factor cachectin. Nature 316(6028):552–554
Tracey KJ, Beutler B, Lowry SF, Merryweather J, Wolpe S, Milsark IW, Hariri RJ, Fahey TJ 3rd, Zentella A, Albert JD et al (1986) Shock and tissue injury induced by recombinant human cachectin. Science 234(4775):470–474
Tracey KJ, Fong Y, Hesse DG, Manogue KR, Lee AT, Kuo GC, Lowry SF, Cerami A (1987) Anti-cachectin/TNF monoclonal antibodies prevent septic shock during lethal bacteraemia. Nature 330(6149):662–664. https://doi.org/10.1038/330662a0
Casey LC, Balk RA, Bone RC (1993) Plasma cytokine and endotoxin levels correlate with survival in patients with the sepsis syndrome. Ann Intern Med 119(8):771–778
Finn PJ, Plank LD, Clark MA, Connolly AB, Hill GL (1996) Assessment of involuntary muscle function in patients after critical injury or severe sepsis. JPEN J Parenter Enteral Nutr 20(5):332–337. https://doi.org/10.1177/0148607196020005332
Lang CH, Frost RA (2007) Sepsis-induced suppression of skeletal muscle translation initiation mediated by tumor necrosis factor alpha. Metabolism 56(1):49–57 doi:S0026-0495(06)00318-0 [pii]. https://doi.org/10.1016/j.metabol.2006.08.025
Li YP, Schwartz RJ, Waddell ID, Holloway BR, Reid MB (1998) Skeletal muscle myocytes undergo protein loss and reactive oxygen-mediated NF-kappaB activation in response to tumor necrosis factor alpha. FASEB J 12(10):871–880
Li YP, Reid MB (2000) NF-kappaB mediates the protein loss induced by TNF-alpha in differentiated skeletal muscle myotubes. Am J Physiol Regul Integr Comp Physiol 279(4):R1165–R1170
Thaloor D, Miller KJ, Gephart J, Mitchell PO, Pavlath GK (1999) Systemic administration of the NF-kappaB inhibitor curcumin stimulates muscle regeneration after traumatic injury. Am J Phys 277(2 Pt 1):C320–C329
Hardin BJ, Campbell KS, Smith JD, Arbogast S, Smith J, Moylan JS, Reid MB (2008) TNF-alpha acts via TNFR1 and muscle-derived oxidants to depress myofibrillar force in murine skeletal muscle. J Appl Physiol 104(3):694–699. doi:00898.2007 [pii]. https://doi.org/10.1152/japplphysiol.00898.2007
Wilcox P, Milliken C, Bressler B (1996) High-dose tumor necrosis factor alpha produces an impairment of hamster diaphragm contractility. Attenuation with a prostaglandin inhibitor. Am J Respir Crit Care Med 153(5):1611–1615
Li X, Moody MR, Engel D, Walker S, Clubb FJ Jr, Sivasubramanian N, Mann DL, Reid MB (2000) Cardiac-specific overexpression of tumor necrosis factor-alpha causes oxidative stress and contractile dysfunction in mouse diaphragm. Circulation 102(14):1690–1696
Supinski GS, Callahan LA (2006) Caspase activation contributes to endotoxin-induced diaphragm weakness. J Appl Physiol 100(6):1770–1777. doi:01288.2005 [pii]. https://doi.org/10.1152/japplphysiol.01288.2005
Llovera M, Garcia-Martinez C, Agell N, Lopez-Soriano FJ, Argiles JM (1997) TNF can directly induce the expression of ubiquitin-dependent proteolytic system in rat soleus muscles. Biochem Biophys Res Commun 230(2):238–241 doi:S0006291X96958271 [pii]
Lecker SH, Solomon V, Mitch WE, Goldberg AL (1999) Muscle protein breakdown and the critical role of the ubiquitin-proteasome pathway in normal and disease states. J Nutr 129(1S Suppl):227S–237S
Li YP, Lecker SH, Chen Y, Waddell ID, Goldberg AL, Reid MB (2003) TNF-alpha increases ubiquitin-conjugating activity in skeletal muscle by up-regulating UbcH2/E220k. FASEB J 17(9):1048–1057
Buck M, Chojkier M (1996) Muscle wasting and dedifferentiation induced by oxidative stress in a murine model of cachexia is prevented by inhibitors of nitric oxide synthesis and antioxidants. EMBO J 15(8):1753–1765
Sen CK, Khanna S, Reznick AZ, Roy S, Packer L (1997) Glutathione regulation of tumor necrosis factor-alpha-induced NF-kappa B activation in skeletal muscle-derived L6 cells. Biochem Biophys Res Commun 237(3):645–649
Li YP, Chen Y, Li AS, Reid MB (2003) Hydrogen peroxide stimulates ubiquitin-conjugating activity and expression of genes for specific E2 and E3 proteins in skeletal muscle myotubes. Am J Physiol Cell Physiol 285(4):C806–C812
Siems W, Capuozzo E, Lucano A, Salerno C, Crifo C (2003) High sensitivity of plasma membrane ion transport ATPases from human neutrophils towards 4-hydroxy-2,3-trans-nonenal. Life Sci 73(20):2583–2590 doi:S0024320503006611 [pii]
Purintrapiban J, Wang MC, Forsberg NE (2003) Degradation of sarcomeric and cytoskeletal proteins in cultured skeletal muscle cells. Comp Biochem Physiol B Biochem Mol Biol 136(3):393–401
Benatti FB, Pedersen BK (2015) Exercise as an anti-inflammatory therapy for rheumatic diseases-myokine regulation. Nat Rev Rheumatol 11(2):86–97. https://doi.org/10.1038/nrrheum.2014.193
Pal M, Febbraio MA, Whitham M (2014) From cytokine to myokine: the emerging role of interleukin-6 in metabolic regulation. Immunol Cell Biol 92(4):331–339. https://doi.org/10.1038/icb.2014.16
Tsujinaka T, Fujita J, Ebisui C, Yano M, Kominami E, Suzuki K, Tanaka K, Katsume A, Ohsugi Y, Shiozaki H, Monden M (1996) Interleukin 6 receptor antibody inhibits muscle atrophy and modulates proteolytic systems in interleukin 6 transgenic mice. J Clin Invest 97(1):244–249. https://doi.org/10.1172/JCI118398
Baltgalvis KA, Berger FG, Pena MM, Davis JM, White JP, Carson JA (2009) Muscle wasting and interleukin-6-induced atrogin-I expression in the cachectic Apc ( Min/+ ) mouse. Pflugers Arch 457(5):989–1001. https://doi.org/10.1007/s00424-008-0574-6
Haddad F, Zaldivar F, Cooper DM (1985) Adams GR (2005) IL-6-induced skeletal muscle atrophy. J Appl Physiol 98(3):911–917. https://doi.org/10.1152/japplphysiol.01026.2004
Pelosi M, De Rossi M, Barberi L, Musaro A (2014) IL-6 impairs myogenic differentiation by downmodulation of p90RSK/eEF2 and mTOR/p70S6K axes, without affecting AKT activity. Biomed Res Int 2014:206026. https://doi.org/10.1155/2014/206026
Kawasumi H, Gono T, Kawaguchi Y, Kaneko H, Katsumata Y, Hanaoka M, Kataoka S, Yamanaka H (2014) IL-6, IL-8, and IL-10 are associated with hyperferritinemia in rapidly progressive interstitial lung disease with polymyositis/dermatomyositis. Biomed Res Int 2014:815245. https://doi.org/10.1155/2014/815245
Okiyama N, Sugihara T, Iwakura Y, Yokozeki H, Miyasaka N, Kohsaka H (2009) Therapeutic effects of interleukin-6 blockade in a murine model of polymyositis that does not require interleukin-17A. Arthritis Rheum 60(8):2505–2512. https://doi.org/10.1002/art.24689
Narazaki M, Hagihara K, Shima Y, Ogata A, Kishimoto T, Tanaka T (2011) Therapeutic effect of tocilizumab on two patients with polymyositis. Rheumatology (Oxford) 50(7):1344–1346. https://doi.org/10.1093/rheumatology/ker152
Acknowledgements
The authors would like to thank Dr. Shelley Rawson for helpful discussion in the preparation of this chapter.
Competing Financial Interest
The authors declare no competing financial interests.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Thoma, A., Lightfoot, A.P. (2018). NF-kB and Inflammatory Cytokine Signalling: Role in Skeletal Muscle Atrophy. In: Xiao, J. (eds) Muscle Atrophy. Advances in Experimental Medicine and Biology, vol 1088. Springer, Singapore. https://doi.org/10.1007/978-981-13-1435-3_12
Download citation
DOI: https://doi.org/10.1007/978-981-13-1435-3_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1434-6
Online ISBN: 978-981-13-1435-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)